Back to Journals » Nature and Science of Sleep » Volume 15
Short Sleep Duration is Associated with Prolonged Virus Shedding in SARS-CoV-2 Omicron-Infected Patients
Authors Lin YN, Zhou LN, Liu ZR , Wang Y, Li SQ , Lu FY, Zhang L , Li QY
Received 18 March 2023
Accepted for publication 23 June 2023
Published 7 July 2023 Volume 2023:15 Pages 547—554
DOI https://doi.org/10.2147/NSS.S411677
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Ying Ni Lin,1,2,* Li Na Zhou,1,2,* Zhuo Ran Liu,3,* Yi Wang,1,2 Shi Qi Li,1,2 Fang Ying Lu,1,2 Liu Zhang,1,2 Qing Yun Li1,2
1Department of Respiratory and Critical Care Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 20025, People’s Republic of China; 2Institute of Respiratory Disease, Shanghai Jiao Tong University School of Medicine, Shanghai, 200025, People’s Republic of China; 3Department of Thyroid and Vascular Surgery, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 200025, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qing Yun Li, Department of Respiratory and Critical Care Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 200025, People’s Republic of China, Tel +81-21-64370045, Email [email protected]
Purpose: Sleep disturbance has been implicated in poor prognosis of coronavirus disease 2019 (COVID-19), but less is known about the influence of short sleep duration on COVID-19 outcomes. We aim to investigate whether short sleep duration is associated with prolonged virus shedding duration in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron-infected patients.
Patients and Methods: A total of 270 patients with a laboratory confirmed COVID-19 diagnosis during SARS-CoV-2 Omicron-predominant period were recruited. Self-reported sleep duration of the patients was collected. The two-way analysis of variance (ANOVA) was used to determine the interactions between sleep duration and variables, and multivariate logistic regression analysis was used to analyze the effect of independent variables on longer virus shedding duration.
Results: The two-way ANOVA revealed a significant sleep duration × snoring interaction effect for virus shedding duration, and a sleep duration × sex interaction effect for virus shedding duration. Multivariate logistic regression model illustrated that patients sleeping < 6 h were at greater risk of prolonged virus shedding duration compared to those sleeping ≥ 6 hours (OR = 1.80, 95% CI = 1.01– 3.26), independent of age, sex, co-existing diseases, vaccination condition, and antiviral treatment.
Conclusion: Short sleep duration (< 6 h) was associated with increased virus shedding in SARS-CoV-2 Omicron-infected patients.
Keywords: sleep duration, SARS-CoV-2 Omicron, COVID-19 pandemic
Introduction
Pandemic coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has lasted for more than 2 years and led to unprecedented public health and socioeconomic crisis. SARS-CoV-2 Omicron, which is a predominately prevalent strain, is responsible for the resurgence of outbreaks in the world due to its dramatically increased transmissibility.1 Omicron causes a high rate of asymptomatic infection and mild COVID-19,2 however, some asymptomatic or mild COVID-19 patients showed a prolonged virus shedding duration. Factors influencing virus shedding duration in SARS-CoV-2 Omicron-infected patients remain largely unknown.
Sleep plays a critical role in maintaining immune system homeostasis and host defense.3 Poor sleep is believed to increase susceptibility to infection.4 A high prevalence of COVID-19 patients complaint of sleep disturbance,5 which in turn, is associated with a slower recovery from lymphopenia, longer hospitalization, and an increased need for intensive care unit (ICU) care in COVID-19 patients.6 Sleep is also related to persistent COVID-19 symptoms.7 Compared with the short COVID-19 patients, the long COVID-19 patients experienced more sleep alterations, including insomnia, sleep quality, daytime sleepiness, nightmares, and sleep apnea.8 Apart from sleep disturbance, short sleep could impair immune function. Short sleep may deregulate immune responses with increased pro-inflammatory signaling, which contributes to an increased risk of onset and/or worsening of infection.4 Compared with individuals sleeping for 7–8 h, those sleeping ≤5 h are more likely to report a head or chest cold9 and pneumonia.10 After an experimental rhinovirus challenge, individuals sleeping ≤6 h are at greater risk of developing the cold.11 Moreover, a systemic review demonstrated that individuals sleeping less than 7 h are more prone to have upper airway respiratory tract infections.12 A link between sleep duration and increased COVID-19 susceptibility is shown using multivariable Mendelian randomization.13 Indeed, extremes of sleep duration are associated with greater odds of COVID-19 infection in a general population.14 However, whether short sleep affects the outcomes of COVID-19 is still unknown. In this study, we aimed to investigate the association between sleep duration and virus shedding duration in SARS-CoV-2 Omicron-infected patients.
Obstructive sleep apnea (OSA) is a common sleep disorder. Patients with OSA experience approximately 8-fold greater risk for COVID-19, and in COVID-19 patients, OSA increases the risk of hospitalization and developing respiratory failure.15 Preexisting sleep apnea is also associated with elevated risk for long COVID-19.16 Evidence has shown that sleep duration and OSA could have additive or synergistic effects on brain health and cardiovascular consequences.17,18 Loud snoring during sleep could be an indicator of OSA. In this study, we evaluated the association between sleep duration and virus shedding duration in SARS-CoV-2 Omicron-infected snorers and non-snorers, and determined whether snoring is an exacerbating factor in any demonstrated relationship between sleep duration and virus shedding duration.
Materials and Methods
Participants and Data Collection
A total of 270 patients with a laboratory confirmed COVID-19 diagnosis (positive SARS-CoV-2 polymerase chain reaction for throat-swab specimens) who were admitted to Ruijin Hospital Cancer (Proton) Center during SARS-CoV-2 Omicron-predominant period (from April 1st 2022 to May 15th 2022) were recruited in the study. The inclusion criteria included: (1) Patients aged between 18 and 65 years; (2) Patients conform to the diagnosis of COVID-19 and were clinically classified as mild type according to the Novel Coronavirus Diagnosis and Treatment Protocol for Pneumonia (Trial Edition 9). The exclusion criteria included: (1) Patients with a history of mental illness and a prior cancer diagnosis; (2) Patients with a history of immune deficiency disease, or use of immunosuppressants or glucocorticoids in the last 3 months; (3) Pregnant or lactating women. The demographic data on age, sex, body mass index (BMI), coexisting diseases, and COVID19 vaccination status were collected upon admission. Additionally, data on symptoms at disease onset, treatment, and blood routine parameters within 24 h of admission were obtained. Virus shedding duration was defined as the period between the date of diagnosis or symptom onset and the date when Ct values of N gene and ORF gene determined by reverse transcription-polymerase chain reaction test (RT-PCR) were reported to be >35 twice consecutively on nasopharyngeal swabs (sampling interval being at least 24 h). The protocol for the study was approved by the ethics committee of Ruijin Hospital and complied with the Declaration of Helsinki. Informed consent was obtained from all patients prior to inclusion.
Assessment of Sleep Habits
All patients were asked to report their average sleep duration in the past 6 months with the following choices to pick: <6 h, ≥6 h to ≤7 h, >7 h to ≤8 h, >8 h. Daytime sleepiness was assessed using Epworth Sleepiness Scale (ESS), which is a self-reported questionnaire of eight questions. The score ranging from 11 to 15 indicates moderate daytime sleepiness, and the score ranging from 16 to 24 refers to severe daytime sleepiness.19 The probability of obstructive sleep apnea (OSA) was assessed using STOP-Bang score, which consists of eight questions, including snoring, daytime tiredness, observed apnea, hypertension, BMI > 35kg/m2, age >50 years old, neck circumference >40 cm, and male, and is scored ranging from 0 to 8.20 In addition, patients were asked “Do you snore during sleep?”.
Statistical Analysis
Statistical analysis was performed using R software (Version 4.2.0). Continuous variables were described using mean and standard error of mean (SEM). The differences between the two groups were compared using Student’s t-test. Two-way ANOVA was used to determine the interactions between sleep duration and variables including age, sex, snoring, coexisting disease, COVID-19 vaccination, and antiviral treatment. Categorical variables were described as number and percentage, and the percentages of categorical variables among groups were compared using Chi-square test. The average virus shedding duration was 14.23 days. Binary logistic regression analysis was used to analyze the effect of independent variables on longer virus shedding duration (>14 days = “1”, ≤14 days =“0”). We initially used a univariate binary logistic regression model to examine the independent variables, including age, sex, snoring, coexisting disease, COVID-19 vaccination, and antiviral treatment, related to longer virus shedding duration. Variables without collinear problems were added into the multivariate binary logistic regression model. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated to determine the association between long virus shedding duration and potential factors. The p value <0.05 was considered significant.
Results
A total of 270 patients were recruited in the study. According to National Sleep Foundation’s sleep time duration recommendations, 7–9 h are recommended for young adults and adults, while <6 h or >10 h are inappropriate sleep.21 A cutoff of 6 h of sleep has been shown to be associated with significant morbidity and mortality.11,22,23 Thus, we categorized the patients into two groups: <6 h (n=77) and ≥6 hours (n=193). Demographic characteristics of the patients are shown in Table 1. Patients sleeping ≥6 h were slightly younger than those sleeping <6 h. No difference was observed in sex, BMI, percentage of snorers, average ESS scores, coexisting diseases (hypertension and/or diabetes), rate of COVID19 vaccination, rate of asymptomatic infection, and percentage of antiviral treatment between the two groups. Patients sleeping <6 h presented with a slightly higher neutrophil count and a lower lymphocyte percentage than those sleeping ≥6 h. No difference was detected in the other blood routine parameters.
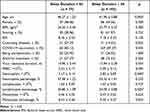 |
Table 1 Demographic Characteristics and Blood Routine Parameters on Hospital Admission of Patients |
Compared with patients sleeping ≥6 h, patients sleeping <6 hours showed a longer virus shedding duration (Table 1). The two-way ANOVA revealed a significant sleep duration × snoring interaction effect (p = 0.010, Table 2) and a sleep duration effect (p = 0.046) for virus shedding duration. The average STOP-Bang score in snores was 3.55 ± 0.15 with 73.12% scoring ≥3 and was significantly higher than that in non-snorers (1.28 ± 0.08 with 10.01% scoring ≥3), indicating a high frequency of co-existing OSA in the snoring subgroups. LSD post-hoc tests indicated that non-snorers sleeping <6 h had a longer virus shedding duration than non-snorers sleeping ≥6 h (p = 0.002), while in patients sleeping ≥6 h, snores showed a prolonged virus shedding compared to non-snores (p = 0.010). A significant sleep duration × sex interaction effect (p = 0.038) and a sleep duration effect (p = 0.045) were also found for virus shedding duration. Post hoc analysis showed that sleeping <6 h prolonged virus shedding duration in males (p = 0.004), and in patients sleeping <6 h, males presented with a longer virus shedding duration than females (p = 0.006). Moreover, a significant age effect was detected for virus shedding duration (p = 0.001, Table 2). Post hoc analysis revealed that sleeping <6 h delayed virus shedding in patients aged younger than 45 years (<6 h vs ≥6 h, p = 0.020), and in patients sleeping ≥6 h, those aged older than 45 years presented with longer virus shedding (p < 0.001). A significant effect of vaccination status was also detected for virus shedding duration (p = 0.032, Table 2), and post hoc analysis showed a longer virus shedding duration in unvaccinated patients than those vaccinated in sleeping ≥6 h group (p = 0.042).
 |
Table 2 Comparisons of Virus Clearance Duration Among Groups |
Compared with those sleeping ≥6 h, patients sleeping <6 h showed a higher percentage of patients with longer virus shedding duration (>14 days) (<6 h vs ≥6 h, 54.55% vs 40.93%, P = 0.042). The association between potential influence factors and long virus shedding duration is shown in Table 3. The univariate logistic regression showed that age ≥45 years, sleeping <6 hours, being COVID-19 vaccinated, and antiviral treatment were associated with long virus shedding duration. Sex (p = 0.088), snoring, and coexisting disease did not significantly affect virus shedding duration. Considering the sex disparity of COVID-19–related morbidity and mortality,24 sex was included in the multivariate logistic regression model. We also entered sleep duration × snoring interaction and sleep duration × sex interaction in the models, but the interactions did not show any significant association with virus shedding duration >14 days. Thus, neither sleep duration × snoring interaction nor sleep duration × sex interaction was included in the multivariate logistic regression model. Sleeping <6 h was an independent predictor for long virus shedding duration (OR = 1.80, 95% CI = 1.01–3.26, P = 0.047), while being female (OR = 0.58, 95% CI = 0.34–0.97, P = 0.039), being vaccinated (OR = 0.36, 95% CI = 0.15–0.80, P = 0.016), and having received antiviral treatment (OR = 0.46, 95% CI = 0.27–0.79, P = 0.005) were protective factors against prolonged virus shedding duration.
 |
Table 3 Risk Factors for Longer Virus Shedding Duration (>14 Days) Using Univariate and Multivariate Analysis |
Discussion
In this study, we illustrated an association between sleep duration and virus shedding duration in SARS-Cov-2 Omicron-infected patients. Logistic regression analysis revealed that short sleep is an independent risk factor for long virus shedding duration. There were also significant interactions between sleep duration and snoring and between sleep duration and sex for virus shedding duration.
Insufficient sleep is believed to increase the risk of infection. Individuals sleeping <7 h in the weeks preceding an exposure to a rhinovirus is 2.94 times more likely to develop a cold than those sleeping ≥8 h.25 A recent meta-analysis also demonstrated that sleeping for less than 7–9 h is associated with increased upper respiratory tract infections.12 In a prospective cohort study of female nurses, sleeping ≤5 h and ≥9 h both increase the risk of pneumonia.10 Adolescents with short sleep (around 6 h) reported more common illness bouts (cold, flu-like, gastroenteritis, and menstrual pain) than those with long sleep (around 7 h).26 Few studies have reported the association between sleep duration and the outcomes of infectious diseases. A study using the UK Biobank showed that the ORs of long or short sleep duration (compared to normal sleep) are greater than one, although not significant, for mortality after COVID-19.27 Also, persistent short nighttime sleep <6 h is associated with increased long COVID-19 risk.28 In the study, we observed that SARS-CoV-2 Omicron-infected patients sleeping <6 h had longer virus shedding duration than those sleeping ≥6 h. Compared to those sleeping ≥6 h, patients sleeping <6 h were 1.80 times more likely to have longer virus shedding when considering potential factors. We were unable to analyze the effects of long sleep on virus shedding because of the low frequency of responses to >8 h in the cohort. We also noticed that patients sleeping <6 h were sleepier than those sleeping ≥6 h during the day, which could be a sign of chronic insufficient sleep. Daytime sleepiness is also found to be a risk for COVID-19 hospitalization.29
The mechanism underlying the link between short sleep and prolonged virus shedding in SARS-CoV-2 Omicron-infected patients is still unknown. One plausible mechanism could be the adverse effect of insufficient sleep on immune system. Sleep deprivation suppresses the differentiation and immune activity of cytotoxic cells, restrains monocyte differentiation, and upregulates several inflammatory genes.30 Sleep duration is inversely associated with levels of circulating cytokines including CRP, IL-6 an IL-5,31–33 indicating a pro-inflammatory status in short sleepers. The effect of short sleep on immune cell counts remains controversial. A study showed an increase in total WBC and neutrophil and monocyte counts,31 while another study reported no association between sleep duration and total WBC counts.32 In the study, we detected a slightly higher neutrophil count and a lower lymphocyte percentage in patients who slept <6 h than in patients sleeping ≥6 h. Another possible mechanism could be that short sleep duration is associated with reduced clinical protection after vaccination against viral infections.34,35 Short sleep duration lowers specific antibody titers' response to vaccination against H1N136 and hepatitis B viruses.37 In this study, we observed that COVID-19 vaccination accelerated virus shedding in SARS-CoV-2 Omicron-infected patients. Vaccinated patients sleeping <6 h had a longer duration of virus shedding than those sleep ≥6 h, indicating a possible impact of short sleep on efficacy of COVID-19 vaccination. However, future research that analyzes the association between sleep duration and antibody titers after COVID-19 vaccination and control for factors including vaccination shots and post-vaccination duration should be conducted to clarify the effects of short sleep on efficacy of COVID-19 vaccination.
Snoring is one of the major symptoms of OSA, and more than two-third snorers in the study reporting a Stop-bang score ≥3 indicated a high frequency of co-existing OSA in the snoring subgroups. OSA is considered to be a risk factor for COVID-19 infection and worse outcomes.15,38 In this study, we detected significant interactions between sleep duration and snoring for virus shedding duration. Snoring delayed virus shedding in patients sleeping ≥6 h, and in non-snorers, patients sleeping <6 h had a longer duration of virus shedding than those sleep ≥6 h. Co-existing with OSA in snoring subgroups may weaken the potential protective effect of longer sleep and prolong virus shedding in SARS-CoV-2 Omicron-infected patients, possibly through dysregulating immune function and inflammatory response.39
Sex differences have been reported in the associations between sleep duration and adverse health consequences, which may be attributed to sex-specific hormonal and behavioral differences.40,41 In this study, we detected significant interactions between sleep duration and sex for virus shedding duration. Sleeping <6 h prolonged virus shedding duration in males but not in females, and in patients sleeping <6 h, males presented with a longer virus shedding duration than females. The results indicated that the impact of short sleep on virus shedding is more pronounced in males than in females. One explanation is the greater biological need for males than for females.42 Lack of sleep may be more likely to cause adverse health outcomes in males.43 Another explanation could be sex differences in innate and adaptive immune responses, with males generally more susceptible to infections than females.44 Indeed, recent studies have reported the sex disparity of COVID-19–related morbidity and mortality, with a male-to-female case fatality ratio ranging from 1.6 to 2.8.24 Short sleep may intersect with sex to worsen the COVID-19–related outcomes.
There were several limitations. Firstly, this was a cross-sectional study, which made us unable to determine the causality. Secondly, sleep duration of the patients was self-reported using a single question, which could induce report bias in the variable. Some prospective measures (sleep diaries/sleep log) were also lacking in the study. Thirdly, no information was provided on daytime and night-time sleep, sleep efficiency, sleep quality, nor psychological variables that can modulate sleep parameters. These sleep and psychological characteristics, other than sleep duration, may affect virus shedding in patients. We did not have information on circadian preference (eg chronotype and the regularity of circadian rhythm), which has been shown to be important in the COVID-19–related health consequences.45,46 Fourthly, we could not determine whether short sleep of the patients occurs as a result of changes in lifestyle during COVID-19 pandemic or just as a trait-like feature of sleep behavior. Moreover, future studies with a larger sample size and a longitudinal design should be conducted to determine the association between sleep duration and long-term prognosis of Omicron-infected patients.
Conclusion
We showed that short sleep (<6 h) was associated with increased virus shedding in SARS-CoV-2 Omicron-infected patients after controlling for age, sex, co-existing diseases, vaccination condition, and antiviral treatment.
Abbreviations
COVID-19, Corona Virus Disease 2019; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; ICU, Intensive Care Unit; BMI, Body Mass Index; RT-PCR, Reverse Transcription-Polymerase Chain Reaction Test; ESS, Epworth Sleepiness Scale; OSA, Obstructive Sleep Apnea; ORs, Odds Ratios; 95% CIs, 95% Confidence Intervals; ANOVA, Analysis of Variance.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (82070089, 82000091); Shanghai Municipal Key Clinical Specialty (shslczdzk02202); Shanghai Top-Priority Clinical Key Disciplines Construction Project (2017ZZ02014); Shanghai Key Laboratory of Emergency Prevention, Diagnosis and Treatment of Respiratory Infectious Diseases (20dz2261100); Cultivation Project of Shanghai Major Infectious Disease Research Base (20dz2210500). We thank Dr Baisong Wang from Department of Biological Statistics, Shanghai Jiao Tong University School of Medicine for confirmation of the statistical approach in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gowrisankar A, Priyanka TMC, Banerjee S. Omicron: a mysterious variant of concern. Eur Phys J Plus. 2022;137(1):100. doi:10.1140/epjp/s13360-021-02321-y
2. Garrett N, Tapley A, Andriesen J, et al. High rate of asymptomatic carriage associated with variant strain omicron. medRxiv. 2022. doi:10.1101/2021.12.20.21268130
3. Bryant PA, Trinder J, Curtis N. Sick and tired: does sleep have a vital role in the immune system? Nat Rev Immunol. 2004;4(6):457–467. doi:10.1038/nri1369
4. Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. 2021;4:1304. doi:10.1038/s42003-021-02825-4
5. Lin YN, Liu ZR, Li SQ, et al. Burden of sleep disturbance during COVID-19 pandemic: a systematic review. Nat Sci Sleep. 2021;13:933–966. doi:10.2147/NSS.S312037
6. Zhang J, Xu D, Xie B, et al. Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: a retrospective cohort study. Brain Behav Immun. 2020;88:50–58. doi:10.1016/j.bbi.2020.05.075
7. Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi:10.1016/j.eclinm.2021.101019
8. Scarpelli S, De Santis A, Alfonsi V, et al. The role of sleep and dreams in long-COVID. J Sleep Res. 2023;32:e13789. doi:10.1111/jsr.13789
9. Prather AA, Leung CW. Association of insufficient sleep with respiratory infection among adults in the United States. JAMA Intern Med. 2016;176(6):850–852. doi:10.1001/jamainternmed.2016.0787
10. Patel SR, Malhotra A, Gao X, Hu FB, Neuman MI, Fawzi WW. A prospective study of sleep duration and pneumonia risk in women. Sleep. 2012;35(1):97–101. doi:10.5665/sleep.1594
11. Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38(9):1353–1359. doi:10.5665/sleep.4968
12. Robinson CH, Albury C, McCartney D, et al. The relationship between duration and quality of sleep and upper respiratory tract infections: a systematic review. Fam Pract. 2021;38(6):802–810. doi:10.1093/fampra/cmab033
13. Peng L, Jing J, Ma J, He S, Gao X, Wang T. Insomnia and sleep duration on COVID-19 susceptibility and hospitalization: a Mendelian randomization study. Front Public Health. 2022;10:995664. doi:10.3389/fpubh.2022.995664
14. Quan SF, Weaver MD, Czeisler M, et al. Insomnia, poor sleep quality, and sleep duration and risk for COVID-19 infection and hospitalization. Am J Med. 2023. doi:10.1016/j.amjmed.2023.04.002
15. Maas MB, Kim M, Malkani RG, Abbott SM, Zee PC. Obstructive sleep apnea and risk of COVID-19 infection, hospitalization and respiratory failure. Sleep Breath. 2021;25(2):1155–1157. doi:10.1007/s11325-020-02203-0
16. Mandel HL, Colleen G, Abedian S, et al. Risk of post-acute sequelae of SARS-CoV-2 infection associated with pre-coronavirus disease obstructive sleep apnea diagnoses: an electronic health record-based analysis from the RECOVER initiative. Sleep. 2023. doi:10.1093/sleep/zsad126
17. Kim REY, Abbott RD, Kim S, et al. Sleep duration, sleep apnea, and gray matter volume. J Geriatr Psychiatry Neurol. 2022;35:47–56. doi:10.1177/0891988720988918
18. Lutsey PL, Norby FL, Gottesman RF, et al. Sleep apnea, sleep duration and brain MRI markers of cerebral vascular disease and Alzheimer’s Disease: the Atherosclerosis Risk in Communities Study (ARIC). PLoS One. 2016;11(7):e0158758. doi:10.1371/journal.pone.0158758
19. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
20. Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–821. doi:10.1097/ALN.0b013e31816d83e4
21. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43.
22. Park S, Lee S, Kim Y, et al. Short or long sleep duration and CKD: a Mendelian randomization study. J Am Soc Nephrol. 2020;31(12):2937–2947. doi:10.1681/ASN.2020050666
23. St-Onge M-P, Grandner MA, Brown D, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American heart association. Circulation. 2016;134(18):e367–e386. doi:10.1161/CIR.0000000000000444
24. Haitao T, Vermunt JV, Abeykoon J, et al. COVID-19 and Sex Differences: Mechanisms and Biomarkers. Mayo Clin Proc. 2020;95(10):2189–2203. doi:10.1161/CIR.0000000000000444
25. Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB. Sleep habits and susceptibility to the common cold. Arch Intern Med. 2009;169:62–67.
26. Orzech KM, Acebo C, Seifer R, Barker D, Carskadon MA. Sleep patterns are associated with common illness in adolescents. J Sleep Res. 2014;23(2):133–142. doi:10.1111/jsr.12096
27. Li P, Zheng X, Ulsa MC, et al. Poor sleep behavior burden and risk of COVID-19 mortality and hospitalization. Sleep. 2021;44(8). doi:10.1093/sleep/zsab138
28. Xue P, Merikanto I, Chung F, et al. Persistent short nighttime sleep duration is associated with a greater post-COVID risk in fully mRNA-vaccinated individuals. Transl Psychiatry. 2023;13:32.
29. Liu Z, Luo Y, Su Y, et al. Associations of sleep and circadian phenotypes with COVID-19 susceptibility and hospitalization: an observational cohort study based on the UK Biobank and a two-sample Mendelian randomization study. Sleep. 2022;45(6). doi:10.1093/sleep/zsac003
30. Liu X, Chen B, Huang Z, et al. Effects of poor sleep on the immune cell landscape as assessed by single-cell analysis. Commun Biol. 2021;4(1):1325. doi:10.1038/s42003-021-02859-8
31. Pérez de Heredia F, Garaulet M, Gómez-Martínez S, et al. Self-reported sleep duration, white blood cell counts and cytokine profiles in European adolescents: the HELENA study. Sleep Med. 2014;15(10):1251–1258. doi:10.1016/j.sleep.2014.04.010
32. Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, et al. Sleep duration and emerging cardiometabolic risk markers in adolescents. The AFINOS study. Sleep Med. 2011;12(10):997–1002. doi:10.1016/j.sleep.2011.05.009
33. Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40–52. doi:10.1016/j.biopsych.2015.05.014
34. Benedict C, Cedernaes J. Could a good night’s sleep improve COVID-19 vaccine efficacy? Lancet Respir Med. 2021;9(5):447–448. doi:10.1016/S2213-2600(21)00126-0
35. Akhtar N, Srivastava RK, Shrivastava D. How losing sleep following vaccination may weaken the response to SARS-CoV vaccines. Sleep Vigil. 2022;6:1–3. doi:10.1007/s41782-022-00198-0
36. Benedict C, Brytting M, Markström A, Broman JE, Schiöth HB. Acute sleep deprivation has no lasting effects on the human antibody titer response following a novel influenza A H1N1 virus vaccination. BMC Immunol. 2012;13:1. doi:10.1186/1471-2172-13-1
37. Prather AA, Hall M, Fury JM, et al. Sleep and antibody response to hepatitis B vaccination. Sleep. 2012;35:1063–1069. doi:10.5665/sleep.1990
38. Mashaqi S, Lee-Iannotti J, Rangan P, et al. Obstructive sleep apnea and COVID-19 clinical outcomes during hospitalization: a cohort study. J Clin Sleep Med. 2021;17(11):2197–2204. doi:10.5664/jcsm.9424
39. Salles C, Lopes JR, Neves M, Brito RS, Bacelar A. Is there a link between COVID-19 and obstructive sleep apnea? Sleep Sci. 2021;14(3):299–302. doi:10.5935/1984-0063.20200078
40. Huang L, Long Z, Xu G, et al. Sex-specific association of sleep duration with subclinical indicators of metabolic diseases among asymptomatic adults. Lipids Health Dis. 2022;21:16. doi:10.1186/s12944-022-01626-w
41. Gonzales JU, Elavsky S, Cipryan L, Jandačková V, Burda M, Jandačka D. Influence of sleep duration and sex on age-related differences in heart rate variability: findings from program 4 of the HAIE study. Sleep Med. 2023;106:69–77. doi:10.1016/j.sleep.2023.03.029
42. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. doi:10.1093/sleep/27.7.1255
43. Svensson T, Saito E, Svensson AK, et al. Association of sleep duration with all- and major-cause mortality among adults in Japan, China, Singapore, and Korea. JAMA Netw Open. 2021;4(9):e2122837. doi:10.1001/jamanetworkopen.2021.22837
44. Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–638. doi:10.1038/nri.2016.90
45. Leone MJ, Sigman M, Golombek DA. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol. 2020;30(16):R930–R931. doi:10.1016/j.cub.2020.07.015
46. Salfi F, Lauriola M, D’Atri A, et al. Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci Rep. 2021;11(1):11416. doi:10.1038/s41598-021-90993-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
