Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Sex Differences in the International Primary Care Airways Group Questionnaire for Screening of Chronic Obstructive Pulmonary Disease: A Retrospective, Cross-Sectional Study
Authors Machiguchi H , Arizono S , Tawara Y, Oomagari M, Yanagita Y , Tanaka T , Senjyu H , Kozu R
Received 25 February 2022
Accepted for publication 2 June 2022
Published 22 June 2022 Volume 2022:17 Pages 1467—1476
DOI https://doi.org/10.2147/COPD.S364088
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Min Zhang
Hikaru Machiguchi,1 Shinichi Arizono,2 Yuichi Tawara,2 Masaki Oomagari,1 Yorihide Yanagita,3 Takako Tanaka,4 Hideaki Senjyu,5 Ryo Kozu4
1Department of Rehabilitation, Seirei Mikatahara General Hospital, Hamamatsu, Japan; 2Department of Physical Therapy, School of Rehabilitation Sciences, Seirei Christopher University, Hamamatsu, Japan; 3Department of Physical Therapy, School of Health Sciences, Toyohashi SOZO University, Toyohashi, Japan; 4Department of Physical Therapy Science, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan; 5Respiratory Care and Rehabilitation Center, Fukujuji Hospital, Kiyose, Japan
Correspondence: Hikaru Machiguchi, Department of Rehabilitation, Seirei Mikatahara General Hospital, 3453 Mikatahara Kitaku, Hamamatsu, Shizuoka, 433-8558, Japan, Tel +81-53-436-1251, Fax +81-53-438-2971, Email [email protected]
Background and Objective: The International Primary Airways Group (IPAG) questionnaire is a useful tool for screening for chronic obstructive pulmonary disease. The cut-off score of the IPAG questionnaire is investigated in Japan. However, its validity has not been examined according to sex, which was the aim of this study.
Methods: We included 4364 participants aged 40 years or older, all current and ex-smokers and never-smokers, who completed the IPAG questionnaire and underwent spirometry. The IPAG questionnaire consists of eight items and the cut-off score is set to 17. We calculated the odds ratios of airflow limitation for each of the eight questions, by sex. We performed receiver operating characteristic analysis, calculating the area under the curve, sensitivity, and specificity for each sex.
Results: For both men (n=2784) and women (n=1580), only three questions were independent risk factors of airflow limitation. The odds ratios for age (≥ 70 years), wheezing, and smoking history (≥ 50 pack-years) were 10.61, 3.50, and 2.40, respectively, for men (all p< 0.001), and 4.30 (p< 0.001), 2.32 (p=0.026), and 5.69 (p=0.014), respectively, for women. For men and women, the areas under the curve were 0.741 and 0.670, respectively. The sensitivity and specificity values, respectively, were as follows: 83.6% and 47.1% for men with a cut-off score of 17; 80.0% and 53.7% for men with a cut-off score of 18; 56.7%, and 65.9% for women with a cut-off score of 17; and 76.7% and 43.9% for women with a cut-off score of 15.
Conclusion: Regardless of sex, only three IPAG questions were deemed useful as screening for airflow limitation. The cut-off scores for men and women may be appropriately set at 18 and 15, respectively, in the Japanese population.
Keywords: sex differences, respiratory airflow, screening, questionnaire, chronic obstructive pulmonary disease
Introduction
Chronic obstructive pulmonary disease (COPD) is now preventable and treatable, and early detection is crucial for its proper clinical treatment. Spirometry is the gold standard method for the early detection of COPD. However, it is difficult to screen the general population using spirometry, since it is not available in many settings. Its implementation rate in the primary care setting is also low.1 Consequently, questionnaires have been developed and used to screen patients for the early detection of COPD.2–5 One of these is the COPD diagnostic questionnaire of the International Primary Airways Group (IPAG), a simple and useful tool to screen patients in primary care and the general population for COPD.6–11 It has been externally validated for use in many countries6–10,12 and was deemed effective in Japan.11,13 Many of these studies included current or ever-smokers,7–10,12,13 and a few included never-smokers.6,11 Therefore, never-smokers should be screened as early as possible to detect COPD, similar to that being done for smokers.
In a recent systematic review, it was estimated that 6.16% of women have COPD, and that the rate of increase in COPD prevalence is higher in women than in men.14 COPD risk factors differ between men and women.15 Furthermore, women experience diagnostic delays compared with men in terms of COPD despite having a higher prevalence of anxiety and a history of exacerbations.16 Additionally, sex differences among patients with COPD were reported, including respiratory symptoms, comorbidities, acute exacerbations, and the effect of smoking.17–19 For example, de Torres et al20 reported that even among male and female patients matched for forced expiratory volume in 1 s (FEV1), female patients experienced a higher degree of dyspnea and had a poorer quality of life. In addition, many studies have shown anatomical differences between men and women.21,22 Therefore, the focus on the sex differences in COPD is important in its care efforts when considering differences in lung function and disease burden. However, the IPAG questionnaire does not currently consider sex differences in COPD.
We hypothesized that COPD-related sex differences would affect the overall score in the IPAG questionnaire, as well as the scores for individual questions. However, the cut-off score for the IPAG questionnaire is 17 regardless of sex.23 The purpose of the present study was to investigate the validity of the IPAG questionnaire as a screening method for airflow limitation depending on sex.
Materials and Methods
Study Design and Participants
A retrospective epidemiological survey was performed on 4427 participants aged 40 years or older, including both smokers and never-smokers. We defined smokers were current or ex-smokers in the same category. They were recruited from 17 hospitals in the Saitama, Ibaraki, Shiga, Kyoto, Osaka, Kagoshima, and Okinawa prefectures, Japan. They participated in full medical checkup,24 attended voluntary health examinations, undertook regularly scheduled check-ups, or undertook screening in outpatient clinics from July 2008 to July 2009. Full medical checkup is conducted to accomplish early detection and treatment of disease. Regularly scheduled check-ups were defined as compulsory annual health examinations undertaken by employees, as per the Industrial Safety and Health Law. Patients undertaking to screen in outpatient clinics were defined as those who had not been diagnosed with respiratory disease and were attending hospital outpatient clinics for the management of other chronic conditions. The study was approved by the Ethics Review Committee of Nagasaki University Graduate School of Biomedical Sciences (approval number: 13061341) and was conducted according to the principles of the Declaration of Helsinki. All participants provided written informed consent before participation.
Measures
The study participants completed the IPAG questionnaire and underwent spirometry. The IPAG questionnaire consists of eight items (21 response choices) related to age, smoking history, body mass index (BMI), coughing, sputum, and allergies. Each question was scored individually, and the total score ranged from 0 to 38. The management handbook for the IPAG questionnaire recommends that it be used for current smokers with a cut-off score of 17; ie, a score of 17 or more by a current smoker is indicative of COPD.23
Spirometry was conducted by trained staff using spirometers that satisfied the medical equipment standard of the Japanese Respiratory Society. FEV1 and forced vital capacity (FVC) were measured, and the FEV1/FVC ratio was calculated. Predicted FEV1 was calculated using the equation recommended by the Special Committee of Pulmonary Physiology (Japan Respiratory Society).25 Participants whose FEV1/FVC ratio was 70% or less were defined an airflow limitation. The severity of the disease was categorized from stage I to IV based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.26 Bronchodilator reversibility testing was not performed as the questionnaire is used for screening purposes only.
Statistical Analysis
The study participants were divided into male and female groups. Differences in continuous variables were compared using the t-test for normally distributed variables and the Mann–Whitney U-test for non-normally distributed variables. Categorical variables were compared using the Chi-squared test. A multiple logistic regression model was performed, which included the eight items from the IPAG questionnaire as independent variables and airflow limitation as to the dependent variable; odds ratios were calculated separately for each group. Sensitivity and specificity were calculated at 1-point intervals, from the minimum to the maximum score in the IPAG questionnaire.
The sensitivity and specificity of the total score for identifying participants with airflow limitation were calculated using the receiver operating characteristic (ROC) curve, and the areas under the curve (AUCs) were calculated. Participants with missing values in the IPAG questionnaire and those with unclear spirometry results were excluded. Data are expressed as median (interquartile range) values, mean ± standard deviation values, or numbers (percentages). All analyses were performed using a commercial statistical software package (IBM SPSS Statistics for Windows, version 24.0; IBM Corp., Armonk, NY, USA) and a p- value of 5% was considered a significant difference.
Results
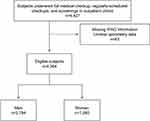
Figure 1 illustrates the flow of participants in this study. After excluding 63 participants with missing values in the IPAG questionnaire and those with unclear spirometry results, we analyzed the results of the remaining 4364. Their characteristics according to sex are summarised in Table 1. There were 2784 male (63.8%) and 1580 female (36.2%) participants. Overall, 285 had airflow limitations—a prevalence of 6.5%; the prevalence among men and women was 8.1% and 3.8%, respectively. Among the participants with airflow limitation, 82.8% had a COPD severity of stage I–II based on the GOLD criteria.
 |
Table 1 Characteristics of Study Participants |
The prevalence of airflow limitation and the corresponding odds ratio for each of the eight questions are presented in Table 2 for male and Table 3 for female participants. For both groups, only three questions were independent predictors of airflow limitation: age, smoking history, and wheezing. Among male participants, the odds ratios for age (≥70 years), wheezing, and smoking history (≥50 pack-years) were 10.61, 3.50, and 2.40, respectively. Among female participants, the odds ratios for age (≥70 years), wheezing, and smoking history (≥50 pack-years or more) were 4.30, 2.32, and 5.69, respectively.
 |
Table 2 Prevalence of Airflow Limitation and Odds Ratios for Male Participants |
 |
Table 3 Prevalence of Airflow Limitation and Odds Ratios for Female Participants |
The ROC curve for each sex is illustrated in Figure 2. The sensitivity and specificity of the male and female participants are shown in Table 4. Among men, the AUC was 0.741; the sensitivity and specificity were 83.6% and 47.1%, respectively, for a cut-off score of 17, and 80.0% and 53.7%, respectively, for a cut-off score of 18. Among women, the AUC was 0.670; the sensitivity and specificity were 56.7% and 65.9%, respectively, for a cut-off score of 17, and 76.7% and 43.9%, respectively, for a cut-off score of 15.
 |
Table 4 The Sensitivity and Specificity of Different Cut-off Scores for Identifying Participants with Airflow Limitation |
Discussion
In this study, we revealed that the validity of the questionnaire differed according to sex and that three of the eight questions could be used to independently identify participants with airflow limitation. The odds ratios for the three questions—relating to age, smoking history, and wheezing—also differed according to sex.
Previous studies comparing the validity of IPAG with COPD-PS showed that the AUCs of IPAG and COPD-PS were 0.775 and 0.747, respectively. The IPAG questionnaire was a useful screening tool for the Japanese.11 In addition, Kawayama et al13 reported that AUCs of IPAG questionnaire were 0.791, and the IPAG questionnaire was a useful tool for the Japanese population.
Sørheim et al27 reported that women in their study were more likely to develop COPD despite being younger than men, having a later onset of smoking, and having smoked less. Women may be more susceptible to the effects of cigarette smoking than men.28 This may be why the odds ratio for airflow limitation was the third-highest for the IPAG question related to smoking history for men; in contrast, the odds ratio was the highest for that question for women. Among male participants aged ≥70 years, the prevalence of airflow limitation was 24.5%, similar to that in the Nippon COPD Epidemiology study (24.4%).29 The odds ratio for airflow limitation in men was the highest for the IPAG question related to age (≥70 years). Therefore, in the IPAG questionnaire, the patient’s age may be the most useful question to identify airflow limitation in men.
In the present study, both sets of odds ratios differed from those reported by Price et al.3 We discovered that the weight of each question was different for men and women. Therefore, we believe that a scoring system that considers sex is required for COPD screening in the Japanese. For both men and women, the three questions on the questionnaire that could be used to effectively identify participants with airflow limitations were the same as those of men and women combined in previous studies in Japan.13,30 Old age, a history of profuse smoking, and the presence of wheezing are also important items in the COPD screening questionnaire developed by Samukawa et al.31
In the study in the US in which the scoring system for the IPAG questionnaire was developed, almost all questions were statistically significant predictors of COPD.3 This difference between Western and Japanese patients may be due to different clinical phenotypes of COPD, as such phenotypes differ even within the Japanese population.32 Questions relating to BMI, coughing, phlegm, and allergies were unable to identify participants with airflow limitation in this study. In the question relating to BMI, the values may be set too high for the Japanese population, for whom the normal value is 18.9–24.5 kg/m2. In this study, more than 60% of men and more than 70% of women had a BMI of less than 25.4, falling within the lowest of the three categories in the question. However, Ogura et al30 reported that BMI was an ineffective measure of COPD even when modified for Japanese patients.
In the present study, over 80% of the participants with airflow limitation were mild or moderate cases, according to the GOLD severity classification. We hypothesize that this is the reason why the questions in the IPAG questionnaire relating to coughing and phlegm were not diagnostically useful in this study.
The question related to allergies is useful in differentiating COPD from asthma. However, many patients have overlapping syndromes of COPD and asthma,33 and the purpose of the IPAG questionnaire is to screen for COPD, not differentiate between COPD and asthma. Therefore, we demonstrated that questions relating to age, smoking history, and wheezing are most important for the early detection of participants with airflow limitation in Japan.
With the cut-off of 17 points recommended in the IPAG diagnosis and management handbook,23 the sensitivity and specificity differed depending on sex in this study. We have revealed that cut-off scores of 18 and 15 may be appropriate for men and women, respectively. Various groups in Japan have examined cut-off values for the IPAG questionnaire. According to Kawayama et al13 and Tsukuya et al11 cut-off scores of 19.5 and 20, respectively, may be more appropriate for Japanese patients. In contrast, Arimura et al34 reported that the cut-off score should be lowered to 14, whereas Ogura et al30 in a study that targeted participants of full medical checkup, deemed a cut-off score of 17 appropriate. In the present study, among men, a cut-off score of 17 yielded a sensitivity and specificity of 83.6% and 47.1%, respectively, and a cut-off score of 18 yielded values of 80.0% and 53.7%, respectively. Price et al3 reported AUC, sensitivity, and specificity values, for a cut-off score of 16.5, of 0.816, 80.4%, and 57.5%, respectively. Although the AUC for men in this study was lower than that reported by Price et al (0.741 vs 0.816), the sensitivity and specificity for a cut-off score of 18 was similar to those reported by Price et al.3 Additionally, unlike in the study by Price et al3 the participants in the present study included never-smokers. In contrast, among women, a cut-off score of 16 yielded a sensitivity and specificity of 58.3% and 61.8%, respectively, and a cut-off score of 15 yielded values of 76.7% and 43.9%, respectively. The AUC was lower in women than in men and, for any given cut-off score, the sensitivity was higher in men and the specificity was higher in women. Furthermore, the AUC and sensitivity for women in this study were lower than those reported by Price et al.3 If the IPAG questionnaire is used for screening among the Japanese population using a cut-off of 17, there is a risk that women with airflow limitation may be overlooked. Therefore, we suggest that the cut-off score should be lowered to 15 for women, to detect those with airflow limitation.
In future studies, the combination that abbreviated the three questions version of IPAG and spirometry needs to investigate in international communities and longitudinal prospective studies following up them. If the three questions of IPAG are useful tool for screening for airflow limitation, we can screen more simply and in a short time.
This study has two main limitations. First, reversibility testing was not conducted. Therefore, participants with airflow limitation may have had lung diseases other than COPD. However, the questionnaire is a screening tool for early detection, not for diagnosis. Second, there were current or ex-smokers in the same category. Therefore, future studies might be separated them. Our study also has two main advantages. First, the sample size was large. Second, to our knowledge, this was the first study to identify sex differences in a COPD screening tool.
Conclusion
The validity of the IPAG questionnaire among Japanese participants differed according to sex in this study; it was deemed less effective for women than for men. Regardless of sex, only three of the eight questions, those relating to age, wheezing, and smoking history, were deemed useful in identifying airflow limitation. The risk of airflow limitation posed by these three questions differed according to sex. A cut-off score of 18 may be appropriate for men and a score of 15 for women, in the Japanese population. Our findings suggest that early airflow obstruction in primary care and the general population may be detected more successfully by changing the cut-off score depending on sex the three questions may be a simple screening tool for airflow limitation. The current IPAG questionnaire is recommended as a useful tool for screening airflow limitations in Japan.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request. Data sharing does not applicable to this article as no new data were created or analyzed in this study.
Acknowledgments
We thank the study participants, the staff of the incorporated medical institutions of the Tokushukai Group, and Professor Sumihisa Honda, Department of Public Health Nursing, Nagasaki University Graduate School of Biomedical Sciences, for statistical advice. This work was supported by Grant-in-Aid for Scientific Research (C) (No. 20K19392 to S Arizono) for Science Research from Japan Society for the Promotion of Science.
Funding
There was no funding obtained in the execution of this study.
Disclosure
Mr. S Arizono reports grants from Hoshi Iryou-Sanki Co. Ltd and NPO Central Japan Lung Study Group, outside the submitted work and grants from Science Research from Japan Society for the Promotion of Science, during the conduct of the study. The other authors have no known conflicts of interest to declare.
References
1. Naberan K, de la Roza C, Lamban M, Gobartt E, Martín A, Miravitlles M. Use of spirometry in the diagnosis and treatment of chronic obstructive pulmonary disease in primary care. Arch Bronconeumol. 2006;42:638–644. doi:10.1157/13095973
2. Price DB, Tinkelman DG, Halbert RJ, et al. Symptom-based questionnaire for identifying COPD in smokers. Respiration. 2006;73:285–295. doi:10.1159/000090142
3. Price DB, Tinkelman DG, Nordyke RJ, Isonaka S, Halbert RJ. Scoring system and clinical application of COPD diagnostic questionnaires. Chest. 2006;129:1531–1539. doi:10.1378/chest.129.6.1531
4. Kida K, Wakabayashi R, Mizuuchi T, Murata A. Screening for suspected chronic obstructive pulmonary disease with an eleven-item pre-interview questionnaire (11-Q). Intern Med. 2006;45:1201–1207. doi:10.2169/internalmedicine.45.1694
5. Martinez FJ, Raczek AE, Selfer FD, et al. Development and initial validation of a self-scored COPD Population Screener Questionnaire (COPD-PS). COPD. 2008;5:85–95. doi:10.1080/15412550801940721
6. Sichletidis L, Spyratos D, Papaioannou M, et al. A combination of the IPAG questionnaire and PiKo-6® flow meter is a valuable screening tool for COPD in the primary care setting. Prim Care Respir J. 2011;20:184–189. doi:10.4104/pcrj.2011.00038
7. Frith P, Crockett A, Beilby J, et al. Simplified COPD screening: validation of the PiKo-6® in primary care. Prim Care Respir J. 2011;20:190–198. doi:10.4104/pcrj.2011.00040
8. Stanley AJ, Hasan I, Crockett AJ, van Schayck OCP, Zwar NA. Validation of the COPD Diagnostic Questionnaire in an Australian general practice cohort: a cross-sectional study. Prim Care Respir J. 2014;23:92–97. doi:10.4104/pcrj.2014.00015
9. Stanley AJ, Hasan I, Crockett AJ, van Schayck OCP, Zwar NA. COPD Diagnostic Questionnaire (CDQ) for selecting at-risk patients for spirometry: a cross-sectional study in Australian general practice. NPJ Prim Care Respir Med. 2014;24:14024. doi:10.1038/npjpcrm.2014.24
10. Spyratos D, Haidich AB, Chloros D, Michalopoulou D, Sichletidis L. Comparison of three screening questionnaires for chronic obstructive pulmonary disease in the primary care. Respiration. 2017;93:83–89. doi:10.1159/000453586
11. Tsukuya G, Samukawa T, Matsumoto K, et al. Comparison of the COPD Population Screener and International Primary Care Airway Group questionnaires in a general Japanese population: the Hisayama study. Int J Chron Obstruct Pulmon Dis. 2016;11:1903–1909. doi:10.2147/COPD.S110429
12. Kotz D, Nelemans P, van Schayck CP, Wesseling GJ. External validation of a COPD diagnostic questionnaire. Eur Respir J. 2008;31:298–303. doi:10.1183/09031936.00074307
13. Kawayama T, Minakata Y, Matsunaga K, et al. Validation of symptom-based COPD questionnaires in Japanese subjects. Respirology. 2008;13:420–426. doi:10.1111/j.1440-1843.2008.01241.x
14. Ntritsos G, Franek J, Belbasis L, et al. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–1514. doi:10.2147/COPD.S146390
15. Aryal S, Diaz-Guzman E, Mannino DM. Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. Int J Chron Obstruct Pulmon Dis. 2014;9:1145–1154. doi:10.2147/COPD.S54476
16. Martinez CH, Raparla S, Plauschinat CA, et al. Gender differences in symptoms and care delivery for chronic obstructive pulmonary disease. J Womens Health. 2012;21:1267–1274. doi:10.1089/jwh.2012.3650
17. Agusti A, Calverley PMA, Celli B, et al., The Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122. doi:10.1186/1465-9921-11-122
18. Gonzalez AV, Suissa S, Ernst P. Gender difference in survival following hospitalisation for COPD. Thorax. 2011;66:38–42. doi:10.1136/thx.2010.141978
19. Celli B, Vestbo J, Jenkins CR, et al. Sex differences in mortality and clinical expressions of patients with chronic obstructive pulmonary disease. The TORCH experience. Am J Respir Crit Care Med. 2011;183:317–322. doi:10.1164/rccm.201004-0665OC
20. de Torres JP, Casanova C, Hernández C, Abreu J, Aguirre-Jaime A, Celli BB. Gender and COPD in patients attending a pulmonary clinic. Chest. 2005;128:2012–2016. doi:10.1378/chest.128.4.2012
21. McClaran SR, Harms CA, Pegelow DF, Dempsey JA. Smaller lungs in women affect exercise hyperpnea. J Appl Physiol. 1998;84(6):1872–1881. doi:10.1152/jappl.1998.84.6.1872
22. Harms CA. Does gender affect pulmonary function and exercise capacity? Respir Physiol Neurobiol. 2006;151(2–3):124–131. doi:10.1016/j.resp.2005.10.010
23. Grouse L, DeWeerdt S, eds. IPAG Diagnosis and Management Handbook. Chronic Airways Diseases: A Guide for Primary Care Physicians. Edgewater: MRC Vision, Inc.; 2005.
24. Takahashi E, Moriyama K, Yamakado M, Ningen Dock Database Group T; The Ningen Dock Database Group. Status of diabetes treatment in Japanese adults: an analysis of the 2009 Japan Society of Ningen Dock database. Intern. Med. 2014;53:1491–1496. doi:10.2169/internalmedicine.53.1876
25. Kubota M, Kobayashi H, Quanjer PH, Omori H, Tatsumi K, Kanazawa M; The Clinical Pulmonary Functions Committee of the Japanese Respiratory Society. Reference values for spirometry, including vital capacity, in Japanese adults calculated with the LMS method and compared with previous values. Respir Investig. 2014;52:242–250. doi:10.1016/j.resinv.2014.03.003
26. Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi:10.1164/rccm.200703-456SO
27. Sørheim IC, Johannessen A, Gulsvik A, Bakke PS, Silverman EK, DeMeo DL. Gender differences in COPD: are women more susceptible to smoking effects than men? Thorax. 2010;65:480–485. doi:10.1136/thx.2009.122002
28. Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J. 1997;10:822–827.
29. Fukuchi Y, Nishimura M, Ichinose M, et al. COPD in Japan: the Nippon COPD Epidemiology study. Respirology. 2004;9:458–465. doi:10.1111/j.1440-1843.2004.00637.x
30. Ogura T, Tejima T, Moritani Y, Matsuzaki Y, Uchimura K, Aoki M; COPD Research Group in Japan Anti-Tuberculosis Association (JATA). The usefulness of COPD questionnaire for screening COPD subjects. J Jpn Respir Soc. 2009;47:971–977.
31. Samukawa T, Matsumoto K, Tsukuya G, et al. Development of a self-scored persistent airflow obstruction screening questionnaire in a general Japanese population: the Hisayama study. Int J Chron Obstruct Pulmon Dis. 2017;12:1469–1481. doi:10.2147/COPD.S130453
32. Tatsumi K, Kasahara Y, Kurosu K, Tanabe N, Takiguchi Y, Kuriyama T; The Respiratory Failure Research Group in Japan. Clinical phenotypes of COPD: results of a Japanese epidemiological survey. Respirology. 2004;9:331–336. doi:10.1111/j.1440-1843.2004.00611.x
33. Miravitlles M, Calle M, Soler-Cataluña JJ. Clinical phenotypes of COPD: identification, definition and implications for guidelines. Arch Bronconeumol. 2012;48:86–98. doi:10.1016/j.arbres.2011.10.007
34. Arimura Y, Yamazaki S, Shirahama T, et al. The accuracy of COPD questionnaires in the general health check-up setting. J Jpn Respir Soc. 2008;46:693–699.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.