Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Social Support, Food Insecurity, and HIV Stigma Among Men Living with HIV in Rural Southwestern Uganda: A Cross-Sectional Analysis
Authors Arinaitwe I , Amutuhaire H, Atwongyeire D, Tusingwire E , Kawungezi PC, Rukundo GZ , Ashaba S
Received 16 April 2021
Accepted for publication 28 May 2021
Published 16 June 2021 Volume 2021:13 Pages 657—666
DOI https://doi.org/10.2147/HIV.S316174
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Innocent Arinaitwe,1 Hildah Amutuhaire,1 Davis Atwongyeire,1 Esther Tusingwire,1 Peter Chris Kawungezi,2 Godfrey Zari Rukundo,3 Scholastic Ashaba3
1Faculty of Medicine, Mbarara University of Science and Technology, Mbarara, Uganda; 2Department of Community Health, Mbarara University of Science and Technology, Mbarara, Uganda; 3Department of Psychiatry, Mbarara University of Science and Technology, Mbarara, Uganda
Correspondence: Scholastic Ashaba
Department of Psychiatry, Mbarara University of Science and Technology, Mbarara, Uganda
Email [email protected]
Background: HIV stigma is one of the major barriers to HIV care due to the fear of disclosure and social discrimination. HIV stigma among men in sub-Saharan countries, including Uganda, has been linked to the fear about how HIV status might affect their status in society. HIV among men in sub-Saharan settings has been associated with feelings of shame, reduced self-worth, and self-blame for their HIV positive status. Information about HIV stigma and its associated factors among men living with HIV in rural Uganda is limited. This study assessed the burden of HIV stigma and its association with social support and food insecurity among men accessing HIV care at a rural health facility in southwestern Uganda.
Methods: We conducted a clinic-based cross-sectional study and consecutively enrolled 252 adult men accessing HIV care at a rural health centre in southwestern Uganda. We collected information on sociodemographic information, HIV stigma, social support, and food insecurity. We fitted modified Poisson regression models to determine the associations between social support, food insecurity, and HIV stigma.
Results: The mean HIV stigma score of the study participants was 70.08 (SD 19.34) and 75% reported food insecurity 5% of whom were severely food insecure. The risk of HIV stigma was lower among those aged 35 years and above (adjusted risk ratio [ARR]=0.89; 95% CI 0.83– 0.96; P=0.003, those who had been on ART for more than 5 years (ARR=0.92; 95% CI=0.84– 0.99; P=0.04), and those who had social support (ARR=0.99; 95% CI=0.98– 0.99; P=< 0.001). Food insecurity was associated with an increased risk of HIV stigma (ARR=1.07; 95% CI 1.00– 1.15; P=0.03). Social support moderated the effect of food insecurity on HIV stigma (P=0.45).
Conclusion: Stigma is common among men living with HIV in rural Uganda and is significantly associated with food insecurity. Social support moderated the effect of severe food insecurity on HIV stigma among men living with HIV. Interventions to build social support systems and to economically empower men living with HIV should be incorporated into the mainstream HIV care clinics.
Keywords: HIV positive men, HIV-related stigma, social support, food insecurity, rural Uganda, sub-Saharan Africa
Introduction
Stigma is a process through which individuals are discredited and discounted by labeling, stereotyping and discrimination based on an undesirable characteristic that they possess.1,2 This process impacts individuals at interpersonal and structural levels and diminishes their opportunities in life.2,3 Stigma is a major challenge in the context of HIV manifesting in the form of negative attitudes by the public towards those affected as well as through negative experiences by those living with HIV.4–6 There are different HIV stigma mechanisms including enacted stigma, internalized stigma, and anticipated stigma.7 Internalized HIV stigma occurs when a person accepts and endorses negative stereotypes and beliefs about HIV or people living with HIV as true and applicable to their own life.7,8 Enacted stigma refers to the discriminatory experiences of the people living with HIV that may manifest in the form of violence and marginalization, while anticipated stigma is the awareness of the negative perceptions about HIV and the expectation that people living with HIV will be discriminated against based on their HIV status.8–10 HIV stigma is one of the major barriers to HIV care due to the fear of disclosure and social discrimination.11 HIV stigma is associated with delays in enrollment and retention in care12–15 and complicates mental health outcomes including depression and suicidality.13,15,16 HIV testing among adults in Uganda has been reported to be dependent on the extent to which individuals anticipate experiencing HIV stigma if they test positive for HIV.17
Studies done in India and Swaziland have documented that men and women experience HIV stigma differently with men experiencing more of internalized stigma compared to women who commonly experience enacted stigma.18–20 Findings from a study in South Africa showed that men reported more perceived HIV stigma than women.21 There is a correlation between HIV status disclosure and perceived HIV stigma whereby HIV status disclosure may lead to HIV stigma but also perceived HIV stigma may prevent people from disclosing their HIV status.22,23 A study in Ethiopia reported that perceived HIV was more prevalent in rural than urban areas.24
Gender norms related to notions of masculinity fuel HIV stigma experiences among men living with HIV in sub-Saharan Africa.25–28 Cultural beliefs in most African settings uphold men in high esteem, suggesting that involvement in HIV care by men would be seen as a sign of weakness against concepts of masculinity synonymous with self-confidence, resilience, and endurance.29,30 HIV among men in South Africa and Swaziland was associated with feelings of shame, reduced self-worth, and self-blame for their HIV positive status.15,20 Additionally, men fear that their HIV status might affect their status in society in relation to respectability, independence, risk taking and emotional control as indicated in studies in Uganda and South Africa.28,31,32 Men believe that HIV testing would interfere with their employment opportunities and hence compromise their ability to provide for their families if found HIV positive.15,28 Men are also reluctant to test for HIV to avoid being blamed for spreading HIV due to their HIV risk sexual behavior and the associated stigma.33–36 As documented by a study in Uganda, perceived HIV stigma among Ugandan men originates from the fear of loss of dignity and status in society due to the association of HIV with promiscuity, being irresponsible, untrustworthy and those living with HIV are often deemed to be dangerous to society.37 Men being the heads of households with a role as providers are more vulnerable to internalized HIV stigma and discrimination at society level.33,38
Previous research in Uganda and Nigeria indicated that men are less likely to take up HIV services, including voluntary counseling and testing and initiation on ART,39,40 are less adherent to antiretroviral therapy (ART) and less virally suppressed compared with women.21,41,42 In Uganda, fewer men are enrolled in care and fewer are adherent to ART with higher HIV-related mortality reported among men compared with women.35,43 HIV-related mortality among men has also been reported to be higher in rural areas than in urban areas.44 Adherence to ART among men in Uganda is reportedly poor due to the fear of rejection,35 while others fear that the side effects of ART or being seen taking HIV medicine may result in community gossip leading to loss of respect and dignity in society.37 Enduring physical symptoms and delays in seeking care was viewed as a sign of strength among men living with HIV in Uganda.35
Factors associated with HIV stigma among adults with HIV include low level of education, symptomatic HIV/AIDS, and lack of HIV status disclosure.45,46 According to the Uganda demographic and health survey,47 few people attain secondary education whereby the majority of those who are enrolled in school dropout at primary level. On average, the median years of schooling in Uganda for men is 3.9 years and 3. 4 years for women.47 Other factors associated with HIV stigma, especially in sub-Saharan Africa, include religion and age,48 as well as having an HIV positive partner.49 Studies on the association between duration of ART and HIV stigma have found mixed findings.48,50 Social support has been associated with reduced HIV stigma among adults living with HIV in Uganda.51,52 Additionally, studies in Uganda have documented a significant association between food insecurity and HIV stigma among adults living with HIV.53,54
Food insecurity is when people are not able to access sufficiently safe and nutritious food for normal growth and development and for an active and healthy life.55 Because food is a social determinant of health,56 food insecurity is associated with poor health outcomes in both the short and long terms.57,58 Uganda is one of the countries with high levels of food insecurity in Sub-Saharan Africa.59,60 A previous population-based study in Uganda reported a prevalence of food insecurity of 25% among women and 9% among men.61 Moreover, 31% of the Ugandan population are absolutely poor, yet poverty and food insecurity have a strong correlation.60 Some of the factors associated with food insecurity in Uganda include limited access to agricultural technology, poverty, dependence on rainy seasons which are no longer sustainable due to climate change and morbidity associated with chronic illnesses.54,62–64 The relationship between HIV stigma and food insecurity has been linked to social distance and reduced involvement in social activities that come when people test positive for HIV, which impacts the ability to access tangible support, paid labor, and cash loans that would enable them to access food.53,65,66 Additionally, HIV is associated with morbidity which affects the ability of adults living with HIV to work on their farms or engage in other economic activities which leads to food insecurity at household level.67,68
Although it has been documented that perceived HIV stigma is a major barrier to enrollment in HIV care and that perceived HIV stigma is more prevalent in rural settings,17,24 information about HIV stigma among men living with HIV in rural south-western Uganda is sparse. Despite literature indicating high levels of food insecurity in Ugandan communities,60,61 the relationship between social support, food insecurity, and HIV stigma among men living with HIV in rural southwestern Uganda is not well understood. This study aimed at understanding HIV stigma and its relationship with social support and food insecurity among men living with HIV in rural southwestern Uganda.
Materials and Methods
Study Setting and Design
This was an observational cross-sectional study to determine the prevalence of HIV stigma and the associated factors among HIV positive men attending an HIV clinic in a rural health facility in southwestern Uganda. The study was conducted at Ruhoko Health Centre IV (RHC IV), in Ibanda District. RHC IV is located about 300 km from Kampala, the Ugandan capital city. The health facility has about 2656 people enrolled for HIV care of whom 832 are adult men. The HIV clinic at this health facility serves people from Ibanda District and the surrounding districts of Kitagwenda, Kazo, and Kiruhura. The clinic handles people with HIV four days a week and the clinic is run by two doctors, six clinical officers, four counselors, fifteen nurses, and two peer educators. About 90 patients are seen per clinic day.
Study Participants
We enrolled adult men aged 18 years and above, who had been on ART for at least 6 months, and were willing and able to provide written informed consent to participate in the study. We consecutively enrolled 252 participants, 5 of the participants who met the study criteria declined participation due to time constraints. We excluded men who were below 18 years, those with acute mental illness symptoms that would interfere with their ability to understand the contents of the questionnaire and the consent form, those who were physically ill and would not be able to stand the length of the interview, and those with communication disabilities like hearing impairment. The sample size was estimated using Cochran’s formula69 using the prevalence of HIV stigma among men (63%) from a study done in Cameroon.48
Data Collection
We consecutively recruited HIV positive men who came to the clinic for their routine visits until we reached our predetermined sample size. We used a researcher-administered questionnaire in a private room within the HIV clinic. We collected details on social demographic data including age, marital status, level of education, religion, occupation, area of residence, and HIV status of the partner. We also collected information on clinical factors that included the ART regimen, the duration on ART, and the presence of ART side effects. We also collected information on HIV stigma using the Berger HIV stigma scale,70 social support using the Multidimensional Scale of Perceived Social Support (MSPSS),71 and food insecurity using the Household Food Insecurity Access Scale (HFIAS).72
Study Measures
The Berger HIV stigma scale is a 40-item scale rated on a 4-point Likert-type scale (1=Strongly Disagree; 2=Disagree; 3=Agree; 4=Strongly Agree) and consists of 4 subscales to measure different forms of stigma: concerns about public attitude, concerns about self-image, concerns about HIV status disclosure and negative self-image. HIV stigma is calculated by summing all the items in the scale.70 The minimum score is 40 and the maximum is 160. High scores indicate higher levels of HIV stigma. The Berger HIV stigma scale has been validated and used among adult populations with HIV in various Sub-Saharan African countries with high reliability (Cronbach’s alpha=0.91).48,73
The 12-item MSPSS that measures three sources of social support (friends, family, and significant other) was used to measure social support in our study. The scale is scored on a 7-point Likert type scale ranging from “1=Very strongly Disagree” to “7=very strongly Agree”. Social support is obtained by summing up the scores for all items with higher scores indicating higher social support.71 The minimum score is 12 and the maximum is 84. The scale has been adapted for use in Uganda showing good reliability (Cronbach’s alpha=0.83).74 The MSPSS has also been used among people living with HIV in rural Uganda.75,76
The Household food insecurity access scale is a 9-item scale where each question has two parts. The first part of each question asks about the occurrence of a specific challenge concerning food insecurity in the last 4 weeks and the second part of the question asks about how often the specific challenge concerning food insecurity had occurred in the last 4 weeks. The first part of the question requires a “yes” or “no” response, while the second part provides three response options (1=Rarely; 2=Sometimes; 3=Often).72 The scale has been validated in eight countries72 and has been adapted for use among adults living with HIV in Uganda with excellent reliability (Cronbach’s alpha=0.91).54,77 The scale measures multiple domains of food insecurity experiences, including worry about availability and supply of food, the quality and quantity of food available, and social challenges of food unavailability.78 Food insecurity is the sum of all the scores from the 9 items with the highest score being 27 and the lowest score is 0. We categorized food insecurity into mild, moderated, and severe food insecurity following the algorithm provided during scale development.72
Ethical Considerations
The study was conducted according to the ethical guidelines of the Declarations of Helsinki.79 We received ethical approval from the research ethics committee of Mbarara University of Science Technology (# 09/01-20). We also received clearance from Uganda National Council for Science and Technology (UNCST) (# RECLEAR/01) as per Ugandan national guidelines. We obtained administrative clearance from Ibanda District Health Office and the facility in-charge at Ruhoko Health Centre IV. All participants provided written informed consent before enrolling in the study. We pre-tested the questionnaire on a small sample of HIV positive men at the facility to test for validity and content applicability to the local context. Data were collected in a private room within the clinic to ensure patient privacy. The questionnaire was administered in Runyankole, a local language spoken in the study area.
Data Management
Data were entered into EpiData software (version 4.6) each day of data collection. Entry was done by two separate entrants. The duplicate files were then validated to identify data entry errors. A validated dataset was then exported to Stata version 16.1 (StataCorp LLC, college station Texas, USA) for cleaning and analysis.
Data Analysis
We summarized sociodemographic characteristics using proportions for categorical variables and means and standard deviations for continuous variables. We then fitted modified Poisson regression models80 to estimate the associations between HIV stigma, food insecurity, and social support after adjusting for other covariates, including age, duration on ART, HIV status of the spouse, religion, and ART-regimen. Significance was determined at a P-value <0.05. We also sought to determine whether social support modified the relationship between food insecurity and HIV stigma. In this analysis, we included social support (continuous variable) as the main effect of exposure to food insecurity and the main product term for the interaction between social support and food insecurity. For both models, we adjusted for the independent variables indicated above.
Results
The study enrolled 252 participants. The majority of the participants were married (72.6%), aged 35 years and above age 35 years and above (70%), and had attained primary education (61.9%). The mean HIV stigma score was 70.08 (SD 19.34) with a minimum HIV stigma score of 40 and a maximum HIV stigma score of 132. The mean social support score was 68.13 (SD 8.88) and more than half (52%) scored below the 50th percentile on the social support scale. Three quarters (75%) of the study participants were food insecure, 5% of whom had severe food insecurity (Table 1).
 |
Table 1 Characteristics of Study Participants (N=252) |
On bivariate analysis, we found that the risk of HIV stigma was lower if participants were aged 35 years and above (unadjusted risk ratio (URR 0.84; 95% CI 0.79–0.90; P= <0.001)), had been on ART for more than 5 years (URR 0.85; 95% CI 0.78–0.93; P= <0.001), and had social support (URR 0.99; 95% CI 0.98–0.99; P= <0.001). However, the risk of HIV stigma was higher among those with food insecurity (URR 1.01; 95% CI 1.02–1.19; P=0.02) (Table 2).
 |
Table 2 Bivariate Analysis of the Factors Associated with HIV Stigma Among Men |
On multivariable Poisson regression analysis, we still found that the risk of HIV stigma was lower among those aged 35 years and above (adjusted risk ratio [ARR]=0.89; 95% CI 0.83–0.96; P=0.003, those who had been on ART for more than 5 years (ARR=0.92; 95% CI=0.84–0.99; P=0.04), and had social support (ARR=0.99; 95% CI=0.98–0.99; P=<0.001). Food insecurity was associated with an increased risk of HIV stigma (ARR=1.07; 95% CI 1.00–1.15; P=0.03) (Table 3).
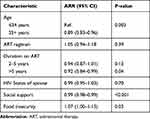 |
Table 3 Multivariate Logistic Regression of Factors Associated with HIV Stigma |
When we included the main effect of social support (high-level social support) in the regression model for HIV stigma, along with product terms to test for an interaction between social support and food insecurity, social support moderated the relationship between food insecurity and HIV stigma, with a non-statistically significant coefficient (P=0.45).
Discussion
The mean HIV stigma score among our study participants was 70.08 (SD 19.34) with a maximum HIV stigma score of 132 on the Berger scale. Food insecurity was associated with an increased risk of HIV stigma, while social support moderated the effect of food insecurity on HIV stigma among our study participants.
The protective influence of social support against HIV stigma in our sample echoes findings of previous studies in Uganda and other sub-Saharan settings indicating that lack of social support is associated with high levels of HIV stigma among adults living with HIV.11,51 However, our findings are unique because the study focuses on men living with HIV in a rural area in Uganda. According to previous research, men shun HIV care services to avoid the stigma associated with HIV which may dent their status in the society.37,81 In addition, men with HIV do not disclose their HIV status to avoid discrimination at work or loss of employment which would compromise their ability to provide for their families which deviates from society's expectations of men in most African settings.15,28–30 Avoidance of HIV care services means that men do not disclose their HIV status,37 which hinders their accessibility to social support.82,83 Lack of social support has been associated with high51 morbidity and mortality rates among men living with HIV in Uganda.35
According to existing literature, social support provides a sense of security for those who are experiencing stressors and promotes positive behaviors including improved self-confidence, self-esteem, and empowerment, which promote positive mental health.84–86 For people living with HIV, social support promotes a sense of belonging and neutralizes negative anticipations and feelings associated with HIV stigma.20,51,85,87 The availability of social support enables people living with HIV to access relevant information and guidance needed to navigate HIV care.52,88 HIV stigma narrows social networks and inhibits social interactions due to self-imposed social isolation related to the fear of negative judgment, shame, and guilt associated with HIV.53
We also found a statistically significant association between HIV stigma and severe food insecurity, which is similar to what has been reported in the previous research.66 HIV stigma predisposes HIV-affected households to food insecurity through limited social interaction and self-isolation by people living with HIV due to feelings of shame, guilt and self-devaluation.65,66 Previous studies show that HIV stigma is associated with higher levels of loneliness and social alienation, which disrupts their social relationships.18,89 Avoidance of social interaction in relation to HIV stigma narrows economic productivity due to the affected people missing out on employment opportunities, inability to engage in income generating activities and limited access to financial support.19 The fear of loss of employment opportunities is one of the documented reasons why men living with HIV do not seek care.37,81 The relationship between HIV stigma, social support and food insecurity in our study is best explained by the hypothetical model described by Takada et al51 (Figure 1). Both perceived HIV stigma and internalized HIV stigma limit accessibility to local social support systems, including sharing food with neighbors and borrowing money from family members and friends, which in turn limit their ability to access food.53,90 In the presence of enacted stigma, people living with HIV are not able to access instrumental supports like sharing food with neighbors or borrowing money to meet their personal needs.51,53,90 Internalized HIV stigma narrows social networks and inhibits social interactions due to self-imposed social isolation related to the fear of negative judgment, shame, and guilt associated with HIV.51,53 With internalized stigma, the affected people alienate themselves, hence cutting off social relationships and this compromises their ability to access emotional support.18,51
The relationship between HIV stigma and food insecurity has also been linked to poverty91 and internalized HIV stigma has been documented to have a greater impact on those with limited resources.18,20,92 The correlation between HIV stigma, food insecurity, and poverty may apply in our study since our participants were from a rural area where the majority of our study participants (79%) were involved in unskilled employment with limited sources of income. It has also been documented that food insecurity is more common in the rural areas due to limited land and poor soil quality which may further explain the food insecurity levels found in our study.93 Additionally, HIV is associated with morbidity which limits the ability of adults with HIV to work in their farms or engage in other economic activities which increases the risk of food insecurity at household level.67,90
Our study findings should be interpreted in light of some study limitations. The study was conducted among men in a rural HIV clinic and this may limit the generalizability of our findings to all men living with HIV in Uganda. Secondly, this was a cross-sectional study making it difficult to determine the causal effect relationship between HIV stigma, social support, and food insecurity. The stigma scale we used did not differentiate between internalized, enacted, and anticipated HIV stigma, which could have affected the interpretation of our findings in relation to the relationship between HIV stigma and food insecurity found in our study, given that existing literature points to a stronger association between internalized HIV stigma and food insecurity.66 Nonetheless, the Berger scale used in this study captures different aspects of HIV stigma including fear of disclosure, public negative attitudes, and self-image under which aspects of internalizing stigma are captured.70 Thirdly, we did not explore for masculinity norms which have been pointed out as a major barrier to HIV care among men living with HIV in most sub-Saharan settings and this could have had an impact on the interpretation of findings in relation to the associations between HIV stigma and food insecurity. However, beyond masculinity norms, previous studies have indicated the relationship between HIV stigma and food insecurity in Uganda. Last but not least, we interviewed only men in this study; hence, the findings do not represent the HIV stigma experiences and challenges of food insecurity and social support among women living with HIV in this setting.
Conclusions
Our findings show that social support and food insecurity are significantly associated with HIV stigma among men accessing HIV care at a rural health facility in southwestern Uganda. We also found that social support moderated the relationship between severe food insecurity and HIV stigma among our participants. Our findings suggest a need to incorporate social support interventions into the mainstream HIV care within the HIV clinics to enable adults living with HIV to form groups through which they can access and cope with the challenges of living with HIV. This is in line with previous studies showing that support groups within HIV clinics and communities are protective against mental health problems and HIV stigma among adults living with HIV.94,95 All our participants reported HIV stigma and HIV stigma is documented as a major barrier to HIV care which indicates a possibility that there are men living with HIV in the community and are not accessing care due to the fear of judgement and discrimination.20,35 There is a need to develop and implement community-based interventions to psychologically empower men in rural areas against HIV stigma to enable them to access care. Additionally, interventions aimed at economically empowering men living with HIV are necessary to overcome challenges of food insecurity since food insecurity is detrimental to HIV treatment outcomes through its interference with ART adherence.
Acknowledgments
We thank our research participants for willingly accepting us to take part in the study. We also acknowledge technical support from the Ibanda District Health Office, the in-charge, and the entire ART Clinic staff at Ruhoko Health center IV.
Disclosure
Mr Innocent Arinaitwe reports grants from the National Institutes of Health (NIH), during the conduct of the study. Ms Hildah Amutuhaire reports grants from the National Institute during the conduct of the study. Mr Davis Atwongyeire reports grants from the National Institutes of Health, during the conduct of the study. Ms Esther Tusingwire reports grants from the National Institutes of Health during the conduct of the study. The authors reported no other potential conflicts of interest for this work.
References
1. Goffman E. Stigma and social identity. Understanding Deviance. 1963;256:265.
2. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385.
3. Parker R, Aggleton P, editors. HIV/AIDS-related stigma and discrimination: a conceptual framework and implications for action. In: Culture, Society and Sexaulity. Routledge. 2007:459–474.
4. Emlet CA. Experiences of stigma in older adults living with HIV/AIDS: a mixed-methods analysis. AIDS Patient Care STDS. 2007;21(10):740–752.
5. Lekas H-M, Siegel K, Schrimshaw EW. Continuities and discontinuities in the experiences of felt and enacted stigma among women with HIV/AIDS. Qual Health Res. 2006;16(9):1165–1190.
6. Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21(1):283–291.
7. Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795.
8. Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160.
9. Audet CM, McGowan CC, Wallston KA, Kipp AM. Relationship between HIV stigma and self-isolation among people living with HIV in Tennessee. PLoS One. 2013;8(8):e69564.
10. Fuster-Ruizdeapodaca MJ, Molero F, Holgado FP, Mayordomo S. Enacted and internalized stigma and quality of life among people with HIV: the role of group identity. Qual Life Res. 2014;23(7):1967–1975.
11. Oke OO, Akinboro AO, Olanrewaju FO, Oke OA, Omololu AS. Assessment of HIV-related stigma and determinants among people living with HIV/AIDS in Abeokuta, Nigeria: a cross-sectional study. SAGE Open Med. 2019;7:2050312119869109.
12. Ashaba S, Kaida A, Burns BF, et al. Understanding coping strategies during pregnancy and the postpartum period: a qualitative study of women living with HIV in rural Uganda. BMC Pregnancy Childbirth. 2017;17.
13. Ashaba S, Kaida A, Coleman JN, et al. Psychosocial challenges facing women living with HIV during the perinatal period in rural Uganda. PLoS One. 2017;12(5):e0176256.
14. Dasgupta S, Sullivan PS, Dasgupta A, Saha B, Salazar LF. Stigma and access to HIV care among HIV-infected women in Kolkata, West Bengal. J Int Assoc Provid AIDS Care. 2013;12(1):44–49. doi:10.1177/1545109711401410
15. Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–1831.
16. Rendina HJ, Weaver L, Millar BM, López-Matos J, Parsons JT. Psychosocial Well-Being and HIV-related immune health outcomes among HIV-positive older adults: support for a biopsychosocial model of HIV stigma and health. J Int Assoc Providers AIDS Care. 2019;18:2325958219888462.
17. Chan BT, Weiser SD, Boum Y, et al. Persistent HIV-related stigma in rural Uganda during a period of increasing HIV incidence despite treatment expansion. AIDS (London, England). 2015;29(1):83.
18. Hasan MT, Nath SR, Khan NS, Akram O, Gomes TM, Rashid SF. Internalized HIV/AIDS-related stigma in a sample of HIV-positive people in Bangladesh. J Health Popul Nutr. 2012;30(1):22.
19. Malavé S, Ramakrishna J, Heylen E, Bharat S, Ekstrand M. Differences in testing, stigma, and perceived consequences of stigmatization among heterosexual men and women living with HIV in Bengaluru, India. AIDS Care. 2014;26(3):396–403.
20. Shamos S, Hartwig KA, Zindela N. Men’s and women’s experiences with HIV and stigma in Swaziland. Qual Health Res. 2009;19(12):1678–1689.
21. Treves-Kagan S, El Ayadi AM, Pettifor A, et al. Gender, HIV testing and stigma: the association of HIV testing behaviors and community-level and individual-level stigma in rural South Africa differ for men and women. AIDS Behav. 2017;21(9):2579–2588.
22. Lyimo RA, Stutterheim SE, Hospers HJ, de Glee T, van der Ven A, de Bruin M. Stigma, disclosure, coping, and medication adherence among people living with HIV/AIDS in Northern Tanzania. AIDS Patient Care STDS. 2014;28(2):98–105.
23. Stutterheim SE, Pryor JB, Bos AE, Hoogendijk R, Muris P, Schaalma HP. HIV-related stigma and psychological distress: the harmful effects of specific stigma manifestations in various social settings. Aids. 2009;23(17):2353–2357.
24. Girma E, Gebretsadik LA, Kaufman MR, Rimal RN, Morankar SN, Limaye RJ. Stigma against people with HIV/AIDS in rural Ethiopia, 2005 to 2011: signs and predictors of improvement. AIDS Behav. 2014;18(6):1046–1053.
25. Fleming PJ, Colvin C, Peacock D, Dworkin SL. What role can gender-transformative programming for men play in increasing men’s HIV testing and engagement in HIV care and treatment in South Africa? Cult Health Sex. 2016;18(11):1251–1264.
26. Fleming PJ, Dworkin SL. The importance of masculinity and gender norms for understanding institutional responses to HIV testing and treatment strategies. AIDS (London, England). 2016;30(1):157.
27. Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. A scoping review on the role of masculine norms in men’s engagement in the HIV care continuum in sub-Saharan Africa. AIDS Care. 2019.
28. Wyrod R. Masculinity and the persistence of AIDS stigma. Cult Health Sex. 2011;13(04):443–456.
29. Izugbara CO, Undie -C-C, Mudege NN, Ezeh AC. Male youth and Voluntary Counseling and HIV-Testing: the case of Malawi and Uganda. Sex Educ. 2009;9(3):243–259.
30. Skovdal M, Campbell C, Madanhire C, Mupambireyi Z, Nyamukapa C, Gregson S. Masculinity as a barrier to men’s use of HIV services in Zimbabwe. Global Health. 2011;7(1):1–14.
31. Mburu G, Ram M, Siu G, Bitira D, Skovdal M, Holland P. Intersectionality of HIV stigma and masculinity in eastern Uganda: implications for involving men in HIV programmes. BMC Public Health. 2014;14(1):1–9.
32. Sileo KM, Reed E, Kizito W, et al. Masculinity and engagement in HIV care among male fisherfolk on HIV treatment in Uganda. Cult Health Sex. 2019;21(7):774–788.
33. Nyanzi-Wakholi B, Lara AM, Watera C, Munderi P, Gilks C, Grosskurth H. The role of HIV testing, counselling, and treatment in coping with HIV/AIDS in Uganda: a qualitative analysis. AIDS Care. 2009;21(7):903–908.
34. Rakgoasi SD, Odimegwu C. Women get infected but men die … !” Narratives on men, masculinities and HIV/AIDS in Botswana. Int J Men’s Health. 2013;12:2.
35. Siu GE, Seeley J, Wight D. Dividuality, masculine respectability and reputation: how masculinity affects men’s uptake of HIV treatment in rural eastern Uganda. Soc Sci Med. 2013;89:45–52.
36. Siu GE, Wight D, Seeley JA. Masculinity, social context and HIV testing: an ethnographic study of men in Busia District, rural eastern Uganda. BMC Public Health. 2014;14(1):1–11.
37. Russell S, Zalwango F, Namukwaya S, et al. Antiretroviral therapy and changing patterns of HIV stigmatisation in Entebbe, Uganda. Sociol Health Illn. 2016;38(1):58–72.
38. Nyanzi B, Nyanzi S, Wolff B, Whitworth J. Money, men and markets: economic and sexual empowerment of market women in southwestern Uganda. Cult Health Sex. 2005;7(1):13–26.
39. Kipp W, Alibhai A, Saunders LD, et al. Gender differences in antiretroviral treatment outcomes of HIV patients in rural Uganda. AIDS Care. 2010;22(3):271–278.
40. Obermeyer CM, Sankara A, Bastien V, Parsons M. Gender and HIV testing in Burkina Faso: an exploratory study. Soc Sci Med. 2009;69(6):877–884.
41. Babalola S. Readiness for HIV testing among young people in northern Nigeria: the roles of social norm and perceived stigma. AIDS Behav. 2007;11(5):759–769.
42. Coetzee D, Hildebrand K, Boulle A, et al. Outcomes after two years of providing antiretroviral treatment in Khayelitsha, South Africa. Aids. 2004;18(6):887–895.
43. UNAIDS. Joint United Nations Programme on HIV:DATA, Update, AIDS Epidemic (AIDS, Issue). UNAIDS; 2019.
44. Alibhai A, Kipp W, Saunders LD, et al. Gender-related mortality for HIV-infected patients on highly active antiretroviral therapy (HAART) in rural Uganda. Int j Women’s Health. 2010;2:45.
45. Sorsdahl KR, Mall S, Stein DJ, Joska JA. The prevalence and predictors of stigma amongst people living with HIV/AIDS in the Western Province. AIDS Care. 2011;23(6):680–685.
46. Swendeman D, Rotheram-Borus MJ, Comulada S, Weiss R, Ramos ME. Predictors of HIV-related stigma among young people living with HIV. Health Psychol. 2006;25(4):501.
47. Uganda Bureau of Statistics. Uganda Demographic and Health Survey; 2016.
48. Ajong AB, Njotang PN, Nghoniji NE, et al. Quantification and factors associated with HIV-related stigma among persons living with HIV/AIDS on antiretroviral therapy at the HIV-day care unit of the Bamenda Regional Hospital, North West Region of Cameroon. Global Health. 2018;14(1):1–7. doi:10.1186/s12992-018-0374-5
49. Nattabi B, Li J, Thompson SC, Orach CG, Earnest J. Factors associated with perceived stigma among people living with HIV/AIDS in post-conflict northern Uganda. AIDS Educ Prev. 2011;23(3):193–205. doi:10.1521/aeap.2011.23.3.193
50. Ashaba S, Cooper-Vince C, Maling S, Rukundo G, Akena D, Tsai A. Internalized HIV stigma, bullying, major depressive disorder, and high-risk suicidality among HIV-positive adolescents in rural Uganda. Global Mental Health. 2018;5(e22):1–10.
51. Takada S, Weiser SD, Kumbakumba E, et al. The dynamic relationship between social support and HIV-related stigma in rural Uganda. Ann Behav Med. 2014;48(1):26–37.
52. Tsai AC, Bangsberg DR, Kegeles SM, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013;46(3):285–294.
53. Tsai AC, Bangsberg DR, Emenyonu N, Senkungu JK, Martin JN, Weiser SD. The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Soc Sci Med. 2011;73(12):1717–1724.
54. Tsai AC, Bangsberg DR, Frongillo EA, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74:12.
55. Anderson SA. Core indicators of nutritional state for difficult-to-sample populations. J Nutr. 1990;120(suppl_11):1555–1600.
56. Marmot M. Social determinants of health inequalities. The Lancet. 2005;365(9464):1099–1104.
57. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830–1839.
58. Martinez SM, Frongillo EA, Leung C, Ritchie L. No food for thought: food insecurity is related to poor mental health and lower academic performance among students in California’s public university system. J Health Psychol. 2018;1359105318783028.
59. Agriculture Organization. The State of Food Insecurity in the World 2014: Strengthening the Enabling Environment for Food Security and Nutrition. Food and Agriculture Organization; 2014.
60. Owino A, Atuhaire L, Wesonga R, Nabugoomu F, Muwanga-Zaake ES (2014). Determining factors that influence household food insecurity in Uganda: a case study of Tororo and Busia districts.
61. Perkins JM, Nyakato VN, Kakuhikire B, et al. Food insecurity, social networks and symptoms of depression among men and women in rural Uganda: a cross-sectional, population-based study. Public Health Nutr. 2018;21(5):838–848.
62. Daily G, Dasgupta P, Bolin B, et al. Food production, population growth, and the environment. Science (New York, NY). 1998;281(5381):1291–1292.
63. Magunda M, Larson W, Linden D, Nater E. Changes in microrelief and their effects on infiltration and erosion during simulated rainfall. Soil Technol. 1997;10(1):57–67.
64. Weiser SD, Gupta R, Tsai AC, et al. Changes in food insecurity, nutritional status, and physical health status after antiretroviral therapy initiation in rural Uganda. J Acquired Immune Def Syndr. 2012;61(2):179.
65. Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS Behav. 2002;6(4):309–319.
66. Shin SS, Carpenter CL, Ekstrand ML, et al. Household food insecurity as mediator of the association between internalized stigma and opportunistic infections. AIDS Behav. 2018;22(12):3897–3904.
67. Mwesigwa D. Household Food Security in Uganda: reflections on the prosperity-for-all programme. Loyola j Soc Sci. 2016;30:2.
68. Thomas R, Friebel R, Barker K, et al. Work and home productivity of people living with HIV in Zambia and South Africa. AIDS (London, England). 2019;33(6):1063.
69. Cochran WG. Sampling Techniques. John Wiley & Sons; 2007.
70. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–529.
71. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41.
72. Coates J, Swindale A, Bilinsky P (2007). Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide: version 3.
73. Feyissa GT, Abebe L, Girma E, Woldie M. Validation of an HIV-related stigma scale among health care providers in a resource-poor Ethiopian setting. J Multidiscip Healthc. 2012;5:97–113. doi:10.2147/JMDH.S29789
74. Nakigudde J, Musisi S, Ehnvall A, Airaksinen E, Agren H. Adaptation of the multidimensional scale of perceived social support in a Ugandan setting. Afr Health Sci. 2009;9 Suppl 1:S35–41.
75. Nakimuli-Mpungu E, Musisi S, Katabira E, Nachega J, Bass J. Prevalence and factors associated with depressive disorders in an HIV+ rural patient population in southern Uganda. J Affect Disord. 2011;135(1–3):160–167. doi:10.1016/j.jad.2011.07.009
76. Seffren V, Familiar I, Murray SM, et al. Association between coping strategies, social support, and depression and anxiety symptoms among rural Ugandan women living with HIV/AIDS. AIDS Care. 2018;30(7):888–895. doi:10.1080/09540121.2018.1441969
77. Miller CL, Bangsberg DR, Tuller DM, et al. Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS Behav. 2011;15(7):1512–1519.
78. Swindale A, Bilinsky P. Development of a universally applicable household food insecurity measurement tool: process, current status, and outstanding issues. J Nutr. 2006;136(5):1449S–1452S.
79. World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373.
80. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706.
81. Siu GE, Wight D, Seeley J. How a masculine work ethic and economic circumstances affect uptake of HIV treatment: experiences of men from an artisanal gold mining community in rural eastern Uganda. J Int AIDS Soc. 2012;15:17368.
82. Bhengu BR, Ncama BP, McInerney PA, et al. Symptoms experienced by HIV-infected Individuals on antiretroviral therapy in KwaZulu-Natal, South Africa. Appl Nurs Res. 2011;24(1):1–9.
83. Treffry-Goatley A, Lessells R, Sykes P, et al. Understanding specific contexts of antiretroviral therapy adherence in rural South Africa: a thematic analysis of digital stories from a community with high HIV prevalence. PLoS One. 2016;11(2):e0148801.
84. Feeney BC, Collins NL. A new look at social support: a theoretical perspective on thriving through relationships. Personality Soc Psychol Rev. 2015;19(2):113–147.
85. Turan B, Fazeli PL, Raper JL, Mugavero MJ, Johnson MO. Social support and moment-to-moment changes in treatment self-efficacy in men living with HIV: psychosocial moderators and clinical outcomes. Health Psychol. 2016;35(10):1126.
86. Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across the life course. Annu Rev Sociol. 2010;36:139–157.
87. Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117(3):497.
88. Maman S, van Rooyen H, Groves AK. HIV status disclosure to families for social support in South Africa (NIMH Project Accept/HPTN 043). AIDS Care. 2014;26(2):226–232.
89. Ware NC, Wyatt MA, Tugenberg T. Social relationships, stigma and adherence to antiretroviral therapy for HIV/AIDS. AIDS Care. 2006;18(8):904–910.
90. Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S–1739S.
91. Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Med. 2013;10(11):e1001557.
92. Visser MJ, Makin JD, Lehobye K. Stigmatizing attitudes of the community towards people living with HIV/AIDS. J Community Appl Soc Psychol. 2006;16(1):42–58.
93. Mamlin J, Kimaiyo S, Lewis S, et al. Integrating nutrition support for food-insecure patients and their dependents into an HIV care and treatment program in Western Kenya. Am J Public Health. 2009;99(2):215–221.
94. Brener L, Broady T, Cama E, Hopwood M, de Wit JB, Treloar C. The role of social support in moderating the relationship between HIV centrality, internalised stigma and psychological distress for people living with HIV. AIDS Care. 2020;32(7):850–857.
95. Flickinger TE, DeBolt C, Waldman AL, et al. Social support in a virtual community: analysis of a clinic-affiliated online support group for persons living with HIV/AIDS. AIDS Behav. 2017;21(11):3087–3099.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

