Back to Journals » Nature and Science of Sleep » Volume 13
Shorter Sleep Predicts Longer Subsequent Day Sedentary Duration in Healthy Midlife Adults, but Not in Those with Sleep Apnea
Authors Thosar SS , Bhide MC , Katlaps I, Bowles NP , Shea SA , McHill AW
Received 29 May 2021
Accepted for publication 14 July 2021
Published 11 August 2021 Volume 2021:13 Pages 1411—1418
DOI https://doi.org/10.2147/NSS.S322459
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Saurabh S Thosar,1– 4 Meera C Bhide,1 Isabel Katlaps,1 Nicole P Bowles,1 Steven A Shea,1,4 Andrew W McHill1,2
1Oregon Institute of Occupational Health Sciences; 2School of Nursing; 3Knight Cardiovascular Institute, School of Medicine; 4OHSU-PSU School of Public Health, Oregon Health and Science University, Portland, OR, 97239, USA
Correspondence: Saurabh S Thosar
Oregon Institute of Occupational Health Sciences, 3181 SW Sam Jackson Park Road, L606/RJH1586, Portland, OR, 97239, USA
Tel +1 503 494-2064
Fax +1 503 494-4278
Email [email protected]
Purpose: Sedentary behavior and suboptimal sleep increase risks for chronic diseases. We hypothesized that sedentary behavior and sleep affect each other and that an underlying sleep disorder would alter these relationships. To test these hypotheses, we studied the bidirectional relationships between sedentary behavior and sleep (duration and efficiency) in healthy controls (HC) and people with untreated obstructive sleep apnea (OSA).
Patients and Methods: Fifty-two volunteers (18 HC, 19 mild OSA [apnea/hypopnea index [AHI] range 5– 14.9/hour], 15 moderate OSA [AHI range 15– 29.9/hour]) were studied with actigraphy and sleep diaries across ∼ 9 consecutive nights of self-selected consistent ∼ 8-hour sleep episodes at home (range 4– 21/nights per person). We analyzed whether total time asleep and sleep efficiency affected the subsequent daytime sedentary duration while controlling for body mass index and whether the severity of OSA altered this relationship. We also tested the reverse relationship, namely whether daytime sedentary duration affected the subsequent night’s sleep and if any such relationship differed with OSA severity.
Results: Overnight sleep duration and efficiency negatively predicted the subsequent day’s sedentary duration in HC (p< 0.02), but not in people with mild or moderate OSA (p> 0.05). There was no significant reverse relationship between daytime sedentary duration and the subsequent night’s sleep duration or efficiency (p≥ 0.2).
Conclusion: In healthy adults, short nighttime sleep predicts a longer duration of sedentary behavior on a subsequent day, but we did not observe this relationship in people with OSA. The mechanisms underlying this association in healthy individuals and its disruption in the presence of OSA need to be studied.
Keywords: sitting time, sedentary behavior, cardiometabolic risk, sleep quality, chronic diseases, sleep disorders
Plain Language Summary
Increased sedentary behavior and poor sleep are associated with increased risk for many chronic diseases. We were interested in exploring how these two common behaviors interact with each other in middle-aged adults. We also included people with sleep apnea, a common condition in this age group. Sleep duration, quality, and physical activity levels were measured for several days using a wrist monitor that senses body position and movement. We discovered that overnight sleep duration and efficiency are inversely associated with subsequent day’s sedentary behavior in healthy participants but not in those with sleep apnea. We did not find a relationship between daytime sedentary behavior and subsequent night’s sleep duration or efficiency. This observational study sets the stage for experimental research to confirm our findings.
Introduction
Prolonged sedentary duration (>6 hours per day) and insufficient sleep (<7 hours per night) and are highly prevalent among US adults.1–3 Both these behaviors independently increase risks for diabetes, cardiovascular disease, and all-cause mortality.4–7 Moreover, it is reasonable that sedentary behavior and sleep affect each other. For instance, it seems possible that after a very active day, an individual is more likely to sleep well on a subsequent night.8 In terms of the reverse association, it is plausible that an individual is more likely to be lethargic after a poor night’s sleep, with increased sedentary behaviors throughout the subsequent day. This latter relationship has been studied in adolescents and young adults; however, the results are not indisputable.9–16 The equivocal results could be due to a lack of objective sleep measurements, differences in experimental protocols, and potential co-occurrence of underlying chronic diseases, including obstructive sleep apnea (OSA). There is likely an intricate interaction between sedentary behavior, sleep, and chronic disease. For instance, habitual insufficient sleep and increased sedentary behavior can increase the risk for obesity, which in turn can increase sedentary behavior, which can also increase the risk for sleep disorders such as OSA.17–20 OSA is highly prevalent in the adult US population and is associated with multiple comorbidities, including diabetes, hypertension, and metabolic syndrome.21–24 Furthermore, people with OSA are more physically inactive than people without OSA, even while controlling for indices of body composition.25,26
As a first step to understanding the interactions between sleep, sedentary behavior, and chronic disease, we tested the hypothesis that nighttime sleep would negatively affect the subsequent day’s sedentary behavior in healthy people at-risk for chronic disease (ie, midlife adults). We also hypothesized that any such relationship observed in healthy people would be altered by the presence of an underlying sleep disorder, namely, untreated OSA without other comorbidities. We also tested the reverse associations that daytime sedentary behavior would negatively affect nighttime sleep in these same groups.
Materials and Methods
These data were collected as part of more extensive studies investigating circadian rhythms and cardiovascular physiology, and we have previously published partial results from two of these studies.27,28 The circadian studies were not powered for these exploratory analyses.
Screening Procedures
This study was conducted in accordance with the Declaration of Helsinki. Oregon Health & Science University’s Institutional Review Board approved all procedures, and each participant signed a written informed consent form before participation.
Fifty-two participants had complete data to be included in the study (Table 1). Based on at-home screening (Itamar Medical Ltd, WatchPAT, Caesarea, Haifa, Israel), 18 participants were healthy controls, 19 had untreated mild OSA (apnea/hypopnea index [AHI] range 5–14.9/hour), and 15 had untreated moderate OSA (AHI range 15–29.9/hour). In a validation against full polysomnography, this WatchPAT device provided 82% positive and 86% negative predictive value for OSA.29 No participant was ever treated with continuous positive airway pressure. We determined participants’ health status via 1) medical history, 2) blood pressure and heart rate measurements, 3) 12 lead electrocardiogram, and 4) fasting blood assay for metabolic and hematological variables, including complete blood count and blood glucose. Body mass index (BMI), calculated as kg/m2, was measured before study participation. 42 of the 52 participants also underwent a physical and psychological exam by a physician. We excluded participants if they were pregnant, had any chronic physical or mental illness, history of smoking, or use of any prescription or non-prescription medication besides birth control as verified by urinalysis of drugs (Speares Medical Inc, Drugsmart 12 panel cup, Alpharetta, GA, USA) and nicotine (Nymox Corporation, NicAlert®, Hasbrouck Heights NJ, USA), or history of travel across more than three time zones in the three months before screening or shift work in the six months before screening.
 |
Table 1 Participant Characteristics |
Sleep Monitoring and Activity Behaviors
Participants’ sleep and activity behaviors were assessed by sleep diary and actigraphy across an average of 9 consecutive nights of self-selected consistent 8 hour sleep periods at home (range 4–21/nights per person). Specifically, we instructed participants to remain in bed for 8 hours, irrespective of whether they were asleep or not, to stabilize the circadian system as these visits occurred before multi-day circadian studies. We checked adherence using: 1) an ActiGraph monitor (Actigraph Corporation, ActiGraph wGT3X-BT, Pensacola, FL, USA), which the participants wore on their non-dominant wrist at all times; 2) phone calls to a time-stamped mailbox at bedtime and upon awakening, and 3) a written sleep diary. We chose to use wrist ActiGraphs due to their ability to simultaneously collect 24-hour activity and sleep data with greater compliance compared to hip monitors.30 Additionally, this monitor is well validated against polysomnography as a tool to measure sleep duration and efficiency in healthy adults and those with OSA.31,32 During this at-home actigraphy monitoring, except for birth control, participants also refrained from over-the-counter medications, health food supplements, caffeinated food and beverages, alcohol, and structured exercise >60 min per day. Adherence to instructions was verified using self-report and sleep diary. Compliance with wearing the ActiGraph was confirmed by a priori criteria using Wear Time Analysis from the ActiLife 6 software. We removed incomplete data from partial days of wearing the device (<22 hours of wear in 24 hours).
Sleep timing, total sleep duration (TSD), and sleep efficiency (SE) were calculated using the Cole-Kripke algorithm in ActiLife 6 with diary sleep/wake times and call-in times to identify the beginning and end of each sleep episode.33 When sleep diary sleep/wake times and call-in times were missing, data for those days were counted as missing data (n=1). We used Freedson Adult 1998 cut-points in ActiLife 6 to define activity levels.34 Sedentary behavior was defined as ≤99 counts per minute of physical activity based on manufacturer guidelines.34,35 We calculated total sedentary duration (TSedD) over 24 hours based on hourly ActiGraph activity counts after accounting for sleep/wake times. TSedD was summed for each hour a participant was awake and classified as sedentary behavior only if most of that hour was spent awake, effectively removing each sleep episode. Classification of wake status for each hour was based on the sleep onset time calculated by the Cole-Kripke algorithm and the out-of-bed time from the sleep diary or call-in.
Statistical Analyses
We included data on participants with at least four days of data, including one weekend day.36 Hours when a participant was asleep (based on sleep onset time from actigraphy and out of bed time from sleep diary or call-in) or when their sleep/wake status was unknown/ambiguous due to missing sleep diary or call-ins were not included in the analysis.
One-way ANOVA tests were used to evaluate differences in TSedD, TSD, SE, and other baseline variables between three groups —HC, mild OSA, and moderate OSA. When a significant main effect was observed, post-hoc tests were used to determine group-specific differences using a Bonferroni correction for multiple comparisons. To test if TSD or SE affected TSedD on the subsequent day, we ran a mixed model analysis with TSedD as the dependent variable, TSD (and separately SE), body mass index (BMI), and group as fixed factors, and participant as a random factor. We included an interaction term of TSD (and separately SE) x group in the model to test if the relationship between TSD (and SE separately) and TSedD is influenced by OSA status. To test if daytime TSedD affected subsequent night’s TSD or SE, we ran similar models with TSD and SE as the independent variables and TSedD as the dependent variable. Although our participants were instructed not to nap during the daytime, we noticed occasional napping based on the sleep diary entries. Therefore, we tested whether nap durations were different between groups and if the results were consistent after removing days when naps occurred. Significance was set at p<0.05. Analyses were performed using Stata 14 (StataCorp LLC, Stata 14, College Station, Texas, USA).
Results
Table 1 describes participants’ characteristics. Table 2 describes mean results by OSA status. Participants wore an ActiGraph monitor on average for at least 22.7-hours per 24-hour day. Overall time in bed was mean 7.97±SD 0.32 h each night. There was no difference between the three groups with regard to number of days of data collected (F(2,49)=0.31, p=0.73), age (F(2,49)=2.61, p=0.08), TSD (F(2,49)=0.18, p=0.83), TSedD (F(2,49)=0.60, p=0.55), SE (F(2,49)=0.46, p=0.63). In line with previous work,37 BMI (F(2,49)=5.45, p=0.007), resting systolic blood pressure (F(2,49)=4.3, p=0.02), diastolic blood pressure (F(2,49)=3.7, p=0.03) heart rate (F(2,49)=4.06, p=0.02), and fasting plasma glucose (F(2,49)=3.97, p=0.03) were different between groups. Post-hoc significant differences were observed only between HC and moderate OSA groups. Two participants with mild OSA and two participants with moderate OSA had a single hypertensive measurement of resting systolic blood pressures. One participant with moderate OSA had a fasting blood glucose of 127 mg/dL, suggestive of diabetes.
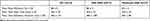 |
Table 2 Activity and Sleep Measures Between Groups |
The overall model examining TSD’s effect on subsequent day’s TSedD trended significance F(5,86)=1.99, p=0.08). There was a significant trend for the interaction between TSD and group (p=0.09), such that TSD negatively predicted subsequent day’s TSedD only in the HC group (p=0.033), but not the mild OSA group (p=0.16) or moderate OSA group (p=0.77). The overall model examining SE’s effect on subsequent day’s TSedD trended significance F(5,79)=2.6, p=0.03). There was a significant interaction between SE and group (p=0.006), such that SE negatively predicted subsequent day’s TSedD only in the HC group (p=0.02), but not the mild OSA group (p=0.72). Specifically, in HC, a one-hour loss in TSD or a ~10% decrease in SE could increase the subsequent day’s TSedD by ~35 minutes. Lastly, we observed a non-significant trend for a positive relationship between SE and the following day’s TSedD in the moderate OSA group (p=0.056; Figure 1).
There was no significant effect of TSedD on subsequent night’s TSD (p=0.7) or SE (p=0.2) in either group. Nap duration was not statistically significant between groups (p>0.1), and even after removing data for days when naps occurred, our results held. The only difference was that the trend in the positive association between SE and subsequent day’s TSedD became statistically significant (and therefore, more robust) for the moderate OSA group (coefficient=+3.66 [95% CI:0.57 to +6.70], p=0.02).
Discussion
Sedentary behavior and insufficient or disrupted sleep are associated with increased risks for chronic disease. We discovered that nighttime sleep duration and efficiency negatively impact subsequent day’s sedentary duration only in healthy individuals, but not in people with untreated mild or moderate sleep apnea. Based on our results, just one hour of sleep loss (totaling 6 h/night of sleep), or low sleep efficiency (totaling 78%/night), such as that in people with insomnia, could increase the subsequent day’s sedentary duration by 35 minutes each day.38 We did not observe a significant association between daytime sedentary behavior and the following night’s sleep parameters, possibly because the participants were on a self-selected fixed ~8-hours/night in bed schedule, thus imposing potential floor or ceiling effects. Whether these results hold in a study without controlled time in bed needs to be evaluated.
It is important to note that the observed relationships existed even after controlling for BMI, which was generally higher in individuals with OSA than HC. There was no significant difference in age between groups in our study, yet people with OSA were slightly older than HC. Therefore, we also reanalyzed our data while including age as a factor, but our results remained nearly identical. We also did not find any difference in daytime sedentary duration, nighttime sleep duration, or sleep efficiency between groups. Nonetheless, as expected, participants with mild and moderate OSA were at greater cardiometabolic risk, as evidenced by increased BMI, blood pressure, heart rate, and fasting plasma glucose level.37 Our participants’ sleep duration and timing were homogenous, including having similar self-selected sleep timings, even in people with OSA. In our study, the average sleep duration for healthy controls was >7 hours, and the sleep efficiency was 88%, which is comparable to normative data in healthy people.39 Moreover, although participants were scheduled to maintain a fixed time in bed, which would be expected to result in sleep duration and efficiency to be identical across the study, we observed small deviations for the time in bed each night (mean time in bed was 7.97±SD 0.32 h/night). To accommodate these deviations and because previous literature has included sleep quality, we included sleep efficiency in our analysis.15 We also included an equal distribution of men and women in our healthy control group and a more than acceptable ratio in the sleep apnea group, as OSA is much more prevalent in men.40 We studied healthy middle-aged people and people with untreated OSA without any other comorbidities (except n=3 mentioned in the methods), making for precise interpretation of these results. Our population was also clinically relevant because midlife adults are likely at increased risk for chronic diseases compared to previously studied low-risk young adults or older adults who already may have developed chronic disease.13–16
A plausible mechanism that may account for the presence of the observed inverse relationship between sleep parameters (TSD and SE) with subsequent day’s TSedD only in healthy controls is one of energy balance. It is well-established that sleep is an energy-conserving state in healthy humans, and overnight sleep deprivation or insufficient sleep results in higher 24-h energy expenditure.41,42 It is also well-established that acute and chronic exercise, which increases energy expenditure during the day, increases sleep duration during the night, even in people with sleep disorders, including sleep apnea.8,43–45 Therefore, we hypothesize that lack of energy conservation during the night (ie, lower sleep duration and efficiency) may lead to increased sedentary behavior (an energy-conserving state) during the day.46 Indeed, there is evidence to suggest that in healthy people, the sleep/wake cycle is impacted by changes in energy homeostasis.47 In people with OSA, the energy homeostasis system is dysfunctional. For instance, OSA is associated with increased resting energy expenditure and increased nighttime energy expenditure, yet people with OSA often gain weight.48–50 Though not statistically significant in our moderate OSA group, there was a positive relationship between SE and daytime sedentary behavior (25 min increase in TSedD per 10% increase in SE), supporting our hypothesis regarding dysfunctional energy balance. In fact, our data of changes in sedentary behavior with differing levels of OSA may suggest a dose-response effect of severity of OSA on the relationship between nighttime sleep parameters and daytime sedentary behavior. Further work, including 24-hour energy expenditure measurement, is needed to test these hypotheses and uncover potential metabolic mechanisms driving these relationships. Our results have potential significance for understanding mechanisms underlying chronic disease. For instance, based on our results, the relationship between poor sleep efficiency and chronic disease could be modulated by sedentary behavior. Future studies need to experimentally determine the separate effects of these behaviors on cardiometabolic parameters.
It is unclear how previous work in this field has handled daytime naps.13–16 Daytime napping is physiologically different from simple daytime sedentary behavior and can also affect nighttime sleep.51 The presence of naps did not have a significant effect on our results.
Several strengths and limitations of our study need to be considered for the full interpretation of the results. Our study’s strength is that participants self-selected an ~8-hour in-bed schedule rather than letting their sleep times fluctuate. This methodology enabled us to examine how sedentary duration and sleep duration/efficiency affected each other during a controlled sleep schedule across the three groups, thereby controlling for confounders such as changes in circadian timing of the sleep episode that could disrupt sleep.52 On the other hand, it is possible that a strict 8-hour schedule in bed could change activity patterns. Our participants’ timing and duration of sleep and activity episodes and the number of days of data were not different, pointing to a homogenous sample for these variables. Furthermore, to control any participant level variability, we included “participant” as a random variable. We could not collect food logs and did not directly measure energy expenditure, which could potentially help explain some of the findings. We also did not collect qualitative details on posture, exercise, occupational status, or sedentary behavior domains (eg, occupational, leisure, or travel). The cutoff of 99 counts per minute to define sedentary behavior in accelerometry analysis is commonly used in the field yet can potentially underestimate sedentary time (~5%, according to one report).35 There is a debate on the best positioning of activity devices and cut points while measuring 24-hour behaviors.53 We used wrist actigraphy to simultaneously measure both sleep and activity for multiple days in one device. We also used the Freedson Adult 1998 activity cut-points that were originally developed for hip actigraphy for activity without a clear standard for wrist-based devices.34,54,55 We note that the lack of population-specific cut-points for defining sedentary behavior using wrist actigraphy is a limitation. There are potential limitations of creating sleep apnea groups based on one night of AHI using a home sleep device, and we included AHI as a continuous variable to overcome this limitation. Our sample size per group is also somewhat limited, and future experimental studies can be powered using this work. Even though we examined subsequent day’s sedentary duration and subsequent night’s sleep parameters, our study was observational, and causality needs to be tested in future investigations.
Our observations shed light on the intertwined nature of sedentary behavior, sleep, and activity. Given the Centers for Disease Control and Prevention (CDC) recommendations for reducing sedentary behavior and increasing moderate-vigorous intensity physical activity to at least 150 minutes a day, it is especially salient to consider these behavioral factors together. To further health-promoting behaviors at a population level, we need to understand how these factors affect each other at an individual level.56
Conclusion
In conclusion, nighttime sleep duration and efficiency are negatively associated with subsequent day’s sedentary duration only in healthy individuals but not in people with untreated sleep apnea. This work lays the foundation for further mechanistic evaluation into energy expenditure abnormalities accompanying obstructive sleep apnea.
Acknowledgments
We thank volunteer participants for their time and efforts.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work is supported by NIH grants R01 HL125893, HL140577, HL142064, K01 HL146992, K01 HL151745, KL2 TR002370, UL1TR000128, R35 HL155681, and by the Oregon Institute of Occupational Health Sciences at Oregon Health & Science University via funds from the Division of Consumer and Business Services of the State of Oregon (ORS 656.630).
Disclosure
The authors have no financial or other competing interests. We declare that the study results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
1. Yang L, Cao C, Kantor ED, et al. Trends in sedentary behavior among the US population, 2001–2016. JAMA. 2019;321(16):1587–1597. doi:10.1001/jama.2019.3636
2. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. doi:10.1016/j.sleh.2014.12.010
3. Liu Y. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:137–141.
4. Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–867. doi:10.1001/archinte.165.8.863
5. Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. doi:10.1001/archinte.163.2.205
6. Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–1492.
7. Katzmarzyk PT, Powell KE, Jakicic JM, et al. Sedentary behavior and health: update from the 2018 Physical Activity Guidelines Advisory Committee. Med Sci Sports Exerc. 2019;51(6):1227.
8. Kubitz KA, Landers DM, Petruzzello SJ, Han M. The effects of acute and chronic exercise on sleep. Sports Med. 1996;21(4):277–291.
9. Booth JN, Bromley LE, Darukhanavala AP, Whitmore HR, Imperial JG, Penev PD. Reduced physical activity in adults at risk for type 2 diabetes who curtail their sleep. Obesity. 2012;20(2):278–284.
10. Bromley LE, Booth JN, Kilkus JM, Imperial JG, Penev PD. Sleep restriction decreases the physical activity of adults at risk for type 2 diabetes. Sleep. 2012;35(7):977–984. doi:10.5665/sleep.1964
11. Van Dyk TR, Krietsch KN, Saelens BE, Whitacre C, McAlister S, Beebe DW. Inducing more sleep on school nights reduces sedentary behavior without affecting physical activity in short-sleeping adolescents. Sleep Med. 2018;47:7–10. doi:10.1016/j.sleep.2018.03.007
12. Garaulet M, Ortega F, Ruiz J, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes. 2011;35(10):1308–1317. doi:10.1038/ijo.2011.149
13. Romney L, Larson MJ, Clark T, Tucker LA, Bailey BW, LeCheminant JD. Reduced sleep acutely influences sedentary behavior and mood but not total energy intake in normal-weight and obese women. Behav Sleep Med. 2016;14(5):528–538. doi:10.1080/15402002.2015.1036272
14. Bailey BW, Deru LS, Christensen WF, et al. Evaluating relationships between sleep and next-day physical activity in young women. J Phys Act Health. 2020;17(9):874–880. doi:10.1123/jpah.2020-0014
15. Kakinami L, O’Loughlin EK, Brunet J, et al. Associations between physical activity and sedentary behavior with sleep quality and quantity in young adults. Sleep Health. 2017;3(1):56–61. doi:10.1016/j.sleh.2016.11.001
16. Madden KM, Ashe MC, Lockhart C, Chase JM. Sedentary behavior and sleep efficiency in active community-dwelling older adults. Sleep Sci. 2014;7(2):82–88. doi:10.1016/j.slsci.2014.09.009
17. Bullock VE, Griffiths P, Sherar LB, Clemes SA. Sitting time and obesity in a sample of adults from Europe and the USA. Ann Hum Biol. 2017;44(3):230–236. doi:10.1080/03014460.2016.1232749
18. Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med. 2012;42(3):e3–e28. doi:10.1016/j.amepre.2011.10.020
19. Simpson L, McArdle N, Eastwood PR, et al. Physical inactivity is associated with moderate-severe obstructive sleep apnea. J Clin Sleep Med. 2015;11(10):1091–1099. doi:10.5664/jcsm.5078
20. Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H, Smith PL. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc. 2008;5(2):185–192. doi:10.1513/pats.200708-137MG
21. Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi:10.1016/j.smrv.2016.07.002
22. Huang T, Lin BM, Stampfer MJ, Tworoger SS, Hu FB, Redline S. A population-based study of the bidirectional association between obstructive sleep apnea and type 2 diabetes in three prospective US cohorts. Diabetes Care. 2018;41(10):2111–2119. doi:10.2337/dc18-0675
23. Hou H, Zhao Y, Yu W, et al. Association of obstructive sleep apnea with hypertension: a systematic review and meta-analysis. J Glob Health. 2018;8(1):010405. doi:10.7189/jogh.08.010405
24. Qian Y, Xu H, Wang Y, Yi H, Guan J, Yin S. Obstructive sleep apnea predicts risk of metabolic syndrome independently of obesity: a meta-analysis. Archiv Med Sci. 2016;12(5):1077–1087. doi:10.5114/aoms.2016.61914
25. Igelström H, Emtner M, Lindberg E, Åsenlöf P. Physical activity and sedentary time in persons with obstructive sleep apnea and overweight enrolled in a randomized controlled trial for enhanced physical activity and healthy eating. Sleep Breath. 2013;17(4):1257–1266. doi:10.1007/s11325-013-0831-6
26. Hargens TA, Martin RA, Strosnider CL, Giersch GEW, Womack CJ. Obstructive sleep apnea negatively impacts objectively measured physical activity. Sleep Breath. 2019;23(2):447–454. doi:10.1007/s11325-018-1700-0
27. Thosar SS, Berman AM, Herzig MX, Roberts SA, Lasarev MR, Shea SA. Morning impairment in vascular function is unrelated to overnight sleep or the inactivity that accompanies sleep. Am J Physiol Regulat Integr Compar Physiol. 2018;315(5):R986–R993. doi:10.1152/ajpregu.00143.2018
28. Thosar SS, Rueda JF, Berman AM, et al. Separate and interacting effects of the endogenous circadian system and behaviors on plasma aldosterone in humans. Am J Physiol Regulat Integr Compar Physiol. 2019;316(2):R157–R164.
29. Yuceege M, Firat H, Demir A, Ardic S. Reliability of the watch-PAT 200 in detecting sleep apnea in highway bus drivers. J Clin Sleep Med. 2013;9(4):339–344. doi:10.5664/jcsm.2584
30. Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48(13):1019–1023.
31. Full KM, Kerr J, Grandner MA, et al. Validation of a physical activity accelerometer device worn on the hip and wrist against polysomnography. Sleep Health. 2018;4(2):209–216.
32. Morgenthaler T, Alessi C, Friedman L. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30(4):519–529. doi:10.1093/sleep/30.4.519
33. Barger LK, Flynn-Evans EE, Kubey A, et al. Prevalence of sleep deficiency and use of hypnotic drugs in astronauts before, during, and after spaceflight: an observational study. Lancet Neurol. 2014;13(9):904–912.
34. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi:10.1097/00005768-199805000-00021
35. Atkin AJ, Gorely T, Clemes SA, et al. Methods of measurement in epidemiology: sedentary behaviour. Int J Epidemiol. 2012;41(5):1460–1471. doi:10.1093/ije/dys118
36. Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S68. doi:10.1249/MSS.0b013e3182399e5b
37. Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569–576.
38. Lichstein KL, Stone KC, Donaldson J, et al. Actigraphy validation with insomnia. Sleep. 2006;29(2):232–239.
39. Luca G, Haba Rubio J, Andries D, et al. Age and gender variations of sleep in subjects without sleep disorders. Ann Med. 2015;47(6):482–491.
40. Won CH, Reid M, Sofer T, et al. Sex differences in obstructive sleep apnea phenotypes, the multi-ethnic study of atherosclerosis. Sleep. 2020;43(5):zsz274. doi:10.1093/sleep/zsz274
41. Markwald RR, Melanson EL, Smith MR, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci. 2013;110(14):5695–5700.
42. Jung CM, Melanson EL, Frydendall EJ, Perreault L, Eckel RH, Wright KP. Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans. J Physiol. 2011;589(1):235–244.
43. Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–449.
44. Iftikhar IH, Kline CE, Youngstedt SD. Effects of exercise training on sleep apnea: a meta-analysis. Lung. 2014;192(1):175–184. doi:10.1007/s00408-013-9511-3
45. Yang P-Y, Ho K-H, Chen H-C, Chien M-Y. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother. 2012;58(3):157–163.
46. Newton JRL, Han H, Zderic T, Hamilton M. The energy expenditure of sedentary behavior: a whole room calorimeter study. PLoS One. 2013;8(5):e63171.
47. Collet T-H, van der Klaauw AA, Henning E, et al. The sleep/wake cycle is directly modulated by changes in energy balance. Sleep. 2016;39(9):1691–1700. doi:10.5665/sleep.6094
48. De Jonge L, Zhao X, Mattingly MS, et al. Poor sleep quality and sleep apnea are associated with higher resting energy expenditure in obese individuals with short sleep duration. J Clin Endocrinol Metab. 2012;97(8):2881–2889.
49. Bamberga M, Rizzi M, Gadaleta F, Grechi A, Baiardini R, Fanfulla F. Relationship between energy expenditure, physical activity and weight loss during CPAP treatment in obese OSA subjects. Respir Med. 2015;109(4):540–545.
50. Phillips BG, Hisel TM, Kato M, et al. Recent weight gain in patients with newly diagnosed obstructive sleep apnea. J Hypertens. 1999;17(9):1297–1300. doi:10.1097/00004872-199917090-00009
51. Campbell SS, Murphy PJ, Stauble TN. Effects of a nap on nighttime sleep and waking function in older subjects. J Am Geriatr Soc. 2005;53(1):48–53.
52. Dijk DJ, Czeisler CA. Paradoxical timing of the circadian rhythm of sleep propensity serves to consolidate sleep and wakefulness in humans. Neurosci Lett. 1994;166(1):63–68.
53. Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–1845.
54. Staudenmayer J, He S, Hickey A, Sasaki J, Freedson P. Methods to estimate aspects of physical activity and sedentary behavior from high-frequency wrist accelerometer measurements. J Appl Physiol. 2015;119(4):396–403.
55. Koster A, Shiroma EJ, Caserotti P. Comparison of sedentary estimates between activPAL and hip- and wrist-worn actigraph. Med Sci Sports Exer. 2016;48(8):1514–1522. doi:10.1249/MSS.0000000000000924
56. Prevention CfDCa. Physical activity: benefits of physical activity. Website; 2021. Available from: https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

