Back to Journals » Clinical Epidemiology » Volume 14
Socioeconomic Disparities in Prehospital Emergency Care in a Danish Tax-Financed Healthcare System: Nationwide Cohort Study
Authors Frydenlund J , Mackenhauer J, Christensen EF , Christensen HC, Væggemose U, Steinmetz J , Johnsen SP
Received 24 January 2022
Accepted for publication 13 March 2022
Published 27 April 2022 Volume 2022:14 Pages 555—565
DOI https://doi.org/10.2147/CLEP.S358801
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eyal Cohen
Juliane Frydenlund,1 Julie Mackenhauer,1 Erika F Christensen,2– 4 Helle Collatz Christensen,5 Ulla Væggemose,6,7 Jacob Steinmetz,8,9 Søren Paaske Johnsen1
1Department of Clinical Medicine, Aalborg University, Aalborg East, 9220, Denmark; 2Department of Clinical Medicine, Aalborg University, Aalborg, 9000, Denmark; 3Clinic for Internal and Emergency Medicine, Aalborg University Hospital, Aalborg, 9000, Denmark; 4Emergency Medical Services, North Denmark Region, Aalborg, 9000, Denmark; 5Danish Clinical Quality Program, National Clinical Registries, Copenhagen, Denmark; 6Department of Research & Development, Prehospital Emergency Medical Services, Central Denmark Region, Aarhus, Denmark; 7Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 8Department of Anaesthesia, Centre of Head and Orthopaedics, Rigshospitalet, Copenhagen, Denmark; 9Danish Air Ambulance, Aarhus, Denmark
Correspondence: Juliane Frydenlund, Department of Clinical Medicine, Aalborg University, Fredrik Bajers Vej 5, Aalborg East, 9220, Denmark, Tel +45 24671465, Email [email protected]
Background: Differences related to socioeconomic status (SES) in use of prehospital emergency medical services (EMS) have been reported. However, detailed data on potential disparities in the quality of the EMS according to SES are lacking.
Methods: A nationwide cohort study of medical emergency calls made to the Danish emergency number 1-1-2 in the period 2016– 2017. To measure quality of care, performance indicators from the Danish Quality Registry for Prehospital Emergency Medical Services were used. SES was based on income, education and adherence to workforce. Poisson regression was used to measure relative risk (RR).
Results: We included 388,378 medical 1-1-2 calls, of which 261,771 were unique individuals; 42% of the calls concerned patients with low education, 5% concerned patients living in relative poverty and 23% concerned patients receiving social subsidy. There were no significant differences between the SES regarding time span for arrival of first EMS units. However, patients receiving social subsidy and retired people were more likely to be released at scene and to call again within 24 hours: Adjusted RRs were 2.79 [2.20; 3.54] and 2.08 [1.58; 2.75], respectively, compared with patients having a job. In addition, patients receiving social subsidy and retired people were more likely to call again within 24 hours after receiving telephone advice only: Adjusted RRs 2.35 [1.95; 2.82] and 1.88 [1.51; 2.35], respectively compared with patients having a job. Adjusted RRs for unplanned hospital contact after being treated and released at scene were higher for patients receiving social subsidy and retired people, respectively, relative to patients having a job.
Conclusion: Patients with low SES were significantly more likely to contact the hospital or EMS again after their first call or after treatment and release at scene compared with patients with high SES. This indicates that callers with low SES did not receive the appropriate help.
Keywords: socioeconomic, prehospital, EMS, register study, Denmark
Introduction
A correlation between socioeconomic status (SES) and health is seen by low educated people having a lower life expectancy then high educated people and higher risk of adverse health outcomes.1–4 Besides, studies have indicated barriers in access to the health-care system for people with low SES.5,6 Social inequity of individual health in general is a consequence of multiple determinants and many of these are not dependent on the health-care system, e.g., the societal distribution of wealth and employment policies. In contrast, SES-related differences in medical care are potentially amenable for intervention within the health-care system.
Equal access to emergency care is a key health policy priority across health-care systems. There are studies reporting SES-related differences in use of prehospital emergency medical services (EMS).7,8 However, more detailed data on the potential differences in the quality of the EMS according to SES are lacking.
The aim of the Danish health-care system is to facilitate the health of the entire population. As the health-care system is almost entirely tax-financed and all acute medical care is free of charge, EMS in Denmark should in theory ensure equal access and equal quality of emergency care for all citizens.9 In this way, Denmark should have the optimal conditions for an equal and fair health-care system, where everyone, regardless of socioeconomic position, receives the same treatment based on their symptoms. However, little is known about potential socioeconomic inequity in emergency care, including to which extent tax-financed health-care systems, similar to Denmark, succeed in ensuring equality in the EMS. We therefore performed a nationwide register-based study to compare the quality of prehospital emergency care according to the patients’ socioeconomic background.
The aim of this study was to examine whether there are socioeconomic disparities in the treatment provided by EMS in Denmark.
Materials and Methods
Design and Setting
This was a nationwide cohort study of emergency medical calls made to the national emergency number 1-1-2 in Denmark. Persons with Danish citizenship, approximately 5.7 million inhabitants, and persons with a long-term residence permit in Denmark have free access to the health services as well as partial reimbursement of the costs of prescribed medication.10
The pre-hospital sector is an integrated part of the health-care system. When calling 1-1-2, the call is transferred, depending on which region is responsible for the system, to the Police Alarm Center or the Fire Brigade in Copenhagen. From here, calls about illness or injury are forwarded to the Emergency Medical Communication Centers (EMCC) where the level of urgency of the incident and the main symptom is assessed according to the level of urgency: A, B, C, D, E/F. This assessment is based on the “Danish Index for Emergency Care”.11 Similar indices are also used in the other Nordic countries. The highest priority level is urgency level A, corresponding to an immediate response, while urgency level E corresponds to a situation where the EMCC call-taker assesses ambulance support unnecessary, and chooses not to dispatch an ambulance and maybe gives advice to call a general practitioner. The paramedics can treat and release the patient at scene. The decision to release a patient at scene requires consultation with an EMS physician (either on-site or by telephone). 1-1-2 is the emergency medical call in all European countries and it will be answered, processed and responded to by the appropriate service(s), either medical, security or fire service, etc.12
Selection of Participants
The population contained all medical 1-1-2 calls in the period 2016–2017. Each Danish citizen has a unique 10-digit civil registration number (CPR number) registered in the Population Register. The CPR number is used in all public registers, which makes it possible to link data across all public registers.10 Calls were excluded if the patient did not have a registered CPR number, if the patient had resided in Denmark for less than 10 years, and if a registration error occurred, e.g., if they were registered dead >1 day before the call (Figure 1). Moreover, callers below 35 years of age were excluded because we assume that people below 35 years had not necessarily reached the highest level of education which was necessary in order to measure SES.
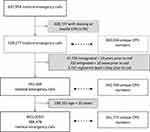 |
Figure 1 Flowchart of included medical 1-1-2 calls and corresponding number of unique patients within each group in Denmark, 2016–2017. |
Performance Indicators
Quality of prehospital care was assessed using seven performance indicators (PI) (Table 1). Five PIs were obtained from the Danish Quality Registry for Prehospital Emergency Medical Services.13 These PIs had been selected by a national multidisciplinary expert group and are concerning arriving time and patients who call again within a short time. The Danish Quality Database for Prehospital Emergency Medical Services is based on information from the regional dispatch software containing individual-level information on dispatch criteria, time stamps for medical emergency call, ambulance dispatch and on-scene times consecutively registered by the EMS or EMCC staff.13 Two additional PIs were defined by the authors, to assess more information on patients’ outcomes.
 |
Table 1 Performance Indicators (PI) Reflecting Quality of Prehospital Emergency Care |
Socioeconomic Status
Socioeconomic status (SES) was assessed according to level of education, income and adherence to the workforce. Data on these variables were obtained from Statistics Denmark, which is an extensive collection of administrative registers, containing individual-level data from governmental agencies.14
Education was defined according to International Standard Classification of Education and the European consensus definitions as low, middle or high.15 Data originated from The Educational Attainment Register,16 which holds information about the highest completed education for all Danish citizens based on the information in The Student Register and The Qualification Register. The primary data source to these statistics is the Student Register with data from 1974 onwards.
Income was grouped as above national median, below national median or poverty (defined as less than 50% of national median). Data came from The Personal Income Statistics,17 which described income for persons who were at least 15 years old at the end of the year and fully liable to pay tax in the year concerned. The income statistics mainly comprise wages and transfers. The captured income amounts on average to 90% of the total gross income.
Adherence to workforce was grouped as: working (including full-time education), age-retirement or social subsidy. If data were not available at the year of emergency call, data from the previous year were used. Adherence to workforce was defined by household level (best in household) for the entire cohort at the year of the emergency call. Data came from the Employment Registry,18 which is an annual labor market statistic based on the population’s adherence to the labor market on the last working day in November.
Co-Variates
Co-variates are factors related to frequent use of emergency health services for people living in high-income countries,8,19 which are also potentially related to socioeconomic position and therefore potential confounding factors. Included covariates were sex, age, cohabitation and comorbidity. Cohabitation was defined as either living alone or with someone else, country of origin (defined as Denmark, other Western countries or non-Western countries), residency (capital, metropolitan, urban, suburban or rural municipalities). Co-morbidity was defined by Charlson Comorbidity Index (CCI) based on diagnoses identified in the Danish National Patient Registry 10 years prior to the emergency call, including substance misuse.20 Grouped as: None (CCI 0), low (CCI 1–2), moderate (CCI 3–4) or high (CCI 5+).
Statistical Methods
We compared the calls on all outcome indicators according to the patients’ education, income and adherence to workforce using the highest possible position as reference (high educational level, above median income and working or education). All estimates included 95% confidence intervals (CI) and medians were reported with inter-quartile ranges (IQR).
For the main analysis we applied robust linear regression based on Huber and biweight iterations to PI-1 and -2 as implemented in the STATA-routine rreg. The purpose of this regression was to limit the effect of serious outliers. Coefficients were calculated as both unadjusted and adjusted for age, sex, cohabitation, area of residency, country of origin and CCI. Additional analyses were done stratified by residency (capital, metropolitan, urban, suburban or rural municipalities) in order to explore possible effect modification by geography.
For PI 3–7, Risk Ratios (RR) were calculated unadjusted, adjusted for sex and age and adjusted for age, sex, cohabitation, area of residency, country of origin and CCI.
To relax the assumption of independence for recurring subjects, we applied the clustered Huber estimator. Patients were included for every contact to the EMCC.
For all adjusted analyses we implemented restricted cubic splines for age with three knots at quantile 0.1, 0.5 and 0.9.
Statistical analyses were performed using Stata 16 (Stata Corporation, College Station, Texas, USA).
Results
In total, we included 388,378 medical 1-1-2 calls regarding 261,771 unique individuals (Figure 1). The median [IQR] number of medical 1-1-2 calls per individual in the two-year period was 1 [1; 3], range (1–223). Of all calls, 42% concerned patients with low education level, 5% concerned patients living in relative poverty and 23% concerned patients receiving social subsidy including early retirement (Table 2). For median time and proportions for each PI see Supplementary Tables 1–3.
 |
Table 2 Characteristics of the Population with Medical 1-1-2 Calls in Denmark 2016–2017 |
There were no significant differences between the socioeconomic groups regarding arrival time of first or supplementary EMS units (PI-1 and -2) among the 203,502 calls resulting in urgency level A-responses. For arrival time of first EMS unit, stratification was made according to residency (capital, metropolitan, urban, suburban or rural municipalities), but virtual no differences across the residency areas were observed. Similar, no major differences were found for the proportion of patients with fulfilled registration of the call-takers assessment according to the specific Danish Index criteria (letter for urgency level and number of Danish Index symptom) according to (PI-3) [Additional file 1].
The highest adjusted RRs were observed for adherence to workforce, where patients receiving social subsidy and retired people were more likely to be released at scene and call again within 24 hours (PI-5): Adjusted RRs were 2.79 [2.20; 3.54] and 2.08 [1.58; 2.75], respectively, when compared with patients having a job. Patients receiving social subsidy and retired people were also more likely to call again within 24 hours after receiving telephone advice only (PI-4): Adjusted RR 2.35 [1.95; 2.82] and 1.88 [1.51; 2.35], respectively compared with patients having a job (Figure 4). Similar patterns for PI-4 and PI-5 were observed for education and income (Figures 2 and 3).
Socioeconomic differences were also observed regarding the likelihood of having an unplanned hospital contact within seven days after release at scene (PI-7). The adjusted RRs were 1.64 [1.50; 1.79] and 1.56 [1.40; 1.74] for patients receiving social subsidy and retired people, respectively, relative to patients having a job, whereas the adjusted RRs were 1.44 [1.28; 1.63] and 1.33 [1.27; 1.40] for patients with an income below the relative poverty line and patients below median income, respectively, relative to patients with an income above median income. No substantial differences in PI-7 were observed in relation to education.
Discussion
In this nationwide study on quality of prehospital EMS, we found that patients with low socioeconomic status as reflected by education, income or adherence to the workforce were more likely to call again within 24 hours after telephone advice only, more likely to call again within 24 hours after being released at scene, and more likely to have an unplanned hospital contact within seven days after being released at scene. In contrast, no differences were found for time span to arrival of the prehospital units on scene or for the registration completeness in relation to socioeconomic status.
We found that a substantial number of the 1-1-2 callers had low SES (Table 2). A previous Danish study, also with data from 2016, found an association between education and likelihood of contacting EMS where low education was associated with greater likelihood of calling 1-1-2.8 In addition, a Canadian study have shown that patients who are frequent users of ambulances have difficulty getting the money to last a month.19 Another Danish study based on data from a medical helpline in the capital, Copenhagen, covering 1.8 million people, found that callers with low income were less often triaged to subsequent face-to-face clinical assessment compared with callers with middle/high SES and the same trend was observed for 30-day mortality.21
Our results indicate that EMCC and EMS personnel do not respond to patients differently in urgent situations (time of 1st and 2nd EMS unit), and similar results have previously been reported in a US study on EMS and SES in patients with stroke.22 This could indicate that unequal treatment may take place in situations of lower urgency, leaving more room and time for interaction between the caller and the call-taker at EMCC and between the patient and the paramedic on scene.
Our finding regarding persons with low SES being more likely to call again or have an unplanned hospital contact within seven days may indicate that the EMCC personnel may be more likely to miss the opportunity to help patients with low SES when they initially seek health care. A possible explanation for this may be, that their health-care needs do not demand an ambulance but rather the out-of-hours health-care services or general practitioner. Due to a low SES it seems that these patients lack the ability to request the appropriate medical help required in their situation. Another explanation could be, that people with low SES are more ill,23 but even though this may be a fact, patients with low SES may still be challenged by how to get proper treatment in their situation.
A study finds an association of low SES and contacting a health-care service outside office hours and contacting EMS rather than out-of-hours primary care.8 Health literacy is likely to play an important role in the interaction that takes place between the EMCC and the patient calling 1-1-2, because the patient’s way of communicating and understanding health-relevant information may impact the treatment he or she receives. If the patient is not able to explain the symptoms correctly or if the patient does not understand in which situations emergency help is required, then this may lower the chance of receiving adequate help. SES is related to the level of health literacy 24–26 and a systematic review on health literacy and emergency care concluded that a substantial proportion of patients in emergency care have limited health literacy and that the information provided to the patients are not properly adjusted in relation to the target group.27 The higher proportion of patients with low health literacy requiring repeated contacts with the emergency care system may reflect that they did not have a similar opportunity (or at least did not conceive that they had an equal opportunity) to seek help from a general practitioner or other health services.
Perspectives
Research has been done in various areas of health on how patients’ socioeconomic differences can have an impact on the treatment they receive at the hospital.9 The meeting between patients with different social backgrounds and the health service can thus be characterized by communicative challenges. The modern health-care system is an efficient and streamlined organization whose function presupposes that patients participate and communicate, relate to information and actively choose between offers. It is well known that communication between different social groups can reflect different experiences, cultures and understandings, which can make communication difficult. A report from the Danish National Board of Health 2011 clarifies reasons and efforts in inequality in health in Denmark. The report tells that the interaction between user and health service is seen as a negotiation, where the user presents his previous experiences, expectations and knowledge about the disease and treatments and the treatment will depend on patients’ education, social status, language skills, etc. On the other hand, there is the health-care system, which is built around an ideal patient who understands the health-care system and the rights that a patient has.28 In reflection of this the construction of the health-care system should be reconsidered on the basis of persons with low SES in order to make sure they know where to go with symptoms that should not be treated by EMS.
Limitations
Limitations should be taken into consideration, when interpreting the study findings. Using the PIs from The Danish Quality Registries for Prehospital Emergency Medical Services we only assessed some aspects of the quality of the emergency medical system, e.g., it was not possible to include a patient perspective, and there were no data concerning the severity of the patients’ acute condition.
We only included patients above 35 years because we assume at this age patients have reached their highest level of education. Hence, the results cannot be extrapolated to younger persons. This was necessary, because we considered SES as a proxy for resources of the individual and ascertain, that the study population were represented by their highest level of education. Still there can be some cases where callers have not yet completed their education, although at age 35 most would have obtained a final education level. Data from the EMCC were incomplete, with 17% of calls not providing a valid CPR number of the 1-1-2 patient. A missing CPR number was more common, if only telephone advice was given, and in cases with lower acuity. There are several other reasons why the CPR number may be missing. This could be due to calls made by a bystander, who does not know the CPR number of the 1-1-2 patient who needs help. However, if an ambulance is dispatched or if the patient is admitted to hospital, the EMS personnel will update the chart with a CPR number, if the patient is identified. Also, if several calls are made regarding the same episode (e.g., traffic accidents), the CPR number may only be registered for one of these calls, which may also explain the high number of contacts with missing information. We cannot exclude the possibility of a SES related selection bias, i.e., a higher proportion of patients with low SES among patients without a recorded CPR number, however, it is not possible to verify this.
Conclusion
No major difference in time of arrival of EMS units in relation to SES was observed in this nationwide population-based study in a tax-financed health-care system, but patients with low SES who called EMS contacted the hospital again after their initial call more often, compared with patients with high SES. This indicate that callers with low SES did not receive the appropriate help according to their symptoms, which possibly should be treated in the health-care system, but not necessarily by the EMS.
Abbreviations
SES, socioeconomic status; EMS, Emergency Medical Services; RR, relative risk; EMCC, Emergency Medical Communication Centers; CCI, Charlson Comorbidity Index; CI, confidence interval; IQR, inter-quartile ranges; PI, performance indicator.
Ethics Approval and Consent to Participate
The study was approved by the Danish Data Protection Agency. According to Danish law, ethical committee approval is not required for registry-based studies.
Data Sharing Statement
The data are available from Statistics Denmark, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Statistics Denmark.
Acknowledgments
Not applicable.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Publication cost were funded by the Karen Elise Jensen Foundation, Aase og Ejnar Danielsens Fond, Gangstedfonden, and Psychiatry in North Denmark Region who had no role in the design, data collection, analysis or writing of this manuscript.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Kinge JM, Modalsli JH, Øverland S, et al. Association of household income with life expectancy and cause-specific mortality in Norway, 2005-2015. JAMA - J Am Med Assoc. 2019;321(19):1916–1925. doi:10.1001/jama.2019.4329
2. Lallo C, Raitano M. Life expectancy inequalities in the elderly by socioeconomic status: evidence from Italy. Popul Health Metr. 2018;16(1):1–21. doi:10.1186/s12963-018-0163-7
3. Brønnum-Hansen H, Baadsgaard M. Widening social inequality in life expectancy in Denmark. A register-based study on social composition and mortality trends for the Danish population. BMC Public Health. 2012;12(1):1-7.
4. Diderichsen F, Andersen I, Manuel C. et al. Health inequality - determinants and policies. Scand J Public Health. 2012;40(Suppl 8):12–105. doi:10.1177/1403494812457734
5. Edwards NM, Varnum C, Overgaard S, Pedersen AB. The impact of socioeconomic status on the utilization of total hip arthroplasty during 1995–2017: 104,055 THA cases and 520,275 population controls from national databases in Denmark. Acta Orthop. 2020;92(1):29–35. doi:10.1080/17453674.2020.1840111
6. Teunter RH, Duncan L. Socioeconomic status, access to health care, and outcomes after acute myocardial infarction in Canada’s universal health care system. Acad Manag Rev. 2007;45:638–646.
7. Kawakami C, Ohshige K, Kubota K, Tochikubo O. Influence of socioeconomic factors on medically unnecessary ambulance calls. BMC Health Serv Res. 2007;7:1–9. doi:10.1186/1472-6963-7-120
8. Søvsø MB, Bech BH, Christensen HC, Huibers L, Christensen EF, Christensen MB. Sociodemographic characteristics associated with contacts to emergency medical services and out-of-hours primary care: an observational study of 2.3 million citizens. Clin Epidemiol. 2020;12:393–401.
9. Lindskou TA, Mikkelsen S, Christensen EF, et al. The Danish prehospital emergency healthcare system and research possibilities. scandinavian journal of trauma, resuscitation and emergency medicine. BioMed. 2019;271–7.
10. Mainz J, Hess MH, Johnsen SP. The Danish unique personal identifier and the Danish civil registration system as a tool for research and quality improvement. Int J Qual Health Care. 2019;31:717–720. doi:10.1093/intqhc/mzz008
11. Andersen MS, Johnsen SP, Sørensen JN, Jepsen SB, Hansen JB, Christensen EF. Implementing a nationwide criteria-based emergency medical dispatch system: a register-based follow-up study. Scand J Trauma Resusc Emerg Med. 2013;21(1):1–8. doi:10.1186/1757-7241-21-53
12. World Health Organization. Emergency medical services systems in the European Union report of an assessment project co-ordinated by the World Health Organization. World Health Organization; 2008.;
13. Christensen EF, Berlac PA, Nielsen H, Christiansen CF. The Danish quality database for prehospital emergency medical services. Clin Epidemiol. 2016;8:667–671. doi:10.2147/CLEP.S100919
14. Statistic Denmark. [Homepage on the internet].Subjects. Available from: https://www.dst.dk/en.
15. UNESCO. International Standard Classification of Education. 2017;(912):1–5. Available from: http://www.uis.unesco.org.
16. Statistics Denmark. Documentation of statistics for the student register 2015; 2015.
17. Denmark S Documentation of statistics for Income Statistics 2019; 2019.
18. Statistics Denmark. Documentation of statistics for register-based labour force statistics 2015 statistics. Stat Denmark [Internet]; 2017:1–20. Available from: https://www.dst.dk/en/Statistik/dokumentation/documentationofstatistics/productivity.
19. Agarwal G, Lee J, McLeod B, et al. Social factors in frequent callers: a description of isolation, poverty and quality of life in those calling emergency medical services frequently. BMC Public Health. 2019;19(1). doi:10.1186/s12889-019-6964-1
20. Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi:10.1016/0021-9681(87)90171-8
21. Gamst-Jensen H, Jensen AN, Christensen EF, et al. Socioeconomic inequality in telephone triage on triage response, hospitalization and 30-day mortality. Eur J Public Health. 2021;31(i):1–3. doi:10.1093/eurpub/ckaa231
22. Kleindorfer DO, Lindsell CJ, Broderick JP, et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: do poorer patients have longer delays from 911 call to the emergency department? Stroke. 2006;37(6):1508–1513. doi:10.1161/01.STR.0000222933.94460.dd
23. Pathirana TI, Jackson CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. 2018;42(2):186–194. doi:10.1111/1753-6405.12762
24. Friis K, Lasgaard M, Osborne RH, Maindal HT. Gaps in understanding health and engagement with healthcare providers across common long-term conditions: a population survey of health literacy in 29 473 Danish citizens. BMJ Open. 2016;6:e009627. doi:10.1136/bmjopen-2015-009627
25. Lastrucci V, Lorini C, Caini S, et al. Health literacy as a mediator of the relationship between socioeconomic status and health: a cross-sectional study in a population-based sample in florence. PLoS One. 2019;14(12):e0227007. doi:10.1371/journal.pone.0227007
26. Stormacq C, Van Den Broucke S, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot Int. 2019;34(5):E1–17. doi:10.1093/heapro/day062
27. Herndon JB, Chaney M, Carden D. Health literacy and emergency department outcomes: a systematic review. Ann Emerg Med. 2011;57:334–345. doi:10.1016/j.annemergmed.2010.08.035
28. Sundhedsstyrelsen. Social ulighed i sundhed og sygdom 2010-2017; 2020;1–263.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



