Back to Journals » Clinical Epidemiology » Volume 13
Sex Differences of Combined Effects Between Hypertension and General or Central Obesity on Ischemic Stroke in a Middle-Aged and Elderly Population
Authors Chen MQ, Shi WR, Wang HY, Sun YX
Received 6 December 2020
Accepted for publication 3 February 2021
Published 10 March 2021 Volume 2021:13 Pages 197—206
DOI https://doi.org/10.2147/CLEP.S295989
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eyal Cohen
Meng-Qi Chen,1 Wen-Rui Shi,1 Hao-Yu Wang,2 Ying-Xian Sun1
1Department of Cardiology, The First Hospital of China Medical University, Shenyang, 110001, People’s Republic of China; 2Department of Cardiology, Coronary Heart Disease Center, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, 100037, People’s Republic of China
Correspondence: Ying-Xian Sun
Department of Cardiology, The First Hospital of China Medical University, 155 Nanjing North Street, Heping District, Shenyang, 110001, People’s Republic of China
Email [email protected]
Background: Hypertension and obesity are recognized as modifiable risk factors for stroke, but their combined effects are unknown. This study aimed to explore the combined effects of hypertension and general or central obesity on the risk of ischemic stroke in a middle-aged and elderly population.
Methods: The data of 11,731 participants (53.5 ± 10.5 years old) were analyzed from the Northeast China Rural Cardiovascular Health Study, 2012– 2013. General obesity (GO) was defined by body mass index (BMI); central obesity (CO) was measured by waist circumference (WC), waist-to-height ratio (WHtR) and waist-to-hip ratio (WHpR).
Results: The overall prevalence of ischemic stroke was 3.1%. After adjusting for age and sex, the odds ratios for having ischemic stroke were 4.31 (3.14– 5.91) among subjects with hypertension, 1.79 (1.40– 2.30) with GO, 1.94 (1.54– 2.43), 1.98 (1.54– 2.53), and 1.65 (1.33– 2.06) with CO measured by WC, WHtR and WHpR, respectively. After full adjustment for potential confounders, the combinations of hypertension and obesity indices (including BMI, WC, WHtR and WHpR) were associated with the highest risk of ischemic stroke, especially in women, which were respectively 7.3-fold, 9.3-fold, 9.9-fold and 7.6-fold higher than that of individuals without both conditions.
Conclusion: Our study results suggest that women with both hypertension and obesity, no matter defined by BMI, WC, WHtR or WHpR, were more likely to have ischemic stroke. A better understanding of the combined effects of these risk factors can help promote primary prevention in susceptible subgroups.
Keywords: ischemic stroke, hypertension, general obesity, central obesity
Introduction
In recent years, stroke has become a challenging health burden worldwide, as the second leading cause of mortality and the number one cause of adult disability.1–3 Although incidence decreased in high-income countries over the past two decades, stroke has increased substantially in low-income and middle-income countries, especially in China.4–6 In China, 2.4 million new stroke cases and 1.1 million stroke-related deaths were added annually, estimated with data from the National Disease Surveillance Points System.7 Because of its high prevalence and mortality as well as the associated disability, better primary prevention of stroke has become a major priority for public health in China and globally.
Hypertension (HTN) is a well-recognized modifiable risk factor for stroke.8 According to the China National Stroke Registry, 72.7% of patients with ischemic stroke had HTN; patients with HTN had an increased risk of recurrent stroke than their counterparts.9,10 For every 10 mmHg reduction in systolic blood pressure (SBP), the risk of stroke recurrence was reduced by 33% (95% CI, 9–51%).11 It has been documented that population with a mean SBP >115 mmHg could explain 60% of the stroke risk.12 Along with HTN, obesity has also been recognized as a modifiable risk factor for stroke.13,14 According to the EUROASPIRE III core survey, 35.5% of first-ever ischemic stroke patients had a body mass index (BMI) ≥30 kg/m2, 62.4% exhibited elevated blood pressure.15 A longitudinal study has demonstrated that BMI ≥ 30.0 kg/m2 had a significantly increased risk of stroke in both men and women.16
Considering the potential relationship between hypertension, obesity and stroke, it is necessary to better understand the association between these conditions. Accordingly, our study aimed to investigate the correlation of ischemic stroke, the most common subtype of stroke, with hypertension and general or central obesity (measured by body mass index, waist circumference, waist-to-height ratio and waist-to-hip ratio), based on the Northeast China Rural Cardiovascular Health Study (NCRCHS) data. We also proposed to explore the relative risk of having ischemic stroke according to the presence of general or central obesity, hypertension, or both conditions.
Methods
Study Population
This study originated from the NCRCHS data, a representative sample of the Chinese population in the Northeast region. The cross-sectional epidemiological survey of NCRCHS was conducted from January 2012 to August 2013. Detailed design about NCRCHS has been fully described elsewhere.17 Subjects (age ≥35 years) had participated in face-to-face interviews and health examinations. Of the 11,956 individuals whose data were used in the 2012–2013 NCRCHS, participants with incomplete biochemical and clinical data were excluded from our study. Therefore, a total of 11,731 participants were enrolled in this work. Written informed consent was provided from all subjects. The Ethics Committee of China Medical University approved this study protocol.
Data Collection
The information about data collection was fully discussed by our previous studies.18,19 Briefly, cardiologists and nurses underwent rigorous training, passed a final exam, and acquired the qualification to conduct the investigation. The information of the investigation was collected through self-administered questionnaires regarding demographic data, anthropometric parameters, and health-related behaviours. The quality assurance process of data collection was administrated by the central steering committee with a subcommittee.
The questionnaires were designed to collect detailed information from all subjects. Smoking and drinking status were stratified into the current status and others based on subjects’ self-reports. BMI was determined as follows: BMI = weight (kg)/height2 (m2). The waist-to-height ratio (WHtR) and waist-to-hip ratio (WHpR) were calculated as follows: WHtR = waist circumference (cm)/height (cm); WHpR = waist circumference (cm)/hip circumference (cm).
After resting for at least 5 minutes in a moderately relaxed and sitting state, blood pressure measurements were taken for each subject 3 times and measured by two randomly selected staff. The average value of 3 readings was used as the result of blood pressure.
After participants were fasting more than 12 hours, blood samples were collected in the morning. For long-term storage, the serum was subsequently separated by calibrated centrifuge and frozen at −20 Celsius degree. The fasting blood samples were analyzed to collect blood biochemical information, including fasting plasma glucose (FPG), serum creatinine (Scr), triglyceride (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C).
Definition
General obesity (GO) was defined as BMI ≥28 kg/m2, regardless of sex.20 Central obesity (CO) was determined as a waist circumference (WC) ≥90 cm or a WHtR ≥0.5 or a WHpR ≥0.9 for men and WC ≥80 cm or a WHtR ≥0.5 or a WHpR ≥0.85 for women.21–23 Hypertension was defined by mean SBP ≥140 mmHg, or mean diastolic blood pressure (DBP) ≥90 mmHg, or self-reported physician-diagnosed hypertension, or current antihypertensive treatment.24 Ischemic stroke was diagnosed by a history of cerebrovascular events, which was determined by either cranial computed tomography or magnetic resonance imaging within the past two years.
Statistical Analysis
For categorical variables, the results were presented as frequencies (percentages). Also, the following continuous variables were displayed as mean values ± standard deviation (SD) or median (interquartile). Pearson’s partial correlation coefficient was performed to reflect the relationship between blood pressures and four obesity indices, and to characterize how blood pressures correlated with these indexes adjusted for age, sex, current smoking, current drinking, FPG, TG, HDL-C, estimated glomerular filtration rate (eGFR). Multivariate logistic regression analysis was conducted to estimate the independent effect of ischemic stroke with general obesity, central obesity in three definitions, and hypertension, which presented with adjusted odds ratios (ORs) and 95% confidence interval (95% CI). Subgroup analyses were performed after classifying the participants according to age, sex, and the presence of hypertension with or without general obesity or central obesity in three different definitions. All statistical analyses were performed using SPSS 25.0 software (IBM corp).
Results
Characteristics of the Study Population
Of the 11,731 participants who enrolled in our study, a total of 367 were classified as having ischemic stroke. Table 1 shows the characteristics of the study population. Among the total subjects with ischemic stroke, less than half were men and the mean age was 63.3 ± 8.6 years. Participants with ischemic stroke had higher age, BMI, FPG, TC, TG, LDL-C, WC, SBP, and DBP, with lower HDL-C, and eGFR, compared with those without ischemic stroke. The proportion of subjects with current smoking and current drinking was lower in the ischemic stroke group. Hypertension, general obesity, and central obesity measured by WC, WHtR and WHpR presented a higher prevalence among participants with ischemic stroke. However, when we analyzed males and females separately, there was no difference in TC between normal and male participants with stroke.
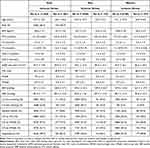 |
Table 1 Characteristics of Study Population Divided by Ischemic Stroke and Sex |
Figure 1 displays the prevalence of ischemic stroke according to the presence of hypertension and GO measured by BMI or CO measured by WC, WHtR and WHpR. The total prevalence of ischemic stroke was highest in subjects with both conditions among the four groups. However, males with hypertension but without general obesity had a higher prevalence than those with both hypertension and GO. The prevalence of ischemic stroke with both hypertension and CO measured by WC, WHtR or WHpR was respectively 5.1% for men vs. 6.8% for women, 5.7% for men vs. 6.4% for women and 5.3% for men vs. 7.3% for women.
Relationship Between Blood Pressures and Obesity Indices
The partial correlation coefficients for blood pressures and obesity indices are presented in Table 2. Age, sex, current smoking, current drinking, FPG, TG, HDL-C and eGFR were adjusted for the analyses. Among two blood pressures and four obesity indices, the greatest correlation was observed between SBP and BMI with a coefficient of 0.26. For obesity indices, the correlation coefficient between WC and WHtR was largest at 0.94.
 |
Table 2 Relationship Between Blood Pressures and Obesity Indices Adjusted by Age, Sex, Current Smoking, Current Drinking, FPG, TG, HDL-C and eGFR |
Risk Factors for Ischemic Stroke
Table 3 displays the results of logistic regression analyses, employed to corroborate the independent risk factors for ischemic stroke. All hypertension, GO, and CO measured by WC, WHtR and WHpR were significant risk factors for ischemic stroke in the total population. After adjustment for age and sex, the ORs for having ischemic stroke were 4.31 (3.14–5.91) among subjects with hypertension, 1.79 (1.40–2.30) among participants with GO, 1.94 (1.54–2.43), 1.98 (1.54–2.53), and 1.65 (1.33–2.06) among subjects with CO measured by WC, WHtR and WHpR, respectively. These correlations still existed after further adjustments for confounding factors, including current smoking, current drinking, FPG, TG, HDL-C, eGFR. Similarly, BMI-defined GO and WHpR-defined CO were correlated with an increased risk of ischemic stroke in both males and females, although no statistical significance in males. However, we observed gender-based differences regarding WHpR-defined CO. Central obesity measured by WHpR was independently correlated with ischemic stroke only in females with adjusted OR of 1.87 (95% CI: 1.34–2.62).
 |
Table 3 Multivariate-Adjusted Odds Ratios (ORs) of the Association of Ischemic Stroke with General Obesity, Central Obesity and Hypertension |
Subgroup Analysis According to Combination of Hypertension and General or Central Obesity
Table 4 exhibits the odds ratios (95% CI) for having ischemic stroke, according to different combinations of hypertension and general or central obesity in subgroups. Individuals without both conditions were recognized as the reference group. Sex, age, current smoking, current drinking, FPG, TG, HDL-C and eGFR were adjusted for our analyses. In the total population, individuals with both hypertension and GO had nearly five times higher risk of ischemic stroke than those without both conditions; subjects with both hypertension and CO measured by WC, WHtR or WHpR also had higher risks than those in the reference groups. The risk of ischemic stroke in participants with both hypertension and GO has increased up to more than five-fold among the middle age group (45≤ age <60 years). Notably, there was an increased risk of ischemic stroke among females who had both hypertension and BMI-defined GO or WHpR-defined CO than their counterparts. Meanwhile, the risk was substantially amplified among females with both hypertension and CO measured by WC or WHtR, which increased up to more than nine-fold risk, compared with females without both conditions.
 |
Table 4 The Odds Ratios for the Presence of Ischemic Stroke According to Combination of Hypertension and General or Central Obesity |
Figure 2 shows the ORs of ischemic stroke according to the presence of hypertension and general obesity or central obesity by sex. For men and women, the odds ratios of ischemic stroke in individuals with both conditions were largest among the four groups in the combination of hypertension and GO. In the other three combinations of hypertension and CO measured by WC, WHtR or WHpR, the odds ratios with both conditions were also the largest among the four groups. The results demonstrated the trend that the risks of ischemic stroke in subjects with both conditions were highest among the four different combinations in both men and women.
Discussion
The present study suggests that hypertension and obesity indices (including BMI, WC, WHtR and WHpR) were independently and positively correlated with an increased risk of ischemic stroke in a middle-aged and elderly population. Most importantly, these risk factors had prominent combined effects: the combinations of hypertension and obesity indices (including BMI, WC, WHtR and WHpR) were associated with the highest risk of ischemic stroke, particularly in women, which were respectively 7.3-fold, 9.3-fold, 9.9-fold and 7.6-fold higher than that of individuals without both conditions. Accordingly, the combined effects of hypertension and general obesity defined by BMI or central obesity measured by WC, WHtR and WHpR were synergistically associated with the risk of ischemic stroke, and the effects were more prominent in women than in men.
To our knowledge, this study is the first to investigate not only the independent impacts of obesity indices (including BMI, WC, WHtR and WHpR) and hypertension on the risk of ischemic stroke, but also the potential combined effects and interactions. Despite providing more information about public health, combined effects and interactions are often neglected. Previous studies have documented similar findings for BMI, WC, WHtR, WHpR or hypertension in association with ischemic stroke, without exploring their combined effects.8,14,25–27 Our findings indicated that the combination of obesity indices (including BMI, WC, WHtR and WHpR) and hypertension was positively correlated with the highest risk of ischemic stroke in total population, especially in women, whose risks were almost three times greater than in men.
Results of our study also show that hypertension, BMI-defined general obesity or WC, WHtR and WHpR-defined central obesity are independently associated with total and female ischemic stroke. Our findings indicate that general obesity and central obesity have similar effects on ischemic stroke risk. Besides, our results also show that hypertension has a greater impact on ischemic stroke risk than general or central obesity. Consistently, hypertension is also a strong risk factor for ischemic stroke among those without obesity. These findings suggest that better control of elevated blood pressure throughout life may have long-term health benefits, with or without obesity.
In the subgroup analyses, the relative risks of having ischemic stroke were estimated according to different combinations of hypertension and general or central obesity, compared with the reference group with neither condition. The presence of concurrent hypertension and GO or CO was correlated with a strikingly increased risk of ischemic stroke in the total population. Moreover, the relative risk of ischemic stroke was remarkably increased among females who had both hypertension and BMI-defined GO or WHpR-defined CO, which increased up to more than seven-fold risk, than their reference groups. Meanwhile, the relative risk was strikingly amplified among females with both hypertension and CO measured by WC or WHtR, which increased up to more than nine-fold risk, compared with those without both conditions. It is worthwhile to determine a potential indicator and biomarker to predict cardiovascular disease in susceptible subgroups, and ischemic stroke, the most common subtype of stroke, has been considered as the important cause of mortality in cardiovascular diseases.3,28 Accordingly, these results may indicate that individuals with hypertension and BMI-defined general obesity or WC, WHtR and WHpR-defined central obesity, particularly women, should focus on preventing ischemic stroke.
The combined effects of hypertension and BMI-defined general obesity or WC, WHtR and WHpR-defined central obesity were more prominent in women compared with men. There is some evidence indicating gender-based differences in the combined effects to ischemic stroke, although the potential mechanisms for this phenomenon still need to be clarified.29–31 Due to the much higher incidence in old age as well as the longer life expectancy, women experienced more stroke prevalence than men.29,32 Furthermore, recent data have shown a downward trend in stroke incidence over time, and this decline was due to a decrease in the incidence of ischemic stroke in men.31,33 Additionally, the body composition of men and women was different; for example, men tended to have more skeletal muscle than women while women may have more body fat than men.34 A recent study conducted in rural Northeast China suggested that compared with male participants with hypertension, female patients were more likely to take antihypertensive drugs, and therefore, antihypertensive treatment might play a role in the gender differences.35 According to a prospective case-control study, increased WC and WHtR were positively and significantly associated with ischemic stroke only in women.26 Although age and many confounding factors were fully adjusted for the regression analysis in this study, the gender-based differences we observed might also come from potential unmeasured confounders. Taken together, the gender-based differences in the combined effects on ischemic stroke are reasonable and acceptable Further study on gender physiology in the combined effects to ischemic stroke is required.
The limitations of this study mainly come from the cross-sectional design, which cannot establish a causal relationship between ischemic stroke and risk factors. To add, the generalizability of our results might be compromised because the study population only included rural residents from northeast China. Additionally, unmeasured or unknown confounding factors may affect the accuracy and validity of the results, such as diet, physical activity and medication information. Despite the limitations, the results of this study would be useful to public health, because we corroborated associations between ischemic stroke with both hypertension and general or central obesity according to gender in a large-scale Chinese population.
Conclusion
In conclusion, obesity indices (including BMI, WC, WHtR and WHpR) and hypertension were independently and positively correlated with an increased risk of ischemic stroke in a middle-aged and elderly population, regardless of gender. Most importantly, the combined effects of hypertension and BMI-defined general obesity or WC, WHtR and WHpR-defined central obesity were synergistically associated with the risk of ischemic stroke, and the effects were more prominent in women than in men. Accordingly, a better understanding of the combined effects of these modifiable risk factors can help promote primary prevention in susceptible subgroups.
Data Sharing Statement
The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
This study was conducted in compliance with the ethical principle of the Declaration of Helsinki. All participants provided written informed consent and all procedures were performed in accordance with the ethical standards. The study protocol was approved by the Ethics Committee of China Medical University (Shenyang, China).
Acknowledgments
This work was supported by the National Key Research and Development Program from the Ministry of Science and Technology of China (grant numbers 2017YFC1307600, 2018YFC1312400); Liaoning science and technology project (grant number 2017107001); and Science and Technology Program of Shenyang, China (grant number 17-230-9-06).
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Liu L, Wang D, Wong KS, Wang Y. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke. 2011;42(12):3651–3654. doi:10.1161/strokeaha.111.635755
2. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/s0140-6736(12)61728-0
3. Collaborators GCoD. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi:10.1016/s0140-6736(17)32152-9
4. Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Global Health. 2013;1(5):e259–e281. doi:10.1016/s2214-109x(13)70089-5
5. Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245–254. doi:10.1016/s0140-6736(13)61953-4
6. Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387(10015):251–272. doi:10.1016/s0140-6736(15)00551-6
7. Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–771. doi:10.1161/circulationaha.116.025250
8. Qureshi A. Acute hypertensive response in patients with stroke: pathophysiology and management. Circulation. 2008;118(2):176–187. doi:10.1161/circulationaha.107.723874
9. Wang Y, Xu J, Zhao X, et al. Association of hypertension with stroke recurrence depends on ischemic stroke subtype. Stroke. 2013;44(5):1232–1237. doi:10.1161/strokeaha.111.000302
10. Kannel W, Wolf P, McGee D, Dawber T, McNamara P, Castelli W. Systolic blood pressure, arterial rigidity, and risk of stroke. The Framingham study. JAMA. 1981;245(12):1225–1229. doi:10.1001/jama.245.12.1225
11. Arima H, Chalmers J. PROGRESS: prevention of recurrent stroke. J Clin Hypertens. 2011;13(9):693–702. doi:10.1111/j.1751-7176.2011.00530.x
12. Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens. 2006;24(3):423–430. doi:10.1097/01.hjh.0000209973.67746.f0
13. Kurth T, Gaziano J, Rexrode K, et al. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111(15):1992–1998. doi:10.1161/01.Cir.0000161822.83163.B6
14. Strazzullo P, D’Elia L, Cairella G, Garbagnati F, Cappuccio F, Scalfi L. Excess body weight and incidence of stroke: meta-analysis of prospective studies with 2 million participants. Stroke. 2010;41(5):e418–e426. doi:10.1161/strokeaha.109.576967
15. Heuschmann P, Kircher J, Nowe T, et al. Control of main risk factors after ischaemic stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur J Prev Cardiol. 2015;22(10):1354–1362. doi:10.1177/2047487314546825
16. Wang C, Liu Y, Yang Q, et al. Body mass index and risk of total and type-specific stroke in Chinese adults: results from a longitudinal study in China. Int J Stroke. 2013;8(4):245–250. doi:10.1111/j.1747-4949.2012.00830.x
17. Chen M-Q, Shi W-R, Shi C-N, Zhou Y-P, Sun Y-X. Impact of monocyte to high-density lipoprotein ratio on prevalent hyperuricemia: findings from a rural Chinese population. Lipids Health Dis. 2020;19(1):48. doi:10.1186/s12944-020-01226-6
18. Shi W, Wang H, Zhou Y, Sun Y, Chen Y. Synergistic interaction of hyperuricemia and hypertension on reduced eGFR: insights from a general Chinese population. Postgrad Med. 2020;1–7. doi:10.1080/00325481.2020.1718387
19. Wang HY, Shi WR, Yi X, Zhou YP, Wang ZQ, Sun YX. Assessing the performance of monocyte to high-density lipoprotein ratio for predicting ischemic stroke: insights from a population-based Chinese cohort. Lipids Health Dis. 2019;18(1):127. doi:10.1186/s12944-019-1076-6
20. Zhou BF. Cooperative Meta-Analysis Group of the Working Group on Obesity in C. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
21. Alberti KG, Zimmet P, Shaw JI. The metabolic syndrome–a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi:10.1016/s0140-6736(05)67402-8
22. Srinivasan SR, Wang R, Chen W, Wei CY, Xu J, Berenson GS. Utility of waist-to-height ratio in detecting central obesity and related adverse cardiovascular risk profile among normal weight younger adults (from the Bogalusa Heart Study). Am J Cardiol. 2009;104(5):721–724. doi:10.1016/j.amjcard.2009.04.037
23. Organization WH. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation. 2008.
24. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi:10.1001/jama.289.19.2560
25. Ab M, Jw C, Pf M, et al. Obesity increases risk of ischemic stroke in young adults. Stroke. 2015;46(6):1690–1692. doi:10.1161/strokeaha.115.008940
26. Rodríguez‐Campello A, Jiménez‐Conde J, Ois A, et al. Sex-related differences in abdominal obesity impact on ischemic stroke risk. Eur J Neurol. 2017;24(2):397–403. doi:10.1111/ene.13216
27. Sh S, Rl S, B-a B, et al. Abdominal obesity and risk of ischemic stroke: the Northern Manhattan Stroke Study. Stroke. 2003;34(7):1586–1592. doi:10.1161/01.Str.0000075294.98582.2f
28. Collaborators GMaCoD. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi:10.1016/s0140-6736(14)61682-2
29. Reeves MJ, Bushnell CD, Howard G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7(10):915–926. doi:10.1016/s1474-4422(08)70193-5
30. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi:10.1161/cir.0000000000000485
31. Madsen TE, Khoury J, Alwell K, et al. Sex-specific stroke incidence over time in the Greater Cincinnati/Northern Kentucky Stroke Study. Neurology. 2017;89(10):990–996. doi:10.1212/wnl.0000000000004325
32. Gall SL, Donnan G, Dewey HM, et al. Sex differences in presentation, severity, and management of stroke in a population-based study. Neurology. 2010;74(12):975–981. doi:10.1212/WNL.0b013e3181d5a48f
33. Koton S, Schneider AL, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312(3):259–268. doi:10.1001/jama.2014.7692
34. Janssen I, Heymsfield S, Wang Z, Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol. 2000;89(1):81–88. doi:10.1152/jappl.2000.89.1.81
35. Xing L, Liu S, Jing L, et al. Trends in prevalence, awareness, treatment, and control of hypertension in Rural Northeast China: 2008 to 2018. Biomed Res Int. 2020;2020:1456720. doi:10.1155/2020/1456720
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


