Back to Journals » Cancer Management and Research » Volume 12
Standard Treatment Remains the Recommended Approach for Patients with Bone Sarcoma Who Underwent Unplanned Surgery: Report from the Japanese Musculoskeletal Oncology Group
Authors Nakamura T , Sugaya J , Naka N, Kobayashi H, Okuma T, Kunisada T , Asanuma K , Outani H, Nishimura S, Kawashima H, Akiyama T, Yasuda T, Miwa S, Sudo A , Ueda T
Received 30 June 2020
Accepted for publication 5 August 2020
Published 12 October 2020 Volume 2020:12 Pages 10017—10022
DOI https://doi.org/10.2147/CMAR.S270178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eileen O'Reilly
Tomoki Nakamura,1 Jun Sugaya,2 Norifumi Naka,3 Hiroshi Kobayashi,4 Tomotake Okuma,5 Toshiyuki Kunisada,6 Kunihiro Asanuma,1 Hedetatsu Outani,7 Shunji Nishimura,8 Hiroyuki Kawashima,9 Toru Akiyama,10 Taketoshi Yasuda,11 Shinji Miwa,12 Akihiro Sudo,1 Takafumi Ueda13
1Department of Orthopaedic Surgery, Mie University Graduate School of Medicine, Tsu 514-8507, Japan; 2Department of Musculoskeletal Oncology, National Cancer Center Hospital, Chuo-ku, Tokyo 104-0045, Japan; 3Musculoskeletal Oncology Service, Osaka International Cancer Institute, Chuo-ku, Osaka 541-8567, Japan; 4Department of Orthopaedic Surgery, The University of Tokyo Hospital, Bunkyo-ku, Tokyo 113-8655, Japan; 5Department of Musculoskeletal Oncology, Tokyo Metropolitan Cancer and Infectious Diseases Center, Komagome Hospital, Bunkyo-ku, Tokyo 113-8677, Japan; 6Department of Orthopaedic Surgery, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama 700-8558, Japan; 7Department of Orthopaedic Surgery, Osaka University Graduate School of Medicine, Suita, Osaka 565-0871, Japan; 8Department of Orthopaedic Surgery, Kindai University Hospital, Osaka-Sayama, Osaka 589-8511, Japan; 9Division of Orthopaedic Surgery, Niigata University Graduate School of Medical and Dental Sciences, Chuo-ku, Niigata 951-8510, Japan; 10Department of Orthopaedic Surgery, Saitama Medical Center, Jichi Medical University, Saitama, Saitama 330-8503, Japan; 11Department of Orthopaedic Surgery, University of Toyama, Toyama 930-0194, Japan; 12Department of Orthopaedic Surgery, Kanazawa University Graduate School of Medical Sciences, Kanazawa 920-8641, Japan; 13Department of Orthopaedic Surgery, Osaka National Hospital, Chuo-ku, Osaka 540-0006, Japan
Correspondence: Tomoki Nakamura
Department of Orthopedic Surgery, Mie University Graduate School of Medicine, 2-174 Edobashi, Tsu, Mie 514-8507, Japan
Tel +81-592315022
Fax +81-592315211
Email [email protected]
Background: The outcomes of unplanned surgery for bone sarcomas have not been frequently discussed. However, it is important to recognize patterns, treatment, and clinical outcomes of unplanned surgeries for patients with bone sarcomas. This multicenter study aimed to characterize the clinical outcomes of patients with bone sarcomas who underwent unplanned surgeries.
Patients and Methods: Data of 43 patients with bone sarcomas who underwent unplanned surgery between 2006 and 2017 were obtained from 23 hospitals in Japan. These included 18 cases of osteosarcoma, 9 of Ewing sarcoma, 8 of chondrosarcoma, and 6 of undifferentiated pleomorphic sarcoma. The study included 28 men and 15 women, with a mean age of 46 years. The mean follow-up duration was 59 months.
Results: The main primary tumor sites were the femur (n = 19), spine (n = 6), pelvis (n = 5), tibia (n = 3), and humerus (n = 3). The primary diagnoses were benign bone tumor (n = 24), trauma (n = 7), bone metastasis (n = 5), osteomyelitis (n = 4), degeneration (n=2), and unknown (n = 1). As unplanned surgeries, curettage, with or without bone graft, was performed in 26 patients; internal fixation was performed in 7; spinal surgery in 5; arthroplasty in 4; and arthroscopy in one. Thirty-eight patients received additional standard treatments. Thirty-four of these patients underwent surgical tumor resections, including amputation (n = 10), and the remaining 4 received radiotherapy or carbon ion radiotherapy as additional standard treatments. The 5-year disease-specific survival (DSS) rates in patients with osteosarcoma, Ewing sarcoma, and chondrosarcoma were 65.5%, 58.3%, and 72.9%, respectively. Twelve (27.9%) patients developed local recurrences (LR); among the total 43 patients studied, the 5-year DSS rates were significantly worse for those who developed LR compared to those who did not (p = 0.03). The 5-year DSS rates in patients with and without LR were 44% and 73.8%, respectively.
Conclusion: We recommend that patients who have undergone unplanned surgery be administered standard treatment, including the option of amputation because herein, LR was shown to be a risk factor for decreased DSS.
Keywords: bone sarcoma, unplanned surgery, local recurrence, osteosarcoma, Ewing sarcoma, chondrosarcoma
Introduction
Bone sarcomas are a rare type of cancer. They are sometimes discovered when a primary bone sarcoma is not suspected, such as during internal fixation of pathological fracture (s), and presumed to be a bone metastasis or benign bone condition.1,2 Less common presentations include surgery for presumed insufficiency fracture (s) or trauma, as well as joint replacement (s) for osteoarthritis.2,3 Furthermore, differentiating bone sarcomas from osteomyelitis can sometimes be very challenging.4 Although unplanned surgeries for soft tissue sarcomas (STS) are much more common and have been widely reported,5–9 the outcomes of unplanned surgeries for bone sarcomas have been discussed less often.2,10–12 One possible reason for this may be that physicians notice the abnormality when performing radiological examinations. For STS, surgical resections are likely to be performed without any radiological examination when the tumor is small and/or subcutaneous. It is important, however, to recognize patterns of unplanned surgery, treatment, and clinical outcomes in patients with bone sarcomas. Therefore, we collected data from patients with bone sarcomas who underwent unplanned surgeries at several centers. This multicenter study by the Japanese Musculoskeletal Oncology Group aimed to characterize the clinical outcomes of patients with bone sarcomas who underwent unplanned surgeries.
Patients and Methods
Data of 43 patients with bone sarcomas who underwent surgeries between 2006 and 2017 were obtained from 23 hospitals that belong to the Japanese Musculoskeletal Oncology Group. There were 28 men and 15 women, with a mean age of 46 years. High- and low-grade tumors were identified in 40 and 3 patients, respectively. Pathological fractures were detected during unplanned surgeries in 18 patients, and the mean follow-up duration was 59 months. Unplanned surgery was defined as follows: surgery performed without the consideration of bone sarcoma, the final diagnosis after unplanned surgery was bone sarcoma, and the final diagnosis was histologically confirmed. However, patients who were diagnosed with a benign or metastatic tumor based on histological examination results of needle or open biopsy were excluded from the present study, even if the final postoperative diagnosis was a bone sarcoma. The standard treatments for bone sarcomas were defined as follows: neoadjuvant and adjuvant chemotherapy and surgical resection were performed in patients with osteosarcoma (OS), Ewing sarcoma, and undifferentiated pleomorphic sarcoma of the bone (UPS); surgical resection alone was the standard treatment in elderly patients; and surgical resection was performed in patients with chondrosarcoma (CS). When radiological treatments, such as radical radiotherapy (Rx) or carbon ion radiotherapy (CIRT), were performed owing to the difficulty of surgical resection, it was included as a standard treatment. This study was conducted in accordance with the Declaration of Helsinki of 1964. We obtained approval from the Institutional Review Board (IRB) at Mie University Hospital before we started the present study, and the IRB waived the need for informed consent due to the retrospective study design. All patient data accessed complied with relevant data protection and privacy regulations.
Statistical Analysis
Statistical associations among clinicopathological factors were evaluated using the Mann–Whitney U-test and Kruskal–Wallis test for quantitative data and the chi-squared (χ2) test for qualitative data. Correlations between continuous factors were tested using the Spearman rank correlation analysis. Disease-specific survival (DSS) was defined as the duration of time between the unplanned surgery for the primary tumor and the documentation indicating the patient was still alive or the date of death owing to sarcoma. Survival curves were plotted using the Kaplan–Meier method, and the Log rank test was used to compare survival and events between the patients. Differences with a p-value <0.05 were considered statistically significant for all analyses.
Results
Truncal tumors were found in 13 patients and extremity tumors in 30 (Figure 1). Primary tumor sites included the femur (n = 19), spine (n = 6), pelvis (n = 5), tibia (n = 3), humerus (n = 3), rib (n = 2), proximal phalanx (n = 2), skull (n = 1), and metacarpal bone (n = 1). There were 18 cases of OS, 9 of Ewing sarcoma, 8 of CS, 6 of UPS, 1 of malignant giant cell tumor, and 1 of angiosarcoma of the bone. The mean age at diagnosis in those with OS, Ewing sarcoma, CS, and UPS was 48.9 (range, 21–79), 21.8 (range, 3–58), 53.5 (range, 30–87), and 66.3 (range, 53–75) years, respectively. The primary diagnoses were benign bone tumor (n = 24), trauma (n = 7), bone metastasis (n = 5), osteomyelitis (n = 4), degeneration (n = 2), and unknown (n = 1). Details regarding the diagnoses are individually summarized in Table 1. As unplanned surgeries, curettage, with or without a bone graft, was performed in 26 patients; internal fixation in 7; spine surgery in 5; arthroplasty in 4; and arthroplasty in one. Of the 43 patients, 38 received additional standard treatment. Thirty-four of those patients underwent surgical tumor resection, including 10 who underwent amputation, and the remaining 4 received Rx or CIRT as additional standard treatments (Figure 1). Of the 34 patients who underwent an additional surgery, the surgical margin was positive in 4 and negative in 30. Twenty-eight of these patients also underwent chemotherapy. Five patients could not undergo any additional standard treatments. Of these, one had OS and exhibited multiple metastases and therefore received palliative therapy. Three had OS and received neoadjuvant chemotherapy; however, they developed metastases during chemotherapy and subsequently received palliative treatment without surgery. The remaining patient had Ewing sarcoma, but information regarding the details of chemotherapy were not available even though the patient underwent additional surgical tumor resections.
 |
Table 1 The Characteristics of Individual Bone Sarcomas |
 |
Figure 1 The flow-chat of the detailed treatment of 43 patients with bone sarcoma. |
Overall, the 5-year DSS rate was 65.3%. For patients with OS, Ewing sarcoma, and CS, the 5-year DSS rates were 65.5%, 58.3%, and 72.9%, respectively. The 5-year DSS rate was significantly worse in those who did not undergo additional standard treatments compared with that in those who received standard treatments (p < 0.0001). Twelve (27.9%) patients developed local recurrence (LR); however, pathological fractures were not related to the development of LR (p = 0.45). Of the 38 patients who underwent additional standard treatments, 9 (23.7%) developed LR, and among the total 43 patients studied, the 5-year DSS rate was significantly worse in those who experienced LR compared with that in those who did not (p = 0.03) (Figure 2). The 5-year DSS rates in patients with and without LR were 44% and 73.8%, respectively. Of the 38 patients who received additional standard treatments, the 5-year DSS was also significantly worse in those with LR than in those without LR (p = 0.03) (Figure 3). The 5-year DSS rates in patients with and without LR were 53.3% and 79.2%, respectively. Of the 27 patients with bone sarcomas of the extremities who received surgical tumor resections, there was no local recurrence (LR) in patients who received amputation although there was not a significant difference between the patients who received limb salvage and amputation in terms of local control (p = 0.12).
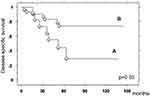 |
Figure 2 The Kaplan–Meier curve showed the disease-specific survival in 43 patients. (A; Patients with local recurrence. B; Patients without local recurrence). |
 |
Figure 3 The Kaplan–Meier curve showed the disease-specific survival in 38 patients who received standard treatment. (A; Patients with local recurrence. B; Patients without local recurrence). |
Discussion
An early diagnosis of bone sarcomas can be challenging because sarcomas can mimic familiar conditions such as sprains, overuse injuries, growing pains, benign bone lesions, and osteomyelitis. Furthermore, the incidence of bone sarcoma is quite low; moreover, it may be misdiagnosed as a more benign condition. To avoid missing the diagnosis, physicians should be aware of the early signs and symptoms, radiographic features, and risk factors such as a common age and tumor location.3,4,13 Conventional radiography in two planes should always be the first evaluation tool for investigation. When a diagnosis of malignancy cannot be excluded with certainty on radiography, the next step should be magnetic resonance imaging of the entire compartment, including the adjacent joints, since it is the best modality for local staging of extremity and pelvic tumors.14 Biopsies of suspected primary malignant bone tumors should be performed. Generally, in the case of high-grade OS, Ewing sarcoma, or UPS, primary chemotherapy is indicated following a biopsy-confirmed diagnosis.14 However, primary chemotherapy was not performed in patients with unplanned surgery. In the case of CS, surgical resection with a wide margin is the standard treatment,14 although curettage or internal fixation as a treatment of benign conditions is usually performed in the patients with unplanned surgery at initial treatment. In the present study, bone sarcomas were initially misdiagnosed as benign bone tumors, osteomyelitis, or fractures. Three of the nine patients with Ewing sarcoma were misdiagnosed with osteomyelitis, while none of the 24 patients with OS or UPS were misdiagnosed. Ewing sarcoma and osteomyelitis can have nearly identical clinical presentations, and imaging features can also exhibit similar patterns.4 Moreover, OS can mimic osteomyelitis, although there were no patients with OS who were misdiagnosed with osteomyelitis in the present study.3
Although an increased rate of LR (9/38 [23.7%]) was observed in the present multicenter study, survival rates were comparable to those for conventionally treated sarcomas.15 Ogura et al reported the clinical outcomes of bone sarcomas in Japan using data from the bone and soft tissue tumor registry.15 The survival rates in patients with OS, CS, and Ewing sarcoma were 67.2%, 86.3%, and 43.3%, respectively. This may be because appropriate treatments after the unplanned surgery were performed in a large proportion of our cohort, although amputation was necessary for 10 of the 27 (37%) patients with extremity tumors. Limb salvage after an unplanned surgery remains controversial. The ability to achieve tumor-free margins is technically difficult due to wide sources of contamination, including the skin, soft tissue, and bone. We reviewed previous studies that included >20 patients with bone sarcomas who underwent unplanned surgeries (Table 2). Some authors reported that good local control was achieved in patients with OS and CS after additional limb salvage surgery.10 However, difficulties in achieving local control with limb salvage are also reflected in the literature, with studies reporting an increase in LR rate.2,11,12 In the present study, 23.7% of the patients who underwent standard treatment developed LR, even though the LR rate after a wide bone tumor resection has been previously estimated to range from 5% to 10%.16 Therefore, we recommend that patients who have undergone unplanned surgery be administered standard neoadjuvant chemotherapy (except for those with CS), and extensive surgical treatment, including the option of amputation, if achieving a sufficiently wide margin is difficult, given that the surgical margin has been reported to be a strong prognostic factor for LR.2,12 In the present study, LR was a prognostic factor for DSS. Bacci et al also reported that LR was a highly significant risk factor for the development of metastasis and death from the tumor in patients with OS.17 Similarly, LR has been reported to be a risk factor for decreased survival in patients with Ewing sarcoma and CS.18,19
 |
Table 2 Literature Review of Unplanned Surgery for Bone Sarcomas |
There were several limitations to this study. First, there were a small number of patients studied, though the sample size was favorably comparable to those reported in previous studies. The present study was also susceptible to the inherent limitations of its retrospective design.
In conclusion, physicians should consider the possibility of bone sarcoma and perform biopsies when atypical symptoms and radiographic findings are present, even if the patient’s age is not typical for sarcoma. Although a higher rate of LR was observed in the present multicenter study, DSS rates were comparable with those for conventionally treated sarcomas. However, patients who developed LR had poor DSS. We recommend that patients who have undergone unplanned surgery be administered standard treatment, including the option of amputation, because LR was a risk factor for decreased DSS.
Acknowledgments
We would like to thank all JMOG members for supporting this study. Particularly, we deeply thank S. Tsukushi, Y. Izubuchi, H. Hiraga, T. Shirai, S. Tsukamoto, M. Hosaka, H. Hatano, H. Futani, I. Fujita, and T. Morii for collecting the data.
Funding
The authors received no financial support for this study.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Spence GM, Dunning MT, Cannon SR, Briggs TW. The hazard of retrograde nailing in pathological fractures. Three cases involving primary musculoskeletal malignancy. Injury. 2002;33(6):533–538. doi:10.1016/S0020-1383(02)00035-9
2. Gaston CL, Nakamura T, Reddy K, et al. Is limb salvage surgery safe for bone sarcomas identified after a previous surgical procedure? Bone Joint J. 2014;96-B(5):665–672. doi:10.1302/0301-620X.96B5.33140
3. Hiller C, Wegler JL, Forest CP. Osteosarcoma: accurately diagnosing this bone-chilling disease. JAPPA. 2016;29(12):29–35.
4. Henninger B, Glodny B, Rudisch A, et al. Ewing sarcoma versus osteomyelitis: differential diagnosis with magnetic resonance imaging. Skeletal Radiol. 2013;42(8):1097–1104. doi:10.1007/s00256-013-1632-5
5. Gingrich AA, Elias A, Michael Lee CY, et al. Predictors of residual disease after unplanned excision of soft tissue sarcomas. J Surg Res. 2017;208:26–32. doi:10.1016/j.jss.2016.08.096
6. Davies AM, Mehr A, Parsonage S, Evans N, Grimer RJ, Pynsent PB. MR imaging in the assessment of residual tumour following inadequate primary excision of soft tissue sarcomas. Eur Radiol. 2014;14(3):506–513. doi:10.1007/s00330-003-2023-4
7. Potter BK, Adams SC, Pitcher JD, Temple HT. Local recurrence of disease after unplanned excisions of high-grade soft tissue sarcomas. Clin Orthop Relat Res. 2008;466(12):3093–3100. doi:10.1007/s11999-008-0529-4
8. Arai E, Nishida Y, Tsukushi S, Wasa J, Ishiguro N. Clinical and treatment outcomes of planned and unplanned excisions of soft tissue sarcomas. Clin Orthop Relat Res. 2010;468(11):3028–3034. doi:10.1007/s11999-010-1392-7
9. Nakamura T, Kawai A, Sudo A. Analysis of the patients with soft tissue sarcoma who received additional resection after unplanned excision: report from the bone and soft tissue tumor registry in Japan. Jpn J Clin Oncol. 2017;47(11):1055–1059. doi:10.1093/jjco/hyx123
10. Kim MS, Lee SY, Cho WH, et al. Prognostic effect of inadvertent curettage without treatment delay in osteosarcoma. J Surg Oncol. 2009;100(6):484–487. doi:10.1002/jso.21371
11. Jeon DG, Lee SY, Kim JW. Bone primary sarcomas undergone unplanned intralesional procedures -the possibility of limb salvage and their oncologic results. J Surg Oncol. 2016;94(7):592–598. doi:10.1002/jso.20607
12. Wang B, Xu M, Zheng K, Yu X. Effect of unplanned therapy on the prognosis of patients with extremity osteosarcoma. Sci Rep. 2016;6(1):38783. doi:10.1038/srep38783
13. Douis H, Saifuddin A. The imaging of cartilaginous bone tumours. II. chondrosarcoma. Skeletal Radiol. 2013;42(5):611–626. doi:10.1007/s00256-012-1521-3
14. Casali PG, Bielack S, Abecassis N, et al. Bone sarcomas: ESMO-PaedCan-EURACAN clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl4):iv79–iv95. doi:10.1093/annonc/mdy310
15. Ogura K, Higashi T, Kawai A. Statistics of bone sarcoma in Japan: report from the bone and soft tissue tumor registry in Japan. J Orthop Sci. 2017;22(1):133–143. doi:10.1016/j.jos.2016.10.006
16. Bacci G, Ferrari S, Mercuri M, et al. Predictive factors for local recurrence in osteosarcoma: 540 patients with extremity tumors followed for minimum 2.5 years after neoadjuvant chemotherapy. Acta Orthop Scand. 1998;69(3):230–236. doi:10.3109/17453679809000921
17. Bacci G, Longhi A, Cesari M, Versari M, Bertoni F. Influence of local recurrence on survival in patients with extremity osteosaroma treated with neoadjuvant chemotherapy: the experience of a single institution with 44 patients. Cancer. 2006;106(12):2701–2706. doi:10.1002/cncr.21937
18. Kim HS, Bindiganavile SS, Han I. Oncologic outcome after local recurrence of chondrosarcoma: analysis of prognostic factors. J Surg Oncol. 2015;111(8):957–961. doi:10.1002/jso.23925
19. Xue R, Lewis VO, Moon BS, Lin PP. Local recurrence of Ewing sarcoma: is wide excision an acceptable treatment? J Surg Oncol. 2019;120(4):746–752.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
