Back to Journals » Journal of Pain Research » Volume 17
Shifts in Students’ Attitudes Towards Pain Patients, Pain, and Opioid Management Following a Dedicated Medical School Pain Curriculum
Authors Durbhakula S, Wang TY, Segna KG, Limerick GR, Broachwala MY, Schatman ME , Zaidi MA, Siddarthan IJ, Toy S
Received 2 November 2023
Accepted for publication 26 February 2024
Published 2 March 2024 Volume 2024:17 Pages 827—835
DOI https://doi.org/10.2147/JPR.S447671
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Timothy Atkinson
Shravani Durbhakula,1 Tony Y Wang,2 Kara G Segna,2 Gerard R Limerick,2,3 Mustafa Y Broachwala,3 Michael E Schatman,4 Munfarid A Zaidi,5 Ingharan James Siddarthan,6 Serkan Toy7
1Department of Anesthesiology, Division of Pain Medicine, Vanderbilt University Medical Center, Nashville, TN, USA; 2Department of Anesthesiology & Critical Care Medicine, Johns Hopkins School of Medicine, Baltimore, MD, USA; 3Department of Physical Medicine & Rehabilitation, Johns Hopkins School of Medicine, Baltimore, MD, USA; 4Department of Anesthesiology, Perioperative Care, and Pain Medicine, New York University Grossman School of Medicine, New York, NY, USA; 5Department of Anesthesiology, Baylor College of Medicine, Houston, TX, USA; 6Department of Anesthesiology, Weill Cornell Medicine, New York, NY, USA; 7Departments of Basic Science Education and Health Systems & Implementation Science, Virginia Tech Carilion School of Medicine, Roanoke, VA, USA
Correspondence: Shravani Durbhakula, Department of Anesthesiology, Division of Pain Medicine, Vanderbilt University Medical Center, Nashville, TN, USA, Email [email protected]
Objective: To examine the immediate effects of a comprehensive pain course on medical students’ pre-existing perceptions and attitudes toward pain patients and opioid management.
Methods: First-year medical students at a major academic medical center enrolled in a required pre-clerkship pain course in June 2020 and completed pre- and post-course online surveys with Likert-scale questions about their attitudes toward pain management and opioid-related issues. Additionally, the surveys included a free-text question where the students listed the first five words that came to mind when hearing the word “opioids”. These words were categorized as “professional” or “lay” words and further as having “positive”, “negative”, or “neutral” connotations. Data analyses included descriptive statistics, as well as non-parametric and parametric tests.
Results: Fifty-four of the 119 students responded to pretest and posttest surveys and were included in paired analyses. There was a significant difference between the number of professional words used before (M=1.21, SD=0.97) and after the course (M=2.40 SD=1.33); t(52)=− 6.39, P< 0.001. Students also used more lay-positive words after the course (M=0.81, SD=0.63) than they used pre-course (M=0.23, SD=0.43); t(51)=− 5.98, P< 0.001. Students’ post-course responses to several key Likert-scale questions showed significant shifts toward more positive attitudes about caring for patients with pain. For example, students acknowledged greater comfort in providing opioids for chronic pain (P< 0.001) where appropriate, and enhanced interest in handling complex pain cases (P< 0.001).
Conclusion: Results showed that a comprehensive, multi-disciplinary pain course could greatly enhance first-year medical students’ attitudes toward pain management, chronic pain patients, and the complex issues surrounding opioids.
Keywords: medical education, opioids, stigma, epidemic, biases, pain
Introduction
Over 100 million Americans suffer from unremitting chronic pain—exceeding the number of Americans affected by heart disease, cancer, and diabetes combined.1 The annual economic burden of chronic pain falls between 560 and 635 billion United States dollars. Pain mismanagement—particularly in relation to the opioid crisis—has inflicted substantial individual and public health damage, while being associated with higher pharmacy, emergency department, inpatient, and total healthcare costs.2
There are 5,871 pain medicine physicians actively practicing. Using data from the United States (US) Census Bureau, we calculate 56,453 Americans per pain medicine physician in contrast to 20,366 per oncologist and 14,717 per cardiologist.3 Unfortunately, 20% of patients with severe chronic pain never reach a pain specialist;4 those who do experience a 7.8-year average delay post-referral, seeing an average of 8 other physicians first.4 Pain management pervasively falls on the shoulders of primary care practitioners, surgeons, oncologists, and others without formal pain training. With unfilled American pain medicine fellowship positions tripling in the last three years,5 effective pain management will more frequently be expected from those without the appropriate skillsets—exponentiating pain-related mistakes and economic burden.
Despite this, pain education in North American medical schools lacks standardization and robustness. The Association of American Medical Colleges’ Curriculum Inventory, a self-reporting curriculum database for medical schools, reveals that 75% of US schools included the topic of “pain management” in at least one required pre-clerkship or clerkship experience from 2019–2020.6 However, the inventory fails to characterize the learning experience’s nature (unclear whether students received one lecture, a dedicated course, or other experience). A study of 117 US and Canadian medical schools found that only 4% had a dedicated pain course, and a mere 16% offered optional pain electives.4,7 Per the literature, US medical schools average 11 total hours of undefined pain education across a 4-year curriculum.7 By comparison internationally, Australian and New Zealand medical schools report a collective median of 20 hours of pain education over four-years, with 53% offering a dedicated pain management elective ranging from 2 to 6 weeks long.8 Pain education in European medical schools varies across countries, with France standing out; 87% of French schools (compared to only 4% of North American schools4,7) provide a 12-hour dedicated pain course supplemented with 7.5 hours of undedicated pain education.9
Striking pain treatment disparities exist in relation to race, ethnicity, gender, and geography. For instance, a 2019 meta-analysis analyzing over 7,000 emergency medicine patients found that Black patients were 35% less likely to receive pain medication than their White counterparts for similar conditions.10 These disparities are rooted in biases and misinformation—which education can address. For instance, a 2016 study showed that 40% of a cohort of 92 White first- and second-year medical students endorsed the false belief that “Black people’s skin is thicker than White people’s”, and 8% percent wrongly believed that “Black people’s nerve endings are less sensitive than Whites”.11
Pain sufferers also experience stigma from providers, which can affect treatment outcomes and compound disparities.12 Patients feel undermined when expressing pain,12 and dismissal of complaints can impede diagnostic diligence and delay treatment.13 Per the National Academy of Sciences, education reduces stigma. Anti-stigma interventions in pain require the systematic presentation of factual information about painful conditions and dispelling of myths.14
Acknowledging the need for better pain education and its power to counteract stigmas and disparities, the Johns Hopkins School of Medicine (JH) mandates a unique, multi-disciplinary, and comprehensive pain course for all first-year medical students. This manuscript primarily examines the immediate effects of the JH curriculum on medical students’ pre-existing perceptions and attitudes toward pain patients and pain management. Secondarily, it evaluates the course’s feasibility in both live and virtual formats.
Methods
This one-group pretest-posttest survey study was conducted in June 2020, approved by Johns Hopkins Institutional Review Board (with IRB # 00251269).
Participants
All 119 first-year medical students were enrolled in this course at the Johns Hopkins School of Medicine in the last month of medical school year one and were eligible and invited to participate in this study. Before taking the survey, students reviewed an IRB-approved letter explaining the study’s purpose, data use, and information protection. Participation in the survey was optional, and the letter stated that participation served as consent.
Course Format
This 21-hour, 4-day pain course is positioned after neurology to facilitate the understanding of pain pathways. Strategically, it integrates with the larger four-year medical school curriculum which includes synergistic components: a formal one-hour opioid-awareness training prior to the pain course in year-one, a separate 15-hour pre-clerkship course on addiction in year-two, and a 1.5-hour pain medicine refresher in year-three prior to surgical clerkship.
The curriculum’s original components were published in 2011 but its effectiveness was not evaluated.15 Since its conception, the course has been updated to reflect the latest developments in the field and revised based on feedback received from structured reviews (conducted yearly by the Office of Medical Student Curriculum and every five years by the Student Assessment and Program Evaluation Committee). For instance, lectures and discussions were added in 2017 on stigma and unconscious bias in pain medicine, as well as gender, ethnic and racial disparities in pain treatment. Methods include lectures, interactive sessions with patient encounters, small group exercises with faculty, podcasts, and games. The course is pass/fail, with passing defined as a score of 70% or higher on a multiple-choice knowledge exam and attendance at all sessions.
The learning objectives of the course are to: 1) develop knowledge and skills in the assessment and treatment of pain; 2) identify evidence-based pharmacological and non-pharmacological therapies that may be effective in managing acute and chronic pain; 3) understand the risks and benefits of using opioid analgesics and why these medicines require intensive scrutiny and monitoring during treatment, including the monitoring of problem behaviors; and 4) describe the potential role for non-physicians in the management of acute and chronic pain, recognizing how physicians can collaborate with other team members to manage pain.
In response to the COVID-19 pandemic, the course was transitioned into a fully virtual format in 2020. The online course combined synchronous and asynchronous sessions and continued incorporating unique features such as faculty-led small groups, patient cases, and games using institutional HIPAA-protected Zoom and Blackboard accounts. A major difference was that the in-person course featured live patient interactions, while the virtual course included pre-recorded patient encounters. The content and style of each course session were replicated from the previous year using instructional design solutions from the Johns Hopkins Office of Online Learning.
Survey Instrument
Students were given a pre-course and post-course survey using Qualtrics software (https://www.qualtrics.com, Qualtrics, Provo, Utah) to evaluate the immediate influence of this online course on students’ attitudes towards pain management, chronic pain patients, and the complex issues surrounding opioids. The survey followed established survey development guidelines for educational research.16,17 Prior to taking the survey, students were asked to provide a unique identifier, which was used to link their pre- and post-course responses while still maintaining their anonymity. The survey also gathered basic demographic information, such as age, gender, and their current specialty of choice.
To address the study objectives, the survey included both free text and quantitative Likert scale responses. The free text question asked students to write down the first five words that came to their minds when they heard the word “opioids”. Students were also asked to use a 5-point Likert scale to evaluate their level of agreement (from strongly disagree to strongly agree) with statements about the characteristics/behaviors of chronic pain patients, the effects of treating chronic pain patients on career satisfaction and wellbeing, the likelihood of treatment successes in pain medicine, and the realities of opioid prescribing.
Data Analysis
Only data from students who responded to both pre- and post-course surveys were included in analyses.
Analysis of First Five Words Related to “Opioids” (Word Categorization & Word Clouds)
The free text responses for pre-course and post-course surveys were categorized as either “professional” words or “lay” words and further categorized as words with a “positive” connotation, “negative” connotation, or “neutral” connotation. Categorization of each word into one of six groups was manually performed by two healthcare professionals independently. They later met and discussed any discrepancies to achieve consensus. A non-healthcare professional served as a tiebreaker where needed. To mitigate bias, the reviewers were blinded to the source of the response words, whether they were from pre- or post-course surveys. We also created visual representations of the free text responses in two separate word clouds (one for pre-course and one for post-course) with the size of any response word corresponding to the number of times it has been mentioned.
To examine the effect of this course on students’ perception of pain patients and pain management, we employed a scoring system to evaluate their utilization of professional terminology instead of layman’s terms. Each professional word they provided among the first five words that came to mind upon hearing the term “opioids” was assigned a value of “1 point”, while lay words received a value of “zero”. Similarly, we examined whether medical students’ use of lay words changed post-course by comparing the frequency of using a positive lay word before and after the course. Subsequently, we conducted a set of paired-sample t-tests to compare the frequency of professional and positive lay words used by each student in their free-text responses before and after the course.
Attitudes Likert Scale
Pre-course and post-course Likert scale responses were compared using the nonparametric Wilcoxon test with a significance level set at p<0.05. Some Likert scale items were negatively worded. These were reversed before analyses and reporting to facilitate interpretation with higher scores as more positive attitudes.
Virtual Format
A secondary goal was to evaluate the quality of the virtual course against the in-person course. To this extent, course evaluations from the online course taught in 2020 were compared against evaluations from the previous year’s (2019) in-person course using the Mann–Whitney U-test. The JH Office of Online Education, the curriculum deans, and the course directors wrote these course evaluations collaboratively. We examined the items that were identical in both years and most pertinent to evaluate student satisfaction with the course. Students were asked to use a 5-point Likert scale to rate the course from excellent to poor or specify their level of agreement (from strongly agree to strongly disagree) with statements about the course quality. As is standard for courses at JH, participation was required from a random sample of 25% of all course participants and optional for the remaining 75%.
Statistical analyses were conducted with Statistical Package for the Social Sciences (IBM SPSS Statistics for Mac, Version 25.0. Armonk, NY: IBM Corp.)
Results
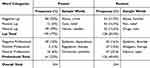
A total of 119 students enrolled and completed the described multi-disciplinary pain course with a passing grade. The demographics (age, gender, and planned specialty of pursuit, if known) of the student population are shown in Table 1. In total, 54 of the 119 students responded to both pretest and posttest surveys. Only these students were included in paired analyses.
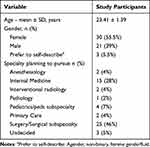 |
Table 1 Demographic Data (n = 54) |
Opioid Word Clouds & Word Categorization
The frequency of words falling into six possible categories (lay-positive, lay-negative, lay-neutral, professional-positive, professional-negative, professional-neutral) is displayed in Table 2. Visual representation of the change in words submitted by students is shown in Figure 1 from (A) pre- to (B) post-course free-text responses. There was a significant difference between the number of professional words used before (M=1.21, SD=0.97) and after the course (M=2.40 SD=1.33); t(52)=−6.39, p<0.001. Students also used more lay-positive words after the course (M=0.81, SD=0.63) than they used pre-course (M=0.23, SD=0.43); t(51)=−5.98, p<0.001.
Attitudes Likert Scale
There were significant changes in students’ responses to attitudinal questions following the course, as reflected in Table 3. Students reported feeling more comfortable providing opioids to chronic pain patients when appropriate (p < 0.001) and believed more strongly that treatment success in chronic pain medicine was not a “matter of luck” (p< 0.001). Students left the course significantly less likely to believe that chronic pain patients would be dissatisfied with a physician’s care (p = 0.001) and less likely to associate treating chronic pain patients with physician burnout (p = 0.027). Post-course, students were more inclined to find a career managing complex pain cases as exciting than they were pre-course (p < 0.001).
 |
Table 3 Mean, Standard Deviation, Median, and Wilcoxon Signed-Ranks Test Results for Pretest and Posttest Survey Responses (n = 54) |
Students’ beliefs that treating chronic pain patients could lead to physician frustration remained neutral (p = 0.139), as well as beliefs about whether chronic pain patients would comply with medical advice (p = 0.205). Similarly, students were neutral about their beliefs that patients with chronic pain would also likely use alcohol or illicit drugs (p = 0.124, 0.109, respectively).
Virtual Format
Our secondary goal was to determine if the virtual implementation of this course was non-inferior to the previous year’s in-person course. Table 4 shows the mean, standard deviation, median, and Mann–Whitney U-test results for student evaluation of the course in 2019 versus 2020. Students rated the overall quality of the course significantly higher in 2020 for the virtual course than the in-person course taught in 2019 (p = 0.002) and favored the virtual course for facilitating lifelong learning habits (p = 0.010) and enhancing their understanding of the material (p = 0.014). Students felt, however, that the in-person course’s clinical correlations better enhanced their understanding of course material than the virtual version (p = 0.002). All students received a passing score (70% or higher) on the knowledge exam and a passing grade in the course for both years.
 |
Table 4 Mean, Standard Deviation, Median, and Mann–Whitney U-Test Results for Student Evaluation of the Course in Years 2019 versus 2020 (for 2019, n = 39; for 2020, n = 34) |
Discussion
To mitigate the adverse effects of pain mismanagement on individuals and society, it is critical to ensure that pain education at the undergraduate medical education level is deliberately designed to be comprehensive, multi-disciplinary, and carefully integrated into the four-year curriculum.15 In this study, we demonstrate that a pain course meeting these criteria can significantly improve medical students’ attitudes towards pain management, chronic pain patients, and the complexities surrounding opioids.
Integrating pain curricula into undergraduate medical education can help ensure that future physicians are grounded in the basic principles of acute and chronic pain management, regardless of their future specialty training.9 The lens through which medical students view clinical encounters in clerkship years is foundational and can reinforce pre-existing beliefs. Early educational intervention prior to clerkships allows educators to bring awareness to unconscious biases towards pain patients and prevent treatment inequities.18 Educators can also overturn false beliefs about biological differences in pain processing11 and address misconceptions surrounding opioids before they impact care.
The significant post-course increase in the use of professional language compared to lay language around opioids suggests that the curriculum deepened the students’ global and conceptual understandings of the role of opioids in medicine and society. Words categorized as lay reflected the expected understanding of the average, non-clinically trained American (ie, “pain killers”, “dangerous”) as well as press/media themes surrounding pain and opioids (ie, “scary”, “rappers”, and “crime”). Words categorized as professional were thematic to the clinical use of opioids (ie, “not first line”, “taper”, “multimodal”, “acute”), opioid side effects (ie, “constipation”, “withdrawal”, “dependence”), and opioid complexities (ie, “uninformed”, “misuse”). The notable shift from lay language pre-course to professional language post-course signified our students’ enhanced medical and scientific grasp of opioid-related issues. In cases where lay words were still chosen, they were significantly more positive (ie, “relief”) than negative (ie, “fear”) in connotation, reflecting a less stigmatizing view of opioids and opioid users post-intervention.
In line with this vocabulary shift, students acknowledged that they would feel more comfortable providing opioids to chronic pain patients when appropriate. Opioids are still an important part of pain treatment and functional recovery for cancer pain, some acute pain states, and some chronic pain patients.19 Clinicians of all specialties will need baseline professional comfort with opioids, chronic pain, and addiction in the context of limited access to pain specialists3 and the endorsement of buprenorphine prescribing in many care settings, as reflected by the removal of the buprenorphine x-waiver in the US.
Post-course, students also indicated that they were less convinced that chronic pain patients would be dissatisfied with a physician’s care and less convinced that the successful treatment of chronic pain patients was a “matter of luck”. They were more likely to find a career that involved managing complex pain cases exciting and were less likely to associate treating chronic pain patients with physician burnout. These changes in student perception are important; negative attitudes towards pain management can discourage students from pursuing careers in pain-related specialties. In addition, preconceived notions about the futility of chronic pain treatment may manifest as disinterest in learning about pain, contempt towards pain patients, or unwillingness to prescribe treatments that can work. Given the prevalence of painful conditions, such attitudes are incompatible with current practice environments across specialties and can ultimately compromise the quality of care.
Students who took the virtual course rated it significantly higher in terms of overall quality and usefulness for developing life-long learning habits compared to those who took the in-person course. This finding parallels the increasing reliance on virtual learning tools in medical education post-pandemic. However, students preferred in-person clinical correlations to virtual ones. In-person correlations featured pain patients who participated in faculty-moderated small-group discussions with students, while virtual clinical correlations featured pre-recorded patient vignettes that were watched and explored in faculty-moderated, digital small groups. As videos lack the dimensionality to replace real-life patient engagement, our course has transitioned into a blended learning model, combining online asynchronous sessions with supplemental in-person synchronous sessions for clinical correlations.
We acknowledge that this is an observational, single-institution study and that not all medical schools will readily dedicate 21 hours to pre-clerkship pain education. Given the finite number of didactic hours available in medical school training, implementation of pain content means fewer hours for another subject. Schools will require a strong pain faculty presence that can advocate for the public health importance of prioritizing pain education. We also recognize that some schools may not have faculty with the expertise or protected non-clinical time to deliver a comprehensive pain curriculum. To address this, we are packaging the online version of our course for distribution to other medical schools which will include virtual-reality-based clinical correlations to supplement asynchronous content, as opposed to the videos and digital breakout rooms used in this study. Virtual reality (VR) learning is superior to screen-based learning, and it expands opportunities for teaching practical skills, such as managing difficult conversations involving opioids or de-escalating situations. VR also enhances the capacity to assess clinical knowledge and competence where appropriate.20
In addition, this study assesses the immediate effects of our curriculum on students’ attitudes and perceptions, instead of longitudinal effects. We cannot yet comment on the long-term impact of this course on attitudes, clinical decision-making, and patient outcomes. Future studies could include follow-up assessments to evaluate the sustained value of the curriculum over time. We are re-administering this survey to this same cohort of students at the end of year-four of medical school. Additionally, research may explore correlations between the completion of this course and prescribing behaviors, the specialty of choice, the number of pain cases seen in practice, or other variables. It is notable that the study was conducted during the COVID-19 pandemic, which necessitated a shift to a fully virtual format. While the study found that the virtual format was generally non-inferior to the in-person format in most areas, it is unclear if this would hold true in a post-pandemic setting.
Conclusion
Undergraduate medical education must predictably improve graduates’ understanding of safe and effective pain treatment modalities, as well as their appreciation of disparities in pain medicine and the impact of stigma on pain care. The finding that a single, 21-hour course had a substantial impact on first-year medical students’ perceptions and attitudes towards pain management underscores the need for high-quality pain education interventions and demonstrates the feasibility of producing a marked shift in perception with a limited amount of didactics.
Funding
No Funding Was Received for This Study.
Disclosure
Shravani Durbhakula has formerly reported consulting payments from Averitas Pharma and Biotronik outside the scope of the submitted work. Michael E. Schatman currently reports ad/comm from Syneos Health and is a research consultant for Modoscript outside the scope of the submitted work. The authors report no other conflicts of interest in this work.
References
1. Seal K, Becker W, Tighe J, Li Y, Rife T. Managing chronic pain in primary care: it really does take a village. J Gen Intern Med. 2017;32(8):931–934. doi:10.1007/s11606-017-4047-5
2. Tkacz J, Pesa J, Vo L, et al. Opioid analgesic-treated chronic pain patients at risk for problematic use. Am J Manag Care. 2013;19(11):871–880.
3. Number of people by active physician specialty 2021: association of American Medical Colleges; Available from: https://www.aamc.org/data-reports/workforce/data/number-people-active-physician-specialty-2021.
4. Dubois MY, Follett KA. Pain medicine: the case for an independent medical specialty and training programs. Acad Med. 2014;89(6):863–868. doi:10.1097/ACM.0000000000000265
5. NRMP. Results and Data Specialties Matching Service® 2023 Appointment Year; 2023.
6. Curriculum topics in required and elective courses in medical school programs: association of American Medical Colleges; Available from: https://www.aamc.org/data-reports/curriculum-reports/data/curriculum-topics-required-and-elective-courses-medical-school-programs.
7. Mezei L, Murinson BB. Pain education in North American medical schools. J Pain. 2011;12(12):1199–1208. doi:10.1016/j.jpain.2011.06.006
8. Shipton EE, Bate F, Garrick R, Steketee C, Visser EJ. Pain medicine content, teaching and assessment in medical school curricula in Australia and New Zealand. BMC Med Educ. 2018;18(1):110. doi:10.1186/s12909-018-1204-4
9. Briggs EV, Battelli D, Gordon D, et al. Current pain education within undergraduate medical studies across Europe: advancing the Provision of Pain Education and Learning (APPEAL) study. BMJ Open. 2015;5(8):e006984. doi:10.1136/bmjopen-2014-006984
10. Lee P, Le Saux M, Siegel R, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: meta-analysis and systematic review. Am J Emerg Med. 2019;37(9):1770–1777. doi:10.1016/j.ajem.2019.06.014
11. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. doi:10.1073/pnas.1516047113
12. De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. 2016;157(8):1607–1610. doi:10.1097/j.pain.0000000000000512
13. Durbhakula S, Fortin A. Turning down the flame on medical gaslighting. J Gen Intern Med. 2023;38(15):3426–3427. doi:10.1007/s11606-023-08302-4
14. Committee on the Science of Changing Behavioral Health Social Norms; Board on Behavioral C, and Sensory Sciences; Division of Behavioral and Social Sciences and Education; National Academies of Sciences, Engineering, and Medicine. Ending discrimination against people with mental and substance use disorders: the evidence for stigma change. Washington (DC): National Academies Press (US); 2016. 4, Approaches to Reducing Stigma. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384914/.
15. Murinson BB, Nenortas E, Mayer RS, et al. A new program in pain medicine for medical students: integrating core curriculum knowledge with emotional and reflective development. Pain Med. 2011;12(2):186–195. doi:10.1111/j.1526-4637.2010.01050.x
16. Toy S, Daly Guris RJ. How to conduct survey-based research. Anaesthesia. 2023;78(7):902–905. doi:10.1111/anae.15943
17. Artino AR, La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research. AMEE Guide No 87 Med Teach. 2014;36(6):463–474.
18. Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain. 2015;16(6):558–568. doi:10.1016/j.jpain.2015.03.003
19. Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95. doi:10.15585/mmwr.rr7103a1
20. Shahrvini B, Baxter SL, Coffey CS, MacDonald BV, Lander L. Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: a survey study. BMC Med Educ. 2021;21(1):13. doi:10.1186/s12909-020-02445-2
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.