Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Social Stigma Toward Individuals with Schizophrenia in a Lebanese Population
Authors Tantawi SA , Kamaleddine AN , Alhajj LA , Naous SM, Kamaleddine NN, Chung S , Joo SW
Received 30 November 2023
Accepted for publication 27 February 2024
Published 8 March 2024 Volume 2024:20 Pages 561—570
DOI https://doi.org/10.2147/NDT.S450385
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Sana Ahmad Tantawi,1 Atifa Nazih Kamaleddine,1 Lama Ali Alhajj,1 Sondos Mohamad Naous,1 Nafez Nazih Kamaleddine,2 Seockhoon Chung,3 Sung Woo Joo3
1Faculty of Medical Sciences, Lebanese University, Hadath, Beirut, Lebanon; 2Faculty of Medicine, Beirut Arab University, Beirut, Lebanon; 3Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
Correspondence: Sung Woo Joo, Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea, Tel +82-2-3010-0742, Fax +82-2-485-8381, Email [email protected]
Background: Schizophrenia has been recognized as the most stigmatized mental disorder, imposing a substantial burden on affected individuals. However, no prior studies have investigated social stigma toward individuals with schizophrenia in Lebanon.
Purpose: We aimed to examine three components of social stigma including knowledge, attitude, and behavior toward individuals with schizophrenia in a Lebanese population and to explore associated factors with the level of social stigma.
Patients and Methods: A cross-sectional online survey was administered, and data from 469 participants were gathered from January 31, 2023, to February 18, 2023. We used previously validated questionnaires to assess the knowledge, attitude (Social Distance Scale), and behavior (Reported and Intended Behavior Scale) of participants toward individuals with schizophrenia. The score for each section was calculated and used to explore the associations between sociodemographic factors and the levels of stigma in each domain.
Results: The study participants had a moderate understanding of schizophrenia. However, a substantial proportion showed negative attitudes and unfavorable behaviors toward individuals with schizophrenia. We identified several sociodemographic factors associated with the knowledge, attitude, and behavior scores. Notably, a higher knowledge score and more positive attitudes were positively correlated with improved intended behaviors.
Conclusion: This study highlights the pervasive stigma encompassing issues in knowledge, attitudes, and behavior surrounding schizophrenia in a Lebanese population. Our study suggests a pressing need for targeted interventions to increase public awareness and decrease the social stigma of schizophrenia in Lebanon.
Keywords: schizophrenia, knowledge, attitude, behavior, stigma
Introduction
Schizophrenia has been acknowledged as a mental disorder that is associated with significant levels of stigma.1 Individuals with schizophrenia often become targets of social stigma from their surrounding society. Stigma is encountered when elements of labeling, stereotyping, separation, status loss, and discrimination co-occur in a power situation that allows these processes to unfold.2 Stigma refers to a complex social phenomenon that encompasses faults in knowledge, attitudes, and behavior, particularly with regard to certain individuals or groups. The knowledge gap associated with stigma often manifests as ignorance, highlighting that despite an abundance of available information, accurate knowledge about mental illness remains limited. Negative attitudes include prejudice, which includes feelings and thoughts such as fear, hatred, distrust, and disgust, directed towards individuals with mental illness. Unfavorable behaviors manifest as discrimination and are often expressed through avoidance and rejection.3
People with schizophrenia were commonly found to be in a vicious cycle of disability, depression, and reduced self-esteem, where these factors contribute to each other. These challenges have been directly linked to the severity of their symptoms.4 Societal prejudice intensifies the challenges individuals with schizophrenia already endure, potentially hindering their recovery process.5 Previous studies have reported the detrimental effects of social stigma on individuals with schizophrenia. The stigma poses a substantial barrier for those seeking professional psychological assistance, leading to delays in early intervention and treatment.6,7 Furthermore, this stigma is associated with decreased self-esteem and increased depression in individuals with schizophrenia.8 It diminishes their quality of life, impacting daily activities and social interactions. Social stigma prevents the effective integration of individuals with schizophrenia into the broader community.7 Globally, individuals with schizophrenia have reported both anticipated and experienced negative discrimination.9 Rates of experienced discrimination are consistently high across countries and manifest in various domains, including work and interpersonal relationships. The extent of stigma varies across countries and is influenced by sociocultural factors. For example, studies have indicated that China exhibits a higher level of stigmatizing attitudes compared to Japan, while Japan, in turn, demonstrates a higher level of stigmatizing attitudes compared to Taiwan.10,11
In most Arab nations, there is a noticeable stigma and lack of awareness concerning mental health issues as a whole, the available facilities for treatment, and the roles played by mental health service providers.6,12 Several key factors may contribute to the social stigma toward individuals with mental illness. First, sociocultural influences play a considerable role, as many individuals in Arabic countries still hold traditional beliefs linking mental illness to concepts such as divine punishment, the evil eye, demons, paranormal activity, and curses. Moreover, there is a prevailing perception that mental illness brings shame, which discourages individuals from seeking mental health services due to fear of damaging their own and their family’s reputation.13 Second, there is a notable deficiency in specialized training for psychiatrists, coupled with a shortage of mental health professionals in these areas. This lack of resources exacerbates the challenge of providing adequate mental healthcare.14 Third, the ongoing turmoil and humanitarian crises, especially in countries such as Palestine, Yemen, and Syria, impede the establishment and operation of robust mental healthcare systems.15–17
A few studies have reported the pervasive social stigma toward individuals with mental illness in Lebanon. One study investigating the knowledge, attitudes, and behaviors toward these individuals found a high degree of stigma and showed that behaviors were more positive when there was a better understanding of the condition.18 Another study involving 203 Lebanese University undergraduates found prevalent cultural misunderstandings about the causes and treatments of mental illness, including beliefs in magic, the evil eye, and divine punishment as potential causes. The authors also reported a link between misconceptions and the public stigma related to mental illness.6
To the best of our knowledge, there is limited evidence regarding the stigma towards individuals with schizophrenia in Lebanon. Therefore, we aimed to examine the knowledge, attitude, and behavior toward individuals with schizophrenia in a Lebanese population and to explore associated sociodemographic factors with the level of social stigma. We hypothesized that individuals with schizophrenia in Lebanon faced significant stigma across three dimensions, including knowledge, attitudes, and behaviors.
Methods
Study Population and Data Collection
Data collection was performed from January 31, 2023, to February 18, 2023. The inclusion criteria were as follows: 1) living in Lebanon, 2) being between 18 and 65 years, and 3) not having a diagnosis of schizophrenia. We recruited participants using a convenience sampling method, which is a non-probabilistic sampling method where participants are selected for a study based on their accessibility and convenience.19 An online questionnaire was used for data collection, and the link to the questionnaire was shared in WhatsApp, Instagram, and Facebook applications. We recruited participants using a convenience sampling method. Convenience sampling is a non-probabilistic sampling method where participants are selected for a study based on their accessibility and convenience. The study was approved by the Institutional Review Board of the University of Ulsan (IRB No. 2023R0003) and conducted by the Declaration of Helsinki. All participants provided informed consent and retained the right to withdraw from the study at any point.
Questionnaire
The questionnaire consisted of four subsections: 1) demographic information, 2) knowledge, 3) attitude, and 4) behavior. In the demographic subsection, participants were asked to provide details on their age, gender, education level, marital status, area of residency, and personal acquaintance with patients with schizophrenia.
In the knowledge subsection, there were eleven items to assess participants’ knowledge about schizophrenia based on previous studies.20,21 The initial eight items assessed knowledge about the clinical symptoms and courses of schizophrenia. The ninth item explored the causes of schizophrenia, and the tenth item assessed treatment options for schizophrenia. The eleventh item was regarding the main source of knowledge about schizophrenia. We calculated the knowledge score as the sum of the correct answers from the first item to the tenth item. A higher knowledge score was considered to indicate a higher level of knowledge of schizophrenia.
To assess participants’ attitudes toward patients with schizophrenia, a 5-item scale based on the Social Distance Scale (SDS) developed by Link et al was used.2 We presented a vignette and asked participants for their responses to the questions. Each item had three response options: Yes, No, and I do not know. An attitude score was calculated by the sum of all responses to questions for which Yes and No responses were included as −1 and +1 points, respectively. A higher attitude score indicated that the participants tended to have more distance from patients with schizophrenia. We categorized participants with negative attitudes based on an attitude score of 0 from a demarcation threshold.
The Reported and Intended Behavior Scale (RIBS) was used to measure stigma-related behaviors toward patients with schizophrenia. A previous study regarding mental illness trauma showed good reliability, validity, and feasibility of this scale.22 The scale includes two sets of four items each. The initial set had four items about the participants’ past or present experiences in specific domains, including cohabitation, professional interactions, proximity, and personal relationships with individuals with mental health issues. The next set had four items that focused on participants’ future intentions to initiate contact with individuals with mental health problems in the same domains. Each item was coded on a 5-point Likert scale: 1 = strongly disagreed to 5 = strongly agreed. The behavior score was calculated by the sum of the four items of the second set. Participants with a higher behavior score were considered to have more favorable behavior toward patients with schizophrenia.
Statistical Analysis
R software (ver. 4.0.2; R development Core Team, Vienna, Austria) was used for statistical analysis. The significance level was set at p<0.05. For descriptive statistics, continuous and categorical variables are presented as means (standard deviations) and numbers (percentages), respectively. Multiple regression analysis was performed to determine the associations of the knowledge, attitude, and behavior scores with demographic variables and the source of information. In each regression model, the other two scores except for the dependent variable were also included as independent variables.
Results
Demographic Characteristics of the Study Participants
We included a total of 469 participants based on the inclusion criteria. The mean age was 25.6 (7.9) years, and 23.0% were male. A majority of the study participants were single (68.7%), and 81.4% of the participants had graduated from university. Most of the participants (85.7%) responded that they did not know someone with schizophrenia. Table 1 presents the demographic factors of the study population.
 |
Table 1 Demographic Characteristics of the Study Population |
Knowledge About Schizophrenia
The mean knowledge score of the participants was 5.1 ± 2.2. Approximately 66% of the participants had a knowledge score between 4 and 7. The rates of correct answers varied across the individual items in the questionnaire. Only 19.1% of the participants provided the correct answer for the item that stated that patients with schizophrenia suffer from split or multiple personalities. In contrast, 81.8% of the participants responded correctly to the item that stated that patients with schizophrenia have bizarre or inappropriate behavior. A large proportion of the study participants responded that they did not know whether or not patients with schizophrenia have apathy (37.9%) or whether most patients with schizophrenia can be cured (47.9%). Social media was chosen by the largest number of participants (30.1%) among the sources of information. Table 2 presents the responses of the study participants to the questionnaire regarding knowledge about schizophrenia.
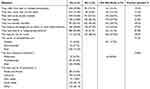 |
Table 2 Responses to the Questionnaire for Knowledge About Schizophrenia |
Attitude and Behavior Toward Individuals with Schizophrenia
Regarding attitude, the mean SDS score was 2.2 ± 2.8. Based on the criterion of 0 as the cutoff for a negative attitude, 72.1% of the study population had a negative attitude toward individuals with schizophrenia. Table 3 presents the responses to the questionnaire regarding attitude toward individuals with schizophrenia.
 |
Table 3 Responses to the Questionnaire for Attitudes Toward Individuals with Schizophrenia |
Regarding behavior, the mean RIBS score was 11.7 ± 3.3. We set the 25th, 50th, and 75th percentiles as the cutoffs for low, medium, and high scores, respectively, for the RIBS scale. Only 13.1% of the participants showed favorable behavior toward individuals with schizophrenia. Table 4 shows the responses to the questionnaire regarding behavior toward individuals with schizophrenia.
 |
Table 4 Responses to the Questionnaire for Behavior Toward Individuals with Schizophrenia |
Factors Associated with the Knowledge, Attitude, and Behavior Scores
Table 5 shows the sociodemographic factors associated with the knowledge, attitude, and behavior scores. Several variables were negatively associated with the knowledge score, including age between 46 and 64 years (β=–1.401, p=0.009), educational attainment of primary school (β=–1.38, p=0.007), information sources except for literature (family and friends: β=–2.366, p<0.001; mass media: β=–1.721, p<0.001; other: β=–2.078, p<0.001; social media: β=–1.897, p<0.001). The knowledge score was positively associated with female gender (β=0.866, p<0.001), a marital status of engaged (β=1.082, p=0.015) and single (β=0.577, p=0.043), knowing someone with schizophrenia (β=1.094, p<0.001), and the behavior score (β=0.084, p=0.012).
 |
Table 5 Associations of the Knowledge, Attitude, and Behavior Scores with Sociodemographic Variables |
Negative associations with the SDS score were found for a marital status of single (β=–0.73, p=0.027), knowing someone with schizophrenia (β=–0.94, p=0.002), and the RIBS score (β=–0.48, p<0.001). Regarding behavior, negative associations with the RIBS score were observed for female gender (β=–0.62, p=0.048), a marital status of single (β=–1.15, p=0.004), age between 30 and 45 years (β=–1.03, p=0.024), the SDS score (β=–0.72, p<0.001), and knowing someone with schizophrenia (β=–0.88, p=0.016). The knowledge score was positively associated with the RIBS scale (β=0.17, p=0.012).
Discussion
To the best of our knowledge, this is the first study to examine social stigma toward individuals with schizophrenia in a Lebanese population. We showed that the study participants had a moderate understanding of schizophrenia, with approximately 75% displaying negative stigmatizing attitudes. A substantial proportion of participants exhibited unfavorable intended behaviors. Several sociodemographic factors were identified as having significant associations with the knowledge, attitude, and behavior scores. Notably, we observed that increased knowledge and more positive attitudes were associated with better behaviors.
The study participants displayed a moderate understanding of schizophrenia with an average knowledge score of 5.1. Approximately, 55% of participants had a score above 5 over 10. This finding aligns with those of prior research conducted in Buenos Aires20 and Columbia21 utilizing the identical knowledge questions. However, these percentages were lower than those from studies conducted in North America and Europe.23–26 A large number of participants held the misconception that schizophrenia is associated with multiple and split personalities. This misconception is consistent with the findings of previous research, suggesting that cultural beliefs and misleading media representations may play a role in this misunderstanding.27,28 Moreover, 40% responded that individuals with schizophrenia are inclined toward violent behavior. In contrast, existing evidence shows that schizophrenia marginally increases the risk of violent behavior and that this risk is accentuated with concurrent alcohol or drug use disorders.29 Such misconceptions might stem from the entertainment industry, which frequently portrays individuals with schizophrenia as unpredictable and aggressive.30 Encouragingly, the majority of participants recognized the optimal treatments for schizophrenia as a combination of psychotherapy and medication and attributed its causes to both genetic and environmental factors. Given these promising insights, further strategies are needed to enhance and disseminate an accurate understanding of the pathophysiology and treatments of schizophrenia to a broader population.
We observed that gender plays a role in knowledge levels, with females showing better understanding than males. This disparity might be due to females’ heightened interest in mental health topics, as reported in several studies.31,32 Age was also associated with the knowledge scores: those older than 46 years displayed lesser awareness than their younger counterparts. This observation mirrors the findings of a Lebanese study that showed reduced knowledge in participants over 70 years old.18 In contrast, a French study reported that knowledge increases with age.31 However, other studies found no significant relationship between age and knowledge.21 The source of information significantly influenced knowledge levels: literature as the primary source was correlated with the most comprehensive understanding. This implied that dissemination of incorrect information about schizophrenia occurred through social media. Individuals whose educational attainments were primary school had lower knowledge levels than those with higher education degrees, aligning with findings in similar studies,20,33 highlighting the positive association between educational attainment and schizophrenia knowledge. No difference in knowledge score was found among different geographic regions in Lebanon. Our findings suggest that awareness campaigns should be widespread throughout the entire country, as a lack of knowledge is prevalent across all areas in Lebanon.
The average SDS score was 2.2, indicating distancing attitudes toward individuals with schizophrenia. Notably, approximately 75% of the participants exhibited negative attitudes toward individuals with schizophrenia. This is consistent with existing literature that emphasizes the prevalent stigma and negative attitudes toward individuals with mental illnesses in Lebanon and many other Arabic nations.12,18 Regarding behavior, the average RIBS score of 11.3 approached the 50th percentile, suggesting a moderately neutral stance. Another study performed in Lebanon that explored perceptions of mental illnesses reported a higher RIBS score of 15.6.18 This finding resonates with those of prior studies that have identified schizophrenia as the most stigmatized condition among various mental health disorders.1
Regarding the sociodemographic factors associated with attitudes and behaviors, we found that females showed a relatively neutral attitude. However, they displayed more unfavorable behaviors toward individuals with schizophrenia, even when considering their higher knowledge level than males. Previous studies have reported mixed results regarding this issue. Li et al found that women showed less stigmatizing behaviors and were more willing to engage with individuals with schizophrenia than men or maintained an attitude as impartial as that of men.34 In contrast, two previous studies adopting the SDS scale and RIBS scale, respectively, did not observe any significant differences in behaviors between the genders.18,20 Wang et al reported that women had more negative implicit attitudes toward mental illness, especially in terms of negative cognition and beliefs, than men.35 However, our finding is limited by the uneven representation of males and females in the study population. Further studies investigating the effect of gender on attitudes and behaviors are needed. One notable finding was the middle-aged group exhibiting lower behavior scores than the younger population. This finding aligns with those of previous research suggesting that behavior toward individuals with mental illnesses may decline with age.36 Marital status of being single was associated with positive attitudes and worse behavior scores. Abolfotouh et al reported similar findings to our results, in which single participants tend to have positive attitudes towards mental illnesses compared to married participants.32 On the other hand, Shanko et al and Taskin et al have shown no significant relationships between marital status and attitudes toward schizophrenia.37,38 Interestingly, knowing someone having schizophrenia was correlated with enhanced knowledge and more favorable attitudes. This finding highlights the influence of personal experiences on attitudes and perceptions. However, we also found that this association did not extend to better behavior scores rather worse behavior scores. This disparity between attitudes and actual behaviors underscores the presence of an attitude-behavior gap in which individuals might hold positive attitudes but struggle to translate them into supportive behaviors. This necessitates further studies to explore potential underlying reasons and to develop interventions that bridge this gap, promoting empathetic and supportive behaviors toward individuals with schizophrenia.
Strength and Limitations
This study examined stigma related to schizophrenia in Lebanon, distinguishing itself as the first of its kind. Our study provides a comprehensive understanding of the study participants’ views on schizophrenia by evaluating their knowledge, attitudes, and behaviors toward individuals with schizophrenia. Several limitations should be acknowledged. First, the cross-sectional design inherently offers a limited depth of evidential support. Second, the study sample was skewed toward the 18–30 age bracket, especially among educated females, due to the online questionnaire distribution method. The overrepresentation suggests that our understanding of stigma in other demographics, including older adults, those with fewer educational attainments, or males, may be restricted. Third, the use of self-reported questionnaires is associated with a possibility of response bias. Fourth, we acknowledged that our scales have not been subjected to linguistic or cultural validation specific to the Lebanese environment. However, the questionnaire we used had been validated by our native researchers to ensure the correct intention of each question. Fifth, we did not assess whether the participants had any mental disorder other than schizophrenia or had a family member with a mental disorder. These factors could also affect the perspective to individuals with schizophrenia.
Conclusion
While the understanding of schizophrenia in Lebanon is moderate, stigmatizing attitudes and behaviors toward individuals with schizophrenia prevail. Notably, although a higher knowledge level was correlated with positive behaviors, a significant divide between attitudes and actual intentions was evident, necessitating further exploration in future studies. Our study aimed at the Lebanese population could contribute to the collective effort to foster inclusive and compassionate societies for individuals with schizophrenia globally. Given our findings, it is important to prioritize educational initiatives, awareness campaigns, and policy changes that foster an inclusive and compassionate society, enabling individuals with schizophrenia to lead enriching lives.
Disclosure
The authors have no potential conflicts of interest to disclose in this work.
References
1. Valery KM, Prouteau A. Schizophrenia stigma in mental health professionals and associated factors: a systematic review. Psychiatry Res. 2020;290:113068. doi:10.1016/j.psychres.2020.113068
2. Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–1333. doi:10.2105/AJPH.89.9.1328
3. Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination? Br J Psychiatry. 2007;190:192–193. doi:10.1192/bjp.bp.106.025791
4. Demirkol ME, Tamam L, Namlı Z, Uğur K, Karaytuğ MO. The mediating effect of depression and disability in the relationship between schizophreniaand self-esteem. Psychiatr Q. 2020;91(2):363–378. doi:10.1007/s11126-019-09706-4
5. Koschorke M, Padmavati R, Kumar S, et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc Sci Med. 2014;123:149–159. doi:10.1016/j.socscimed.2014.10.035
6. Rayan A, Fawaz M. Cultural misconceptions and public stigma against mental illness among Lebanese university students. Perspect Psychiatr Care. 2018;54(2):258–265. doi:10.1111/ppc.12232
7. Rayan A, Obiedate K. The correlates of quality of life among Jordanian patients with schizophrenia. J Am Psychiatr Nurses Assoc. 2017;23(6):404–413. doi:10.1177/1078390317710498
8. Yang LH. Application of mental illness stigma theory to Chinese societies: synthesis and new directions. Singapore Med J. 2007;48(11):977–985.
9. Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet. 2009;373(9661):408–415. doi:10.1016/S0140-6736(08)61817-6
10. Haraguchi K, Maeda M, Mei YX, Uchimura N. Stigma associated with schizophrenia: cultural comparison of social distance in Japan and China. Psychiatry Clin Neurosci. 2009;63(2):153–160. doi:10.1111/j.1440-1819.2009.01922.x
11. Kurumatani T, Ukawa K, Kawaguchi Y, et al. Teachers’ knowledge, beliefs and attitudes concerning schizophrenia- A cross-cultural approach in Japan and Taiwan. Soc Psychiatry Psychiatr Epidemiol. 2004;39(5):402–409. doi:10.1007/s00127-004-0758-0
12. Al-Krenawi A. Mental health practice in Arab countries. Curr Opin Psychiatry. 2005;18(5):560–564. doi:10.1097/01.yco.0000179498.46182.8b
13. Zolezzi M, Alamri M, Shaar S, Rainkie D. Stigma associated with mental illness and its treatment in the Arab culture: a systematic review. Int J Soc Psychiatry. 2018;64(6):597–609. doi:10.1177/0020764018789200
14. Shahda M, Sherra K, Mahmoud E, Elsaid O. Consultation–liaison psychiatric services in Dubai, UAE: a descriptive analysis study. Egypt J Psych. 2016;37:111. doi:10.4103/1110-1105.193017
15. Marie M, Hannigan B, Jones A. Mental health needs and services in the West Bank, Palestine. Int J Ment Health Syst. 2016;10:23. doi:10.1186/s13033-016-0056-8
16. Shoib S, Ullah I, Handuleh JIM, Arafat SMY, Ramalho R. Mental health crisis in Yemen. Asian J Psychiatr. 2021;64:102793. doi:10.1016/j.ajp.2021.102793
17. Hamza MK, Hicks MH. Implementation of mental health services in conflict and post-conflict zones: lessons from Syria. Avicenna J Med. 2021;11(1):8–14. doi:10.4103/ajm.ajm_141_20
18. Abi Doumit C, Haddad C, Sacre H, et al. Knowledge, attitude and behaviors towards patients with mental illness: results from a national Lebanese study. PLoS One. 2019;14(9):e0222172. doi:10.1371/journal.pone.0222172
19. Elfil M, Negida A. Sampling methods in clinical research; an educational review. Emerg. 2017;5:1.
20. Leiderman EA, Vazquez G, Berizzo C, et al. Public knowledge, beliefs and attitudes towards patients with schizophrenia: buenos Aires. Soc Psychiatry Psychiatr Epidemiol. 2011;46(4):281–290. doi:10.1007/s00127-010-0196-0
21. Grandon P, Aguilera AV, Bustos C, Alzate EC, Saldivia S. Evaluation of the stigma towards people with a diagnosis of schizophrenia using a knowledge scale. Rev Colomb Psiquiatr. 2018;47(2):72–81.
22. Evans-Lacko S, Rose D, Little K, et al. Development and psychometric properties of the reported and intended behaviour scale (RIBS): a stigma-related behaviour measure. Epidemiol Psychiatr Sci. 2011;20(3):263–271. doi:10.1017/S2045796011000308
23. Thompson AH, Stuart H, Bland RC, et al. Attitudes about schizophrenia from the pilot site of the WPA worldwide campaign against the stigma of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2002;37(10):475–482. doi:10.1007/s00127-002-0583-2
24. Stuart H, Arboleda-Florez J. Community attitudes toward people with schizophrenia. Can J Psychiatry. 2001;46(3):245–252. doi:10.1177/070674370104600304
25. Arboleda-flórez J. Stigma and discrimination: an overview 2005. World Psychiatry. 2005;4(supplement 1):8–10.
26. Gaebel W, Baumann A, Witte AM, Zaeske H. Public attitudes towards people with mental illness in six German cities: results of a public survey under special consideration of schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2002;252(6):278–287. doi:10.1007/s00406-002-0393-2
27. Schomerus G, Kenzin D, Borsche J, Matschinger H, Angermeyer MC. The association of schizophrenia with split personality is not an ubiquitous phenomenon: results from population studies in Russia and Germany. Soc Psychiatry Psychiatr Epidemiol. 2007;42(10):780–786. doi:10.1007/s00127-007-0235-7
28. Clement S, Foster N. Newspaper reporting on schizophrenia: a content analysis of five national newspapers at two time points. Schizophr Res. 2008;98(1–3):178–183. doi:10.1016/j.schres.2007.09.028
29. Fazel S, Langstrom N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. JAMA. 2009;301(19):2016–2023. doi:10.1001/jama.2009.675
30. Owen PR. Portrayals of schizophrenia by entertainment media: a content analysis of contemporary movies. Psychiatr Serv. 2012;63(7):655–659. doi:10.1176/appi.ps.201100371
31. Durand-Zaleski I, Scott J, Rouillon F, Leboyer M. A first national survey of knowledge, attitudes and behaviours towards schizophrenia, bipolar disorders and autism in France. BMC Psychiatry. 2012;12:128. doi:10.1186/1471-244X-12-128
32. Abolfotouh MA, Almutairi AF, Almutairi Z, et al. Attitudes toward mental illness, mentally ill persons, and help-seeking among the Saudi public and sociodemographic correlates. Psychol Res Behav Manag. 2019;12:45–54. doi:10.2147/PRBM.S191676
33. Economou M, Richardson C, Gramandani C, Stalikas A, Stefanis C. Knowledge about schizophrenia and attitudes towards people with schizophrenia in Greece. Int J Soc Psychiatry. 2009;55(4):361–371. doi:10.1177/0020764008093957
34. Li J, Li J, Thornicroft G, Huang Y. Levels of stigma among community mental health staff in Guangzhou, China. BMC Psychiatry. 2014;14:231. doi:10.1186/s12888-014-0231-x
35. Wang X, Huang X, Jackson T, Chen R. Components of implicit stigma against mental illness among Chinese students. PLoS One. 2012;7:9.
36. Aznar-Lou I, Serrano-Blanco A, Fernandez A, Luciano JV, Rubio-Valera M. Attitudes and intended behaviour to mental disorders and associated factors in Catalan population, Spain: cross-sectional population-based survey. BMC Public Health. 2016;16:127. doi:10.1186/s12889-016-2815-5
37. Shanko A, Abute L, Tamirat T. Attitudes towards schizophrenia and associated factors among community members in Hossana town: a mixed method study. BMC Psychiatry. 2023;23(1):80. doi:10.1186/s12888-023-04555-9
38. Taskin EO, Sen FS, Aydemir O, Demet MM, Ozmen E, Icelli I. Public attitudes to schizophrenia in rural Turkey. Soc Psychiatry Psychiatr Epidemiol. 2003;38(10):586–592. doi:10.1007/s00127-003-0655-y
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
