Back to Journals » Journal of Pain Research » Volume 15
Spinal Cord Stimulation in Special Populations: Best Practices from the American Society of Pain and Neuroscience to Improve Safety and Efficacy
Authors Lee JM, Lee D, Christiansen S, Hagedorn JM , Chen Z, Deer T
Received 17 May 2022
Accepted for publication 11 September 2022
Published 19 October 2022 Volume 2022:15 Pages 3263—3273
DOI https://doi.org/10.2147/JPR.S372921
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Robert Twillman
Jennifer M Lee,1 David Lee,2 Sandy Christiansen,3 Jonathan M Hagedorn,4 Zheyan Chen,3 Timothy Deer5
1Department of Sports & Spine, EvergreenHealth Medical Group, Kirkland, WA, USA; 2Fullerton Orthopedic Surgery Medical Group, Fullerton, CA, USA; 3Department of Anesthesiology & Perioperative Medicine, Oregon Health Sciences University, Portland, OR, USA; 4iSpine Pain Physicians, Maple Grove, MN, USA; 5The Spine and Nerve Center of the Virginias, Charleston, WV, USA
Correspondence: Jennifer M Lee, Email [email protected]
Abstract: Chronic bleeding disorders, allergy to implants, and chronic infections are all complicating factors when considering neuromodulation therapies. The American Society of Pain and Neuroscience (ASPN) determined a need for clinical guidance in these special patient populations that have increased risk of complications, in order to ensure patient safety and optimal outcomes with device implantation. The purpose of this publication was to review the published literature and explore the unique clinical challenges encountered among several special patient populations with relation to spinal cord stimulation. The executive board of the ASPN appointed a diverse group of well-established physicians to develop best practice guidelines regarding spinal cord stimulation implantation in these special populations. The physicians used the United States Preventive Services Task Force (USPSTF) structured guidelines for grading and level of certainty to make evidence-based recommendations about clinical practice. Where sufficient evidence was lacking to justify a USPSTF ranking, the physicians queried experts in neuromodulation and achieved consensus. These best practices and interventional guideline found the evidence for the use of neuromodulation in specialized patient populations to be relatively modest.
Keywords: guidelines, metallurgic allergy, epidural hematoma, epidural abscess
Introduction
Though spinal cord stimulation (SCS) has been an established therapy for the treatment of chronic pain for many years, the past decade has been notable for multiple remarkable advancements in the science. There has been rapid innovation in lead design, programming algorithms, and pulse generator capabilities. Research following these technological improvements has highlighted the safety and efficacy of this therapy for the treatment of a variety of chronic pain conditions. In reflection of these developments, there has been increased utilization of SCS. Among the Medicare population alone, a review of outpatient billing claims between 2009 and 2018 revealed a 186% increase in SCS trials.1
Given the increased utilization, pain physicians inherently encounter patient scenarios in which pain treatment with SCS requires special consideration. The most common complication of SCS is lead migration (88.5%),2 though the incidence of this migration causing failure of therapy is much lower (14%).3 Far less common are certain other rare complications for which the authors wish to raise awareness and encourage consideration. The American Society of Pain and Neuroscience (ASPN) has determined a need for clinical guidance in these special patient populations related to the increased risk of complications, and to ensure patient safety and optimal outcomes with SCS. Those special circumstances include patients who have chronic bleeding disorders, allergic or immunologic sensitivity to implanted materials, and a history of spine infections. Though the incidence of epidural hematoma may be as low as 0.5%, the clinical consequences of this event is can be devastating.4 Similarly, postoperative infection is among the most foreboding consequences of neuromodulation. Despite the recent bounty of literature in the field of neuromodulation, definition on the prevention and management of those patients at highest risk for infection is lacking. Also wanting is direction on the management of patients with metallurgic hypersensitivity, a rare and confounding condition.
Best clinical practices for neuromodulation have been established over time and continue to evolve based on peer-reviewed evidence and the innovation of new methods and equipment. Traditionally, these best practices have been the result of the review of available evidence, consideration of the standard of care, and the achievement of thoughtful consensus among clinical experts within the specialty. For the pain physician, these best practices provide a resource for best clinical management of individual patient treatments.
The purpose of this publication is to review the published literature and explore the unique clinical challenges encountered among several special patient populations in relation to SCS. The authors aim to increase awareness of the potential risk among patients with chronic bleeding disorders, metallurgic allergy, and/or a history of chronic infections. The authors aim to provide best practice guidelines for the management of neuromodulation therapy among these special patient populations.
Methods
The executive board of the ASPN accepted nominations of a diverse group of well-established physicians to develop best practice guidelines regarding SCS implantation in several unique patient populations, including patients with a history of chronic bleeding disorders, those with a history of metallurgic allergy, and those patients at increased risk of infection. Authors were selected based on clinical experience, expertise in neuromodulation, and prior experience with guideline development.
The development of this guidance involved PubMed and MEDLINE databases, and the United States Preventive Services Task Force (USPSTF). The USPSTF is an independent, volunteer panel of national experts in disease prevention and evidence-based medicine. The USPSTF structured guidelines for grading and level of certainty are intended to be used in making evidence-based recommendations about clinical preventive services (Table 1).5 Where sufficient evidence (Table 2) is lacking to justify a USPSTF ranking, recognized experts representing the current state of neuromodulation were queried and consensus was achieved (Table 3). Note: A quorum was defined as 80% of participants available for the vote.
 |
Table 1 Hierarchy of Studies by the Type of Design (US Preventive Services Task Force) |
 |
Table 2 Meaning of Recommendation Degrees (US Preventive Services Task Force) |
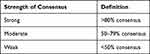 |
Table 3 Strength of Consensus |
Unique Patient Populations
Chronic Bleeding Disorders
Scope of the Problem
SCS has enjoyed increased popularity over the past decade in the treatment of chronic pain owing to its safety profile, established efficacy for several chronic pain pathologies, and minimally invasive nature. The last of these is especially attractive among patients with medical comorbidities aiming to avoid the risks of general anesthesia, prolonged recovery times with more invasive surgical options, and procedural blood loss. While there are published guidelines by the Neuromodulation Appropriateness Consensus Committee (NACC) regarding chronic anticoagulation therapy during SCS procedures, this situation differs critically from the care of patients with chronic bleeding disorders. The risk for patients with chronic bleeding disorders extends beyond the immediate perioperative time frame. There is a theoretical increased bleeding risk related to the presence of SCS leads in the epidural space, which coexists with a network of epidural venous plexuses. The consequences and management of spontaneous or late bleeding must be considered as well. Specifically, we consider patients with chronic thrombocytopenia and hepatic dysfunction.
Disease State: Chronic Thrombocytopenia
There exists a myriad of rare causes of chronic thrombocytopenia which require special consideration in relation to SCS. Causes include, but are not limited to, myelodysplastic syndromes (MDS), aplastic anemia, leukemias, and hypersplenism. The severity of thrombocytopenia and platelet dysfunction among patients with MDS is variable.6,7 Among those afflicted, data indicate that 26% have moderate thrombocytopenia (platelet counts 20,000–50,000 cells/L) and 17% have severe thrombocytopenia (platelet counts <20,000 cells/L). Though the severity of thrombocytopenia is benchmarked by serum platelet counts, this does not reliably predict clinical manifestations or complications of the disorder. Furthermore, the clinical presentation may range from minor signs, such as petechiae, gingival bleeding, or traumatic hematomas, to more deleterious complications that can include occult bleeding or retinal hemorrhage. The incidence of hemorrhagic complication is reported to range from 3% to 53%, and hemorrhagic deaths range from 14% to 24%.7 In the cohort of MDS patients who progress to acute myelogenous leukemia (AML), treatment with chemotherapy is further associated with an increased incidence and severity of thrombocytopenia.8,9 Consistent with the data from MDS, the incidence of bleeding disorders among patients with aplastic anemia is increased in those with platelet counts less than 20,000 cells/L.10
Perioperative Treatment: Chronic Thrombocytopenia
Mitigation of the bleeding risk related to chronic thrombocytopenia centers around the transfusion of platelets. There are inconsistencies and gaps in the guidelines for prophylactic platelet transfusion among different societies and agencies. Spanish, Italian, and British guidelines provide more specific recommendations on the transfusion threshold according to the bleeding risk of the planned procedure.11–13 For neurosurgical or ophthalmologic procedures, the Spanish guidelines recommend prophylactic platelet transfusion for platelet counts less than 80,000 cells/L, while the British and Italian recommendations suggest transfusion for platelet counts less than 100,000 cells/L. Though these guidelines may direct the implanting physicians on perisurgical management of the coagulopathy, they do not assist in the mitigation of risk beyond this period of time. However, the NACC guidelines state that SCS lead insertion and removal are the time periods when the risk of bleeding is highest.
Disease State: Hepatic Dysfunction
Patients with hepatic dysfunction are also deserving of special consideration with regard to risk of bleeding complications. Impairments in hemostasis are multiple, and may include thrombocytopenia, platelet dysfunction, coagulation factor II, V, VII, VIII IX, X, and XI deficiencies, vitamin K deficiency, elevated tissue plasminogen activator (t-PA) levels, low levels of alpha-2-antiplasminogen, and dysfibrinogenemia.14 The typically slow progressive nature of liver disease does allow for compensatory mechanisms to the perturbations in the hematologic system; however, in states of advanced disease these mechanisms are overcome and clinically evident bleeding or clotting disturbances may occur.15 Laboratory testing of coagulation in patients with chronic liver disease is an important element of a clinician’s presurgical assessment, though such tests do not measure relevant compensatory mechanisms, including protein C and von Willebrand factor levels. Perhaps the most frequently considered coagulation measurement, the international normalized ratio (INR), has been repeatedly reported to be an inadequate predictor of procedural bleeding in cases of percutaneous,16 laparoscopic,16 and coronary artery catheterization procedures,17 and others.
Perioperative Treatment of the Issue: Hepatic Dysfunction
Common serologic tests of coagulation alone are inadequate in the presurgical assessment. The utility of the INR in predicting bleeding risk is an area of controversy. The American Association for the Study of Liver Diseases states that no specific INR level is clearly predictive of bleeding risk,18 while the Society of Interventional Radiology recommends correction of INR, with fresh frozen plasma (FFP) or vitamin K, to 1.5 for moderate- to high-risk procedures.19 Platelet count is similarly inadequate as a stand-alone test indicating risk of bleeding in patients with hepatic dysfunction. This is related to the platelet dysfunction in the coagulation cascade in the environment of hypothrombinemia and other coagulation factor deficiencies. Unfortunately, advanced functional tests of the coagulation system, including platelet function assays and rotational thromboelastometry (TEG), are not widely available in non-academic practices. However, these tests would be beneficial in this scenario.
Recommendations with Evidence Grading
Patients with chronic inherited and acquired bleeding disorders represent a special population which requires careful weighing of risks and benefits, and active engagement in discussions with the patient and patient’s representatives. Whenever possible, the pain physician should engage the necessary multidisciplinary team, including hematology, oncology, hepatology, and others, as appropriate to plan the safest course of treatments that responsibly balances the risks of SCS treatment (Table 4).
 |
Table 4 Recommendations Regarding Implanting Spinal Cord Stimulator Device in Patients with Chronic Bleeding Disorders |
Allergic or Immunologic Reaction to Neuromodulation Implants
Scope of the Problem
Allergic contact dermatitis (ACD) is a type 4 or delayed-type hypersensitivity (DTH) response. The initial or induction phase of ACD occurs when the hapten combines with a protein to form a complex that leads to the expansion of an allergen-specific T-cell population; the name for this process is sensitization. During the elicitation phase, re-exposure to the antigen leads to the development of dermatitis. It results from the contact of an offending chemical or antigen with the skin, and the subsequent T-cell-mediated response.20 Morphology and location of the dermatitis are often the best indicators of the offending agent. Metals are common causes of ACD, with nickel being the most common.
ACD occurs in approximately one in five people. Although ACD is common, allergic or immunologic reactions to medical implants are not frequently reported in association with spinal cord stimulators. The incidence has been estimated to be as low as 0.1%.21 Metallurgic reactions reported for pacemakers and similar implantable devices, while more prevalent, are still rare. Given the rarity of allergic reactions to implantable devices, it is possible that it is underdiagnosed and mistaken for infection. Clinically, patients with allergic reactions to implantable devices have presented with progressive cutaneous symptoms and discomfort months after implantation, in the absence of signs or symptoms of infection (ie fever, chills, and constitutional changes).
An allergic response to implantable devices often results as a reaction to implantable device componentry; these include the implantable pulse generator (IPG), electrodes (on leads), leads, and lead extensions. Components are typically covered with a silicone or polymer coating to limit external exposure to internal materials in the IPG casing and leads. As a result, only the titanium housing, polymer coating, and electrode contacts directly interact with human tissue. Other materials often found within SCS componentry include platinum, stainless steel, MP-35N alloy, gold, silicone, parylene, polysulfone, polyetherenetherketone (PEEK), polymer fluorinated ethylene propylene (FEP), fluoropolymer, and epoxy. While rare, identifying a reaction to SCS componentry is essential to 1) prevent disruption or failure of the SCS therapy, 2) optimize the patient postoperative experience, and 3) limit postoperative sequelae.
Evidence of Allergic or Immunologic Reactions to SCS Implants
In a 2021 publication, the authors identified a total of 13 case reports of hypersensitivity to neuromodulation devices.22 The majority of those cases (11/13) involved SCS, with one to deep brain stimulation and one to an occipital nerve stimulator. Five out of 13 cases reported allergies to nickel compounds prior to implantation, and six patients had reported a history of allergies to other sources. Symptoms occurred between eight days and three years after implantation; 11 out of the 13 hypersensitivities manifested within six months of surgery. In one case where the hypersensitivity reaction presented at three years post-surgery, the silicone coating over the electrode was torn.23 In the majority of these reports, the outcome was SCS explantation.
On review of the literature, there were a few additional case reports/series of hypersensitivity reactions following SCS implantation. Chaudhry et al described three reported cases of allergic reaction: the first case was a reaction to lead extension hardware, the second case a reaction to leads and/or possibly the anchors, and the third case a reaction to lead extension and the IPG.24 The SCS systems were explanted in all three instances, with uneventful reimplantation in one of the reported cases. Delaplace et al reported on two separate cases of allergic reaction.25 The first case detailed a cutaneous inflammatory erythema in the dorsolumbar region associated with reduced efficiency of stimulation. Removal of the neurostimulator led to resolution of the cutaneous symptoms. Histopathologic examination of the biopsy sample showed foreign-body granuloma formation. The same symptoms subsequently recurred on the surgical scar and histopathology showed granuloma formation in response to particles of silicone present in the connector. The cutaneous eruption subsided rapidly after excision. In the second case, pruriginous reticular erythema was rapidly observed on the skin just above the neurostimulator, with papules around the erythema. Histopathology of two cutaneous biopsies showed evidence of contact dermatitis. Skin-patch tests performed with components of the neurostimulator leads proved positive to two types of silicone after 72 hours. The condition was successfully controlled using topical corticosteroid therapy.
In the rarest of cases, there may be a hypersensitivity reaction within the spinal canal. In one reported case, a patient developed tolerance to a percutaneously placed cervical SCS four months after implantation, followed by the onset of spastic quadriparesis nine months after implantation.26 The stimulator was explanted, and contrast-enhanced MRI revealed an enhancing epidural mass where the system had been placed, with severe spinal cord compression. Decompression was carried out, and the patient experienced neurologic improvement. Pathologic examination revealed fibrotic tissue with granulomatous and multinucleated giant cell reactions. The authors, on review, identified six similar cases associated with paddle electrode placement. The small number of cases precludes a complete understanding of the pathophysiology, but it appears to be an exaggerated inflammatory reaction, based on histologic reports. Inciting events of inflammatory reactions could include foreign body reaction, subclinical allergic response, infection, hemorrhage, and dynamic instability with local repetitive trauma. The authors stopped short of suggesting that this was due to an allergic reaction, but admitted that it could not be fully excluded.
Perioperative Treatment of the Issue: Allergic Reactions
Current vendors of neuromodulation systems utilize similar component materials, which include, but are not limited, to silicone rubber (lead anchors), polyurethane (leads, extensions), titanium (IPG), and platinum/iridium (electrodes). Device vendors also offer an “allergy test kit”, which includes small samples of each of these components. For those patients with a history of hypersensitivity reactions to other medical device products, or in cases where the patient or physician has concern about such reactions, the kit may be requested and applied topically as a skin patch test.
Physicians should also be attentive to signs of cutaneous hypersensitivity reactions during both the SCS trial and post-implantation time periods. If there are signs or symptoms of suspected contact allergy, a preliminary work-up should be performed to rule out infection, given the similar appearance of these conditions. If negative, patch testing should be performed (if not already done prior) to identify the specific allergen. In the published literature, only two such cases reported successful treatment with topical corticosteroids.25,27 If device explant is required, tissue samples should be obtained for histologic evaluation to distinguish and confirm the diagnosis of allergic reaction versus infection. If an allergic reaction exists, histologic samples of the involved tissue will demonstrate evidence of an acute and chronic inflammatory reaction involving multinucleated giant cells, eosinophils, and resultant tissue necrosis.
Recommendations with Evidence Grading
The evidence supports that all patients should be screened for contact allergies prior to implantation (Table 5). Additional precautions are necessary for the special population of patients with allergy or immunologic reactions to implanted medical devices. Pain physicians are recommended to refer all patients in this special population to a dermatologist or an allergist who specializes in patch testing. If infection cannot be ruled out, the device must be modified in order to be safely implanted.
 |
Table 5 Recommendations Regarding Implanting Spinal Cord Stimulator Device in Patients with Allergy or Immunologic Reaction to Implanted Medical Devices |
High Risk for Infection
Scope of the Problem
Surgical spine infection is among the most serious complications of SCS implantation. Though the overall incidence is low, at 2.45%, surgical spine infections are associated with significant morbidity, mortality, and healthcare-related costs.21,28–30 Most commonly, symptoms are as subtle as incisional pain and wound erythema, though the majority of cases ultimately require device explantation.31 Treatment, however, may range from systemic antibiotics to urgent explantation of the implanted device, and, in the most severe cases, spinal debridement and stabilization.
Infections in the spine most commonly affect the discs or vertebral bodies (spondylodiscitis), followed by the epidural space (epidural abscesses), meninges (arachnoiditis or meningitis), and spinal cord (intramedullary abscesses).32
Most causes of spine infections are bacterial in origin, with staphylococcus species being the most common in developed countries.33 Immunocompromised patients are more at risk for spinal infections from viral infections, including human immunodeficiency virus (HIV), herpes simplex virus I and II, cytomegalovirus, and varicella zoster. Fungal infections are extremely rare but can occur in immunocompromised individuals.
The incidence of all-cause spine infections has been steadily increasing over the years, with an estimated 6.5 cases per 100,000 each year. Risk factors include previous spine surgery with or without instrumentation, diabetes, advanced age, intravenous drug use, HIV infection, immunosuppression, history of cancer, renal failure, infection at a distant source, and liver cirrhosis.34 Studies report postoperative spondylodiscitis rates following spine surgery of up to 3%, and the infection can cause persistent axial back pain.35,36 One study of failed back surgery syndrome patients reported up to a 7% prevalence of a history of postoperative spondylodiscitis.37
Perioperative Treatment: SCS Reimplantation Following Infection-Related SCS Explantation
With the rising incidence of chronic spine infection and/or history of spine infections, it is important to consider how to address these patient populations when planning future neuromodulation procedures. The NACC published recommendations for infection prevention and management in 2017. Though the evidence is weak, following SCS-associated infection the NACC recommends the resolution of infectious symptoms for at least 90 days prior to considering reimplantation.38
Perioperative Treatment: SCS Implantation in the Setting of Chronic Infection or Previous Spine Infection
There is an absence of high-quality evidence addressing de novo or reimplantation of SCS in the setting of chronic infection or previous spine infection. There have been isolated case reports of patients with SCS infections treated with device removal and targeted antibiotics, and successfully reimplanted without infection relapse.39,40 One case report describes two patients with HIV-related neuropathy treated with SCS without any infectious complications at 14-month and three-year follow-up visits.41
However, while there is a gap in the neuromodulation-specific literature, there is more extensive literature in the neurosurgery, orthopedic surgery, cardiology, and plastic surgery realms that may be applicable to neuromodulation surgeries.
In patients with a history of previous surgical spine infection, one orthopedic surgery study reported a statistically significant risk factor of deep infection with subsequent surgeries among this patient population.42 One descriptive, retrospective cohort analysis found that superficial spinal surgical site infections could be effectively treated by local wound care and antibiotic therapy.43 Similarly, the first line treatment of postoperative discitis is non-operative management with long-term antibiotics.44–47 Spinal hardware infections are harder to treat. There are case reports and retrospective reviews of the successful treatment of infected spinal hardware with early detection, aggressive surgical debridement, and appropriate antibiotics, without removal.47–50
Instrumentation in the setting of infection remains controversial in the neurosurgery literature. There is not one standard universal protocol for treating deep wound infections utilizing spinal instrumentation. While, traditionally, it was thought that explantation of spinal implants was critical for source control of the infection, current practices now vary in terms of the criteria for hardware removal. According to Mavrogenis et al, spinal hardware placement can be safe and successful after a pre-existing spinal infection has been treated with thorough debridement and antibiotic administration.51 Surgeons have also safely placed spinal hardware in actively infected sites for urgent spine stabilization, with low rates of complication, 1.74% to 4.2%.52–54 These rates are comparable to those in patients who develop infected hardware with no prior history of spinal infection, which range between 1.9% and 4.4%.42,43,48,55–57 One retrospective review found no significant increase in the rates of recurrent infection or reoperation in patients who underwent instrumented fusion versus decompression alone for primary spinal infections.58
In the plastic surgery literature, the reinfection rate after cranioplasty is reported to be as high as 32%. Infection rates are higher when surgeons perform the cranioplasty procedures within 14 days of the initial craniectomy, with the hypothesis that interrupting the wound healing process may predispose to subsequent wound infections.59,60
With cardiac generator pocket infections, the American Heart Association recommends reimplanting the generator on the contralateral side to lower the risk of reinfection.61
Recommendations with Evidence Grading
Evidently, assessment and management considerations with respect to SCS rely on the extrapolation of evidence from related surgical specialty experience. On this basis, the evidence supports considering each infection on a case-by-case basis (Table 6). There is evidence to support the use of oral antibiotics for superficial infections; in contrast, deeper infections, infections presenting after one year of implantation, and those associated with neurologic complications often need extended intravenous antibiotic therapy for many months, and reimplantation may not be advisable.
 |
Table 6 Recommendations Regarding Implanting Spinal Cord Stimulator Device in Patients with a History of Spine Infection |
If the surgeon plans future neuromodulation surgery, the increased risk of recurrent infection inherent in all revision surgeries should be included in the informed consent discussions with patients. The patient should also be informed of the possibility of further increased risk of infection due to a history of spine infection. If the physician and patient make a joint decision to proceed to spinal cord stimulator implantation, the pain physician should consider consulting infectious disease or clinical microbiology professionals to advise on perioperative antimicrobial management based on the patient’s infection history. Patients with pre-existing blood-borne infections, such as hepatitis or HIV, should work with their infectious disease or primary care doctor to decrease the viral load before implantation.62
Lastly, physicians should work with patients preoperatively to optimize all other factors that contribute to infection risk, including obesity, glucose management, and tobacco use.63 The NACC guidelines specifically recommend superior glucose control and smoking cessation for at least four weeks prior to surgery.38 They also recommend optimizing nutritional status and limiting the use of preoperative steroids.38,64
Conclusion
As the utilization of neuromodulation expands, based on strengthened evidence and expanded indications, physicians are increasingly confronted with challenging clinical scenarios. The risks inherent in these conditions often make these patient populations poor candidates for invasive, conventional surgical options. As such, neuromodulation, in some instances, is the most appropriate therapy for refractory pain among medically challenging patients. As a result, the authors identified a need for further guidance, as comprehensive and cohesive guidance for the management of special patient populations does not currently exist. In this publication, the authors performed a narrative review of patients with chronic bleeding disorders, or allergic or immunologic reactions to implant materials, and those patients with a history of previous spine infection, in relation to neuromodulation. Using the resources of PubMed and MEDLINE database searches, evidence-based assessment from USPSTF, and expert physician consensus, the authors formalized management recommendations. Consensus recommendations for each patient population were accompanied by level of evidence and recommendation strength to help guide applicability.
Evidence for the use of neuromodulation in specialized patient populations was found to be relatively modest. This is likely attributable to the select nature of the patient populations studied. This review paper illustrates the general need for further studies. Despite this, recommendations were based on fundamentally sound principles shared in both the pain and surgical communities. All recommendations incorporate 1) the necessity for preparation, 2) communication and collaboration among allied treating physicians, and 3) shared decision making with the patient. The use of these recommendations may allow for the safe and effective use of neuromodulation in a patient population that has few therapeutic options for pain management.
Disclosure
Dr Sandy Christiansen reports grants from Avanos, during the conduct of the study. Dr Jonathan M Hagedorn reports personal fees including funded research from Abbott and Saluda; and personal fees from Boston Scientific and Nevro, outside the submitted work. Dr Timothy Deer reports personal fees for consultant, research, and/or stock options from Abbott, Saluda, Nalu, and Mainstay, during the conduct of the study; and personal fees for consultant, research, and/or stock options from Vertos, SpineThera, Cornerloc, Ethos, SPR Therapeutic, Medtronic, Boston Scientific, PainTeq, Tissue Tech, Spinal Simplicity, and Avanos, outside the submitted work; in addition, Dr Timothy Deer has a patent for DRG Leads pending for Abbott. The remaining authors report no conflicts of interest.
References
1. Manchikanti L, Pampati V, Vangala BP., et al. Spinal Cord Stimulation Trends of Utilization and Expenditures in Fee-For-Service (FFS) Medicare Population from 2009 to 2018. Pain Physician. 2021;24:293–308. doi:10.36076/ppj.2021.24.401
2. Dombovy-Johnson ML, D’Souza RS, Ha CT, Hagedorn JM. Incidence and risk factors for spinal cord stimulator lead migration with or without loss of efficacy: a retrospective review of 91 consecutive thoracic lead implants. Neuromodulation Technol Neural Interface. 2022;25(5):731–737. doi:10.1111/ner.13487
3. Patel SK, Gozal YM, Saleh MS, Gibson JL, Karsy M, Mandybur GT. Spinal cord stimulation failure: evaluation of factors underlying hardware explantation. J Neurosurg Spine. 2019;32(1):133–138. doi:10.3171/2019.6.SPINE181099
4. Labaran L, Jain N, Puvanesarajah V, Jain A, Buchholz AL, Hassanzadeh H. A retrospective database review of the indications, complications, and incidence of subsequent spine surgery in 12,297 spinal cord stimulator patients. Neuromodulation Technol Neural Interface. 2020;23(5):634–638. doi:10.1111/ner.12952
5. US Preventive Services Task Force Procedure Manual. US Prev Serv Task Force; 2021. Available from: https://uspreventiveservicestaskforce.org/uspstf/about-uspstf/methods-and-processes/procedure-manual.
6. Bowen D, Culligan D, Jowitt S, et al. Guidelines for the diagnosis and therapy of adult myelodysplastic syndromes. Br J Haematol. 2003;120(2):187–200. doi:10.1046/j.1365-2141.2003.03907.x
7. Kantarjian H, Giles F, List A, et al. The incidence and impact of thrombocytopenia in myelodysplastic syndromes. Cancer. 2007;109(9):1705–1714. doi:10.1002/cncr.22602
8. Lee ST, Jang JH, Suh HC, Hahn JS, Ko YW, Min YH. Idarubicin, cytarabine, and topotecan in patients with refractory or relapsed acute myelogenous leukemia and high-risk myelodysplastic syndrome. Am J Hematol. 2001;68(4):237–245. doi:10.1002/ajh.1188
9. Gupta P, LeRoy SC, Luikart SD, Bateman A, Morrison VA. Long-term blood product transfusion support for patients with myelodysplastic syndromes (MDS): cost analysis and complications. Leuk Res. 1999;23(10):953–959. doi:10.1016/S0145-2126(99)00113-7
10. Singh M, Singh V, Singh DP, Bohra GK, Misra AK. Hemorrhagic manifestation in different etiologies of pancytopenia: a prospective, cross-sectional study. J Fam Med Prim Care. 2021;10(2):804–808. doi:10.4103/jfmpc.jfmpc_1117_20
11. Arbona FCP. Guía sobre la transfusión de Componentes sanguíneos y derivados plasmáticos, Sociedad Española de Transfusión Sanguínea y Terapia Celular (SETS). 2015.
12. Liumbruno G, Bennardello F, Lattanzio A, Piccoli P, Rossetti G. Recommendations for the transfusion of plasma and platelets. Blood Transfus. 2009;7(2):132. doi:10.2450/2009.0005-09
13. Estcourt LJ, Birchall J, Allard S, et al. Guidelines for the use of platelet transfusions. Br J Haematol. 2017;176(3):365–394. doi:10.1111/bjh.14423
14. Lisman T, Leebeek FWG, de Groot PG. Haemostatic abnormalities in patients with liver disease. J Hepatol. 2002;37(2):280–287. doi:10.1016/S0168-8278(02)
15. Northup PG, Caldwell SH. Coagulation in Liver Disease: a Guide for the Clinician. Clin Gastroenterol Hepatol. 2013;11(9):1064–1074. doi:10.1016/j.cgh.2013.02.026
16. Gilmore IT, Burroughs A, Murray-Lyon IM, Williams R, Jenkins D, Hopkins A. Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: an audit by the British Society of Gastroenterology and the Royal College of Physicians of London. Gut. 1995;36(3):437. doi:10.1136/gut.36.3.437
17. Townsend JC, Heard R, Powers ER, Reuben A. Usefulness of International Normalized Ratio to Predict Bleeding Complications in Patients With End-Stage Liver Disease Who Undergo Cardiac Catheterization. Am J Cardiol. 2012;110(7):1062–1065. doi:10.1016/j.amjcard.2012.05.043
18. Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver biopsy. Hepatology. 2009;49(3):1017–1044. doi:10.1002/hep.22742
19. Patel IJ, Davidson JC, Nikolic B, et al. Consensus Guidelines for Periprocedural Management of Coagulation Status and Hemostasis Risk in Percutaneous Image-guided Interventions. J Vasc Interv Radiol. 2012;23(6):727–736. doi:10.1016/j.jvir.2012.02.012
20. Aquino M, Rosner G. Systemic contact dermatitis. Clin Rev Allergy Immunol. 2019;56(1):9–18. doi:10.1007/s12016-018-8686-z
21. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg Spine. 2004;100(3):254–267. doi:10.3171/spi.2004.100.3.0254
22. Brown A, Mandelberg NJ, Munoz‐Mendoza D, et al. Allergy Considerations in Implanted Neuromodulation Devices. Neuromodulation Technol Neural Interface. 2021;24(8):1307–1316. doi:10.1111/ner.13332
23. Nosbaum A, Rival-Tringali A, Barth X, et al. Nickel-induced systemic allergic dermatitis from a sacral neurostimulator. Contact Dermatitis. 2008;59(5):319–320. doi:10.1111/j.1600-0536.2008.01434.x
24. Chaudhry ZA, Najib U, Bajwa ZH, Jacobs WC, Sheikh J, Simopoulos TT. Detailed analysis of allergic cutaneous reactions to spinal cord stimulator devices. J Pain Res. 2013;6:617. doi:10.2147/JPR.S44676
25. Delaplace M, Maître F, Dufour T, et al. Érythème cutané provoqué par une neurostimulation cordonale postérieure: Deux observations. Vol. 137. Elsevier; 2010:297–300
26. Scranton RA, Skaribas IM, Simpson RK. Spinal stimulator peri-electrode masses: case report. J Neurosurg Spine. 2015;22(1):70–74. doi:10.3171/2014.10.SPINE1425
27. McKenna K, McCleane G. Dermatitis induced by a spinal cord stimulator implant. Contact Dermatitis. 1999;41(4):229. doi:10.1111/j.1600-0536.1999.tb06142.x
28. Hoelzer BC, Bendel MA, Deer TR, et al. Spinal Cord Stimulator Implant Infection Rates and Risk Factors: a Multicenter Retrospective Study. Neuromodulation. 2017;20(6):558–562. doi:10.1111/ner.12609
29. Follett KA, Boortz-Marx RL, Drake JM, et al. Prevention and management of intrathecal drug delivery and spinal cord stimulation system infections. J Am Soc Anesthesiol. 2004;100(6):1582–1594. doi:10.1097/00000542-200406000-00034
30. Hayek SM, Veizi E, Hanes M. Treatment-limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation Technol Neural Interface. 2015;18(7):603–609. doi:10.1111/ner.12312
31. Bendel MA, O’Brien T, Hoelzer BC, et al. Spinal cord stimulator related infections: findings from a multicenter retrospective analysis of 2737 implants. Neuromodulation Technol Neural Interface. 2017;20(6):553–557. doi:10.1111/ner.12636
32. Butler JS, Shelly MJ, Timlin M, Powderly WG, O’Byrne JM. Nontuberculous Pyogenic Spinal Infection in Adults: a 12-Year Experience From a Tertiary Referral Center. Spine. 2006;31(23). doi:10.1097/01.brs.0000244662.78725.37
33. Waheed G, Soliman MA, Ali AM, Aly MH. Spontaneous spondylodiscitis: review, incidence, management, and clinical outcome in 44 patients. Neurosurg Focus. 2019;46(1):E10. doi:10.3171/2018.10.FOCUS18463
34. Duarte RM, Vaccaro AR. Spinal infection: state of the art and management algorithm. Eur Spine J. 2013;22(12):2787–2799. doi:10.1007/s00586-013-2850-1
35. Van Goethem J, Parizel P, Jinkins J. MRI of the postoperative lumbar spine. Neuroradiology. 2002;44(9):723–739. doi:10.1007/s00234-002-0790-2
36. Onesti ST. Failed back syndrome. The Neurologist. 2004;10(5):259–264. doi:10.1097/01.nrl.0000138733.09406.39
37. Hayashi D, Roemer FW, Mian A, Gharaibeh M, Müller B, Guermazi A. Imaging features of postoperative complications after spinal surgery and instrumentation. Am J Roentgenol. 2012;199(1):W123–W129. doi:10.2214/AJR.11.6497
38. Deer TR, Provenzano DA, Hanes M, et al. The Neurostimulation Appropriateness Consensus Committee (NACC) recommendations for infection prevention and management. Neuromodulation Technol Neural Interface. 2017;20(1):31–50. doi:10.1111/ner.12565
39. Schwartz RH, Southerland W, Urits I, Kaye AD, Viswanath O, Yazdi C. Successful Reimplantation of Spinal Cord Stimulator One Year after Device Removal Due to Infection. Surg J. 2021;7(01):e11–e13. doi:10.1055/s-0040-1722179
40. Esquer Garrigos Z, Farid S, Bendel MA, Sohail MR. Spinal cord stimulator infection: approach to diagnosis, management, and prevention. Clin Infect Dis. 2020;70(12):2727–2735. doi:10.1093/cid/ciz994
41. Knezevic NN, Candido KD, Rana S, Knezevic I. The Use of Spinal Cord Neuromodulation in the Management of HIV-Related Polyneuropathy. Pain Physician. 2015;18(4):E643–50.
42. Ter Gunne AFP, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine. 2009;34(13):1422–1428. doi:10.1097/BRS.0b013e3181a03013
43. Ter Gunne AFP, Mohamed AS, Skolasky RL, Van Laarhoven CJ, Cohen DB. The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine. 2010;35(13):1323–1328. doi:10.1097/BRS.0b013e3181bcde61
44. Chelsom J, Solberg CO. Vertebral osteomyelitis at a Norwegian university hospital 1987-1997: clinical features, laboratory findings and outcome. Scand J Infect Dis. 1998;30(2):147–151. doi:10.1080/003655498750003537
45. Chang CW, Tsai TT, Niu CC, et al. Transforaminal Interbody Debridement and Fusion to Manage Postdiscectomy Discitis in Lumbar Spine. World Neurosurg. 2019;121:e755–e760. doi:10.1016/j.wneu.2018.09.211
46. Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res. 2002;398:50–59. doi:10.1097/00003086-200205000-00008
47. Hegde V, Meredith DS, Kepler CK, Huang RC. Management of postoperative spinal infections. World J Orthop. 2012;3(11):182. doi:10.5312/wjo.v3.i11.182
48. Glassman SD, Dimar JR, Puno RM, Johnson JR. Salvage of instrumented lumbar fusions complicated by surgical wound infection. Spine. 1996;21(18):2163–2169. doi:10.1097/00007632-199609150-00021
49. Núñez-Pereira S, Pellisé F, Rodríguez-Pardo D, et al. Implant survival after deep infection of an instrumented spinal fusion. Bone Jt J. 2013;95-B(8):1121–1126. doi:10.1302/0301-620X.95B8.30784
50. Kasliwal MK, Tan LA, Traynelis VC. Infection with spinal instrumentation: review of pathogenesis, diagnosis, prevention, and management. Surg Neurol Int. 2013;4(Suppl 5):S392–S403. doi:10.4103/2152-7806.120783
51. Mavrogenis AF, Megaloikonomos PD, Igoumenou VG, et al. Spondylodiscitis revisited. EFORT Open Rev. 2017;2(11):447–461. doi:10.1302/2058-5241.2.160062
52. Rayes M, Colen CB, Bahgat DA, et al. Safety of instrumentation in patients with spinal infection: clinical article. J Neurosurg Spine SPI. 2010;12(6):647–659. doi:10.3171/2009.12.SPINE09428
53. Lee JS, Suh KT. Posterior lumbar interbody fusion with an autogenous iliac crest bone graft in the treatment of pyogenic spondylodiscitis. J Bone Joint Surg Br. 2006;88-B(6):765–770. doi:10.1302/0301-620X.88B6.17270
54. Rath SA, Neff U, Schneider O, Richter HP. Neurosurgical Management of Thoracic and Lumbar Vertebral Osteomyelitis and Discitis in Adults: a Review of 43 Consecutive Surgically Treated Patients. Neurosurgery. 1996;38(5):548. doi:10.1097/00006123-199605000-00013
55. Olsen MA, Nepple JJ, Riew KD, et al. Risk Factors for Surgical Site Infection Following Orthopaedic Spinal Operations. JBJS. 2008;90(1):215. doi:10.2106/JBJS.F.01515
56. Olsen MA, Mayfield J, Lauryssen C, et al. Risk factors for surgical site infection in spinal surgery. J Neurosurg Spine. 2003;98(2):149–155. doi:10.3171/spi.2003.98.2.0149
57. Fang A, Hu SS, Endres N, Bradford DS. Risk Factors for Infection After Spinal Surgery. Spine. 2005;30(12):54. doi:10.1097/01.brs.0000166532.58227.4f
58. Bydon M, De la Garza-Ramos R, Macki M, et al. Spinal Instrumentation in Patients with Primary Spinal Infections Does Not Lead to Greater Recurrent Infection Rates: an Analysis of 118 Cases. World Neurosurg. 2014;82(6):e807–e814. doi:10.1016/j.wneu.2014.06.014
59. Soto E, Restrepo RD, Grant JH, Myers RP. Outcomes of Cranioplasty Strategies for High-Risk Complex Cranial Defects: a 10-Year Experience. Ann Plast Surg. 2021. doi:10.1097/sap.0000000000003019
60. Morton RP, Abecassis IJ, Hanson JF, et al. Predictors of infection after 754 cranioplasty operations and the value of intraoperative cultures for cryopreserved bone flaps. J Neurosurg JNS. 2016;125(3):766–770. doi:10.3171/2015.8.JNS151390
61. Baddour LM, Epstein AE, Erickson CC, et al. Update on Cardiovascular Implantable Electronic Device Infections and Their Management. Circulation. 2010;121(3):458–477. doi:10.1161/CIRCULATIONAHA.109.192665
62. Horberg MA, Hurley LB, Klein DB, et al. Surgical Outcomes in Human Immunodeficiency Virus–Infected Patients in the Era of Highly Active Antiretroviral Therapy. Arch Surg. 2006;141(12):1238–1245. doi:10.1001/archsurg.141.12.1238
63. Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017;152(8):784–791. doi:10.1001/jamasurg.2017.0904
64. Ismael H, Horst M, Farooq M, Jordon J, Patton JH, Rubinfeld IS. Adverse effects of preoperative steroid use on surgical outcomes. Am J Surg. 2011;201(3):305–309. doi:10.1016/j.amjsurg.2010.09.018
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
