Back to Journals » Journal of Pain Research » Volume 17
Studies on Pain Associated with Anxiety or Depression in the Last 10 Years: A Bibliometric Analysis
Authors Zhang Q , Sun H , Xin Y, Li X, Shao X
Received 28 August 2023
Accepted for publication 21 December 2023
Published 5 January 2024 Volume 2024:17 Pages 133—149
DOI https://doi.org/10.2147/JPR.S436500
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jonathan Greenberg
Qianyuan Zhang,1 Haiju Sun,1 Yinuo Xin,1 Xiaoyu Li,1 Xiaomei Shao1,2
1Key Laboratory of Acupuncture and Neurology of Zhejiang Province, Department of Neurobiology and Acupuncture Research, The Third Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou, 310053, People’s Republic of China; 2Key Laboratory for Research of Acupuncture Treatment and Transformation of Emotional Diseases, The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, 310009, People’s Republic of China
Correspondence: Xiaomei Shao, Email [email protected]
Background: The prevalence of pain comorbid and anxiety/depression in clinical observations has been high, and the number of related publications has increased in recent years. Nevertheless, few studies have used bibliometric methods to analyze the scientific research on comorbid pain and depression/anxiety. The aim of this study was to systematically examine the trends in global scientific research on comorbid pain and depression/anxiety from 2012 to 2022.
Methods: Papers published between 2012 and 2022 were identified in the Web of Science database. Publications that examined comorbid pain and depression/anxiety were included. The language was limited to English. CiteSpace, Excel and VOSviewer were used to analyze the volume of publications, countries, institutions, authors, cocited authors, and keywords.
Results: A total of 30,290 papers met the inclusion criteria of the study. Using CiteSpace, VOSviewer and Excel, the results showed that the United States (10,614 publications), Harvard University (1195 publications), and Jensen, Mark P. (77 publications) were the most productive country, institution, and author, respectively. The hotspots and frontiers were “relationship between depression and pain”, “gender differences in pain and depression/anxiety domains”, “study of specific pain types with depression/anxiety”, “treatment of pain combined with anxiety/depression”, and “effects of COVID-19 on patients with pain combined with depression/anxiety”.
Conclusion: These findings indicate a growing interest in the field of comorbid pain and depression/anxiety. The research has been broad and deep, but there is still much room for growth. Furthermore, there is a need for more mature global collaborative networks as well as more high-quality research results in the future.
Keywords: pain, depression, anxiety, bibliometric analysis, CiteSpace, VOSviewer
Introduction
The International Association for the Study of Pain (IASP) defines pain as “an unpleasant subjective sensory and emotional experience associated with tissue damage or potential tissue damage”. Traditionally, pain is categorized as either acute pain or chronic pain. Chronic pain affects approximately 20% of adults in developed countries, including more than 7500 individuals in the US, and pain is a major cause of functional disability.1 In addition, pain results in a considerable medical burden worldwide. The prevalence and cost of chronic pain are major health care problems in the U.S.2,3 The total cost of pain accounted for up to 3% of the gross domestic product of European countries, which was much greater than the cost of cancer or heart disease.4 Pain negatively affects the daily activities of most patients and can have adverse effects on mental health, employment status, sleep, etc.5 Additionally, various biological, psychological, and social factors dynamically influence the perception of pain.6 Men and women respond differently to pain, such that women tend to exhibit higher pain sensitivity and a higher risk of clinical pain.7
Anxiety and depression are the most prevalent mental illnesses and are among the top 10 causes of disability worldwide. Depression is characterized by altered mood states, such as a reduced experience of positive emotions, and cognitive impairments, such as difficulties with attention and memory.8 Anxiety is a psychological and physiological emotional state that is a general reflection of stressful situations and can be triggered when an individual’s physical functioning and quality of life are severely impaired.9 According to a report by the World Health Organization, the global prevalence of depression is estimated to be 4.9%,10 and that of anxiety is approximately 20%, suggesting that 350 million people in the world suffer from depression and that 264 million people are affected by anxiety disorders.
The subjective perception of pain is emphasized in the definition of pain, and previous studies have revealed that pain has both sensory-discriminative and emotional-affective dimensions.11 This raises a new question: what is the role of maladaptive emotions, such as depression/anxiety, in the perception of pain?12,13 Previous studies have demonstrated that there is a high degree of comorbidity between pain and depression.14,15 An epidemiological investigation showed that the prevalence of depression in patients with chronic pain was 52%, and 65% of depressed patients had pain symptoms.16 Acute pain can adversely affect a patient’s mood after surgery. In the same postoperative period, the incidence of depression was reported to range from 21% to 50% in the study population with low preoperative levels of depression (0–11.8%), which indicates that pain can adversely affect the prognosis and treatment of depression, and vice versa. Similarly, anxiety can increase pain levels.17 Pain is partly an emotional experience, so the correspondence between pain and physical impairment is variable, and the interactions among pain, depression, and anxiety symptoms are complex.18 A variety of novel therapeutic approaches, such as emotion-focused exposure treatment, are now available for chronic pain patients with cooccurring emotional problems. A variety of interventions, such as alternative pharmacotherapies (eg, ketamine, cannabinoids19) and cognitive‒behavioral therapy, have been shown to reduce the impact of pain on negative outcomes.20 Cointerventions for patients with emotional disorders (such as depression and anxiety) comorbid with pain are becoming a new trend in treatment. With the continuous development of pain therapeutics and psychosomatic medicine, the relationships between pain, anxiety, and depression have attracted an increasing amount of attention. Therefore, understanding the current research trends and hot spots in this field may help us with in-depth research and thus yield new insights into the treatment of pain patients.
Bibliometric analysis is a tool that combines data mining and visualization to evaluate scientific research both quantitatively and qualitatively and to predict research trends in specific fields. The current study used CiteSpace and VOSviewer, two bibliometric analysis software packages, to construct visual maps of global trends in pain and anxiety/depression-related research. A visual analysis of the literature can provide a valuable, timely, reproducible, and flexible way to summarize valuable information that may be hidden under detailed information, such as authors, institutions, countries, journals, or keywords. In this study, a comprehensive analysis of the global literature published in the past 10 years on the relationship between pain and anxiety/depression was conducted using a bibliometric approach through CiteSpace and VOSviewer. The aim of this study was to provide insights regarding the study of new treatments and therapies for pain.
Materials and Methods
Literature Sources and Retrieval Methods
The data were downloaded from the WOS database on August 4, 2023. The data retrieval strategy was as follows: ((TS=(depression)) OR TS=(anxiety)) AND TS=(pain).
The types of literature selected for this study were articles and reviews. Letters, editorial materials, etc., were excluded. The retrieval period was set to 10 years, so only articles published between 2012 and 2022 were included. In addition, the language of publication was limited to English to ensure the accurate interpretation of the results. A total of 31,706 articles were downloaded based on this advanced search strategy. After eliminating duplicate records, 30,290 studies remained. The specific search strategies and results are shown in Table 1.
 |
Table 1 Data Sources |
Data Extraction and Analysis Methods
EndNote X9 and Microsoft Excel 2019 were used to download publications and extract data. The data were downloaded in plain text format with complete records and references and then imported into VOSviewer and CiteSpace for analysis. VOSviewer and CiteSpace were then used to construct maps based on the bibliometrics. The setup parameters for VOSviewer are as follows. The full counting method was employed, and the maximum number of documents was set at 25. Full counting means that the mapping is performed exclusively according to the frequency of cocitations or co-occurrences rather than weights. The purpose of setting the maximum number of documents is to ensure that the proper number of nodes and links are displayed in the graph. The time slice in CiteSpace was set to “1”, and the time partition was set to run from 2012 to 2022. For the set factor G-index (k = 25), the top N was set to 25. The “time slice” was set to “1”, which means that the software generated network diagrams for each year and then synthesized the network diagrams of each year in the final result. The G-index is an arithmetic index, and the larger the value of k is, the more data will be derived. Based on the large number of articles, we chose a value of 25. This index takes into account both the quantity and quality of researchers’ academic outputs and measures the research results of the researcher. In the top N, we selected the 25 countries with the highest number of occurrences or citations for use in the mapping. Nodes were used to select countries, institutions, authors, and keywords. According to the requirements, a visual knowledge map was drawn. In the knowledge graph, the node size represents the frequency of co-occurrence or reference. The color of the node indicates the year, and the connections between the nodes indicate cooperation, co-occurrence, or cocitation. A node with high centrality is the key node in a specific field and is an important indicator of the degree of influence. Sudden detection marks an outbreak in a certain period of research and was the research hotspot at that time.
Results
Analysis of Annual Publications
A total of 300,783 records on depression or anxiety and 317,368 records on pain were identified, which indicates that both areas are receiving considerable attention (Table 1). The search strategy yielded 31,706 papers, including 27,444 articles and 4262 reviews. After removing duplicates, 30,290 papers remained.
Figure 1 shows a significant increase in the number of papers published each year since 2012, with 1775 papers related to pain and anxiety or depression published in 2012. By 2022, 10 years later, the number of works published each year was almost three times that of 2012. The number of publications per year reached its peak in 2022 (n=4507).
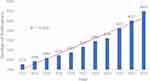 |
Figure 1 Number of articles published and the mode fitting curve from 2012 to 2022. |
In addition, a growth trend model [coefficient of determination (R2) = 0.952] was produced using Excel, which showed that there was a significant correlation between publication year and publication quantity (Figure 1).
Analysis of Countries or Regions and Institutions
The publications from England, Scotland, Northern Ireland, and Wales were reclassified as being from the UK, and publications from Taiwan were reclassified as being from China. Therefore, the 30,290 publications on pain, anxiety, and depression were published across 152 countries or regions. Table 2 shows the number of publications from the top 10 countries or regions. The largest number of publications came from the United States (10,614, 35.04%), followed by China (2919, 9.64%), the UK (2507, 8.28%), Canada (2074, 6.84%), and Germany (1814, 5.99%; Table 2). In the collaborative network constructed using CiteSpace, the size of nodes represents the number of publications published in a country or region, and the lines in the network represent the collaborative relationships between countries. As shown in Figure 2, the collaboration between countries/regions is shown in the network diagram, with a total of 31 nodes and 238 links. Studies on pain and anxiety/depression were published from 692 institutions. The top 10 institutions published 7783 papers, accounting for approximately 25.69% of the total number of papers (Table 2). Harvard University (1195, 3.95%) was the most prolific institution (Table 2), followed by the University of California System (1103 papers, 3.64%), the US Department of Veterans Affairs (794, 2.62%), and the Veterans Health Administration (774, 2.53%). Figure 3 shows the network of institutions.
 |
Table 2 Top 10 Countries and Institutions Contributed to the Publications |
 |
Figure 2 The collaboration network of countries related to pain associated with anxiety or depression. |
 |
Figure 3 The collaboration network of institutions related to pain associated with anxiety or depression. |
Analysis of Authors and Cocited Authors
Analysis of Authors
A total of 130,238 authors contributed 30,290 articles (Figure 4). Table 3 lists the 10 most prolific authors. The most prolific authors were Mark P. Jensen and David Ring. Mark P. Jensen mainly studied the relationship between pain and psychological state in different subject groups, such as adolescents and veterans. He also studied the relationships between different degrees of pain and psychological factors, such as chronic pain and high-impact chronic pain; different pain types, including low back pain, back pain, musculoskeletal pain, and migraine; and different psychological states, such as anxiety, depression, sleep disorders, and cognitive decline. David Ring mainly studied the relationship between recovery after musculoskeletal injury and mental health. Figure 5 shows the relationships between the top ten authors according to the number of publications. Jensen Mark P, Edwards Robert R, Gerdle Bjorn, and Vlaeyen Johan W.S. all made significant contributions in the field of clinical neurology. Jensen Mark P, in particular, has published 160 articles in this field. Ring David and Vran Ceanu Ana-naria have each contributed to the field of orthopedics. Ring David published 492 articles, while Vran Ceanu Ana-naria published 57. Bruera Eduaro and Miaskowski Christine published 488 and 252 articles on oncology, respectively. Figure 6 shows the top 20 most cited authors by starting year. Dekker, Joost, Kashikar-zuck, and Susmita were cocited for the longest time; they were cited for 5 years before 2022. Furthermore, Li, Jie Wang, Wei Smith, Lee, Schwedt, and Todd J. Mayer Emeran A and Van oudenhove Lukas co-authored seven articles on brain-gut interactions from 2010 to 2021. Koyanagi Ai and Vancampfort Davy have been working together since 2016 and have published 73 articles as of 2023. In 2018, they published the most articles together.21 Their first published article was on the epidemiology of back pain in individuals with depression, psychosis, anxiety, sleep disorders, and stress sensitivity. The article noted that depression, psychosis, anxiety, sleep disturbances, and stress sensitivity are closely related to back pain – specifically, they are significantly related to chronic back pain.22 Koyanagi Ai has also worked with Smith Lee. The two began working together in 2018 and have continued working together as of 2023. In 2021, these two authors published the most articles together (62). Vancampfort Davy and Smith Lee coauthored articles in Psychiatry from 2017 to 2022; across their articles, depression, somatization and anxiety were the most frequent keywords. The trio of Zvolensky Michael J, Rogers Andrew H, and Ditre Joseph W have been coauthoring articles in Substance Abuse, Psychology Clinical, and other journals since 2018.
 |
Table 3 Top 10 Authors and Co-Cited Authors of Pain and Anxiety/Depression Research |
 |
Figure 4 The co-occurrence network of authors on pain associated with anxiety or depression. |
 |
Figure 5 The collaborative network of top 10 authors in terms of posting volume. |
 |
Figure 6 Top 20 Authors with the strongest citation bursts. |
Analysis of Co-Cited Authors
A total of 365,651 cocited authors were included in this paper for visual analysis. Figure 7 shows the collaboration network of the authors with a cocited frequency >22. Among them, Kroenke and K were the most frequently cited, with 3381 citations. His earliest research was on the relationship between physical illness and psychodynamic psychotherapy. The influence of mental health on physical health cannot be ignored.
 |
Figure 7 The collaborative network of authors with a total of more than 22 citations. |
Analysis of Co-Cited References
A cocited reference is defined as one or more references that were cocited in one or more publications. The top 10 cocited references on pain and anxiety/depression are shown in Table 4. The citation volume of the top 10 cocited references in this study ranged from 104 to 231. The most highly cited reference was the Diagnostic and Statistical Manual of Mental Disorders, which was published in 2013 (231 citations), followed by the CDC guideline for prescribing, which was published in 2016 in the MMWR Recomm Rep (170 citations).
 |
Table 4 Top 10 Co-Cited References on Pain and Anxiety/Depression |
To better understand the inherent characteristics of the cited studies in a given field, a cluster analysis was carried out, and the 28,854 reference networks were divided into 16 clusters. Figure 8 shows that the labels of the clusters are located on the right side of the graph. The largest cluster was #0 neuropathic pain, followed by #1 opioids. In earlier studies, fibromyalgia (#2), catastrophizing (#5) and pet (#8) were more common. Clusters representing new developments since 2015 include chronic low back pain (#9), COVID-19 (#11), virtual reality (#13) and irritable bowel syndrome (#15).
 |
Figure 8 The timeline view for references co-citation cluster. # Represents a prefix for serial numbers. |
Analysis of Keywords
According to bibliometric theory, keywords show the hot spots and trends in the research field. Keyword analysis also provides a typical overview of research trends that represent the journal, as they reflect the focus of an article or one author.
Out of the 30,290 articles, 55,887 were extracted (Figure 9). The larger the nodes in the graph are, the more frequently this keyword appears. The top 20 keywords for frequency and centrality are listed in Table 5. Among them, the most common occurrence was depression (6853), followed by quality of life (5226), pain (5118) and anxiety (4318), which was consistent with the study theme. Among the remaining keywords, chronic pain, low back pain and neuropathic pain were common types of pain. These keywords could explain why there is such a strong relationship between pain and depression/anxiety. Depression or anxiety may cause pain, and pain may worsen depression or anxiety. Research on the mechanism of pain may be important for exploring the mechanism of action against depression; further research is needed to prove this. Burst detection of keywords based on the growth rate of keyword citations. The burstiness of keywords is a valuable indicator of the most active research topic; this metric tests whether a research field is hot in a given period and highlights emerging topics. Figure 10 lists the top 20 keywords with the strongest burst intensity. The keyword “major depression” had an explosive period from 2011 to 2014, with an explosive power of 27.7. The keywords “impact questionnaire”, “positron emission tomography”, “randomized” and “panic disorder” lasted the longest at 7 years, with “impact questionnaire” having the largest burst intensity at 20.59. In addition, the keywords that started to emerge in the past 3 years included opioid use (12.09), resilience (11.42) and patient-reported outcome measure (10.48). Figure 11 shows the high-frequency keywords as an overlay map, with the colors representing the average year of publication. As shown in the chart, COVID-19, mental health, distraction, etc., were emerging fields.
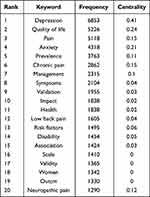 |
Table 5 Top 20 Keywords in Terms of Frequency in the Research |
 |
Figure 9 The co-occurrence network of keywords. |
 |
Figure 10 Top 20 keywords with the strongest citation bursts. |
 |
Figure 11 The overlay visualization of keywords. |
Discussion
Global Trends in Pain and Depression/Anxiety Comorbidity Research
The results of our bibliometric study provided a systematic overview of pain and depression/anxiety comorbidity research over the last decade. The global trends in published papers show that pain and depression/anxiety comorbidity research has continued to grow over time. This implies that there has been increasing interest in anxiety- or depression-related pain over the last decade.
In terms of the number of publications on comorbid pain and depression/anxiety, the highest number of publications were from the US (10,449, 36.21%), followed by the UK (2856, 9.90%), China (2792, 9.68%), Canada (2034, 7.05%) and Germany (1769, 6.13%). The top ten institutions in terms of number of publications accounted for 14.56% of the total number of papers (Table 2), and five of the top ten institutions were from the US, indicating the country’s strong scientific strength and emphasis on pain and anxiety/depression research. Figures 2 and 3 show that there is a strong link between countries and institutions and that the relationship between pain and anxiety/depression is a global issue. Developed countries and their institutions account for a larger proportion of the total number of publications. This is mainly because developed countries invest more money, technology, and personnel in the medical field, and the prevalence of chronic pain associated with anxiety/depression is more prevalent in developed countries.33 However, among the top ten countries and institutions, only three countries and two institutions have a centrality greater than 0.1, which means that most of the countries and institutions only have internal cooperation or a small amount of external cooperation. Therefore, researchers and institutions from different countries should remove academic barriers and seek more cooperation to carry out high-quality and in-depth research.
The University of Washington ranked first in terms of postings, followed by Univ Toronto (542 articles, 1.88%), Harvard Med Sch (468, 1.62%), and Univ Michigan (412, 1.43%).
Analysis of Hotspots and Frontiers in Pain Associated with Anxiety or Depression
The keyword occurrence frequency, overlay display and burst detection results were analyzed.
We have summarized the research hotspots and frontiers related to pain and anxiety/depression.
Relationship Between Depression and Pain
In recent years, pain, especially chronic pain, has been considered a disease itself rather than a simple symptom.34 The relationship between this disease and alterations in the nervous system has received increasing attention, and in chronic pain, neuroinflammation is often the result of peripheral damage and overactivity of primary sensory neurons.21,35 Walker AK found that inflammation of the central nervous system may lead to pain sensitization and chronicization.36 Hong et al proposed that the inflammatory process in depression induces changes in the central nervous system.37 Since chronic pain and depression are highly comorbid, many people have speculated that there is a common underlying mechanism. Moreover, depression plays an important role in patients’ perception of pain. People’s perception of pain varies greatly, and factors that affect pain include genetic susceptibility and sex.38 In addition, psychological processes also greatly influence the perception of pain.39 A cognitive-behavioral model has been proposed to explain the role of cognitive assessment variables in mediating the development of emotional problems after chronic pain. Currently, the most widely accepted explanation is that the relationship between pain and depression is two-way.40 However, there is ongoing controversy in the field as to whether depression is an antecedent or a consequence of pain.
Gender Differences in Pain and Depression/Anxiety Domains
The phrase “the pain field has moved on from debating whether sex differences in pain exist to recognizing the importance of these differences” was stated in a consensus report published in the journal Pain in 2007. Women are more likely than men to be diagnosed with chronic pain conditions,41 such as fibromyalgia, migraines, tension headaches, or irritable bowel syndrome. Women also have a higher risk of anxiety and depression in their lifetime,42 so women are an area of interest for researchers. In 2014, Slavich’s team proposed a social signaling theory of depression,43 which solved the key questions related to the onset and recurrence of depression and answered questions about why early-life stress can strongly predict the onset of depression, as well as comorbid anxiety and certain physical conditions, such as asthma, rheumatoid arthritis, chronic pain, and cardiovascular disease. An expansion of this kind of research has also demonstrated that ovarian hormone fluctuations modulate female susceptibility to stress, brain structure and function, and inflammatory activity and responsiveness.44
Study of Specific Pain Types in Patients with Depression/Anxiety
According to the most frequently occurring keywords, research on this particular type of pain has focused more on “chronic pain”, “low back pain” and “neuropathic pain”. Chronic pain often develops from acute pain, and this transition depends on several pain features and individual characteristics.45 Depression is considered one of the major risk factors for pain chronicity,46 and it can also predict the persistence of pain in musculoskeletal injuries. There is a wide range of chronic pain; in particular, “low back pain” and “neuropathic pain” are highly prevalent and thus have been well studied in terms of treatments and the factors affecting them. For example, fatigue severity and sensitivity exacerbate depression in patients with low back pain.47 A cutting-edge study by Hsu and YC investigated pain behaviors in rats subjected to nerve pain induced by sparse nerve injury (SNI) and inflammatory pain induced by complete Fuchs’ adjuvant (CFA) and revealed that the neuropathically pained rats exhibited more pronounced depressive-like behaviors.48
The predicted hotspots for future pain types based on keywords with high burst intensity were “acute myocardial infarction”, “rheumatoid arthritis”, “peripheral nerve injury”, and “tension type headache”. Research on these types of pain has focused primarily on the relationship between disease severity and depression/anxiety levels,49,50 the correlation of disease comorbidity depression/anxiety with sleep disorders51 and ways of responding to pain.52
Treatment of Pain Combined with Anxiety/Depression
There are multiple treatments for pain combined with anxiety/depression. Examples include traditional medications, including antidepressants (serotonin and norepinephrine reuptake inhibitors, among others), approved by the Federal Drug Administration (FDA) for the treatment of depression, and various chronic pain conditions. The keyword burst chart shows that positron emission tomography, integrative medicine, medical marijuana, etc., are also gaining importance in treatment. Among them, PET/CT combines the functional imaging of PET and the anatomical information of CT to show the metabolism, function, blood flow, cell proliferation and receptor distribution of tissue cells at the molecular level. This method is widely used to examine tumors, cardiovascular diseases, neurological lesions, etc., to provide information on the physiological and pathological diagnosis of diseases for clinical and experimental studies. PET/CT has become an indispensable and important imaging method, and it has been proven to be one of the most important means for the research and treatment of pain combined anxiety/depression.53 Additionally, the combination of Western and Chinese medicine is receiving increasing amounts of attention worldwide. Acupuncture, a traditional Chinese medical treatment, has also been proven to be very effective in treating chronic pain and depression, even in primary care. Often, acupuncture is used as a complementary method and has been shown to be effective at reducing depression and pain when compared to counseling or routine care alone.54,55 Additionally, the use of machine learning is growing in the United States and Europe, but there is conflicting evidence about its effectiveness and safety.22,56 The number of studies in this area is also increasing.
Notably, long-term opioid use (>90 days) is significantly associated with an increased risk of a new depression diagnosis.57 In 2017, prescription opioids accounted for 36% of opioid-related overdose deaths in the United States.58 After strong advocacy for the safer use of opioids for chronic pain in accordance with the 2016 CDC guidelines, that percentage dropped to 32% in 2018.59 Preventing the opioid crisis is especially important in chronic pain, such as advanced cancer pain.60 The potential mechanisms underlying the association between opioid use and new depressive diagnoses and the extent of the association between opioid use and death in patients with chronic pain need to be determined.
Impact of COVID-19 on Patients with Pain Combined with Depression/Anxiety
After it was first reported in China in December 2019, COVID-19 caused a pandemic, infecting more than 73 million people worldwide and killing more than 660 people as a result. Pain, including myalgia, headache, and chest pain, is one of the common symptoms in patients infected with COVID-1961 and is one of the leading causes of disability. The impact of COVID-19 is particularly pronounced in patients with pain combined with depression/anxiety. In one study, 98% of patients were forced to stop complementary or alternative treatments during blockade, and higher levels of anxiety and depression were significantly associated with subjective perceptions of deterioration.62 Several studies have investigated significant increases in VAS pain intensity and depression/anxiety levels in chronic pain patients during the COVID-19 pandemic compared to the prepandemic period.63,64 An increasing number of studies have examined on the mechanism through which COVID-19 mediates the increase in pain and depression/anxiety levels in patients; however, there are still few definitive validated results.65,66
Strengths and Limitations
The visualization of knowledge maps is helpful for highlighting research topics, hot spots, and trends in the field of pain related to anxiety and depression. We found other bibliometric articles that involved specific psychological topics and other articles on pain, but there were no specific bibliometrics linking anxiety/depression to pain. Therefore, this paper is a novel article on this topic. This study has several limitations.
First, publications were collected from only the WOSCC database, which means that some influential literature may have been omitted from the analysis. Therefore, other databases, such as Scope, EBSCO, and Purchest, can be used to supplement bibliometric analyses in future research. The language of the publications was English only, and only articles and reviews were selected as publication types; other types of articles were excluded because they may have obscured some hot spots in this field. Finally, the number of papers related to pain and anxiety/depression may increase rapidly, and the constant updating of databases may lead to discrepancies between the data from the literature analysis and the actual research progress.
Conclusion
An analysis of the number of papers published each year showed that the field of pain, depression and anxiety is currently undergoing a period of rapid growth. The analysis of countries, institutions and authors indicated an increasingly microscopic perspective of observation, but the consistency is clear: this is a global research topic. However, the overall collaborative network is not yet mature enough. In terms of keywords, the relationships between pain and depression/anxiety, sex differences, different types of pain, treatment modalities, and the relationship of pain with COVID-19 are research hotspots and future trends. Overall, research in the area of pain and depression/anxiety has been extensive and in-depth, but there is still much potential for development. Furthermore, there is a need for more mature global collaborative networks and high-quality research results in the future.
Data Sharing Statement
The date used to support the present findings are available from the first author or the corresponding author a reasonable request.
Funding
This work was financially supported by National Natural Science Foundation of China: 82074518; China Postdoctoral Science Foundation: 2022M722853; Postgraduate Science Foundation of Zhejiang Chinese Medical University: 2022YKJ08.
Disclosure
The authors report no conflicts of interest.
References
1. Pergolizzi J, Ahlbeck K, Aldington D, et al. The development of chronic pain: physiological change necessitates a multidisciplinary approach to treatment. Curr Med Res Opin. 2013;29(9):1127–1135. doi:10.1185/03007995.2013.810615
2. Loeser JD, Melzack R. Pain: an overview. Lancet. 1999;353(9164):1607–1609. doi:10.1016/S0140-6736(99)01311-2
3. Gatchel RJ, Peng YB, Peters ML, Fuchs PM, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. doi:10.1037/0033-2909.133.4.581
4. Henschke N, Kamper SJ, Maher CG. The epidemiology and economic consequences of pain. Mayo Clin Proc. 2015;90(1):139–147. doi:10.1016/j.mayocp.2014.09.010
5. McCarberg BH, Nicholson BD, Todd KH, Palmer T, Penles L. The impact of pain on quality of life and the unmet needs of pain management: results from pain sufferers and physicians participating in an Internet survey. Am J Ther. 2008;15(4):312–320. doi:10.1097/MJT.0b013e31818164f2
6. Fillingim RB. Individual differences in pain: understanding the mosaic that makes pain personal. Pain. 2017;158(Suppl 1):S11–S18. doi:10.1097/j.pain.0000000000000775
7. Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111(1):52–58. doi:10.1093/bja/aet127
8. Dehn LB, Beblo T. Depressed, biased, forgetful: the interaction of emotional and cognitive dysfunctions in depression. Neuropsychiatr. 2019;33(3):123–130. doi:10.1007/s40211-019-0307-4
9. Oei TP, Boschen MJ. Clinical effectiveness of a cognitive behavioral group treatment program for anxiety disorders: a benchmarking study. J Anxiety Disord. 2009;23(7):950–957. doi:10.1016/j.janxdis.2009.06.004
10. Smith K. Mental health: a world of depression. Nature. 2014;515(7526):181. doi:10.1038/515180a
11. Du JY, Fang JF, Wen C, et al. The effect of electroacupuncture on PKMzeta in the ACC in regulating anxiety-like behaviors in rats experiencing chronic inflammatory pain. Neural Plast. 2017;2017:1–13. doi:10.1155/2017/3728752
12. Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168–176.
13. Boersma K, Södermark M, Hesser H, et al. Efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: a randomized controlled trial. Pain. 2019;160(8):1708–1718. doi:10.1097/j.pain.0000000000001575
14. Means-Christensen AJ, Roy-Byrne PP, Sherbourne CD, et al. Relationships among pain, anxiety, and depression in primary care. Depression Anxiety. 2008;25(7):593–600. doi:10.1002/da.20342
15. Hampton SN, Nakonezny PA, Richard HM, Wells JE. Pain catastrophizing, anxiety, and depression in Hip pathology. Bone Joint J. 2019;101-b(7):800–807. doi:10.1302/0301-620X.101B7.BJJ-2018-1309.R1
16. Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–2445. doi:10.1001/archinte.163.20.2433
17. Lumley MA, Cohen JL, Borszcz GS, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol. 2011;67(9):942–968. doi:10.1002/jclp.20816
18. Gómez Penedo JM, Rubel JA, Blättler LA, et al. The complex interplay of pain, depression, and anxiety symptoms in patients with chronic pain: a network approach. Clin J Pain. 2020;36(4):249–259. doi:10.1097/AJP.0000000000000797
19. Ishak WW, Wen RY, Naghdechi L, et al. Pain and depression: a systematic review. Harvard Rev Psychiatry. 2018;26(6):352–363. doi:10.1097/HRP.0000000000000198
20. Thong ISK, Tan G, Jensen MP. The buffering role of positive affect on the association between pain intensity and pain related outcomes. Scand J Pain. 2017;14(1):91–97. doi:10.1016/j.sjpain.2016.09.008
21. Paladini A, Fusco M, Coaccioli S, Skaper SD, Varrassi G. Chronic pain in the elderly: the case for new therapeutic strategies. Pain Physician. 2015;18(5):E863–E876.
22. Aarstad HJ, Aarstad KH, Heimdal J, Olofsson J. Mood, anxiety and sense of humor in head and neck cancer patients in relation to disease stage, prognosis and quality of life. Acta Oto Laryngologica. 2005;135(5):1–20.
23. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. American Psychiatric Publishing, Inc. 2013.
24. Deborah D, Tamara MH, Roger C CDC guideline for prescribing opioids for chronic pain - United States. MMWR Recomm Rep. 2016. doi:10.1001/jama.2016.1464
25. Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American college of rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010. doi:10.1002/acr.20140
26. Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States. MMWR-Morbidity and Mortality Weekly Report. 2018. doi: 10.15585/mmwr.mm6736a2
27. Sheng JY, Liu S, Wang YC, et al. The link between depression and chronic pain: neural mechanisms in the brain. Neural Plast. 2017. doi:10.1155/2017/9724371
28. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States. Jama-Journal of The American Medical Association. 2016. doi:10.1001/jama.2016.1464
29. Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2016. doi:10.1136/annrheumdis-2016-209724
30. Olesen J Headache Classification Committee of the International Headache Society (IHS) the International Classification of Headache Disorders,
31. Treede RD, Rolf W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP Classification of chronic pain for the international Classification of diseases (ICD-11). Pain. 2019. doi:10.1097/j.pain.0000000000001384
32. Mittal VA, Walker EF Diagnostic and statistical manual of mental disorders. Psychiatry Res. 2011. doi:10.1016/j.psychres.2011.06.006
33. Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9(10):883–891. doi:10.1016/j.jpain.2008.05.005
34. Apkarian AV, Bushnell MC, Treede R, Zubieta J. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9(4):463–484. doi:10.1016/j.ejpain.2004.11.001
35. Ji RR, Xu ZZ, Gao YJ. Emerging targets in neuroinflammation-driven chronic pain. Nat Rev Drug Discov. 2014;13(7):533–548. doi:10.1038/nrd4334
36. Bonvini RF, Roffi M, Righini M. New techniques for the endovascular treatment of peripheral arterial disease. J Mal Vascul. 2014;66(1):80–101. doi:10.1016/j.jmv.2010.10.004
37. Hong H, Kim BS, Im HL. Pathophysiological role of neuroinflammation in neurodegenerative diseases and psychiatric disorders. Int Neurourol J. 2016;20(Suppl 1):S2–S7. doi:10.5213/inj.1632604.302
38. Diatchenko L, Nackley AG, Tchivileva IE, Shabalina SA, Maixner W. Genetic architecture of human pain perception. Trends Genet. 2007;23(12):605–613. doi:10.1016/j.tig.2007.09.004
39. Paller CJ, Campbell CM, Edwards RR, Dobs AS. Sex-based differences in pain perception and treatment. Pain Med. 2009;10(2):289–299. doi:10.1111/j.1526-4637.2008.00558.x
40. Kroenke K, Wu J, Bair MJ, et al. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–973. doi:10.1016/j.jpain.2011.03.003
41. Mogil JS. Sex differences in pain and pain inhibition: multiple explanations of a controversial phenomenon. Nat Rev Neurosci. 2012;13(12):859–866. doi:10.1038/nrn3360
42. Iverson KM, Hendricks AM, Kimerling R, et al. Psychiatric diagnoses and neurobehavioral symptom severity among OEF/OIF VA patients with deployment-related traumatic brain injury: a gender comparison. Womens Health Issues. 2011;21(4 Suppl):S210–S217. doi:10.1016/j.whi.2011.04.019
43. Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140(3):774–815. doi:10.1037/a0035302
44. Slavich GM, Sacher J. Stress, Sex hormones, inflammation, and major depressive disorder: extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology. 2019;236(10):3063–3079. doi:10.1007/s00213-019-05326-9
45. Antonio Mingorance J, Montoya P, Vivas Miranda JG, Riquelme I. Differences in postural balance, pain sensitivity and depression between individuals with acute and chronic back pain. J Clin Med. 2022;11(10). doi:10.3390/jcm11102700
46. Guo YF, Wang Y, Sun Y, Wang JY. A brain signature to differentiate acute and chronic pain in rats. Front Comput Neurosc. 2016;10. doi:10.3389/fncom.2016.00041
47. Manning K, Kauffman BY, Rogers AH, Garey L, Zvolensky MJ. Fatigue severity and fatigue sensitivity: relations to anxiety, depression, pain catastrophizing, and pain severity among adults with severe fatigue and chronic low back pain. Behav Med. 2022;48(3):181–189. doi:10.1080/08964289.2020.1796572
48. Hsu YC, Ma KH, Guo SL, et al. The occurrence of pain-Induced depression is different between rat models of inflammatory and neuropathic pain. J Clin Med. 2021;10(17):4016. doi:10.3390/jcm10174016
49. Aburuz ME, Masa’deh R. Gender differences in anxiety and complications early after acute myocardial infarction. J Cardiovasc Nurs. 2017;32(6):538–543. doi:10.1097/JCN.0000000000000375
50. McKinley S, Fien M, Riegel B, et al. Complications after acute coronary syndrome are reduced by perceived control of cardiac illness. J Adv Nurs. 2012;68(10):2320–2330. doi:10.1111/j.1365-2648.2011.05933.x
51. Kim J, Cho SJ, Kim WJ, et al. Insomnia in tension-type headache: a population-based study. J Headache Pain. 2017;18(1):18. doi:10.1186/s10194-017-0805-3
52. Ficek SK, Wittrock DA. Subjective stress and coping in recurrent tension-type headache. Headache. 1995;35(8):455–460. doi:10.1111/j.1526-4610.1995.hed3508455.x
53. Brandt M, Cardinale J, Aulsebrook ML, Gasser G, Mindt TL. An overview of PET radiochemistry, part 2: radiometals. J Nucl Med. 2018;59(10):1500–1506. doi:10.2967/jnumed.117.190801
54. Hopton A, Macpherson H, Keding A, Morley S. Acupuncture, counselling or usual care for depression and comorbid pain: secondary analysis of a randomised controlled trial. BMJ Open. 2014;4(5):e004964. doi:10.1136/bmjopen-2014-004964
55. You JY, Li H, Xie D, Chen R, Chen M, Fernández-de-las-Peñas C. Acupuncture for chronic pain-related depression: a systematic review and meta-analysis. Pain Res Manag. 2021;2021:6617075. doi:10.1155/2021/6617075
56. Feingold D, Brill S, Goor-Aryeh I, Delayahu Y, Lev-Ran S. Depression and anxiety among chronic pain patients receiving prescription opioids and medical marijuana. J Affect Disord. 2017;218:1–7. doi:10.1016/j.jad.2017.04.026
57. Scherrer JF, Salas J, Schneider FD, et al. Characteristics of new depression diagnoses in patients with and without prior chronic opioid use. J Affect Disord. 2017;210:125–129. doi:10.1016/j.jad.2016.12.027
58. Wilson N, Kariisa M, Seth P, Smith H, Davis NL. Drug and opioid-Involved overdose deaths - United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290–297. doi:10.15585/mmwr.mm6911a4
59. Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624–1645. doi:10.15585/mmwr.rr6501e1
60. Sumitani M, Nishizawa D, Hozumi J, Ikeda K. Genetic implications in quality palliative care and preventing opioid crisis in cancer-related pain management. J Neurosci Res. 2022;100(1):362–372. doi:10.1002/jnr.24756
61. Tang DL, Comish P, Kang R, Hobman TC. The hallmarks of COVID-19 disease. PLoS Pathog. 2020;16(5):e1008536. doi:10.1371/journal.ppat.1008536
62. Aloush V, Gurfinkel A, Shachar N, Ablin JN, Elkana O. Physical and mental impact of COVID-19 outbreak on fibromyalgia patients. Clin Exper Rheumatol. 2021;39(3):S108–S114. doi:10.55563/clinexprheumatol/rxk6s4
63. Bilen A, Kucukkepeci H. Pain Intensity, depression, and anxiety levels among patients with chronic pain during COVID-19 pandemic. J Nerv Ment Dis. 2022;210(4):270–275. doi:10.1097/NMD.0000000000001466
64. Rau LM, Grothus S, Sommer A, et al. Chronic pain in schoolchildren and its association with psychological wellbeing before and during the COVID-19 pandemic. J Adolesc Health. 2021;69(5):721–728. doi:10.1016/j.jadohealth.2021.07.027
65. Sahin T, Ayyildiz A, Gencer-Atalay K, et al. Pain symptoms in COVID-19. Am J Physical Med Rehabilit. 2021;100(4):307–312. doi:10.1097/PHM.0000000000001699
66. Mutiawati E, Kusuma HL, Fahriani M, et al. Headache in post-COVID-19 patients: its characteristics and relationship with the quality of Life. Medicina Lithuania. 2022;58(10). doi:10.3390/medicina58101500
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
