Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Streamlining the Multi-Disciplinary Team Meeting: The Introduction of Robust Pre-Preparation Methods and Its Effect on the Length of Case Discussions
Authors Merker L , Conroy S , El-Wakeel H, Laurence N
Received 22 August 2022
Accepted for publication 15 December 2022
Published 4 March 2023 Volume 2023:16 Pages 613—622
DOI https://doi.org/10.2147/JMDH.S387174
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Louise Merker,* Soraya Conroy,* Hassan El-Wakeel, Nicola Laurence
Department of Breast Surgery, Royal United Hospital, Bath, UK
*These authors contributed equally to this work
Correspondence: Louise Merker; Soraya Conroy, Email [email protected]; [email protected]
Introduction: The multidisciplinary team (MDT) approach has long been considered the optimal way in which to deliver a high standard of care to patients with breast cancer. With a growing number of patients and ever-increasing complexity of cases, the strain on time and resource of the MDT is becoming increasingly evident. It is therefore essential that local hospital departments adapt their MDT processes to better streamline discussions and optimise efficiency. The Royal United Hospital in Bath is a district general hospital in the UK. Approximately 500 patients with cancers are treated annually, and the MDT discusses approximately 60 patients per week.
Methods: To improve our MDT meeting processes and increase productivity, we created a concise MDT template using Microsoft Access™: giving all clinicians the ability to add patients and information in real time. We also allocated weekly preparation time whereby a senior clinician ensured all patients were prepared prior to the meeting with results and potential outcomes prepopulated where possible.
Results: We recorded the time spent discussing patients during 6 MDT meetings before and after implementation of changes. Cases were classified by pathology category to determine if there were differences following the preparation changes. Overall, we significantly reduced our average MDT discussion time (p=0.02). We significantly reduced average discussion time in postoperative malignant cases (p< 0.0006) and expected benign core biopsy cases (p< 0.0047), allowing appropriate redistribution of time towards discussion of more complex cases, reflected by the significant increase in time spent discussing complex radiology cases (p< 0.025).
Conclusion: We offer an effective method for improving the MDT meeting preparation and presentation by ensuring each patient is appropriately prepared prior to the meeting, and outcomes for those simple cases are already prepopulated. This creates additional time within the meeting to discuss more complex clinical cases while allowing all members of the team an opportunity to discuss all patients if needed.
Keywords: breast cancer, multidisciplinary team, MDT, service evaluation, streamlining
Introduction
The multidisciplinary team (MDT) approach has long been considered the gold standard for the management of patients with cancer.1 MDT meeting (MDTM) facilitates cohesive working by multiple disciplines to ensure that optimal treatment decision is made for each patient and that care pathways are personalised while adhering to national guidance, thus ultimately improving outcomes.2,3 In addition to the obvious benefits on patient care, MDTM also has a number of secondary benefits including an educational and learning component, team communication and development, enhanced recruitment into clinical trials, audit and service evaluation.3
Since the commencement of the NHS Breast Screening Programme at the end of the 1980’s, the review of all breast cancer patients during an MDTM has evolved to become the established standard of care. UK cancer policy continues to highlight the importance of MDT in delivery of care.1 However, like many aspects of the health service; the MDT is under increasing volume pressures. Breast cancer is the most commonly diagnosed cancer in the UK, with 55,200 new cases every year.4 With a growing number of patients, an older population with greater co-morbidities and development of new and innovative treatments, it is vital that the MDT adapts and evolves to meet these increasing demands: to ensure the ongoing delivery of high standard care, in the most efficient way.1,2
MDTs are clearly essential in providing high-quality cancer care and are a globally adopted approach to managing breast cancer.5 Despite this, cancer still remains a leading cause of death in the UK and effectiveness between MDTs can vary nationally.6 In 2015, the Independent Cancer Taskforce published recommendations to improve cancer care. They recommended that MDTM be as streamlined as possible, with processes in place to facilitate quicker decision-making for patients on standardised treatment pathways to allow time for focused discussions on more clinically challenging cases.1 This idea is echoed within the Hayes-Wheelwright matrix, which is a model applied across a range of industry whereby high volume simple product manufacture should be quick and automated to allow time for the manufacture of highly customised low volume products.7 Soukup et al developed a tool to assess the clinical complexity of cancer patients in order to differentiate between simple and complex cases. They propose, that by using such a tool, cases selected for MDT could be based on complexity, allowing for less complex cases to be managed using evidence-based predetermined protocols.8 A report from Cancer Research UK also highlighted the need to apply protocol-driven treatment pathways to patients who meet criteria: in order to minimise discussion had on these patients during MDTM, to allow for more effective and lengthy discussion on complex cases.2
In 2017, a national survey was conducted of 1220 UK-based MDT members asking for recommendations on how to improve the efficacy of the MDT. The results supported the concept of streamlining discussions to prioritise complex cases, which would benefit from more time.9 Most recently, NHS England and NHS Improvement published further guidance on how MDTMs can become more streamlined in their approach whilst maintaining high-quality standardised treatment pathways: allowing longer discussions of cases where needed to ensure optimum use of clinical time.10
Through collaborative work from the relevant associations who represent the clinical groups in attendance at the breast MDTM, a Breast MDTM Toolkit has been developed.3 This toolkit provides a useful framework from which individual breast cancer care providers can increase efficiency of their MDTMs and maximise their streamlining potential. The toolkit suggests the following principles:3
- Only patients requiring true multidisciplinary input are to be discussed.
- Patients on predetermined agreed algorithms will be recorded and not discussed.
- The time spent in the MDTMs should be reduced for all members of the MDT, in particular radiologists and pathologists.
Within the breast cancer department at Bart’s Health NHS Trust in London, a pre-MDTM triage meeting was trialled. A small number of clinicians meet and decide which patients are listed for formal discussion and who are potentially suitable for management by protocolisation using pre- agreed standards of care. In addition, patients would be removed if a plan could be made by the smaller group. This meeting also highlighted patients that should not be listed but delayed, as all information would not be available at the time of the meeting. Through their streamlining changes, on completion of this pilot, Barts Health reduced their breast MDT list size by 35%.10
Other organisations have also implemented changes to optimise the functions of the multidisciplinary team. A London-based hospital introduced a number of interventions designed to improve the “multidisciplinary tumour boards” (ie the multidisciplinary team) ability to reach treatment decisions for patients with urological cancers.11 Following their interventions, they reported a significant reduction in time spent discussing each patient as well as an overall meeting duration (p<0.001), suggesting increased efficiency of these meetings.
Much work has been done to look at what makes a successful MDT. Soukup et al describe the following five domains:12
- Background to multidisciplinary teams in cancer care.
- Key performance indicators of effective teams and their meetings.
- Factors that are known to affect team processes.
- Assessment of cancer MDT working.
- Improvement of cancer MDT working and its impact on patient care.
When attempting to make changes to the MDT, it can be helpful to use a systems approach, which describes and evaluates the functioning of an MDTM. Lamb et al divide the elements of the MDT into input, process and output.13 Each of these is suggested to have a technical and non-technical aspect.
We discuss our outcomes after implementing MDTM streamlining strategies in our breast department: by assessing the impact on overall MDTM length, as well as time spent on individual case discussions. When considering Lamb et al13 approach to evaluating and streamlining MDTM, the areas that we were primarily interested in were:
- technical input: Information
- technical process: expert review of information
- technical outcome: documentation of the decision.
We also considered secondary improvements in the non-technical processes of teamwork and open discussion.
Method
The key members of the breast MDTM in our hospital include 5 consultant breast surgeons, 4 oncology doctors, 1 consultant radiotherapist, 2 radiologists, 1 pathologist, 1–2 breast care nurses, 1 radiographer and an MDT co-ordinator. All biopsy results are discussed, as are all cross-sectional imaging and postoperative histology. In addition, patients are added by all members of the team who require multidisciplinary decision-making to further their ongoing management. Each meeting is scheduled for two hours and there is no limit on patient numbers. On average 60 patients are discussed each week. If a definitive treatment plan has not been reached for a patient, for example if they require further imaging such as a breast MRI, the patient would be rediscussed at the next MDTM once the additional imaging has been completed.
Previously, our MDT list was a written paper document with three categories: pre-operative, post-operative and radiology and all patients were discussed by the whole team. It was often noted that several patients had incomplete information available at the time of the MDT, which was necessary to make a management decision. There were incidences where it was not clear why a patient had been added to the MDTM or by whom and if relevant follow-up or investigations had been arranged. Time was often spent during the meeting, looking up relevant results (eg ECHO reports and blood tests) or past treatments and past medical history: this was especially so in more complex cases.
To streamline our MDTM, we employed a number of methods. First, we implemented a new system to enter patient information. A specific “Access template” was created in Microsoft Access™. The new template allows real-time access for all members of the MDT to add their patients for discussion, along with relevant information and possible clinical questions requiring an answer. This is available from their hospital desktop PC. A dropdown box within Access™ allows detailed categorisation of patients, so in the final prepared list the patients are listed in specific categories. These specific categories are as follows: postoperative malignant, HER2 results, complex radiology discussion, surgical/oncology discussion, metastatic patients, expected malignant core biopsy results, breast MRI results, MDT approval required (eg risk reduction surgery), patients for registration only, expected benign core biopsy results, post-operative benign, and other. These more detailed and specific categories were agreed upon by the department and ensured focused and engaged discussion of the more complex cases at the start of the meeting. It also allowed oncologists to leave prior to the end of the meeting to attend their other clinical duties, when cases not requiring their input, such as post-operative benign, were being discussed.
Our second significant change was to include a 5 h/week protected time within the job plan of a senior breast surgeon – to allow pre-meeting preparation of all cases. This would include straightforward cases as well as complex cases. All relevant information relating to the MDT discussion is taken from the electronic notes, radiology, and histological results. These are all available from the IT system used at our hospital with easy, quick access. The relevant information is summarised and added to the Access template. This summarisation shows all relevant information to enable the team to agree on an appropriate outcome. The summary and use of abbreviations are universally known to the team and therefore allow faster decision-making. The preparing clinician adds in a proposed outcome for each entry. The finalised prepared MDT list with all information and proposed outcomes is then exported and emailed to all MDT members, including the MDT co-ordinator, the early afternoon before the meeting (Figure 1). This allows for all team members to review the summarised information prior to the meeting; to note any concerns and to give thought to research any potential discussion areas. It also allows the MDT co-ordinator to prepopulate the MDT outcomes on the cancer registry (Somerset Cancer Registry) which can still be altered during the meeting. Preparation time is also available for radiology and pathology team members to undertake the same pre-meeting information gathering process.
Data were collected from six MDTMs in October and November 2018 prior to MDTM streamlining changes and from six MDTMs during October 2019 to January 2020 after the changes were implemented. The time spent discussing each patient was recorded in seconds by a member of the MDT before and after streamline changes had been made. Recording of discussion commenced when the patient's name was read, until end of all discussions regarding that patient.
Statistical analysis: The data was recorded in an Excel™ spread sheet and grouped based on categories from the AccessTM template. Five categories that were discussed and therefore analysed included; complex radiology discussion, postoperative malignant pathway, expected benign core biopsy, expected malignant core biopsy and other. This was then analysed using GraphPad Prism 9.0.0™, and statistical significance was assessed through a Mann–Whitney test.
After using the new MDTM format for several months a qualitative survey was undertaken using Survey Monkey™. Eight questions were sent to all MDTM members in an anonymised link except for identification of role within the MDT. Sixteen responses were received in total. The questions focused on whether members liked the new format, found the information readable and accurate and found it to improve patient discussions. Free comment boxes were available for each question to allow members to highlight any specific concerns or comments for further improvement.
For this study, we have followed UK National Health Research Authority guidance, confirmed by completing the decision tools and we have also sought guidance from our local institutions Research & Development Department. Guidance from these groups confirm that this is not research requiring ethical review or consent to be taken. We have also followed our local GDPR guidelines to ensure data protection principles are met and only people involved in direct clinical care of patients had access to identifiable data as part of the study.
Results
A total of 227 patients were discussed in the 6 MDTM pre-streamlining changes. Of these, 49 were postoperative malignant pathway discussions, 38 were complex radiological discussions, 123 were discussion of results from core biopsies (63 benign and 60 malignant), and 17 were other discussions such as pathology results following symmetrising surgery or patients who were on neoadjuvant, endocrine, or chemo-therapy. Following streamlining changes a total of 248 patients were discussed. Fifty-three were discussions regarding postoperative malignant pathway, 47 were complex radiological discussions, 106 were discussion of results from core biopsies (54 benign and 52 malignant, respectively), and 42 were other (Table 1).
 |
Table 1 All Results |
Length of discussion for each patient varied from a minimum of 4 s up to a maximum of 767 s. Except for complex radiology discussions, the mean time spent in seconds (s) discussing each patient category reduced following the introduction of the template (Table 1). The reduction in discussion time of postoperative malignant pathway and expected benign core biopsy was statistically significant with p=0.0006 and p=0.0047, respectively (Figures 2 and 3). The greatest time saving occurred in the postoperative malignant pathway category, where we found a 27s reduction in discussion time.
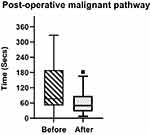 |
Figure 2 Box plot of post-operative malignant pathway discussion time in seconds, before and after change (p=0.0006, Mann–Whitney U-Test). |
 |
Figure 3 Box plot of expected benign core biopsy discussion time in seconds, before and after change (p=0.0047, Mann–Whitney U-Test). |
Complex radiology discussions significantly increased in time (p=0.025) (Figure 4). This increase was negated by the reduction in time spent on discussion of other cases: resulting in a significant reduction in overall MDTM length (p=0.02).
 |
Figure 4 Box plot of complex radiology discussion time in seconds, before and after change (p=0.025, Mann–Whitney U-Test). |
Following the introduction of the streamlining template, we asked our MDTM members to provide feedback on the new format of the meetings. We had a total of 16 responses with every discipline of the MDT represented. Overall, 80% of members felt the new template was beneficial in improving patient case presentation and preferred the streamlined MDTM, with 75% feeling they had more confidence in the outcomes offered by the MDT. The majority of members did not feel comfortable with the removal of simple cases from the MDTM and wished to continue discussing all patients. The results of the survey were circulated to all members of the MDT including free-text comments alongside how we have taken feedback on board to further improve the quality of our meetings.
Discussion
The provision of safe breast cancer treatment has been delivered using a multidisciplinary team meeting for over 20 years. Traditionally, all cases are discussed at the MDT. Certainly, in our MDTM all cases, including simple cases, remain listed in their entirety: allowing any MDT member to query or note possible errors in the provisional plan. However, should this continue to be mandatory? Could we remove a collection of patients who are straightforward and fulfil a set of criteria to allow their exclusion from the main meeting? This raises the possibility that we may be able to generate local standards of care (SoC’s), thus allowing safe removal of patients, predicted to follow well-established plans, from the MDTM.10 The notion that non-complex patients may be treated according to predetermined protocols and thus removed from the main MDT discussion has been proposed in previous studies.8 Removal of such cases, however, would exclude these patients from potential nuanced discussion and it would become challenging to say, with total certainty, that optimum management was undertaken. Within our breast MDTMs, there are incidences where a patient outcome should have been “straightforward” but additional contributions by a radiologist, pathologist, or breast care nurse has led to a change in the management. As such, there was a concern regarding removal of patients to a separate pre-MDT.
As an MDT, we would argue that with good preparation and presentation of straightforward cases, the time for these patients to be presented is minimal. The Association of Breast Surgery (ABS) is our UK national professional body for clinicians involved in providing breast cancer management. The MDTM Toolkit produced by the ABS in collaboration with radiologists, pathologists, and oncologists suggests a pre-MDT meeting or a triaging meeting.3 Prep with one clinician could be thought as comparable to a pre-MDT meeting but with a full MDT stamp. It allows any member of the MDT time to question each case if there is an anomaly. As such, there is no concern about excluding a case thought to be straightforward in error, and no need for a separate meeting.
The main aim of our template is to have all information readily available and a provisional treatment pathway suggested. It is therefore expected that categories, which are managed by well-established guidelines, such as postoperative malignancy and benign core biopsy, would show the greatest reduction in time. The significant increase in discussion time for complex radiology since the introduction of the template is not necessarily a failing but instead reflects a shift of focus towards more complex decision-making.
The aim of the pre-MDT suggested by the ABS was to reduce the actual MDT workload by excluding any duplicate listing, checking clinical information accuracy, and assessing whether the patients required full team discussion. The 5 h of pre-meeting preparation time we suggest is comparable. We are a paper light service with clinic letters, radiology, and histology results all available electronically. The list is pre-populated with all the relevant clinical information available, and any inappropriate, duplicate, or incomplete referrals screened out – saving time in the MDTM.
The completed list is made available to all team members prior to the meetings, thus allowing further scrutiny. There was concern that if provisional plans were proposed, the team would lose concentration, thus missing potential errors. Contrary to this, we found members more engaged with the MDT and more alert to note errors, which can occur when relying on one person's preparation. Lead preparing clinicians are also rotated to prevent clinician fatigue and to remove any element of bias that may be present with one individual preparing all the meetings.
MDT meetings risk becoming process focussed due to time pressures and the need to comply with national standards in information recording. This may lead to an apathetic MDT with reduced interaction and debate between different attending disciplines. Increasing workload coupled with minimal extra MDTM time may leave little opportunity for meaningful discussions. De Iesa et al found that only 12.4% of treatment decisions provisionally made by clinicians were altered by discussion at the MDTM.14 This is likely due to the many evidence-based, standardised treatment protocols that exist within breast surgery and is not necessarily a negative finding. However, this low rate of alteration in treatment decision may represent clinician fatigue and a lack of engagement with case discussions.15 By reordering our meeting, to first discuss complex cases where a standardised protocol may not exist, we believe clinicians will be protected from meeting fatigue and be ready to engage with discussions of these more challenging cases.
The preparation of the MDTM also offers significant training benefits to trainees working in the unit. If simple cases are excluded, the training experience may be lost. Under supervision from the lead consultant, a trainee can prepare the MDTM: reviewing the patient results and providing a proposed treatment plan based on their understanding. This allows trainee time to consolidate treatment pathways and earmark gaps in their knowledge. Undertaking this as a training activity will help prepare trainees effectively for progression to consultancy, which is in keeping with the generic professional capabilities’ framework outlined in the new surgical curriculum planned for August 2021.16,17
In addition to the training benefits of preparing MDTM, ensuring all patients remain on the discussion list increases the number of potential patients that may be considered for enrolment in clinical trials. By having the relevant clinical information prepared beforehand, trial consideration is a realistic option for all patients. This can be highlighted at MDTM and as the team becomes familiar with the available trials, more patients will be successfully recruited.
Each discipline need not be present for every case. Grouping patients into categories enhances efficiency and allows for flexibility during MDTM. Categorising patients allows the meetings “order of discussion” to be rearranged to fit with the clinical needs of the unit. In our unit, oncology time is pressured. We have therefore chosen to start with cases more likely to require oncology input. Formatting our meetings in this way ensures oncology’s vital attendance at the MDTM whilst allowing their staff to then join a late start morning clinic.
We have shown that through our streamlining methods it is possible not only to reduce the overall length of the MDTM but to redirect the focus of the meeting towards more complex cases to encourage valuable discussion here. As the meeting is pre-prepared, we believe it is safe to give minimal airtime to those patients who have pre-agreed management plans as these are based on established guidelines – with little further to be added by the MDT.
Finally, an additional aim in streamlining MDTMs is to reduce cost. MDTM is a very expensive meeting given the number of senior clinicians present. Our streamlining strategies have been shown to reduce the meeting time, and we anticipate that as these changes become embedded within our department, we will likely become even more efficient. With the pre-preparation of the MDT and opportunity to review cases prior to the main meeting, clinicians can verify the information of their patients scheduled for discussion at the MDT. This ensures, that even in the absence of the patient’s named clinician, patients are accurately represented and appropriate MDT decisions are made. This may increase availability of clinicians to engage in other clinical activities.
Since this data was collected, we have further adapted our Breast MDTM in response to the COVID −19 pandemic: primarily through the use of remote meeting tools. We elected not to include this data in our analysis due to the many variables including different case mix, changes in demand on the service, and computer issues and felt it would not provide a fair comparison. However, due to our streamlining interventions with effective pre-meeting preparation and use of the online Access Template, we have found that the transition to a more virtual MDTM has been relatively seamless.
One of the main limitations of our study is that it was undertaken in a single centre. The methods used in our unit will not be suitable for all units, particularly those of higher patient volumes. However, our aim was to showcase our recognition of the need to evaluate and improve our MDTM in light of increasing workload, which is a national problem. Future work should focus on assessing quality of MDTM decisions to ensure decision-making meets the gold standard in every case so that we can guarantee the best possible outcomes for our patients.
Conclusion
MDT meeting plays a vital role in providing safe, up-to-date management of breast cancer patients in the UK. However, in its traditional format, the quality of these meetings has come into question. Increased time pressures have forced the meetings to become more process driven in an effort to achieve the workload required. Discussion and debate has been greatly stifled: defeating the purpose of bringing together a variety of medical professionals in a forum for deliberation. Through a simple template and increased pre-meeting preparation, we have devised an effective method for increasing the clinician debate on more complex cases. In addition to likely improved patient outcome, it also brings back the educational element to the MDTM, which is of benefit to all members. Eventually, it may be possible to remove certain cases who fulfil agreed standards of care (SoC) criteria from discussion and allow these to be managed through well-evidenced treatment protocols. This would further reduce the workload on the MDTM and release more time for debate. This may be of particular benefit in larger volume units.
Through the combined use of our breast MDTM template, along with protected pre-MDT preparation time, we offer an effective method to streamline the MDT meeting whilst enhancing participant engagement and focusing the team. This has increased the time available for discussion of complex breast cancer cases, without increasing the overall duration of the MDT meeting. With growing numbers of breast cancer patients surviving longer, 76% survive 10 years or more,18 there will undoubtedly be an increase in complexity in MDT cases given a number of these patients will go on to develop recurrences or second breast cancers. This is in addition to the increased number of treatments for patients with metastatic disease. It is therefore essential that the time available for discussion of these complex discussions is protected: to ensure we continue to deliver the best care we can for our patients.
Disclosure
Louise Merker and Soraya Conroy are co-first authors for this study. Mr Hassan El-Wakeel is a Director of Collaboration Digital Ltd, a software company. The authors report no other conflicts of interest in this work.
References
1. Independent Cancer Taskforce. Achieving world-class cancer outcomes. A strategy for England 2015–2020. Available from: https://www.cancerresearchuk.org/sites/default/files/achieving_world-class_cancer_outcomes_-_a_strategy_for_england_2015-2020.pdf.
2. Cancer Research UK. Meeting patients’ needs: improving the effectiveness of multidisciplinary team meetings in cancer services. Available from: https://www.cancerresearchuk.org/sites/default/files/full_report_meeting_patients_needs_improving_the_effectiveness_of_multidisciplinary_team_meetings_.pdf.
3. Improving the Efficiency of Breast Multidisciplinary Team Meetings. A toolkit for breast services; 2020. Available from: https://associationofbreastsurgery.org.uk/media/251959/breast-mdtm-toolkit-v-3.pdf.
4. Cancer Research UK. Breast cancer statistics 2015–2017; 2021. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer.
5. Saini KS, Taylor C, Ramirez AJ, et al. Role of the multidisciplinary team in breast cancer management: results from a large international survey involving 39 countries. Ann Oncol. 2012;23(4):853–859. doi:10.1093/annonc/mdr352
6. Department of Health and Social Care. An overview of the findings from the 2010–2011 National Cancer Peer Review of cancer services in England. Available from: https://www.gov.uk/government/publications/national-cancer-peer-review-programme-report-2010-11.
7. Hayes HR, Wheelwright CS. Link manufacturing process and product life cycles. Available from: https://hbr.org/1979/01/link-manufacturing-process-and-product-life-cycles.
8. Soukup T, Morbi A, Lamb BW, et al. A measure of case complexity for streamlining workflow in multidisciplinary tumor boards: mixed methods development and early validation of the MeDiC tool. Cancer Med. 2020;9(14):5143–5154. doi:10.1002/cam4.3026
9. Hoinville L, Taylor C, Zasada M, Warner R, Pottle E, Green J. Improving the effectiveness of cancer multidisciplinary team meetings: analysis of a national survey of MDT members’ opinions about streamlining patient discussions. BMJ Open Qual. 2019;8(2):e000631. doi:10.1136/bmjoq-2019-000631
10. NHS England and NHS Improvement. Streamlining multi-disciplinary team meetings: guidance for cancer alliance; 2020. Available from: https://www.england.nhs.uk/wp-content/uploads/2020/01/multi-disciplinary-team-streamlining-guidance.pdf.
11. Lamb BW, Green JSA, Benn J, Brown KF, Vincent CA, Sevdalis N. Improving decision making in multidisciplinary tumor boards: prospective longitudinal evaluation of a multicomponent intervention for 1421 patients. J Am Coll Surg. 2013;217(3):412–420. doi:10.1016/j.jamcollsurg.2013.04.035
12. Soukup T, Lamb BW, Arora S, Darzi A, Sevdalis N, Green JS. Successful strategies in implementing a multidisciplinary team working in the care of patients with cancer: an overview and synthesis of the available literature. J Multidiscip Healthc. 2018;11:49–61. doi:10.2147/JMDH.S117945
13. Lamb B, Green JSA, Vincent C, Sevdalis N. Decision making in surgical oncology. Surg Oncol. 2011;20(3):163–168. doi:10.1016/j.suronc.2010.07.007
14. de Ieso PB, Coward JI, Letsa I, et al. A study of the decision outcomes and financial costs of multidisciplinary team meetings (MDMs) in oncology. Br J Cancer. 2013;109(9):2295–2300. doi:10.1038/bjc.2013.586
15. Soukup T, Gandamihardja TAK, McInerney S, Green JSA, Sevdalis N. Do multidisciplinary cancer care teams suffer decision-making fatigue: an observational, longitudinal team improvement study. BMJ Open. 2019;9(5):e027303. doi:10.1136/bmjopen-2018-027303
16. General Medical Council. Generic professional capabilities framework. GMC; 2017. Available from: https://www.gmc-uk.org/-/media/documents/generic-professional-capabilities-framework--0817_pdf-70417127.pdf.
17. Intercollegiate Surgical Curriculum Programme. The new surgical curriculum for August. 2021.
18. Cancer Research UK. Breast cancer survival statistics; 2020. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer/survival#heading-Zero.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

