Back to Journals » International Journal of General Medicine » Volume 16
Sociodemographic Factors Related to Adverse Donor Reactions in Shenzhen
Authors Sun LY , Yu Q, He CM, Wang SX
Received 8 October 2023
Accepted for publication 17 November 2023
Published 23 November 2023 Volume 2023:16 Pages 5493—5499
DOI https://doi.org/10.2147/IJGM.S443682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandul Yasobant
Li-Yan Sun,1 Qiong Yu,2 Cai-Ming He,2 Song-Xing Wang3
1Institution of Transfusion Medicine, Shenzhen Blood Center, Shenzhen, People’s Republic of China; 2Quality Control Department, Shenzhen Blood Center, Shenzhen, People’s Republic of China; 3Business Management Department, Shenzhen Blood Center, Shenzhen, People’s Republic of China
Correspondence: Song-Xing Wang, Email [email protected]
Background: The adverse donor reaction (ADR) means the uncomfortable feeling felt by blood donors during the whole process of blood donation, which can affect the blood donation behavior of blood donors. So, it is very necessary for blood centers to monitor and prevent it.
Methods: Data about ADRs in Shenzhen Blood Center from January 2018 to December 2022 were collected, and correlation analysis was conducted using SPSS 24.0 software.
Results: From January 2018 to December 2022, a total of 1265 ADRs occurred in 642,767 blood donations in Shenzhen Blood Center, with an incidence of 0.20%. Most of the ADRs were mild and occurred during blood collections (> 90%). The ADR rate of young individuals aged 18– 29 years old was the highest (p< 0.0001). In addition, a higher ADR rate was observed in first-time blood donors, whole blood donors, and blood donors who donated in the mobile sites (p< 0.05).
Conclusion: The occurrence of ADRs is related to the sociodemographic factors of blood donors, including age, donation type, donation history, and donation sites. Shenzhen Blood Centers should pay special attention to the process of blood donation among young blood donors aged 18– 29 years old, first-time blood donors, whole-blood donors, and blood donors who donate at mobile sites to further reduce the occurrence of ADRs.
Keywords: blood donors, adverse donor reactions, sociodemographic factors
Introduction
Blood donation is considered a simple and safe procedure. In general, blood donors do not experience adverse symptoms and tolerate the donation process. Adverse reactions can occasionally occur when a donor donates whole blood or blood components. Blood donors can feel uncomfortable, including dizziness, nausea, vomiting, even syncope, and incontinence. The incidence of ADRs can lead to the termination of the donation procedure, even to reduce the return rates for a subsequent donation among whole blood donors and apheresis donors.1,2 Reducing ADRs is detrimental to the retention of blood donors and the provision of adequate blood supply. Therefore, it is very necessary to investigate the factors affecting the occurrence of ADRs and eliminate or reduce these factors by preventive means.
The standard for Surveillance of complications Related to Blood Donation was published in 2008 by the International Society of Blood Transfusion and the International Haemovigilance Network. It was revised in 2014 by the Alliance of Blood Operators, the European Blood Alliance, and the Association for the Advancement of Blood and Biotherapies, which provided the classification criteria of the ADRs.3 Since then, many countries have begun to pay attention to the ADRs.4
In 2017, the National Health and Family Planning Commission of the People’s Republic of China issued the Guidelines on the Classification of Blood Donation Adverse Reaction (WS/T551-2017), which specified the classification, severity assessment, and relevance of ADRs during blood donation. Blood centers in different regions of China have started monitoring ADRs in accordance with national standards and reported their incidence and limited studies of ADRs in China have been reported.5
The purpose of this study was to investigate the incidence and associated factors of ADRs in Shenzhen of China. This was fulfilled by observing ADRs in the process of blood collection and analyzing the characteristics of blood donors.
Methods
According to the guidelines for the classification of ADRs, we divided ADRs into three categories as follows. Mild ADRs are characterized by pallor, sweating, anxiety, vertigo, yawning, nausea, etc. Moderate ADRs are characterized by hypotension, vomiting, and transient loss of consciousness. Severe ADRs include syncope, convulsions, incontinence, etc.
From January 2018 to December 2022, there were 642,767 data about donations in Shenzhen Blood Center were recorded. When a blood donor experienced an ADR, the staff of Shenzhen Blood Center filled in the corresponding position of the “Shenzhen Blood Donation Registration Form” and enters the details in the modern blood station management information system (Tangshan Qiao Technology Co., Ltd, China).
SPSS 24.0 statistical software was used to analyze the data. The statistical data was shown as rate (%) and the Chi-square test was used. p<0.05 was considered statistically significant.
Results
From January 2018 to December 2022, there were 642,767 donations from 269,120 first-time blood donors and 199,129 repeat blood donors in Shenzhen Blood Center, which consisted of 514,944 whole blood donations and 127,823 platelet donations. Among these, 191,216 donations were collected from mobile blood donation sites and 451,471 donations were collected from fixed blood donation sites. In Table 1, only 1265 number of ADRs experienced by blood donors was recorded. The total rate of ADRs among first-time blood donors was higher than that of repeat blood donors, whole blood donors than apheresis donors, male blood donors than female blood donors, young blood donors aged 18–29 years old than the other three groups, and blood donors who donated at mobile sites than fixed sites (p<0.0001). Most of the ADRs occurred during the process of blood collection in Figure 1.
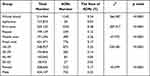 |
Table 1 The Total Rate of ADRs Among Donors |
 |
Figure 1 The proportion of ADRs during and after blood collection. |
In Figure 2, the highest number of donations was observed in 2022, but the highest rate of ADRs was observed in 2018. The increasing number of donations and the decreasing trend of the rate of total ADRs were observed, and there was a significant difference in the rate of total ADRs between each year (p<0.05). Among 1265 ADRs, most of them were mild ADRs, and the decreasing trend of mild ADRs was observed from 2018 to 2022 in Table 2 (p<0.05).
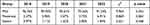 |
Table 2 The Proportion of ADRs in Different Degrees |
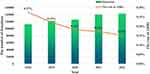 |
Figure 2 The number of donations and the rate of total ADRs in Shenzhen from 2018 to 2022. |
Regarding the sociodemographic aspects of blood donors in Table 3, the rate of ADRs among females and males varied differently each year (p<0.01). The annual rate of females was higher than that of males, although the difference in the rate of ADRs between males and females in 2020 was not statistically significant (p>0.05). From 2018 to 2022, the ADR rate of males decreased significantly (p<0.001). As for the effect of age, the rate of ADRs among blood donors aged 18–29 years old was highest compared to the other three groups (p<0.0001), and only the rate of ADRs among blood donors aged 18–29 years old varied significantly differently each year (p<0.0001). In the group of blood donors with different donation histories, the ADR rate among first-time blood donors was higher than that among repeat blood donors each year (p<0.0001), and the decreasing trend of ADR rate was observed among first-time blood donors from 2018 to 2022 (p<0.0001).
 |
Table 3 The Rate of ADRs Among Different Donors from 2018 to 2022 |
In addition, the occurrence of ADRs was related to the donation sites and the type of blood donation. In Table 3, we found that the incidence of ADRs in fixed blood donation sites was significantly lower than that in mobile blood donation sites (p<0.05), and the ADR rate in the mobile blood donation sites decreased year by year (p<0.05). As for the type of blood donation, the rate of ADRs among whole blood donors was significantly higher than that in apheresis donors (p<0.0001), and there was no significant difference in the rate of ADRs among apheresis donors in these five years (p>0.05).
Discussion
Some blood donors may experience ADRs before, during, and after donating blood. In our study, we only found the ADRs during and after donating blood, and most of these occurred during the process of blood collecting. In the process of blood collection, the occurrence of ADRs will lead to the termination of blood collection, which is a huge loss for the blood center, including the cost of consumables, labor, and blood donors. After blood collection, the occurrence of ADRs will reduce the willingness of blood donors to donate blood again, which is unfavorable to the recruitment of blood donors. Therefore, it is necessary to reduce the incidence of ADRs, especially for the severe ADRs.
The degree of ADRs is not consistent among different individuals. Although the majority of blood donors with ADRs are characterized by mild symptoms, a few blood donors have serious ADRs. In our study, the rate of severe ADRs was 0.003%, which was lower than it was in French (0.15%).6 Among the severe ADRs, we found that more than half of severe ADRs (55%) occurred after blood donation, and 5 of them suffered a fall injury due to dizziness. Therefore, the staff must introduce some information about the ADRs to blood donors, which may help blood donors take measures to prevent and avoid unnecessary injury due to the ADRs. In addition, the duration of ADRs among most blood donors (99.6%) who experienced ADRs was less than 10 minutes. So, the observation time after blood donation allows the staff to take professional measures to deal with the ADRs, thereby avoiding the occurrence of moderate or even severe ADRs.
In several reports, the ADR is considered to be related to a variety of factors. Among these factors, the gender and the age of blood donors are the most widely studied. The higher rates of ADRs were observed among young individuals (aged 18–29 years old) in most countries, such as Bosnia and Herzegovina and Pakistan.7,8 In our study, blood donors aged 18–29 years old are more likely to have ADRs, which is consistent with some research. In terms of gender, many studies have shown that female donors have a higher probability of ADRs.9–11 But in our study, the rate of ADRs among females is higher than among males except for 2020, which may be affected by COVID-19. Based on this, we can not confirm that the ADRs in Shenzhen are related to gender. Compared to females, the incidence of ADRs in males decreased significantly from 2018 to 2020 (p<0.01), and the decreasing rate of ADRs among males can facilitate the retention of male blood donors.
In addition, the donation sites and donation type were also related to the occurrence of ADRs.12–15 Some researchers reported that ADRs occur more often when donating blood in well-medicalized donation centers compared to mobile donation sites.14,15 But in our study, we found that the ADRs occurred more often when donating blood in the mobile sites compared to the fixed sites. It may be associated with the donation type of blood donors. In Shenzhen, apheresis blood components can only be collected at fixed blood donation sites, while whole blood can be collected at mobile donation sites. In our study, the blood donors in Shenzhen who donated whole blood were easier to have the ADRs than apheresis donors, which is contrary to the conclusions of other researchers.12,13 It could be for a variety of reasons. One may be that the number of apheresis donors in our study is smaller than that of whole-blood donors. Another may be that in Shenzhen Blood Center, all apheresis blood donors are repeat donors, but most of the whole blood donors are first-time donors. Our results showed that the rate of ADRs among repeat blood donors was lower than that among first-time blood donors in Shenzhen (0.12% vs 0.38%), which was also observed in other countries.16 Therefore, taking measures to prevent the occurrence of ADRs in first-time blood donors may be one of the important ways to reduce the incidence of ADRs.
As we all know, the rate of ADRs is different from one country to another. It may be related to sample size and population differences. In Asia, India was the country with the most research done about ADRs. The latest report showed that the overall ADR rate in India was 0.24%.17 In our study, the overall ADR rate in Shenzhen of China was 0.20%, which was lower than it was in India. The reason for the lower ADR rate in Shenzhen may be that the staff of Shenzhen Blood Center is not sensitive to the ADRs, or the awareness of blood donors to the ADRs is insufficient, which leads to the failure to register some ADRs. Therefore, the staff in Shenzhen Blood Center must know the performance of ADRs. Then the staff should popularize the ADRs that may occur in the process of blood collection to blood donors so that the ADRs can be reported to the staff promptly. In addition, the staff should timely register the occurrence of ADRs to avoid loss of information.
In order to prevent the decrease of the ADR rate caused by the neglect of the staff and blood donors, Shenzhen Blood Center has taken some measures. The application of a monitoring and warning system for ADRs can monitor the situation of blood donors in the process of blood donation in real-time through the linkage with the intelligent blood collection system. When it detects the ADRs of blood donors, it can immediately feedback on the situation to the staff, to help the staff effectively record and deal with the ADRs.
In fact, Shenzhen Blood Center has been working to reduce the incidence of ADRs by improving services and the environment for blood donation. It includes giving donors appropriate sugar water to drink before donating blood. If the blood donor feels uncomfortable during the blood donation process, the staff will immediately stop blood collection, and press acupoints to relieve the symptoms of the blood donor, as well as follow-up reports. As for improving the environment, Shenzhen Blood Center completes the renovation or construction of a blood donation site every year, which greatly optimizes the blood donation environment and improves the experience of blood donors. Whether these measures are effective is worth further investigation.
Conclusion
In conclusion, from 2018 to 2022, the overall rate of ADRs was low in Shenzhen of China, and most of the ADRs were mild and occurred during blood collections. Young individuals aged 18–29 years old, first-time blood donors, whole blood donors, and blood donors in mobile donation sites were easier to have the ADRs. All the results indicate that donating blood is a relatively safe process in Shenzhen. To further reduce the rate of ADRs in Shenzhen, Shenzhen Blood Center should pay attention to the process of blood donation in the above individuals who are prone to ADRs.
Data Sharing Statement
All data generated or analysed during this study were included in this published article, and all data can be available from upon request and obtained from the corresponding author.
Ethics Approval
This study complies with the Declaration of Helsinki and was approved by the Medical Ethics Committee of Shenzhen Blood Center. The informed consent was obtained from all subjects, and all methods were carried out in accordance with relevant guidelines and regulations.
Acknowledgments
We wish to acknowledge the Medical Ethics Committee of Shenzhen Blood Center for reviewing and approving all the procedures involved in this study. Special thanks to the staff of Tangshan Qiao Technology Co., Ltd. for helping us collect data. We also take this opportunity to thank all members of this project, for their commitment and contribution during the performance of this study. All authors thank the Shenzhen Blood Center for the permission to publish the finding.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was financially supported by National Natural Science Foundation of China (No. 82261138630), Shenzhen Key Discipline Project of Blood Transfusion Medicine (No. SZXK070), Research project of Shenzhen Blood Center (No. SZBC202210).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Newman BH, Newman DT, Ahmad R, et al. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46(8):1374–1379. doi:10.1111/j.1537-2995.2006.00905.x
2. de Farias CLG, Bassolli L, Mendrone-Junior A, et al. The impact of immediate adverse donation reactions on the return of volunteers undergoing platelet apheresis. Transfus Apher Sci. 2022;61(4):103424. doi:10.1016/j.transci.2022.103424
3. International Society of Blood Transfusion Working Party on Haemovigilance. Standard for surveillance of complications related to blood donation; 2014. Available from: http://www.aabb.org/research/hemovigilance/DocumentStandard-for-Surveillance-of-Complications-Related-to-Blood-Donation.
4. Taheri Soodejani M, Haghdoost AA, Okhovati M, et al. Incidence of adverse reaction in blood donation: a systematic review. Am J Blood Res. 2020;10(5):145–150.
5. Yang J, Fan D, Xie D, et al. First donor haemovigilance system at a national level in China: establishment and improvement. Vox Sang. 2023;118(5):357–366. doi:10.1111/vox.13421
6. Riga A, Sapey T, Bacanu M, et al. Blood donors--Serious adverse reactions (SAR) 2010–2014 EFS Châteauroux, France. Transfus Clin Biol. 2015;22(2):62–65. doi:10.1016/j.tracli.2015.04.002
7. Sultan S, Baig MA, Irfan SM, et al. Adverse reactions in allogeneic blood donors: a tertiary care experience from a developing country. Oman Med J. 2016;31(2):124–128. doi:10.5001/omj.2016.24
8. Smajic SC, Becarevic M, Klapic S, et al. Adverse reactions and complication in voluntary blood donors. Mater Sociomed. 2023;35(2):92–96. doi:10.5455/msm.2023.35.92-96
9. Ibrahim N, Mohd Noor N, Zulkafli Z. Prevalence and factors associated with vasovagal reaction among whole blood donors in hospital Universiti Sains Malaysia. Transfus Clin Biol. 2023;30(2):238–243. doi:10.1016/j.tracli.2023.01.004
10. Radovčić MK, Ljubičić J, Očić T, et al. Blood collection failures from a blood establishment perspective. Transfus Med. 2021;31(2):88–93. doi:10.1111/tme.12762
11. Prakash S, Das PK, Mishra D, et al. Incidence and risk predictors analysis of adverse donor reactions in whole blood donation. Transfus Clin Biol. 2020;27(4):207–212. doi:10.1016/j.tracli.2020.09.003
12. Burkhardt T, Dimanski B, Karl R, et al. Donor vigilance data of a blood transfusion service: a multicenter analysis. Transfus Apher Sci. 2015;53(2):180–184. doi:10.1016/j.transci.2015.03.014
13. Piccinini V, Marano G, Catalano L, et al. Vasovagal reactions in whole blood and apheresis donors: a cross-sectional study on donor haemovigilance data from 2016 to 2019 in Italy. Blood Transfus. 2022;20(4):281–291. doi:10.2450/2021.0114-21
14. Donald SJ, McIntyre WF, Dingwall O, Hiebert B, Ponnampalam A, Seifer CM. Is donating blood for the faint of heart? A systematic review of predictors of syncope in whole blood donors. Transfusion. 2019;59(9):2865–2869. doi:10.1111/trf.15442
15. Wei WH, Smith M, Vera A, et al. Novel risk patterns of vasovagal reactions in NZ blood donations complicated by COVID-19 restrictions. Front Public Health. 2023;11:1180279. doi:10.3389/fpubh.2023.1180279
16. Brunson DC, Belanger GA, Sussmann H, et al. Factors associated with first-time and repeat blood donation: adverse reactions and effects on donor behavior. Transfusion. 2022;62(6):1269–1279. doi:10.1111/trf.16893
17. Bisht A, Marwaha N, Arora S, et al. National blood donor vigilance programme of India: analysis of donor adverse reactions reported during initial 2 years of implementation (2016 and 2017). Asian J Transfus Sci. 2021;15(1):1–11. doi:10.4103/ajts.ajts_195_20
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
