Back to Journals » Nature and Science of Sleep » Volume 15
Sleep Disturbances in Adolescents with Attention-Deficit/Hyperactivity Disorder
Authors Gruber R, Salamon L, Tauman R, Al-Yagon M
Received 19 August 2022
Accepted for publication 23 January 2023
Published 20 April 2023 Volume 2023:15 Pages 275—286
DOI https://doi.org/10.2147/NSS.S386435
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sarah L Appleton
Reut Gruber,1,2 Liron Salamon,3 Riva Tauman,4 Michal Al-Yagon3
1Department of Psychiatry, McGill University, Montreal, QC, Canada; 2Attention, Behaviour and Sleep Lab, Douglas Mental Health University Institute, Montreal, QC, Canada; 3Department of School Counseling and Special Education, Tel-Aviv University, Tel-Aviv, Israel; 4Sleep Disorders Center, Tel Aviv Souraski Medical Center, Tel Aviv, Israel
Correspondence: Reut Gruber, Department of Psychiatry, McGill University, Montreal, QC, Canada, Email [email protected]
Introduction: Delayed sleep phase syndrome (DSPS) and insomnia disorders are prevalent in adolescents and are comorbid with attention-deficit/hyperactivity disorder (ADHD), but only limited information is available regarding the prevalence of DSPS and insomnia in adolescents with ADHD. Moreover, previous studies comparing objective sleep parameters averaged the findings across all participants of each group (ADHD, control) regardless of each individual’s level of reported sleep disturbance. This might have resulted in inconsistency between information obtained by objective and subjective sleep measures in adolescents with ADHD. The objectives of the present study were 1) to compare the prevalence of risk for DSPS and insomnia in adolescents with ADHD and control adolescents in our samples; 2) to compare objectively measured sleep characteristics of adolescents with ADHD and controls while taking into consideration their levels of risk for DSPS or their level of insomnia; and 3) to compare the ADHD symptom levels of adolescents with moderate/high and low risk for DSPS or insomnia.
Methods: Seventy-three adolescents (37 ADHD, 36 controls) aged 12– 15 years participated in a cross-sectional study. Actigraphy was used to characterize objective sleep parameters and parents’ or adolescents’ reports were used to characterize subjective sleep parameters.
Results: Of the participants in the ADHD and control groups, 33.33% and 27%, respectively, had moderate/high levels of risk for DSPS. Adolescents in the high-risk group for DSPS had an objectively measured delayed sleep schedule and more variable sleep duration, time in bed, and sleep efficiency compared to adolescents in the low-risk group for DSPS, regardless of their ADHD diagnosis. Adolescents with higher levels of insomnia spent more time in bed and had more variable sleep efficiency compared to adolescents with no insomnia, regardless of their diagnosis.
Conclusion: The prevalence of moderate/high risk for DSPS was similarly high in adolescents with ADHD and controls. Participants’ subjective reports of sleep disturbances were consistent with their objective sleep parameters when the type and level of subjectively defined sleep disturbance were considered. ADHD symptom levels were not different in adolescents with moderate/high or low risk for DSPS or insomnia.
Keywords: delayed sleep phase, insomnia, subjective sleep measures, actigraphy
Introduction
Attention-deficit/hyperactivity disorder (ADHD) affects approximately 3–5% of youth.1–3 Biological and psychosocial changes in adolescence have been shown to result in a significant rise in the prevalence of insomnia and the onset of delayed sleep phase sleep syndrome3,4 (DSPS) in the general population of adolescents.5–7 A diagnosis of ADHD has been linked to a wide range of sleep problems,8–12 and it has been proposed that untreated sleep disturbances exacerbate ADHD.13 However, evidence regarding the prevalence or nature of sleep differences among adolescents with ADHD is limited and inconsistent. Most existing studies examining sleep issues in individuals with ADHD have focused on younger children8,14,15 or adults9 and, of those conducted with adolescents, several did not include control samples.11
Findings from studies in adolescents that included ADHD and control groups are inconsistent, with between-group differences observed in subjective sleep measures but not in objective sleep measures.16,17
Studies using subjective measures to examine differences in the circadian preferences of school-age children with ADHD and control children revealed mixed findings. One study conducted in 52 children with ADHD and 52 controls and another study conducted in 26 children with ADHD and 49 controls revealed increased “eveningness” preference in children with ADHD.18,19 In contrast, a subsequent study failed to find any significant difference in the circadian preferences of participants with ADHD (n = 44) or controls (n=243).20 No such study has been conducted in adolescents with ADHD. Moreover, no PSG study has been conducted in children or adolescents with ADHD and circadian rhythms sleep disorders. Meanwhile, two studies conducted by the same investigator using objective measures of circadian preferences in school-age children with ADHD found that melatonin secretion was delayed in children with ADHD compared to controls.21,22
This may reflect that the studies comparing objective sleep parameters averaged the findings across all participants of each group (ADHD, control) regardless of each individual’s level of reported sleep disturbance. This might have masked between-group differences existing between adolescents with and without subjectively defined sleep disturbances.
Clear characterization of the sleep problems of adolescents with ADHD is essential for effective management of ADHD, as untreated sleep disturbances might cause suffering among adolescents and their parents and could exacerbate the severity of symptoms of ADHD. Insufficient and poor-quality sleep are associated with cognitive impairment, poor physical and mental health, increased accidents, and diminished quality of life23–26 Adolescents are particularly vulnerable to such impacts, given the rapid and critical changes that occur in their physical, cognitive, and emotional regulation during this developmental period.27
The objectives of the present study were 1) to compare the prevalence of risk for DSPS and insomnia in adolescents with ADHD and control adolescents in our samples; 2) to compare objectively measured sleep characteristics of adolescents with ADHD and controls while taking into consideration their levels of risk for DSPS or their level of insomnia; and 3) to compare the ADHD symptom levels of adolescents with moderate/high and low risk for DSPS or insomnia.
We hypothesized that 1) The prevalence of adolescents with moderate/high risk for DSPS or insomnia will be higher in the group of adolescents with ADHD compared to controls; 2) Objective sleep parameters of adolescents with ADHD and controls with subjectively reported moderate/high risk for DSPS or insomnia will be poorer than those of adolescents with ADHD and controls with low risk for DSPS or no insomnia; and, 3) The ADHD symptoms of adolescents with a moderate/high risk for DSPS/insomnia will be higher than those of adolescents with little or no risk for sleep disturbances.
Materials and Methods
Participants
A sample of 73 adolescents aged 12–15 years (total mean age = 13.19, SD = 1.3) participated in the study. Thirty-six of the participants were typically developing adolescents (17 boys and 19 girls; mean age=13, SD=0.97), and 37 had ADHD (17 boys, 20 girls; mean age=13.3, SD=0.98).
Of the adolescents with ADHD, 19 (51.4%) had inattentive subtype and 18 (48.6%) had combined subtype; and 56.8% had used medication for ADHD symptoms (5 participants were on dextroamphetamine + amphetamine; 16 were on methylphenidate).
Sixteen percent of the TPD adolescents and 15% of the adolescents with ADHD were from families with an SES below the national average, 26% of each group came from families with an SES at the national average, and 59% of the TPD adolescents and 58% of the adolescents with ADHD were from families with an SES above the national average.
Inclusion criteria for the ADHD group comprised 1) a diagnosis of ADHD based on the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5),3 an ADHD Rating Scale score ≥90th percentile for age and gender,28 and eligibility to be coded as “ADHD” by the Israeli Ministry of Education. For the control group, the inclusion criteria comprised the absence of parental report of any medical, emotional, or academic issue and school confirmation that the student had no academic or behavioral problem.
Exclusion criteria for all participants comprised a major medical condition or impairment; or classification by the Sleep Disorders Inventory for Students – Adolescents (SDIS-A) as having a high risk for obstructive sleep apnea syndrome (OSAS) or periodic limb movement disorder/restless leg syndrome (PLMD/RLS).
Procedure
Recruitment of controls and ADHD participants was done via the school system. 45 Teachers from 29 schools participated in the study. They each invited students and parents to participate in the study via letters. Interested parents and adolescents provided written consent and assent, respectively. In addition, information about the study was disseminated to clinicians attending presentations on ADHD. The study complied with the Declaration of Helsinki and was approved by the Tel-Aviv University Institutional Review Board.
Each participant’s sleep pattern was assessed in the home environment using actigraphy and sleep log for 5 consecutive school nights. Eligible adolescent participants were each given a wristwatch-like actigraph device (Actiwatch 64, Mini-Mitter, Bend, OR, USA) and instructed to wear it on their nondominant wrist at bedtime for 6 consecutive nights. During the same period, they were asked to fill out a daily sleep log in which they indicated their bedtime and wake up time.
Parents were asked to provide demographic information and complete questionnaires regarding their child’s ADHD symptoms, sleep, and daytime behavior.
Measures
Subjective Sleep Measures
The Delayed Sleep Phase Syndrome (DSPS) Subscale of the Sleep Disorders Inventory for Students – Adolescents (SDIS-A)29–31 was completed by the parents to subjectively assess the risk for DSPS. Parents rated the frequency of their child’s sleep behaviors on a 7-point Likert scale. Based on these ratings, each child’s sleep was classified as “normal sleep”, “caution range”, or “high risk” relative to DSPS. Classification into the high-risk group indicates that there is a 90% chance that the teen has DSPS. The scale has a predictive validity of 96%, an internal consistency of 0.92, and a test–retest reliability of 0.86.
The Insomnia Severity Index (ISI),32,33 which is a 7-item self-report scale of insomnia symptoms over the previous 2 weeks, was completed by the adolescents to assess nighttime and daytime symptoms of insomnia. Responses are reported on a Likert scale from 0 to 4, producing total scores of 0–28. Cutoff scores are as follows: 0–7 reflects no clinically significant insomnia, 8–14 indicates subthreshold insomnia, 15–21 suggests moderate-severity insomnia, and 22–28 indicates severe insomnia.34 The scale has been validated for use in adolescents with high internal consistency (α = 0.90) and acceptable test–retest reliability (0.76).35–37
Objective Sleep Measure
Nighttime sleep was monitored by actigraphy, which uses a wristwatch-like device (AW-64 series, Mini-Mitter, Sunriver, OR, USA http://www.actigraphy.respironics.com/solutions/actigraphy.aspx) to evaluate sleep by measuring movement. Actigraphy has been shown to be a reliable method for evaluating sleep in the studied age group.38 The Actiware Sleep 6.1 software (Mini-Mitter) was used to score sleep and wakefulness. This software package applies a sleep-scoring algorithm that was previously validated and found to display a high degree of correspondence with polysomnographic data.39–41 The actigraphic data were analyzed in 1-min epochs. The total number of activity events was computed for each epoch; if the threshold sensitivity value of the mean score during the active period was exceeded, the epoch was scored as awake. Otherwise, the epoch was scored as sleep. The reported bedtime and wake time (provided by sleep logs) were used as the start and end times for the analyses and were set by the researcher based on the sleep log and actigraphy data. Sleep onset and wake up time were calculated by the software. The indices utilized in this study included means and night-to-night variability (standard deviations) measures of 1) the sleep schedule, which was the times of sleep onset and sleep offset (wake up time); 2) the sleep duration, which was the sum of the epochs between sleep onset and sleep end that were scored as “sleep” according to the algorithm; 3) time in bed, which was the interval from the time the subject went to bed (bedtime) to the time the subject arose (wake up time); and 4) the sleep efficiency, which was the time in bed spent sleeping divided by the total time in bed expressed as a percentage.
ADHD symptoms
The ADHD Rating Scale (ADHD-RS) 528 is a parent-report inventory for children and adolescents. It includes two symptom subscales, Inattention and Hyperactivity/Impulsivity, which are rated by parents on a 4-point Likert scale (0 = “never/rarely” to 3 = “very often”). Ratings are summed per subscale, and the subscale ratings are combined to obtain a total score. The scale has high internal consistency (α = 0.94) and test–retest reliability (r = 0.79 to 0.85).28
Demographics and Control Variables
Psychopathology
The Youth Self Report (YSR) Total Problems scale42 is a widely used self-report questionnaire composed of 112 items that assess problem behaviors in adolescents (ages 11–17). Each item has three possible answers (0 = not true, 1 = sometimes true, 2 = often true). Raw scores are converted to T scores: ≤59 is considered in the normal range, while scores of 60–64 are considered bat risk and scores above 65 are considered clinical. It has high test–retest reliability (r = 0.79) and internal consistency (α = 0.83).
Demographic information regarding the caregivers’ education, marital status, and household income was collected through a background questionnaire.
Health information was collected using a parental questionnaire asking about each of the child’s medical issues and related treatment; this questionnaire was designed to allow parents to provide detailed and complete information about any health issue encountered by their child.
Analysis
Tabulations for categorical variables and descriptive statistics for continuous variables were used to present demographic and sleep data for the ADHD and control groups.
Risk Level for DSPS: Participants in the SDIS-A31 caution range and high-risk categories for DSPS were combined into a “moderate/high risk” group, which was compared against the normal sleep group.
Insomnia: Responses on the ISI33,34 were classified into three categories: no clinically significant insomnia (0–7), subthreshold insomnia (8–14), and clinical insomnia (>15).
To test the prevalence of risk for DSPS and insomnia, categorical variables were expressed as percentages and between-group comparisons were performed using the Chi-square test of independence.
Of the adolescents with ADHD, 56.8% (N=21) had used medication for ADHD symptoms (5 participants were on dextroamphetamine + amphetamine and 16 were on methylphenidate). Before proceeding with the multivariate analysis of covariance, we examined the potential confounding influence of medication use on the main study outcomes (subjective and objective sleep measures) to determine whether medications should be retained as covariates in our subsequent analyses. A Chi-square test was used to examine the proportion of adolescents on medication among those with different levels of risk for DSPS or in different insomnia groups.
In addition, a parallel one-way analysis of variance (ANOVA) was conducted to compare actigraphically measured sleep patterns of participants with ADHD on stimulant medication vs medication-naïve participants with ADHD.
To compare objective sleep parameters of adolescents with ADHD and controls having different levels of sleep disturbances, MANCOVAs were conducted on the means and night-to-night variability of actigraphic measures of sleep duration (time in bed, sleep duration), sleep schedule (sleep onset, sleep end), and sleep efficiency, using the Diagnosis (ADHD or control) and Sleep Disturbance Level (DSPS: moderate/high risk or normal sleep; Insomnia: Clinical Insomnia, Subthreshold Insomnia, No Insomnia) as between-subject factors while adjusting for age, medication status, and total YSR score. Post hoc pairwise comparisons were performed using the method of Scheffe.43
To compare the ADHD symptom levels of adolescents with and without reported sleep disturbances, MANCOVAs were conducted on ADHD-RS scores using the Sleep Disturbance Level as a between-subject factor while adjusting for age, medication status, and total YSR score. Post hoc pairwise comparisons were performed using the method of Scheffe.
All statistical analyses were performed using SPSS Statistics for Windows.44
Results
Tables 1 and 2 present the demographic and sleep characteristics of participants in the ADHD and control groups.
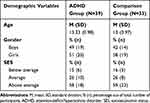 |
Table 1 Demographic of Adolescents with ADHD and Typically Developing Adolescents |
 |
Table 2 Objective Sleep Measures of Adolescents with ADHD and Typically Developing Adolescents without Consideration of Different Levels of Subjectively Reported Sleep Disturbances |
Comparison of Demographics for the ADHD and Control Groups
Socioeconomic Status (SES)
A Chi-square test was used to examine the proportions of adolescents with ADHD and control adolescents coming from families of the different SES levels. The proportion of participants in the different SES groupings did not differ by diagnosis (X2 = 0.09, p > 0.05).
Parent’s Education Level
The average years of education was 17 (SD=2.87) for mothers and 15.8 (SD=2.29) for fathers of participants in the ADHD group, and 17.43 (SD=2.72) for mothers and 16.27 (SD=2.5) for fathers of participants in the control group. MANCOVA was conducted to compare the education levels of mothers and fathers of participants with ADHD and controls. The results revealed that there was no significant difference (F(2, 64) = 0.34, p< 0.72).
Comparison of Actigraphy-Based Sleep Measures Obtained for Boys and Girls
MANOVAs conducted to examine gender differences in actigraphic sleep measures revealed that there was no significant difference (F (5,65)=.47; p>0.47). Actigraphic recordings indicated that for girls, on average, the time in bed was 503.96 min (SD=56.19) per night, actual sleep time was 511.35 min (SD = 48.91 min) per night, sleep onset time was 23:13 (SD=51.03), sleep offset time was 7:12 (SD=44.44), and sleep efficiency was 83.04% (SD=5.33). For boys, on average, the time in bed was 498.66 min (SD=52.02) per night, actual sleep time was 410.23 min (SD = 50.39 min) per night, sleep onset time was 22:50 (SD=147.06 min), sleep offset time was 7:10 (SD=25.31), and sleep efficiency was 82.35% (SD=5.08).
Comparison of Actigraphy-Based Sleep Measures for ADHD and Control Groups Without Consideration of Different Levels of Subjectively Reported Sleep Disturbances
MANOVAs conducted to compare the actigraphic measures of adolescents with ADHD and controls revealed no significant difference (F (5,65)=1.43; p>0.23). Actigraphic recordings indicated that, on average, the time in bed was 511.35 min (SD = 48.91 min) per night for participants in the control group and 493.05 min (SD = 57.40) per night for participants in the ADHD group. The actual sleep time was 426.43 min (SD=34.2) per night for the control group and 402.96 min (SD=52.82) per night for the ADHD group. The mean sleep onset time was 22:40 (SD = 124.31 min) in the control group and 23:22:23 (SD=66.24 min) in the ADHD group. The mean sleep offset time was 7:12:05 (SD = 31:51 min) in the control group and 7:11:04 (41:33) in the ADHD group. Sleep efficiency was 83.7% (SD=4.3) in the control group and 81.92 (SD=5.8) in the ADHD group.
Comparison of Sleep Measures for Stimulant-Treated and Stimulant-Naive Patients
The Chi-square test used to examine the proportion of adolescents on medication among those with different levels of risk for DSPS or in different insomnia groups revealed that the proportion of participants on stimulant medication did not differ by the risk level for DSPS or by insomnia group (X2 (1, N = 36) = 0.99, p > 0.05; X2 (1, N = 36) = 0.82, p > 0.05, respectively).
ANOVA that was conducted to compare actigraphically measured sleep patterns of participants with ADHD on stimulant medication vs medication-naïve participants with ADHD revealed that there was a statistically significant difference in actual sleep time between participants with ADHD on/not on stimulants medication (F(1,35)=4.33, p<0.05). Actigraphic recordings indicated that for medication-naïve participants with ADHD, on average, the time in bed was 509.35 min (SD = 67.01 min) per night, actual sleep time was 418.17 min (SD=56.51) per night, mean sleep onset time was 23:10 (SD = 71.42 min), mean sleep offset time was 7:16:38 (SD = 39:06 min), and sleep efficiency was 82.33% (SD 5.95). For participants with ADHD taking stimulant medications, on average, the time in bed was 479.93 min (SD = 45.7 min) per night, actual sleep time was 390.65 min (SD=47.44) min per night, mean sleep onset time was 23:31 (SD = 61.56 min), mean sleep offset time was 7:06:34 (SD = 43.51 min), and sleep efficiency was 81.58% (SD 5.82). Medication status was therefore used as a covariate in the MANCOVAs performed to test the study’s research questions.
Prevalence of Subjectively Reported Sleep Disturbances in Participants with ADHD and Controls
Moderate/high risk for DSPS was found in 33.33% of the ADHD group and 27% of the control group (p > 0.05). Subthreshold insomnia was found in 46.2% of the ADHD group and 15.2% of the control group (x2 = 8.57, p < 0.02). Clinical insomnia was found in 10.3% of the ADHD group and 9.1% of the control group (p > 0.05).
Comorbidity Between DSPS and Insomnia
Four percent of the participants in the Low risk for DSPS and 26% of the Moderate/high risk for DSPS group had clinical insomnia (x2 = 9.55, p < 0.04).
Objective Sleep Parameters of Participants with ADHD and Controls with Different Levels of Subjectively Reported Sleep Disturbances
Table 3 and Table 4 present descriptive statistics for demographics and actigraphic sleep measures of participants grouped based on their diagnostic status (ADHD or control) and their level of risk for DSPS or insomnia.
 |
Table 3 Objective Sleep Measures of Adolescents with ADHD and Typically Developing Adolescents in Different Risk Levels for Delayed Sleep Phase Syndrome |
 |
Table 4 Objective Sleep Measures of Adolescents with ADHD and Typically Developing Adolescents with Different Levels of Insomnia |
MANCOVAs were conducted to compare actigraphically measured sleep patterns of participants with ADHD and controls in the moderate/high vs low risk for DSPS groups. The results revealed a significant Sleep Disturbance Level main effect for the sleep schedule (F(2, 63) = 4.36, p < 0.01). Post hoc analyses revealed that participants with moderate/high risk for DSPS ended their sleep significantly later in the morning (F(2, 63) = 7.27, p < 0.001) than those of the low risk for DSPS group (sleep offset time: low risk for DSPS 7:04:10 (0:29:34) moderate/high risk for DSPS 7:31:44 (0:47:49), respectively.
DSPS risk level also had a main effect for night-to-night variability (F(5, 59) = 5.57, p < 0.001). The time in bed, actual sleep, and sleep efficiency of participants in the moderate/high DSPS risk group were more variable than those of the low risk for DSPS group (Time in Bed: low risk for DSPS 50.99 minutes, SD=25.31 moderate/high risk for DSPS 80.11 SD=39.87)); (Actual sleep time: low risk for DSPS: 48.2 minutes SD=22.23; moderate/high DSPS risk 66.43 minutes SD=34.33) Sleep Efficiency: low risk for DSPS 3.3% SD=1.55 moderate/high risk for DSPS 4.95% SD=4) F(5, 59) = 11.43, p<0.001 (F(5, 59) = 4.67, p < 0.03), and (F(5, 59) = 5.7, p < 0.02), respectively).
There was no main effect for Diagnosis nor was there any interaction between Diagnosis and Sleep Disturbance Level.
MANCOVAs were conducted to compare actigraphically measured sleep patterns of participants with ADHD and controls having different levels of insomnia symptoms (no insomnia, subthreshold insomnia, or clinical insomnia on the ISI). The results revealed a significant Sleep Disturbance Level main effect on sleep duration (F(2, 61) = 4.43, p < 0.01). Post hoc analyses revealed that participants in the clinical insomnia group spent the most time in bed (528.66 minutes), followed by participants in the subclinical insomnia group (512.41 minutes), and then participants in the no insomnia group, who spent the least amount time in bed (491.35 minutes) (F(1,71) = 5.08, p < 0.007). The actual sleep duration was not significantly different among the three groups. The results revealed also a significant Sleep Disturbance Level main effect for night-to-night variability (F(5, 58) = 2.89, p < 0.02). Post hoc analyses revealed that participants in the clinical insomnia and subthreshold insomnia groups had higher sleep efficiency variability (5% and 4.4%, respectively, than participants in the no insomnia group (3.2%), (F(2,29) = 5.38, p < 0.007).
There was no main effect for Diagnosis, nor was there any interaction between Diagnosis and Sleep Disturbance Level.
ADHD Symptoms of Adolescents with and without Sleep Disturbances
Table 5 and Table 6 present descriptive statistics for the ADHD symptoms of adolescents with and without sleep disturbances.
 |
Table 5 ADHD Symptoms of Adolescents with ADHD in Different Risk Levels for Delayed Sleep Phase Syndrome |
 |
Table 6 ADHD Symptoms of Adolescents with ADHD with Different Levels of Insomnia |
MANCOVAs conducted to compare the ADHD symptom severity levels of participants with different levels of risk for DSPS (moderate/high vs low risk) or insomnia symptoms did not yield any significant findings.
Discussion
This study examined prevalence rates of DSPS and insomnia in adolescents with ADHD and controls, and compared the objective sleep parameters of adolescents with ADHD and controls with high and low levels of parent-reported DSPS and/or self-reported insomnia.
In contrast to the study’s hypothesis, there was no between-group difference in the prevalence of moderate/high risk for DSPS; it was high in both groups. About a third of adolescents in the ADHD (33.33%) and control (27%) groups had moderate/high levels of risk for DSPS. This finding is consistent with a study that found a 26% prevalence rate of DSPS in patients with ADHD,45 and with study showing that evening circadian preference is associated with sleep problems and daytime sleepiness in adolescents with ADHD11 It is also consistent with a recent study showing that circadian typology among typically developing adolescents is skewed towards eveningness.46 Together, the present findings are consistent with the body of research showing that sleep disruptions related with changes in circadian preferences are common in all adolescents beyond their ADHD status (e.g.).47,48
About a tenth of the adolescents in the ADHD (10.3%) and control (9.1%) groups manifested clinical levels of insomnia. This is slightly lower than the rate found by Chiang et al in their ADHD group, but consistent with the prevalence rates of insomnia documented in the general population of adolescents.49,50 The rate of subthreshold insomnia was three times higher in the ADHD group (46.2%) than in the control group (15.2%). Together, the results indicate that 86.2% of the participants with ADHD in the current study had clinical or subclinical levels of insomnia. This prevalence rate is consistent with reports from studies conducted in younger participants with ADHD and with reported clinical impressions.2,4,14,15
This study is the first to consider the participants’ levels of sleep disturbances when comparing their objective sleep parameters. Adolescents with subjectively determined moderate/high risk for DSPS in the ADHD and control groups woke up later in the mornings and had higher night-to-night variability of their sleep duration, time in bed, and sleep efficiency compared to adolescents with ADHD and controls at low risk for DSPS. Similarly, adolescents with higher levels of subjectively determined insomnia symptoms in the ADHD and control groups spent more time in bed despite their sleep being of the same duration as adolescents with no insomnia, and had more variable sleep efficiency compared to those in the ADHD and control groups with no insomnia. These findings are consistent with recent reports that sleep variability (ie, the night-to-night changes in sleep measures within an individual) is as an important feature of insomnia.51,52 Together, these findings show that adolescents with high levels of subjective sleep disturbances had poorer objectively measured sleep, indicating that there is consistency between objective and subjective measures of sleep. Future research is needed to further characterize the daytime functioning of adolescents with high levels of subjective sleep disturbances and poorer objectively measured sleep.
Consistent with study’s hypothesis and with previous studies, comparison of actigraphy-based sleep measures for ADHD and control groups without consideration of different levels of subjectively reported sleep disturbances revealed no significant difference.
The findings of this study showing that risk of later waking and higher variabilities in sleep duration, sleep efficiency, and night-to-night variation in sleep patterns are associated with higher risk for DSPS or insomnia in adolescents in general, beyond their diagnostic group, could support the hypothesis that sleep challenges are transdiagnostic – that is – they extend beyond disorder boundaries. A recent meta-analysis revealed that variability and patterns of sleep quality are associated with daytime behaviors in children with autistic spectrum disorder (ASD).53 Future studies should include objective and subjective sleep measures, as well as measures that examine behavioral problems and daytime functioning in adolescents with ADHD, with the goal of examining the extent to which sleep variability contributes to their daytime challenges.
The study’s findings do not support the idea that sleep disturbances exacerbate symptoms of inattention in adolescents with DSPS54 or insomnia.
Future studies should examine the extent to which the risk for DSPS and insomnia may be increased by modifiable behaviors that are highly prevalent among adolescents in general, and in particular among adolescents with ADHD, such as the increased use of electronic devices at night immediately prior to bedtime.
In addition, such research must further examine the negative bidirectional cycle between the pubertal shift in the circadian system toward a delayed sleep phase and developmental changes in adolescence, including decreased parental control and increased use of electronic devices or alcohol/substance use at night.
The methodological strengths of the study include 1) the use of valid objective sleep measures; 2) the use of valid standardized subjective sleep measures; 3) accounting for the use of medications and psychopathology in the analysis; 4) the inclusion of a well-characterized ADHD sample; 5) the inclusion of an even numbers of boys and girls.
The clinical strengths of the study include 1) the integration of subjective sleep disturbance measures with actigraphy, which is consistent with the American Academy of Sleep Medicine40,55 practice parameters recommending the use of actigraphy to assist in evaluating patients with DSPS or insomnia; 2) the exclusion of any participants with suspected PLMS or OSA.
Clinical Implications
The findings showing that the risk of DSPS is high in adolescents with and without ADHD suggest that assessment of sleep processes and sleep disturbances, particularly the risk for insomnia or DSPS, should be incorporated into the screening processes for all adolescents who present with daytime difficulties.
Given the negative impact of sleep disturbances on adolescents’ mental, cognitive, and physical health, it is essential that clinicians in educational or health settings integrate sleep assessments and interventions into their screening, diagnosis and ongoing care for adolescents, particularly emphasizing this when caring for adolescents with behavioral and functional difficulties.
Limitations
The study’s limitations are as follows: 1) This was a narrowly focused study that did not use probability sampling or a whole-population approach. Broad-focus studies that use probability sampling in representative populations of adolescents should be conducted to obtain prevalence estimates for insomnia and DSPS in adolescents with and without ADHD. 2) The sample size was small and might have limited the detectability of sleep parameter differences in adolescents with ADHD vs controls when subgrouped by their different levels of subjectively determined sleep disturbances. Future studies using larger samples of well-characterized adolescents are needed to identify potential differences between these subgroups. 3) Participants were screened for PLMD or OSA using a parent-based screen rather than polysomnography.
In sum, the current study examined the sleep of adolescents with ADHD and typically developing adolescents using subjective and objective measures. The study found that the prevalence of moderate/high risk for DSPS was similarly high in adolescents with ADHD and controls, and that night-to-night variations in sleep patterns are associated with high risk for DSPS or insomnia in adolescents in general, beyond their diagnostic group. In addition, the results showed that subjective reports of sleep disturbances were consistent with objectively measured sleep parameters when the type and level of subjectively defined sleep disturbance were considered. Our findings highlight the prevalence of sleep and circadian problems in adolescents with and without ADHD, and support the importance of screening for insomnia and DSPS when assessing adolescents with daytime behavioral or attentional problems.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2(2):104–113.
2. Wajszilber D, Santisteban JA, Gruber R. Sleep disorders in patients with ADHD: impact and management challenges. Nat Sci Sleep. 2018;10:453–480. doi:10.2147/NSS.S163074
3. American Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™.
4. Wiggs LD. Chapter 3 - epidemiology and etiology of behavioral insomnias, circadian rhythm disorders, and parasomnias in ADHD. In: Hiscock H, Sciberras E, editors. Sleep and ADHD. Academic Press; 2019:63–93.
5. Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr Clin North Am. 2011;58(3):637–647. doi:10.1016/j.pcl.2011.03.003
6. Andrade MM, Benedito-Silva AA, Domenice S, Arnhold IJ, Menna-Barreto L. Sleep characteristics of adolescents: a longitudinal study. J Adolesc Health. 1993;14(5):401–406. doi:10.1016/s1054-139x(08)80016-x
7. Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–184. doi:10.1016/s1054-139x(02)00506-2
8. Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2006;10(6):381–398. doi:10.1016/j.smrv.2006.03.004
9. Sobanski E. Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. 2006;256(Suppl 1):26–31.
10. Baird AL, Coogan AN, Siddiqui A, Donev RM, Thome J. Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Mol Psychiatry. 2012;17(10):988–995. doi:10.1038/mp.2011.149
11. Becker SP, Kapadia DK, Fershtman CEM, Sciberras E. Evening circadian preference is associated with sleep problems and daytime sleepiness in adolescents with ADHD. J Sleep Res. 2020;29(1):e12936. doi:10.1111/jsr.12936
12. Snitselaar MA, Smits MG, van der Heijden KB, Spijker J. Sleep and circadian rhythmicity in adult ADHD and the effect of stimulants: a review of the current literature. J Atten Disord. 2017;21(1):14–26. doi:10.1177/1087054713479663
13. Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Semin Pediatr Neurol. 1996;3(1):44–50. doi:10.1016/s1071-9091(96)80028-3
14. Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48(9):894–908. doi:10.1097/CHI.0b013e3181ac09c9
15. Martins R, Scalco JC, Ferrari Junior GJ, Gerente J, Costa MDL, Beltrame TS. Sleep disturbance in children with attention-deficit hyperactivity disorder: a systematic review. Sleep Sci. 2019;12(4):295–301. doi:10.5935/1984-0063.20190088
16. Owens J, Sangal RB, Sutton VK, Bakken R, Allen AJ, Kelsey D. Subjective and objective measures of sleep in children with attention-deficit/hyperactivity disorder. Sleep Med. 2009;10(4):446–456. doi:10.1016/j.sleep.2008.03.013
17. Chin WC, Huang YS, Chou YH, et al. Subjective and objective assessments of sleep problems in children with attention deficit/hyperactivity disorder and the effects of methylphenidate treatment. Biomed J. 2018;41(6):356–363. doi:10.1016/j.bj.2018.10.004
18. Durmuş FB, Arman AR, Ayaz AB. Chronotype and its relationship with sleep disorders in children with attention deficit hyperactivity disorder. Chronobiol Int. 2017;34(7):886–894. doi:10.1080/07420528.2017.1329207
19. Gruber R, Fontil L, Bergmame L, et al. Contributions of circadian tendencies and behavioral problems to sleep onset problems of children with ADHD. BMC Psychiatry. 2012;12:212. doi:10.1186/1471-244x-12-212
20. van der Heijden KB, Stoffelsen RJ, Popma A, Swaab H. Sleep, chronotype, and sleep hygiene in children with attention-deficit/hyperactivity disorder, autism spectrum disorder, and controls. Eur Child Adolesc Psychiatry. 2018;27(1):99–111. doi:10.1007/s00787-017-1025-8
21. Van der Heijden KB, Smits MG, Van Someren EJ, Gunning WB. Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder. Chronobiol Int. 2005;22(3):559–570. doi:10.1081/cbi-200062410
22. Van der Heijden KB, Smits MG, Van Someren EJ, Ridderinkhof KR, Gunning WB. Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. J Am Acad Child Adolesc Psychiatry. 2007;46(2):233–241. doi:10.1097/01.chi.0000246055.76167.0d
23. Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S266–82. doi:10.1139/apnm-2015-0627
24. Dutil C, Walsh JJ, Featherstone RB, et al. Influence of sleep on developing brain functions and structures in children and adolescents: a systematic review. Sleep Med Rev. 2018;42:184–201. doi:10.1016/j.smrv.2018.08.003
25. Roeser K, Eichholz R, Schwerdtle B, Schlarb A, Kübler A. Relationship of sleep quality and health-related quality of life in adolescents according to self- and proxy ratings: a questionnaire survey. Front Psychiatry. 2012;3:76. doi:10.3389/fpsyt.2012.00076
26. Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6(1):23–27. doi:10.1016/j.sleep.2004.06.003
27. Kansagra S. Sleep disorders in adolescents. Pediatrics. 2020;145(Suppl 2):S204–s209. doi:10.1542/peds.2019-2056I
28. DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD Rating Scale? 5 for Children and Adolescents: Checklists. Norms, and Clinical Interpretation. Guilford Publications; 2016.
29. Bradley-Klug M, Ferron J, Anderson WM, Benbadis SR. Pediatric sleep disorders: validation of the sleep disorders inventory for students. School Psych Rev. 2008;37(3):409–431. doi:10.1080/02796015.2008.12087886
30. Luginbuehl M, Kohler WC. Screening and evaluation of sleep disorders in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18(4):825–838. doi:10.1016/j.chc.2009.04.012
31. Luginbuehl ML. The Initial Development and Validation Study of the Sleep Disorders Inventory for Students. ProQuest Dissertations & Theses Global; 2003:3116431.
32. Morin CM. Insomnia: Psychological Assessment and Management. Guilford Press; 1993.
33. Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi:10.1093/sleep/34.5.601
34. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi:10.1016/s1389-9457(00)00065-4
35. Alvaro PK, Roberts RM, Harris JK. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. 2014;15(8):934–941. doi:10.1016/j.sleep.2014.03.019
36. Chahoud M, Chahine R, Salameh P, Sauleau EA. Reliability, factor analysis and internal consistency calculation of the Insomnia Severity Index (ISI) in French and in English among Lebanese adolescents. eNeurologicalSci. 2017;7:9–14. doi:10.1016/j.ensci.2017.03.003
37. Chung KF, Kan KK, Yeung WF. Assessing insomnia in adolescents: comparison of Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index. Sleep Med. 2011;12(5):463–470. doi:10.1016/j.sleep.2010.09.019
38. Meltzer LJ, Walsh CM, Traylor J, Westin AM. Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep. 2012;35(1):159–166. doi:10.5665/sleep.1608
39. Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2(5):389–396. doi:10.1016/s1389-9457(00)00098-8
40. Littner M, Kushida CA, Anderson WM, et al. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep. 2003;26(3):337–341. doi:10.1093/sleep/26.3.337
41. Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children’s sleep patterns. Arch Pediatr Adolesc Med. 2008;162(4):350–358. doi:10.1001/archpedi.162.4.350
42. Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. Department of Psychiatry, University of Vermont Burlington; 1991.
43. Enderlein G, Scheffé H. The analysis of variance. Biometrical J. 1961;3(2):2.
44. IBM. SPSS Statistics for Windows. Version 28.0. IBM; 2021.
45. Bijlenga D, van der Heijden KB, Breuk M, et al. Associations between sleep characteristics, seasonal depressive symptoms, lifestyle, and ADHD symptoms in adults. J Atten Disord. 2013;17(3):261–275. doi:10.1177/1087054711428965
46. Saxvig IW, Evanger LN, Pallesen S, et al. Circadian typology and implications for adolescent sleep health. Results from a large, cross-sectional, school-based study. Sleep Med. 2021;83:63–70. doi:10.1016/j.sleep.2021.04.020
47. Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11(3):191–199. doi:10.1046/j.1365-2869.2002.00302.x
48. Carskadon MA, Tarokh L. Developmental changes in sleep biology and potential effects on adolescent behavior and caffeine use. Nutr Rev. 2014;72(Suppl1):60–64. doi:10.1111/nure.12147
49. Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117(2):e247–56. doi:10.1542/peds.2004-2629
50. Chiang HL, Gau SS, Ni HC, et al. Association between symptoms and subtypes of attention-deficit hyperactivity disorder and sleep problems/disorders. J Sleep Res. 2010;19(4):535–545. doi:10.1111/j.1365-2869.2010.00832.x
51. Sánchez-Ortuño MM, Edinger JD. Internight sleep variability: its clinical significance and responsiveness to treatment in primary and comorbid insomnia. J Sleep Res. 2012;21(5):527–534. doi:10.1111/j.1365-2869.2012.01010.x
52. Lemola S, Ledermann T, Friedman EM. Variability of sleep duration is related to subjective sleep quality and subjective well-being: an actigraphy study. PLoS One. 2013;8(8):e71292. doi:10.1371/journal.pone.0071292
53. Whelan S, Mannion A, Madden A, et al. Examining the Relationship Between Sleep Quality, Social Functioning, and Behavior Problems in Children with Autism Spectrum Disorder: A Systematic Review. Nat Sci Sleep. 2022;14:675–695. doi: 10.2147/NSS.S239622
54. Sivertsen B, Harvey AG, Pallesen S, Hysing M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J Sleep Res. 2015;24(1):11–18. doi:10.1111/jsr.12254
55. Morgenthaler T, Alessi C, Friedman L, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30(4):519–529. doi:10.1093/sleep/30.4.519
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
