Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 9
Sexually transmitted diseases among female commercial sex workers in Finote Selam town, northwest Ethiopia: a community-based cross-sectional study
Authors Anteneh ZA, Agumas YA, Tarekegn M
Received 10 November 2016
Accepted for publication 3 February 2017
Published 2 March 2017 Volume 2017:9 Pages 43—49
DOI https://doi.org/10.2147/HIV.S127319
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Zelalem Alamrew Anteneh,1 Yirdaw Amare Agumas,2 Molalign Tarekegn3
1School of Public Health, Bahir Dar University, 2Networks of Charitable Societies of HIV Positive Association in Amhara Region (NAP+), 3Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia
Background: Female commercial sex workers (FCSWs) are considered a high-risk group for acquiring sexually transmitted diseases (STDs), yet the reported prevalence varies in studies around the world. The aim of this study was to determine the magnitude and associated factors of STDs among female sex workers.
Methods: A community-based cross-sectional study was conducted among female sex workers in Finote Selam town. A total of 389 sex workers were studied using census method. Data were collected using an interview with structured questionnaires. The data were entered and analyzed by using SPSS version 20 software package.
Results: The findings of this study showed that the overall prevalence of STDs was 20.6%. The reported prevalence of genital discharge, ulcer, and bubo was 15.9%, 15.2%, and 11.6%, respectively. In the multivariable logistic regression analysis, respondents who did not use a condom were about four times at higher risk of STDs than those who were using a condom consistently (adjusted odds ratio [AOR] = 4.07; 95% confidence interval [CI]: 1.812, 9.139). Respondents who experienced condom breakages were more than 12 times more likely to report STDs than those who never experienced condom breakages (AOR = 12.291, 95% CI: 5.701, 26.495).
Conclusion: The findings of this study showed that one in five commercial sex workers in Finote Selam town had STDs. Sex without a condom and condom breakage during sexual intercourse showed a significant association with STDs. Therefore, the Woreda Health Office in collaboration with nongovernmental organizations in the area should work on safe sex promotion to enhance consistent condom use and reduce condom breakage through continuous education among commercial sex workers.
Keywords: sexually transmitted infections, commercial sex workers, vaginal discharge
Introduction
Sexually transmitted diseases (STDs) refer to those conditions caused by pathogens that can be acquired and transmitted through unprotected sexual intercourse. They can be caused by bacteria, viruses, protozoa, fungi, and ectoparasites.1,2
STDs are known for causing a variety of clinical syndromes, including abnormal genital discharge, genital ulcer/sore, inguinal bubo, and lower abdominal pain in females.3,4
STDs are global public health problems which cause acute illness, infertility, long-term disability, and death, with severe medical and psychological consequences in millions of males, females, and infants.5 Worldwide, approximately one million people acquire a new curable STD every day, and more than 340 million new cases occur each year. Adolescents and young adults have the highest rates of curable STDs; one in 20 adolescents acquires a new STD each year.6 STDs are among the world’s most common diseases with an annual incidence next to diarrheal diseases, malaria, and respiratory diseases.7,8
Different scholars who are working in the area believe that the magnitude of STDs is considerably increasing from day to day. The worldwide incidence of major bacterial and viral STDs is estimated at over 125 million cases yearly.1,7,8
The majority of these new infections occur among young adults aged up to 25 years, whilst approximately one-third occur among individuals younger than 20 years of age.9 Females in the age range of 14 to 19 years are almost twice as susceptible to STDs than boys of the same age.8
Eighty-six percent of the world’s burden of STDs occurs in the developing countries, the greatest burden being in the poorest countries, many of which are in sub-Saharan Africa, where identification and management of STDs are limited, and the STDs disproportionately affect females. The morbidity from STDs (excluding HIV) in females aged 15–49 years ranks second next to maternal causes.3,7
Untreated bacterial STDs in females result in pelvic inflammatory disease in up to 40% of infections, and one in every three of these will result in infertility.10 Tubal damage from STDs can lead to ectopic (tubal) pregnancy, which can result in up to 10% of maternal mortality in settings where prevalence of STDs is high.6 Chronic pelvic pain from untreated bacterial STDs is an important reason for health care visits among females. STDs are also among the leading causes of disability-adjusted life years lost for females of reproductive age in the developing countries.4,8
According to Ethiopian Demographic and Health Survey 2005, the prevalence of STDs was 2% among sexually active males and females.11 Female commercial sex workers (FCSWs) have been viewed both by laypersons and epidemiologists as one of the high-risk groups for infections and transmission of STDs.12,13 In the geographical area of our study, the Finote Selam town, the vulnerability of FCSWs to STDs is very high due to a high sexual networking from the nearby Birrshelko military camp, Birr agricultural development industry, and the reason that it is a common resting place for long-truck drivers.
Therefore, the aim of this study was to determine the magnitude of STDs and the factors that could contribute to them among commercial sex workers in the town.
Methods
A community-based cross-sectional study was conducted among female sex workers in Finote Selam town from March 20 to May 5 in 2015. The town is located 389 km away from Addis Ababa (capital city of Ethiopia) in the northwest of the country. The total population size of the town according to 2012 census report was 42,062 (21,286 males and 20,776 females).
Study population
According to the recent mapping documents of HIV/AIDS Prevention & Controls Office (HAPCO) and Females, Children & Youth Affairs Office report, there were 400 female sex workers in the town. The study included all the available sex workers using census method.
Variables
The occurrence of STD was a dependent variable. Some of the predictor variables were age, educational status, unsafe sex, alcohol use, drug use, forced sex, etc.
Measurements
The occurrence of sexually transmitted infections was identified if an FCSW had experienced symptoms of vaginal discharge or genital ulcer or inguinal bubo or more than one of these symptoms in the last 12 months of the survey.
Condom use, condom slippage, condom breakage, alcohol use, and drug use were all measured in the last 12 months prior to the survey.
An FCSW was identified as any woman who used sex as a source of income.
Data collection instrument and procedure
The data were collected through face-to-face interview using a structured questionnaire. There were 33 questions organized in to sociodemographic and sexual behavior sections. The questionnaire contained both close-ended (yes/no and multiple-choice) and open-ended items. The tool was designed in English and translated into the local language Amharic, and back-translated to English by language experts to ensure original meaning was maintained. The Amharic version was used for collecting the data. Census method was used to include the whole sex workers registered on mapping document by HAPCO and Females, Children & Youth Affairs Office in the town. The study participants were traced between 8:00 AM and 12:30 PM from house to house where they were living.
A census is the procedure of systematically acquiring and recording information about the members of a given population. It is a type of survey that includes all the existing eligible study population.
Six commercial sex workers were recruited as data collector. The criteria for inclusion of data collectors were the following: female sex worker, educational level of 10th grade and above, and a sex worker who ever participated in data collection activities in similar other studies. Female sex workers who fulfilled these criteria were enlisted. Three nurses who had experience of supervision in similar data collections were selected as supervisors. Training was provided for 1 day on the overall data collection procedures.
The objective of the study was clearly discussed to ensure the data collectors were very familiar with the aim of the study and data collection process. The completed questionnaire was checked daily by the supervisors and the principal investigators for completeness. Any obstacles or issues that did arise with data collection were discussed over night with data collectors and the supervisors and resolved. A pretest or pilot survey was conducted with 40 female sex workers in Bahir Dar city before the conduct of the main survey.
Data processing and analysis
Prior to data entry, questionnaires were checked for errors, coded, and entered into Statistical Package for the Social Sciences (SPSS) version 20 software package. Data were cleaned by doing simple frequency and cross tabulation analyses between each independent and dependent variables.
Descriptive statistics, such as frequencies and percentages, and multivariable logistic regression analysis were computed.
Variables that showed an association with STD in bivariate analysis at a P-value of less than 0.20 were identified and were included in multivariable analysis, and the model was built with backward elimination.
Ethical approval
Ethical clearance was obtained from the research and the ethical review committee of GAMBY College of Medical Sciences. Permission letters were obtained from Amhara Regional Health Bureau and Finote Selam town health office. Verbal consent was obtained from each participant, and the participants were told that they had the right not to respond to questions that they did not wish to answer and could voluntarily withdraw from the survey at any time.
Results
Sociodemographic characteristics of commercial sex workers in Finote Selam town
Data of 389 out of the total 400 registered commercial sex workers in the town were included in the analysis, resulting in a response rate of 97.25%.
The mean age of participants was 27.46±7.71 years. The majority, 53.2%, were home-based sex workers, and about 7.5% were phone-based workers. The average number of years reported working in the industry was 3.71±3.35 years. In terms of education, 166 (42.7%) participants had completed from grade 1 to 8. About 47.6% of the sex workers included in the study had been farmers before they commenced sex work (Table 1).
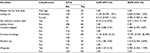
  | Table 1 Sociodemographic characteristics of female commercial sex workers in Finote Selam town, northwest Ethiopia, May 2015 Abbreviation: SD, standard deviation. |
Sexual behavior of commercial sex workers in Finote Selam town
The findings of this study showed that all of the respondents have had sex before they commenced sex work. The mean and standard deviation of the age at first sexual initiation was 15.78±3.215 years. It was found that 46% of the respondents initiated sex through marriage. However, 7.7% of the total respondents reported violence as part of their first experiences of sex.
More than one-half (55.8%) of the respondents had been married before they entered sex work, of which 25.4% were divorced and 9.3% were widowed. About 18%, 10%, and 6.4% of the sample reported one, two, and more than two children, respectively.
Regarding the number of sexual partners, 64 (16.5%) participants reported two or more sexual clients per day. Only 3.3% of sex workers ever had anal sex with their partners. However, no single participant had reported oral sex. With regard to condom use, 11.1% of participants had sex without a condom for all sex with paying clients during their sexual life; the major reason mentioned was higher payment (48.8%) for unprotected sex. The report indicated that 120 (30.8%) participants had nonpaying clients; out of them, 53.3% had reported no condom use at all whenever they had sex with their nonpaying clients. This study further indicated that 36% and 54% of the respondents ever had experienced condom slippage or breakage, respectively. Regarding substance use, 46.8% of participants had used alcohol, and 17% of the respondents reported using other drugs prior to sex (Table 2).
  | Table 2 Sexual behaviors of commercial sex workers in Finote Selam town, northwest Ethiopia, May 2015 |
In this study, 20.6% of participants had experienced one or more of the three symptoms characteristic of STDs in the last 12 months of the study period: 62 (15.9%), 59 (15.2%), and 45 (11.6%) of the total respondents had experienced vaginal discharge, vaginal ulcer, and inguinal bubo syndromes, respectively (Figure 1).
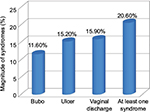  | Figure 1 The prevalence of sexually transmitted diseases among commercial sex workers in Finote Selam town, northwest Ethiopia, May 2015. |
Regarding the health-seeking behavior of the sex workers, out of the total respondents who experienced the STD syndrome, 6.2% visited the traditional healers and holy water-seeking treatment to their concern.
Factors associated with STDs among commercial sex workers in Finote Selam town
In the bivariate logistic regression analysis between different predictor variables and STDs, condom use, mode of sexual initiation, sex without condom for paying clients, condom slippage, condom breakage, sex after alcohol intake, and sex after drug intake in the last 12 months were found to show association at a P-value of 0.20. However, only sex without a condom for all paying clients and condom breakage were found to have an association with STDs at a significance level of 0.05.
The finding showed those commercial sex workers who had sex without a condom for paying clients were more than four times more likely to report STDs as compared to individuals who used a condom (adjusted odds ratio [AOR] = 4.07, 95% confidence interval [CI]: 1.8, 9.1). Also, the odds of STDs among sex workers who ever had condom breakage in the last 12 months of the study were more than 12 times as compared to the sex workers who did not experience condom breakage during sexual intercourse (AOR = 12.291, 95% CI: 5.7, 26.4) (Table 3).
Discussion
The objective of this study was to determine the magnitude and associated factors of STDs among commercial sex workers in Finote Selam town. Out of the total study participants included, data of only 11 (2.75%) respondents were excluded from analysis due to gross incompleteness. The probable reason for this high response rate might be that our data collectors were members of commercial sex workers who had some data collection experience. This, in turn, reduces the social desirability and nonresponse bias. The findings of our study showed that the overall prevalence of STDs was 20.6%. This is consistent with a study conducted in Malawi among sex workers, where the prevalence of STDs was 20%.14 However, our finding was much lower than that from Addis Ababa which reported an STD prevalence rate of 47.9%.15 The probable reason for this discrepancy might be difference in the duration of the study and the interventions used for the target group.
The findings of the current study are much higher than the findings of the surveillance survey conducted among sex workers in Ethiopia, where the prevalence of reported vaginal ulcer and discharge was only 5%.4 The probable reason for the difference might be the difference in sample size and that the national data were recorded only for vaginal ulcer and discharge.
The findings of this study showed remarkably high proportion of consistent condom use during sexual intercourse with paying clients. This is in accordance with a study conducted among sex workers of licensed non-brothel establishments of Bahir Dar city, where the prevalence of consistent condom use was 88.1%.16 However, our finding is much higher than that of a study conducted in Addis Ababa, where the proportion of consistent condom use among sex workers was 40%.17 The probable reason for the difference might be the difference in sample size, as the current study was conducted only in a single town whereas the other studies were done at national level on a large population.
The current study also indicated that the magnitude of consistent condom use was high among female sex workers compared to the People’s Republic of China, where the magnitude was less than 50%.18
In this study, the prevalence of condom breakage during sexual intercourse in the last 12 months was 46%, which is very much higher than the finding from a study conducted in Bahir Dar city, where the prevalence of condom breakage was reported to be 4.4%,16 and our finding is also higher than the findings of a survey conducted in both the developed and developing countries, where the magnitude breakage varied between 1% and 13%.19 Moreover, the finding from this study was much higher than a study conducted in Nevada among sex workers, where the prevalence of condom breakage was less than 1%.20
In the current study, the prevalence of condom slippage was found to be 36%. It contrasts with a study conducted in Bahir Dar city, where the prevalence was 1.5%.16 This shows that the magnitude of condom slippage was more than 24 times greater in this study than the study conducted in Bahir Dar city. Additionally, the finding of our study is much higher than a similar study conducted in sub-Saharan Africa, where the prevalence of condom slippage ranged from 1% to 5% during vaginal intercourse.19
The prevalence of condom slippage in our study was much higher than other studies. The probable reason for the high prevalence of condom breakage and slippage in the current study might be lack of intervention regarding proper condom use; this demands training on proper condom use to minimize condom slippage and breakage to the lowest possible.
In the present study, the prevalence of drug use before and during sex was 17%. This is higher than the findings of another study, where the magnitude of drug use during sex was 10.7%.4 In the current study, it was found that inconsistent condom use and condom breakage were significantly associated with the occurrence of STDs. Commercial sex workers who had sex without condom with paying clients were more likely to report STDs compared to those who used condom. This finding is supported by a study conducted in Malawi among FCSWs, where unsafe sexual intercourse was significantly associated with STDs.14
Respondents who ever experienced condom breakage during sexual intercourse were more likely to report STDs as compared to those with no condom breakage. Evidences showed that sexual activity with no condom among persons who exchange sex increases the risk of getting or transmitting HIV and other STDs because the infection is transmitted from one person to the other with no barrier.21,22
Limitation of the study
This study has a limitation as it did not test for STDs but used self-reported data on syndromes of STDs to determine both the prevalence of STDs and the factors that affect them.
Conclusion
The current study showed that one in five commercial sex workers in Finote Selam town reported STDs. The study also revealed that inconsistent condom use and condom breakages were significant predictors of STDs among sex workers in the town.
Therefore, the Woreda Health Office in collaboration with the nongovernmental organizations should work better at increasing awareness and skills that promote consistent condom use, and the correct use of condoms in order to prevent condom breakage and slippage during sexual intercourse.
Acknowledgments
The authors are indebted to all the participants of this study. They would like to thank their data collectors and supervisors for their valuable time spent on collecting data; besides, they would like to acknowledge Bahir Dar University College of Medical Sciences which provided ethical approval for the study.
Author contributions
ZAA was involved in writing the research proposal, data analysis and interpretation, and manuscript writing. YAA conceptualized the research problem, and was involved in writing the proposal, data analysis, report writing, and manuscript preparation. MT was involved in writing research proposal, report writing, and manuscript preparation. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines. MMWR Recomm Rep. 2015;64(RR-033):1–137. | ||
Minichiello V, Rahman S, Hussain R. Epidemiology of sexually transmitted infections in global indigenous populations: data availability and gaps. Int J STD AIDS. 2013;24(10):759–768. | ||
Bryan C. Sexually transmitted diseases. Available from: http://www.microbiologybook.org/Infectious%20Disease/Sexually%20Transmitted%20Diseases.htm. Accessed October 18, 2016. | ||
Alem A, Kebede D, Mitike G, Enqusellase F, Lemma W. Unprotected sex, sexually transmitted infections and problem drinking among female sex workers in Ethiopia. Ethiop J Health Dev. 2006;20(2):93–98. | ||
World Health Organization. HIV/AIDS and other sexually transmitted infections. Available from: http://www.who.int/ith/diseases/hivaids/en/. Accessed December 30, 2016. | ||
Public Health at Glance. Sexually transmitted infections in developing countries. Available from: http://web.worldbank.org/archive/website01213/WEB/0__CO-54.HTM. Accessed December 30, 2016. | ||
Bereket Y, Terefe G, Mulat T. Prevalence and associated factors of sexually transmitted infections among students of Wolaita Sodo University, Southern Ethiopia. Int J Sci Technol Res. 2013;2(2):86–94. | ||
Centers for Disease Control and Prevention (CDC). STDs in adolescents and young adults [updated December 16, 2014]. Available from: https://www.cdc.gov/std/stats13/adol.htm. Accessed September 12, 2016. | ||
Joint United Nations Programme on HIV/AIDS (UNAIDS). Beginning of the end of the AIDS epidemic. July 2014 [updated September 2014]. Available from: www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf. Accessed December 28, 2016. | ||
Refaat B, Dalton E, Ledger WL. Ectopic pregnancy secondary to in vitro fertilization-embryo transfer: pathogenic mechanisms and management strategies. Reprod Biol Endocrinol. 2015;13(1):30. | ||
Central Statistical Agency [Ethiopia] and ORC Macro. Ethiopia Demographic and Health Survey 2005. Addis Ababa: Central Statistical Agency [Ethiopia] and ORC Macro; 2006. | ||
Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7):538–549. | ||
Scorgie F, Chersich MF, Ntaganira I, Gerbase A, Lule F, Lo YR. Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS Behav. 2012;16(4):920–933. | ||
Zachariah R, Spielmann MP, Harries AD, Nkhoma W, Chantulo A, Arendt V. Sexually transmitted infections and sexual behaviour among commercial sex workers in a rural district of Malawi. Int J STD AIDS. 2003;14(3):185–188. | ||
Desta S, Feleke W, Yusuf M, et al. Prevalence of STD and STD related risk factor in sex workers of Addis Ababa. Ethiop J Health Dev. 1990;4(2):149–153. | ||
Alemayehu A. Magnitude of and Factors Associated with Male Condom Use and Failure Rate Among Commercial Sex Workers of Bahir Dar Town Licensed Non-brothel Establishments, Ethiopia [master’s thesis]. Addis Ababa: Addis Ababa University; 2004. | ||
Aklilu M, Messele T, Tsegaye A, et al. Factors associated with HIV-1 infection among sex workers of Addis Ababa, Ethiopia. AIDS. 2001;15(1):87–96. | ||
Wong WC, Yim YL, Lynn H. Sexually transmitted infections among female sex workers in Hong Kong: the role of migration status. J Travel Med. 2011;18(1):1–7. | ||
Shelton JD, Johnston B. Condom gap in Africa: evidence from donor agencies and key informants. BMJ. 2001;323(7305):139. | ||
Albert AE, Warner DL, Hatcher RA, Trussell J, Bennett C. Condom use among female commercial sex workers in Nevada’s legal brothels. Am J Public Health. 1995;85(11):1514–1520. | ||
Wilton J. CATIE: Canada’s sources for HIV and hepatitis C information. Condoms for the prevention of HIV and STI transmission. 2013. Available from: http://www.catie.ca/en/fact-sheets/prevention/condoms. Accessed May 10, 2016. | ||
Centers for Disease Control and Prevention (CDC). STDs and HIV – CDC fact sheet [updated November 17, 2015]. Available from: http://www.cdc.gov/std/hiv/stdfact-std-hiv-detailed.htm. Accessed October 18, 2016. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.