Back to Journals » Psychology Research and Behavior Management » Volume 16
Social Support and Daytime Sleepiness Among Chinese Medical Students: Mediating Roles of Loneliness and Problematic Smartphone Use
Received 26 July 2023
Accepted for publication 25 September 2023
Published 5 October 2023 Volume 2023:16 Pages 4083—4093
DOI https://doi.org/10.2147/PRBM.S432400
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Sijian Chen,1,2 Honghe Li,1 Deliang Wen1
1Institute for International Health Professions Education and Research, China Medical University, Shenyang, People’s Republic of China; 2School of Nursing, China Medical University, Shenyang, People’s Republic of China
Correspondence: Deliang Wen, Institute for International Health Professions Education and Research, China Medical University, No. 77 Puhe Road, Shenyang, Liaoning, 110122, People’s Republic of China, Email [email protected]
Background: Sleep problems have become a serious threat to public health worldwide. Daytime sleepiness is an important indicator of many sleep problems, which have a significant impact on academic performance, physical and mental health, and wellbeing among medical students. We aimed to explore the factors associated with daytime sleepiness among medical students.
Methods: We conducted a cross-sectional survey of 466 medical students recruited via convenience sampling. Self-rated psychometric scales, including the Social Support Rate Scale, the Epworth Sleepiness Scale, the Chinese version of the UCLA loneliness scale, and the Mobile Phone Addiction Index (MPAI), were utilized to evaluate social support, daytime sleepiness, loneliness, and problematic smartphone use. A sequential mediation model was constructed with daytime sleepiness as the dependent variable, social support as the independent variable, and loneliness and problematic smartphone use as mediating variables. Age, gender, and grade were taken as covariates.
Results: Social support among medical students was negatively associated with loneliness, problematic smartphone use, and daytime sleepiness (p < 0.01). A sequential mediation analysis showed that loneliness (the first mediator) and problematic smartphone use (the second mediator) sequentially mediated the path from social support to daytime sleepiness among medical students (β = − 0.008; 95% CI = − 0.016, − 0.002). Moreover, there were also significant mediating roles observed in the relationship between social support and daytime sleepiness via loneliness only (β = − 0.037; 95% CI = − 0.062, − 0.015) and problematic smartphone use only (β = − 0.022; 95% CI = − 0.041, − 0.008).
Conclusion: Social support, loneliness, and problematic smartphone use among medical students influenced their daytime sleepiness. Interventions targeting medical student loneliness and problematic smartphone use behaviors might attenuate the effects from low levels of social support and further improve daytime sleepiness.
Keywords: social support, daytime sleepiness, loneliness, problematic smartphone use
Introduction
Good quality sleep is a crucial indicator of human health, and sleep issues have become a widespread public health problem.1 Research on daytime sleepiness is relatively limited, despite some efforts that have been made to understand sleep problems in diverse populations.2–5 Daytime sleepiness is a common phenomenon and physiological state in which individuals desire to sleep during the day.6 Daytime sleepiness is also an indicator of numerous physical and mental health problems (eg, insufficient sleep, insomnia, and psychological distress).7–9 Based on the significant impact of daytime sleepiness on an individual’s physical and mental health and wellbeing, there has been increasing concern about daytime sleepiness. Most studies on daytime sleepiness have focused on populations with sleep-related breathing disorders2,10,11 or those secondary to somatic and psychiatric disorders.12–15 Several studies have also shown a high prevalence of daytime sleepiness, poor sleep quality, and poor sleep health among medical students,9,16 nurses,17 and the general population.18 However, these studies are only the beginning regarding the prevalence of daytime sleepiness.
Over the past decade, sleep issues have been the most detected mental health problem among Chinese college students.19 Daytime sleepiness among medical students adversely affects their cognitive function,20 academic performance,21 professional performance in clinical practice,22 and social interactions,23 and is a risk factor for a number of mental disorders.24,25 According to the social-ecological model of sleep, societal, social, and individual factors affect sleep health. At the individual level, attitudes, psychology, health behaviors, and other factors influence sleep health. Home, neighborhood, work/school, socioeconomics, and other factors contribute to the social level, while globalization, technology, public policy, and others are related elements at the societal level. The individual level is embedded within the social level, which, in turn, is embedded within the societal level.26 These societal and social/interpersonal factors, filtered through the social structure, ultimately influence sleep at the individual level.6
Social support in social/interpersonal-level factors is characterized as an individual’s perception or experience of affection, concern, value, belonging, or assistance in connection with others,27 which is frequently evaluated by the structure of social networks or the function of network members.27,28 According to the social-ecological model, social support can influence the emotions and health-related behaviors of individuals,29,30 which could affect individual sleep health. Moreover, there is also an association between social support and daytime sleepiness.31 Research on the relationship between social support and daytime sleepiness among nurses and college students in recent years shows that social support is negatively related to daytime sleepiness.17,32 Despite this evidence about the adverse effect of poor social support on daytime sleepiness, questions regarding the mediating factors that contribute to this association remain unanswered.33 In light of the critical role of social support for physical and mental health and the significant impact of daytime sleepiness on medical students, it is essential to investigate the association between social support and daytime sleepiness to elucidate important mediating mechanisms that could serve as potential intervention targets. This might also provide a new perspective to explore the pathways in which social relationships affect sleep health.
Loneliness and problematic smartphone use are important indicators of mental health problems among medical students.34 Loneliness is commonly referred to as feelings of depression, melancholy, poor spirits, and emptiness,35 which is a state of unmet individual or social-emotional needs.36,37 Medical students are in a crucial developmental period, building interpersonal relations and acquiring a sense of belonging, but loneliness has substantial adverse effects on their health and wellbeing. Previous studies have explored loneliness and daytime sleepiness, but the findings were inconsistent. Earlier research found that high levels of loneliness affect daily life and are associated with poor sleep quality, increasing daytime sleep symptoms.38 While Kurina et al found that loneliness was a significant predictor of sleep fragmentation in adults, they did not find an association between loneliness and daytime sleepiness. Recently, an increasing number of studies have shown that the relationship between loneliness and sleep health is bidirectional, with increased loneliness contributing to the continuation of a vicious cycle of poor sleep quality, prolonged loneliness, and excessive daytime sleepiness. Individuals exposed to this vicious cycle may continue to suffer from high loneliness, poor sleep quality, and excessive daytime sleepiness.39,40 Social support, a significant indicator of social relationships, is regarded as the most critical component that can effectively alleviate and predict the developmental trajectory of loneliness.41 However, there is a lack of research on mediating the relationship between loneliness on social support and daytime sleepiness.
Problematic smartphone use is a common health behavior problem among college students, described as a cognitive, emotional, and behavioral pattern of excessive use of smartphones that negatively impacts the individual’s daily life.42 Theoretically, the compensatory model of internet use explains this relationship.43–45 In reality, perceived stress and difficulties, and the lack of social support may prompt individuals to use an escape-coping strategy to satisfy their needs or relieve their negative emotions through a convenient online world, which can increase their problematic smartphone use behavior and lead to overindulgence. Social support has been found to be a protective factor for individual development and health.46 Among the consequences of problematic smartphone use, most research has focused on sleep disorders.45 Previous findings suggest that adolescents with lower perceived social support have problematic smartphone use behaviors and significantly higher severity of depressive symptoms and daytime sleepiness.47 The findings may support the hypothesis that problematic smartphone use might mediate the association between social support and daytime sleepiness. Therefore, the roles of loneliness and problematic smartphone use in the relationship between social support and daytime sleepiness should be explored more broadly and thoroughly.
Furthermore, loneliness may influence individual decisions to use the internet for gratification, which, in turn, may affect problematic internet use.48 According to the Interaction of Person-Affect-Cognition-Execution (I-PACE) model for problematic and addictive behaviors, adolescents with high levels of loneliness might use online social relationships to satisfy their social-emotional needs.49 A longitudinal association also exists between loneliness and problematic smartphone use.50,51 A study of Chinese college students found that those with lower levels of loneliness were less likely to experience problematic smartphone use after 6 and 18 months.51 Recent research on adolescents also revealed that loneliness mediates the association between perceived social support from family and friends and problematic smartphone use.46 These findings might provide support for the hypothesis that loneliness and problematic smartphone use might sequentially mediate the association between social support and daytime sleepiness. Therefore, further research is needed to determine the causal relationships between these variables with the aim of exploring the pathways in which social relationships affect sleep health.41
We aimed to explore the interrelationship between social support, loneliness, problematic smartphone use, and daytime sleepiness among medical students, as well as to test whether loneliness and problematic smartphone use play a sequential mediation role in the relationship between social support and daytime sleepiness. Based on the literature review, a theoretical hypothesis model was established, as shown in Figure 1. We hypothesized that: (1) loneliness would play a mediating role in the relationship between social support and daytime sleepiness among medical students; (2) problematic smartphone use would play a mediating role in the relationship between social support and daytime sleepiness among medical students; and (3) loneliness and problematic smartphone use would serially mediate the relationship between social support and daytime sleepiness among medical students.
Materials and Methods
Participants
Between November 3 and 14, 2022, we conducted a series of self-reported questionnaires with undergraduate medical students recruited from Chinese Medical University. We determined the estimated sample size to be 383 through the following formula: 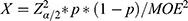 , using a power of 80%, a confidence level of 95%, and a margin of error of 5%.52,53 Accounting for potential invalid data (ie, up to 15% invalid), the minimum number of participants was determined to be 450. We distributed a total of 466 questionnaires. All participants entered the study voluntarily with any incentive and could withdraw at any time, and all participants provided informed consent before completing the measures. Exclusion criteria for all participants included self-reported sedative medication or recreational drug use; self-reported suffering from central disorders of hypersomnolence, sleep-related breathing disorders, circadian rhythm sleep-wake disorders, and excessive sleepiness secondary to other somatic diseases and mental disorders. A total of 455 students completed the questionnaires, 53 invalid responses were excluded, and 402 (86.27%) were effectively recovered. The sample consisted of 175 male and 227 female students aged 19–25 years (mean: 22.488 ± 1.828 years), including 43 first-year, 59 second-year, 98 third-year, 133 fourth-year, and 69 fifth-year undergraduate medical students. The Human Research Ethics Committee of China Medical University approved this study (ref no. 2023126).
, using a power of 80%, a confidence level of 95%, and a margin of error of 5%.52,53 Accounting for potential invalid data (ie, up to 15% invalid), the minimum number of participants was determined to be 450. We distributed a total of 466 questionnaires. All participants entered the study voluntarily with any incentive and could withdraw at any time, and all participants provided informed consent before completing the measures. Exclusion criteria for all participants included self-reported sedative medication or recreational drug use; self-reported suffering from central disorders of hypersomnolence, sleep-related breathing disorders, circadian rhythm sleep-wake disorders, and excessive sleepiness secondary to other somatic diseases and mental disorders. A total of 455 students completed the questionnaires, 53 invalid responses were excluded, and 402 (86.27%) were effectively recovered. The sample consisted of 175 male and 227 female students aged 19–25 years (mean: 22.488 ± 1.828 years), including 43 first-year, 59 second-year, 98 third-year, 133 fourth-year, and 69 fifth-year undergraduate medical students. The Human Research Ethics Committee of China Medical University approved this study (ref no. 2023126).
Measures
Social Support
The Social Support Rate Scale (SSRS) developed by Xiao for the Chinese population54,55 was used to comprehensively examine the social support of medical students. The SSRS contains 10 items and is divided into three dimensions (objective support, subjective support, and use of social support). Higher total scores reflect a higher level of social support. Cronbach’s α was 0.781 in the present study.
Daytime Sleepiness
Daytime sleepiness was assessed by the Epworth Sleepiness Scale (ESS),56 containing eight different scenarios commonly encountered in daily life (eg, “Sitting and reading”), in which participants estimate their likelihood of falling asleep or dozing off. Each item is scored on a 4-point Likert scale (0 = never, 3 = high chance). The sum of the eight-item scores yields a total score that ranged from 0 to 24. A total score between 0 and 10 is considered normal, and a score greater than 10 is considered excessive daytime sleepiness.56,57 In this study, Cronbach’s α of ESS was 0.739.
Loneliness
Loneliness was measured using the Chinese version of the UCLA loneliness scale58 developed by Russell.59 This measure consists of 20 items (eg, “Do you often feel lonely?”), including 11 positive and nine negative scoring items. All items are scored on a 5-point Likert scale (1 = never, 5 = always), with higher total scores reflecting higher levels of loneliness. Cronbach’s α in the present study was 0.908.
Problematic Smartphone Use
The current study utilized the Mobile Phone Addiction Index (MPAI) to evaluate problematic smartphone use,60 of which is widely employed in the Chinese college student population.61,62 The MPAI consists of 17 items that examine four domains, including “inability to control craving”, “feeling anxious and lost”, “withdrawal/escape”, and “productivity loss” (eg, “Your friends and family complained about your use of the mobile phone”). All items are scored on a 5-point Likert scale (1 = not at all, 5 = always). Higher total scores indicate higher levels of problematic smartphone use. In this study, MPAI (Cronbach’s α = 0.910) showed good internal consistency.
Data Analysis
Statistical Package for Social Sciences (SPSS 28.0, SPSS Inc., Chicago, IL) and Hayes’s PROCESS Macro were utilized to analyze our data. First, demographic characteristics were analyzed using descriptive statistics, and the scores for each measure were expressed as means and standard deviations. Counting data was reported as percentages (%). Examining the histograms and analyzing the skewness and kurtosis values of the variables in the study revealed that the data were approximately normally distributed. We examined the relationship between social support, daytime sleepiness, loneliness, and problematic smartphone use by Pearson correlation analysis. After adjusting the demographic characteristics of the participants, a multiple linear regression model was developed to determine the association between social support, daytime sleepiness, loneliness, and problematic smartphone use. Second, we evaluated the sequentially mediating effects of loneliness and problematic smartphone use in the association between social support and daytime sleepiness. Hayes’s PROCESS Macro (http://www.afhayes.com) was specially developed to assess the complex models, including mediators and moderators.63 To test the hypothesized model (Figure 1), we conducted mediation model analyses using PROCESS Macro (Models 6).64 In the mediation model, social support was the independent variable; daytime sleepiness was the dependent variable; and loneliness and problematic smartphone use were the first and second mediators, respectively. Moreover, age, gender, and grade were controlled for in the mediation model because prior evidence has shown that they are important confounders in daytime sleepiness.26,65,66 All study variables were standardized before the mediation model analyses. Based on 5000 bootstrap samples, the confidence intervals (CIs) determined whether the effects were statistically significant.64 The 95% bias-corrected CIs did not contain zero, indicating that the effect was significant. P-values < 0.05 were considered statistically significant.
Results
Common Method Bias
Considering that the data for the current study were collected from participant self-reports, there may have been a common method bias. Based on the research on confidentiality and the reverse scoring of some items, we examined the data for common method bias employing Harman’s single-factor test. Without rotation, the results indicated 10 factors with a characteristic root greater than 1, and the variance shown by the first factor was 22.141% (< 40%). Therefore, the results demonstrated that there was no significant common method bias in the present study.
Descriptive Statistics and Correlational Analysis
Table 1 shows the means, standard deviations (SDs), and correlation matrix for several crucial research variables. There was a negative correlation between social support and daytime sleepiness (r = −0.360, p < 0.01), loneliness (r = −0.164, p < 0.01), and problematic smartphone use (r = −0.224, p < 0.01). Loneliness was positively correlated with daytime sleepiness (r = 0.448, p < 0.01) and problematic smartphone use (r = 0.391, p < 0.01). There was a positive correlation between problematic smartphone use and daytime sleepiness (r = 0.380, p < 0.01).
 |
Table 1 Means, Standard Deviations, and Correlations of the Main Study Variables (N = 402) |
Multiple Linear Regression
The collinearity analysis of social support, daytime sleepiness, loneliness, and problematic smartphone use demonstrated that the tolerance values ranged from 0.81 to 0.97 and that variance inflation factor (VIF) values were around 1.00, with daytime sleepiness serving as the dependent variable. Daytime sleepiness was used as the dependent variable, and hierarchical regression was utilized. After controlling demographic variables (age, gender, and grade), the variables of social support, loneliness, and problematic smartphone use were gradually added to form four models, as displayed in Table 2. All crucial research variables showed a linear regression relationship (β = −0.266, 0.331, and 0.188, respectively; all p-values < 0.001).
 |
Table 2 Multiple Linear Regression of Daytime Sleepiness in Medical Students |
Testing for Sequential Mediation Effect
A bias-corrected percentile bootstrap test was used to analyze the sequential mediating effects of loneliness and problematic smartphone use on social support and daytime sleepiness. Age, gender, and grade were taken as covariates. The pathway analysis of social support, daytime sleepiness, loneliness, and problematic smartphone use revealed that all direct associations (social support to loneliness, problematic smartphone use, and daytime sleepiness; loneliness to problematic smartphone use and daytime sleepiness; problematic smartphone use to daytime sleepiness) were significant (Figure 2 and Table 3). There were significant indirect effects observed in the relationship between social support and daytime sleepiness via loneliness only (β = −0.037; 95% CI = −0.062, −0.015), problematic smartphone use only (β = −0.022; 95% CI = −0.041, −0.008), or loneliness and problematic smartphone use sequentially (β = −0.008; 95% CI = −0.016, −0.002). These results indicate that loneliness and problematic smartphone use were mediators of the association between social support and daytime sleepiness (Table 3).
 |
Table 3 Bootstrapping Results of the Sequential Mediation Model on Daytime Sleepiness |
Discussion
Loneliness and problematic smartphone use might play an independent or sequential mediating role between social support and daytime sleepiness. To our knowledge, this is the first study investigating the relationships between social support, loneliness, problematic smartphone use, and the severity of daytime sleepiness symptoms among medical students.
Based on the study population, our primary findings are as follows: First, the direct effect measured in the current study indicated that lower levels of social support were directly associated with higher levels of daytime sleepiness among medical students. Similar results were found recently, indicating that the social support level of female shift nurses was significantly and negatively associated with daytime sleepiness and insomnia,17 and that the level of social support among college students was a predictor of daytime sleepiness.32 Moreover, our findings subscribed to the social-ecological theoretical model. Low levels of social support (social-level risk factors) have the potential to heighten individual levels of stress and anxiety.67 When confronted with the various obstacles and adversities of life, individuals may experience increased levels of anxiety and a diminished ability to effectively manage these challenges. This can be attributed to an absence of social support and a limited interpersonal network of dependable individuals with whom they can confide and seek solace.68 Consequently, these circumstances may impede the process of falling asleep and aggravate individual insufficient sleep or sleep-related problems.26
Second, we examined the effects of loneliness and problematic smartphone use on the association between social support and daytime sleepiness symptoms. Our main findings were that loneliness and problematic smartphone use had serial mediating roles in the relationship between social support and daytime sleepiness, and social support was associated with daytime sleepiness symptoms by increasing loneliness levels and problematic smartphone use behaviors, thus supporting our hypothesis. These findings are consistent with a previous study conducted among 1056 Chinese adolescents, which reported that loneliness mediated the relationship between social support and problematic smartphone use.46 Also, the results of a study conducted among Turkish university students found that loneliness predicted problematic smartphone use.69 In the present study, social support had significant indirect effects on problematic smartphone use through loneliness. Medical students with lower levels of social support may suffer from social isolation, and they are more likely to experience loneliness.34,70 This also supports the I-PACE model,49 namely that medical students with higher levels of loneliness are more prone to utilizing online social interactions to meet their social-emotional and social relationship needs, and are more at risk of exhibiting problematic smartphone use behaviors, emotional problems, and poor sleep health.71,72
Third, our results suggested the mediating role of loneliness in the relationship between social support and daytime sleepiness. Specifically, lower levels of social support are associated with higher levels of loneliness, which in turn indirectly affect the development of daytime sleepiness symptoms. This may be considering loneliness is normally accompanied by emotional stress and anxiety in individuals, both of which can increase emotional insecurity at night, making it more difficult to fall asleep and promoting increased daytime fatigue and daytime sleepiness.73 Similarly, Grey et al found that exposure to lower levels of social support were associated with higher levels of loneliness and depression, which ultimately led to more severe sleep problems.74 Furthermore, we explored the role of problematic smartphone use in the relationship between social support and daytime sleepiness. Problematic smartphone use mediated the relationship between social support and daytime sleepiness symptoms. A recent meta-analysis has found similar results, which reported that excessive smartphone use among nursing students was associated with lower levels of perceived social support sleep quality.75 Meanwhile, a study in China investigated that the detection rate of smartphone addiction among 2741 medical students was as high as 52.8%, and medical students with smartphone addiction had higher levels of insomnia and subhealth.76 Additionally, our findings support the compensatory model of internet use.43–45 Medical students with low levels of social support are prone to escape and gratify their needs or alleviate their negative emotions via the online world, which may increase their problematic smartphone use behaviors and impact their physical and mental health. Therefore, social support may also have indirect effects on daytime sleepiness through medical student loneliness or problematic smartphone use only.
Sleep health among medical students is an important issue. To our knowledge, this is the first study to investigate the mediating effects of loneliness and problematic smartphone use in the relationship between social support and daytime sleepiness. This makes it possible to explore the pathways in which social relationships affect sleep health through a sequential mediation model between these variables. Meanwhile, a socio-ecological model of sleep provides a framework to consider the dynamic interplay among individual, social, and societal factors.1 Interventions based on social/interpersonal-level factors (ie, social support) and individual level factors (ie, loneliness) can improve outcomes (ie, problematic smartphone use and daytime sleepiness). Family and group supportive therapies, as well as cognitive behavioral therapy, have been demonstrated to be beneficial.77–79 The social and environmental determinants of sleep health are commonly beyond the scope of individual behavior.1 Therefore, it is crucial to think about multilevel prevention strategies to improve sleep health when conducting intervention research.80
This study also had several limitations. First, we could not provide evidence of causality due to the cross-sectional design, which does not account for temporal effects. Future studies should use a longitudinal design to establish and validate causal relationships. Second, all variables used in the current study were evaluated based on self-reports from the participants. Future studies utilizing multiple methods to collect data should be conducted, such as objective monitoring to measure daytime sleepiness levels and diagnostic assessment by a clinical specialist to exclude participants with sleep disorders. Third, all the participants in this study were medical students from a college in northeastern China. Consequently, the findings may not be applicable to other professional populations and cannot be generalized to other countries. Future research should recruit a larger, more representative sample to validate our findings. Finally, measures of sleep duration and blue light-emitting device usage before bedtime were not obtained, which have been suggested to influence the onset of daytime sleepiness.81,82 Therefore, there is a residual confounding risk from unmeasured covariates. In future studies, it is recommended to include sleep duration and blue light-emitting device usage before bedtime as covariates.
Conclusions
The present study provides evidence of factors mediating the relationship between daytime sleepiness and social support among medical students. Specifically, we describe two mediating factors in the aforementioned relationship. For medical students, social/interpersonal-level factors had a significant impact on their sleep health. Additionally, social support affected daytime sleepiness, and this relationship was mediated by loneliness and problematic smartphone use. Further research is essential to confirm the effects of these factors on daytime sleepiness. Furthermore, our study provided evidence that loneliness and problematic smartphone use could be used as interventional entry points to improve daytime sleepiness among medical students. Interventions targeting loneliness and health-related behaviors among medical students may mitigate the effects from low levels of social support, and further improve their daytime functions.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study was reviewed and approved by the Human Research Ethics Committee of China Medical University (ref no. 2023126). All procedures performed in studies involving human participants were in accordance with the ethical standards and with the Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Acknowledgments
The authors wish to thank all the participants for their efforts in the study.
Funding
This research was supported by the Liaoning Social Science Planning Fund Project [grant number L20AED006] and the Research Projects of the School of Nursing of China Medical University [grant number 2022HL-16].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hale L, Troxel W, Buysse DJ. Sleep health: an opportunity for public health to address health equity. Annu Rev Public Health. 2020;41(1):81–99. doi:10.1146/annurev-publhealth-040119-094412
2. Lal C, Weaver TE, Bae CJ, Strohl KP. Excessive daytime sleepiness in obstructive sleep apnea. mechanisms and clinical management. Ann Am Thorac Soc. 2021;18(5):757–768. doi:10.1513/AnnalsATS.202006-696FR
3. Guo M, Feng T, Liu M, et al. Causal roles of daytime sleepiness in cardiometabolic diseases and osteoporosis. Eur Rev Med Pharmacol Sci. 2022;26(8):2755–2764. doi:10.26355/eurrev_202204_28605
4. Dauvilliers Y, Verbraecken J, Partinen M, et al. Pitolisant for daytime sleepiness in patients with obstructive sleep apnea who refuse continuous positive airway pressure treatment. A randomized trial. Am J Respir Crit Care Med. 2020;201(9):1135–1145. doi:10.1164/rccm.201907-1284OC
5. Liguori C, Toledo M, Kothare S. Effects of anti-seizure medications on sleep architecture and daytime sleepiness in patients with epilepsy: a literature review. Sleep Med Rev. 2021;60:101559. doi:10.1016/j.smrv.2021.101559
6. Holding BC, Sundelin T, Schiller H, Åkerstedt T, Kecklund G, Axelsson J. Sleepiness, sleep duration, and human social activity: an investigation into bidirectionality using longitudinal time-use data. Proc Natl Acad Sci U S A. 2020;117(35):21209–21217. doi:10.1073/pnas.2004535117
7. Gandhi KD, Mansukhani MP, Silber MH, Kolla BP. Excessive daytime sleepiness: a clinical review. Mayo Clinic Proceed. 2021;96(5):1288–1301. doi:10.1016/j.mayocp.2020.08.033
8. Kaur G, Singh A. Excessive daytime sleepiness and its pattern among Indian college students. Sleep Med. 2017;29:23–28. doi:10.1016/j.sleep.2016.08.020
9. Sameer HM, Imran N, Tarar TN, Khawaja IS. Association of excessive daytime sleepiness with psychological distress in medical students. Prim Care Companion CNS Disord. 2020;22(1):19m02531. doi:10.4088/PCC.19m02531
10. Steffen A. Patient related outcome and therapy effects in stimulation treatment of sleep-related breathing disorders. Laryngorhinootologie. 2022;101(S 01):103–113. doi:10.1055/a-1647-8601
11. Khasawneh L, Odat H, Khassawneh BY, et al. Efficacy of pillar implants to reduce snoring and daytime sleepiness. Future Sci OA. 2021;7(6):FSO701. doi:10.2144/fsoa-2021-0020
12. Stefani A, Högl B. Sleep in Parkinson’s disease. Neuropsychopharmacology. 2020;45(1):121–128. doi:10.1038/s41386-019-0448-y
13. Büttner-Teleagă A, Kim Y-T, Osel T, Richter K. Sleep disorders in cancer-a systematic review. Int J Environ Res Public Health. 2021;18(21):11696. doi:10.3390/ijerph182111696
14. Smagula SF, Jia Y, Chang C-CH, Cohen A, Ganguli M. Trajectories of daytime sleepiness and their associations with dementia incidence. J Sleep Res. 2020;29(6):e12952. doi:10.1111/jsr.12952
15. Mikael Lopes J, Galvão FD, Oliveira AG. Risk of death in the elderly with excessive daytime sleepiness, insomnia and depression: prospective cohort study in an Urban Population in Northeast Brazil. Arq Bras Cardiol. 2021;117(3):446–454. doi:10.36660/abc.20200059
16. da Silva Cardoso GM, da Silva MP, de Castro Corrêa C, Weber SA. Insomnia and excessive daytime sleepiness in medical students: consequences of the use of technologies? Sleep Sci. 2022;15(Spec 1):116–119. doi:10.5935/1984-0063.20220008
17. D’Ettorre G, Pellicani V, Caroli A, Greco M. Shift work sleep disorder and job stress in shift nurses: implications for preventive interventions. Med Lav. 2020;111(3):195–202. doi:10.23749/mdl.v111i3.9197
18. Thorarinsdottir EH, Bjornsdottir E, Benediktsdottir B, et al. Definition of excessive daytime sleepiness in the general population: feeling sleepy relates better to sleep-related symptoms and quality of life than the Epworth sleepiness scale score. Results from an epidemiological study. J Sleep Res. 2019;28(6):e12852. doi:10.1111/jsr.12852
19. Chen Y, Zhang Y, Yu G. Prevalence of mental health problems among college students in mainland China from 2010 to 2020: a meta-analysis. Adv Psychol Sci. 2022;30(5):991–1004. doi:10.3724/SP.J.1042.2022.00991
20. Peng L, Gao L, Gao C, et al. Daytime sleep behaviors and cognitive performance in middle- to older-aged adults living with and without HIV Infection. Nat Sci Sleep. 2022;14:181–191. doi:10.2147/NSS.S339230
21. Maheshwari G, Shaukat F. Impact of poor sleep quality on the academic performance of medical students. Cureus. 2019;11(4):e4357. doi:10.7759/cureus.4357
22. Pikovsky O, Oron M, Shiyovich A, Perry ZH, Nesher L. The impact of sleep deprivation on sleepiness, risk factors and professional performance in medical residents. Isr Med Assoc J. 2013;15(12):739–744.
23. Dagnew B, Dagne H, Andualem Z. Depression and its determinant factors among university of Gondar medical and health science students, Northwest Ethiopia: institution-based cross-sectional study. Neuropsychiatr Dis Treat. 2020;16:839–845. doi:10.2147/NDT.S248409
24. Liu X, Liu -Z-Z, Wang Z-Y, Yang Y, Liu B-P, Jia C-X. Daytime sleepiness predicts future suicidal behavior: a longitudinal study of adolescents. Sleep. 2019;42(2). doi:10.1093/sleep/zsy225
25. Dickinson DL, Wolkow AP, Rajaratnam SMW, Drummond SPA. Personal sleep debt and daytime sleepiness mediate the relationship between sleep and mental health outcomes in young adults. Depress Anxiety. 2018;35(8):775–783. doi:10.1002/da.22769
26. Michael AG. Sleep, Health, and Society. Sleep Med Clin. 2017;12(1):1–22. doi:10.1016/j.jsmc.2016.10.012
27. Taylor SE. Social Support: a Review. In: Friedman HS, editor. The Oxford Handbook of Health Psychology.
28. de Grey RG K, Uchino BN, Trettevik R, Cronan S, Hogan JN. Social support and sleep: a meta-analysis. Health Psychol. 2018;37(8):787–798. doi:10.1037/hea0000628
29. Huang Y, Su X, Si M, et al. The impacts of coping style and perceived social support on the mental health of undergraduate students during the early phases of the COVID-19 pandemic in China: a multicenter survey. BMC Psychiatry. 2021;21(1):530. doi:10.1186/s12888-021-03546-y
30. Jiang M, Zhao Y, Wang J, et al. Serial multiple mediation of the correlation between internet addiction and depression by social support and sleep quality of college students during the COVID-19 Epidemic. Psychiatry Investig. 2022;19(1):9–15. doi:10.30773/pi.2021.0147
31. Billings ME, Hale L, Johnson DA. Physical and social environment relationship with sleep health and disorders. Chest. 2020;157(5):1304–1312. doi:10.1016/j.chest.2019.12.002
32. Lee J, Suh S. The relationship between subjective sleep, emotions, social support and excessive daytime sleepiness in female undergraduate students. J Sleep Med. 2017;14(1):36–42. doi:10.13078/jsm.17005
33. Robbins R, Jean-Louis G, Gallagher RA, et al. Examining social capital in relation to sleep duration, insomnia, and daytime sleepiness. Sleep Med. 2019;60:165–172. doi:10.1016/j.sleep.2019.03.019
34. Peng P, Hao Y, Liu Y, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2023;321:167–181. doi:10.1016/j.jad.2022.10.040
35. Killeen C. Loneliness: an epidemic in modern society. J Adv Nurs. 1998;28(4):762–770. doi:10.1046/j.1365-2648.1998.00703.x
36. Chu HY, Chan HS. Loneliness and social support among the middle-aged and elderly people with visual impairment. Int J Environ Res Public Health. 2022;19(21):14600. doi:10.3390/ijerph192114600
37. Rokach A, Matalon R, Rokach B, Safarov A. The effects of gender and marital status on loneliness of the aged. Soc Behav Pers. 2007;35(2):243–254. doi:10.2224/sbp.2007.35.2.243
38. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. doi:10.1007/s12160-010-9210-8
39. Wilson KA, Ferguson SA, Rebar A, Alfrey KL, Vincent GE. Comparing the effects of FIFO/DIDO workers being home versus away on sleep and loneliness for partners of Australian mining workers. Clocks Sleep. 2020;2(1):86–98. doi:10.3390/clockssleep2010009
40. Griffin SC, Williams AB, Ravyts SG, Mladen SN, Rybarczyk BD. Loneliness and sleep: a systematic review and meta-analysis. Health Psychol Open. 2020;7(1):205510292091323. doi:10.1177/2055102920913235
41. Zhang X, Dong S. The relationships between social support and loneliness: a meta-analysis and review. Acta Psychol. 2022;227:103616. doi:10.1016/j.actpsy.2022.103616
42. Billieux J. Problematic use of the mobile phone: a literature review and a pathways model. Curr Psychiatry Rev. 2012;8(4):299–307. doi:10.2174/157340012803520522
43. Zhao C, Xu H, Lai X, et al. Effects of online social support and perceived social support on the relationship between perceived stress and problematic smartphone usage among Chinese undergraduates. Psychol Res Behav Manag. 2021;14:529–539. doi:10.2147/PRBM.S302551
44. Kardefelt-Winther D. Problematizing excessive online gaming and its psychological predictors. Comput Human Behav. 2014;31:118–122. doi:10.1016/j.chb.2013.10.017
45. Amiri M, Dowran B, Salimi H, Zarghami MH. The problematic use of mobile phone and mental health: a review study in Iran. J Educ Health Promot. 2020;9:290. doi:10.4103/jehp.jehp_268_20
46. Lin S, Yuan Z, Niu G, Fan C, Hao X. Family matters more than friends on problematic social media use among adolescents: mediating roles of resilience and loneliness. Int J Ment Health Addiction. 2023;1–19. doi:10.1007/s11469-023-01026-w
47. Nowak M, Rachubińska K, Starczewska M, et al. Correlations between problematic mobile phone use and depressiveness and daytime sleepiness, as well as perceived social support in adolescents. Int J Environ Res Public Health. 2022;19(20):13549. doi:10.3390/ijerph192013549
48. Li J, Zhan D, Zhou Y, Gao X. Loneliness and problematic mobile phone use among adolescents during the COVID-19 pandemic: the roles of escape motivation and self-control. Addict Behav. 2021;118:106857. doi:10.1016/j.addbeh.2021.106857
49. Brand M, Wegmann E, Stark R, et al. The Interaction of Person-Affect-Cognition-Execution (I-PACE) model for addictive behaviors: update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neurosci Biobehav Rev. 2019;104:1–10. doi:10.1016/j.neubiorev.2019.06.032
50. Kim JH. Longitudinal associations among psychological issues and problematic use of smartphones. J Media Psychol. 2019;31(3):117–127. doi:10.1027/1864-1105/a000234
51. Wang A, Wang Z, Zhu Y, Shi X. The prevalence and psychosocial factors of problematic smartphone use among Chinese college students: a three-wave longitudinal study. Front Psychol. 2022;13:877277. doi:10.3389/fpsyg.2022.877277
52. Population proportion - sample size - select statistical consultants. Available from: https://select-statistics.co.uk/calculators/sample-size-calculator-population-proportion/.
53. Soubra R, Hasan I, Ftouni L, Saab A, Shaarani I. Future healthcare providers and professionalism on social media: a cross-sectional study. BMC Med Ethics. 2022;23(1):4. doi:10.1186/s12910-022-00742-7
54. Shuiyuan X. The influence of social support on physical and mental health. Chinese Ment Health J. 1987;1:183–187.
55. Zhou SJ, Wang LL, Yang R, et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;74:39–47. doi:10.1016/j.sleep.2020.06.001
56. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
57. Yu YK, Yao ZY, Wei YX, et al. Depressive symptoms as a mediator between excessive daytime sleepiness and suicidal ideation among Chinese college students. Int J Environ Res Public Health. 2022;19(23):16334. doi:10.3390/ijerph192316334
58. Liu H, Wang H. Mobile phone addiction tendency and loneliness in college students. Chin Ment Health J. 2012;26(1):66–69.
59. Russell DW. UCLA loneliness scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40. doi:10.1207/s15327752jpa6601_2
60. Leung L. Linking psychological attributes to addiction and improper use of the mobile phone among adolescents in Hong Kong. J Child Media. 2008;2(2):93–113. doi:10.1080/17482790802078565
61. Liu S, Zhou W, Wang J, Chen B, He G, Jia Y. Association between mobile phone addiction index and sugar-sweetened food intake in medical college students stratified by sex from Shanghai, China. Nutrients. 2021;13(7):2256. doi:10.3390/nu13072256
62. Li L, Griffiths MD, Mei S, Niu Z. Fear of missing out and smartphone addiction mediates the relationship between positive and negative affect and sleep quality among Chinese university students. Front Psychiatry. 2020;11:877. doi:10.3389/fpsyt.2020.00877
63. Hayes AF, Montoya AK, Rockwood NJ. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australas Mark J. 2017;25(1):76–81. doi:10.1016/j.ausmj.2017.02.001
64. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford publications; 2013.
65. Isa T, Sugimoto T, Murata S, et al. Lower physical activity is associated with daytime sleepiness in children aged 9–12 years. J Child Health Care. 2019;23(3):415–424. doi:10.1177/1367493519864756
66. Berger M, Hirotsu C, Haba-Rubio J, et al. Risk factors of excessive daytime sleepiness in a prospective population-based cohort. J Sleep Res. 2021;30(2):e13069. doi:10.1111/jsr.13069
67. Özmete E, Pak M. The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Soc Work Public Health. 2020;35(7):603–616. doi:10.1080/19371918.2020.1808144
68. Roohafza HR, Afshar H, Keshteli AH, et al. What’s the role of perceived social support and coping styles in depression and anxiety? J Res Med Sci. 2014;19(10):944–949.
69. Karaoglan Yilmaz FG, Avci U, Yilmaz R. The role of loneliness and aggression on smartphone addiction among university students. Curr Psychol. 2022;1–9. doi:10.1007/s12144-022-03018-w
70. Ray ME, Coon JM, Al-Jumaili AA, Fullerton M. Quantitative and qualitative factors associated with social isolation among graduate and professional health science students. AJPE. 2019;83(7). doi:10.5688/ajpe6983
71. Alzhrani AM, Aboalshamat KT, Badawoud AM, et al. The association between smartphone use and sleep quality, psychological distress, and loneliness among health care students and workers in Saudi Arabia. PLoS One. 2023;18(1):e0280681. doi:10.1371/journal.pone.0280681
72. Alinejad V, Parizad N, Yarmohammadi M, Radfar M. Loneliness and academic performance mediates the relationship between fear of missing out and smartphone addiction among Iranian university students. BMC Psychiatry. 2022;22(1):550. doi:10.1186/s12888-022-04186-6
73. Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14(4):227–238. doi:10.1016/j.smrv.2009.10.007
74. Grey I, Arora T, Thomas J, Saneh A, Tohme P, Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020;293:113452. doi:10.1016/j.psychres.2020.113452
75. Osorio-Molina C, Martos-Cabrera MB, Membrive-Jiménez MJ, et al. Smartphone addiction, risk factors and its adverse effects in nursing students: a systematic review and meta-analysis. Nurse Educ Today. 2021;98:104741. doi:10.1016/j.nedt.2020.104741
76. Liu H, Zhou Z, Huang L, Zhu E, Yu L, Zhang M. Prevalence of smartphone addiction and its effects on subhealth and insomnia: a cross-sectional study among medical students. BMC Psychiatry. 2022;22(1):305. doi:10.1186/s12888-022-03956-6
77. Hoang P, King JA, Moore S, et al. Interventions associated with reduced loneliness and social isolation in older adults: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(10):e2236676. doi:10.1001/jamanetworkopen.2022.36676
78. Kodsi A, Bullock B, Kennedy GA, Tirlea L. Psychological interventions to improve sleep in young adults: a systematic review and meta-analysis of randomized controlled trials. Behav Sleep Med. 2022;20(1):125–142. doi:10.1080/15402002.2021.1876062
79. Bisdounis L, Saunders KEA, Farley HJ, et al. Psychological and behavioural interventions in bipolar disorder that target sleep and circadian rhythms: a systematic review of randomised controlled trials. Neurosci Biobehav Rev. 2022;132:378–390. doi:10.1016/j.neubiorev.2021.12.002
80. Barnes CM, Drake CL. Prioritizing sleep health: public health policy recommendations. Perspect Psychol Sci. 2015;10(6):733–737. doi:10.1177/1745691615598509
81. Wahl S, Engelhardt M, Schaupp P, Lappe C, Ivanov IV. The inner clock—Blue light sets the human rhythm. J Biophotonics. 2019;12(12):e201900102. doi:10.1002/jbio.201900102
82. Alves FR, de Souza EA, de França Ferreira LG, de Oliveira Vilar Neto J, de Bruin VMS, de Bruin PFC. Sleep duration and daytime sleepiness in a large sample of Brazilian high school adolescents. Sleep Med. 2020;66:207–215. doi:10.1016/j.sleep.2019.08.019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


