Back to Journals » International Journal of General Medicine » Volume 16
Severe, Persistent, Disruptive Fatigue Post-SARS-CoV-2 Disproportionately Affects Young Women
Authors Price JK , de Avila L, Stepanova M, Weinstein AA , Pham H, Keo W, Racila A, Gerber S, Lam BP , Gerber LH, Younossi ZM
Received 26 July 2023
Accepted for publication 14 September 2023
Published 27 September 2023 Volume 2023:16 Pages 4393—4404
DOI https://doi.org/10.2147/IJGM.S423910
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jillian Kallman Price,1 Leyla de Avila,1 Maria Stepanova,1– 3 Ali A Weinstein,4 Huong Pham,1 Wisna’odom Keo,1 Andrei Racila,1 Suzannah Gerber,1 Brian P Lam,1– 3 Lynn H Gerber,1,3,* Zobair M Younossi1– 3,*
1Betty and Guy Beatty Center for Integrated Research, Inova Health System, Falls Church, VA, USA; 2Center for Liver Disease, Department of Medicine, Inova Fairfax Medical Campus, Falls Church, VA, USA; 3Inova Medicine, Inova Health System, Falls Church, VA, USA; 4Department of Global and Community Health, George Mason University, Fairfax, VA, USA
*These authors contributed equally to this work
Correspondence: Jillian Kallman Price, Research Investigator, Outcomes Research, Beatty Liver and Obesity Research Program, Center for Integrated, Research, Department of Medicine, Inova Health System, Claude Moore Health Education and Research Building, Inova Fairfax Medical Campus, 3300, Gallows Road, Falls Church, VA, 22042, USA, Tel +1-703-776-3032, Fax +1-703- 776-4386, Email [email protected]
Introduction: Post-acute SARS-CoV-2 (PASC) symptoms are often persistent, disruptive, and difficult to treat effectively. Fatigue is often among the most frequently reported symptoms and may indicate a more challenging road to recovery.
Purpose: To describe the natural history, symptomology, and risk profile of long-term post-acute SARS-CoV-2.
Patients and Methods: Participants treated for SARS-CoV-2 within a large, community health system in the US were enrolled prospectively in a longitudinal, observational PASC study examining participants at enrollment and 6 months. Medical history, symptom reporting, validated measures of cognition, and patient-reported outcomes (PROs), were performed for all participants and repeated during study follow-up visits.
Results: A total of 323 participants completed baseline evaluations. Sixty one participants indicated clinically significant fatigue (23.1% at baseline); a representative sample of 141 enrollees also completed a baseline Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) in-depth fatigue reporting questionnaire, 37 had severe fatigue. The severely fatigued (FACIT-F ≤ 29.7) were significantly younger, female, had more anxiety and depression, had a higher resting heart rate, reported more sick days, and were less physically active post-COVID. They were more likely to have a diagnosis of chronic kidney disease (13.5% vs 2.9%) but less likely to have a history of cancer (8.1% vs 23.1). Participants who were severely fatigued reported health, diet, weight, and sleep were worse than those not severely fatigued post-COVID (p = 0.02 to 0.0002). Fatigue was significantly correlated with impairment of all PROs administered after COVID-19 infection.
Conclusion: Fatigue is a common symptom post-COVID-19 infection and is associated with lower reported well-being and function. Those with severe fatigue tended to be younger and female and have a past medical history of anxiety, depression, kidney disease, and more sedentary lifestyles.
Keywords: symptom severity, functional assessment of chronic illness therapy-fatigue, FACIT-F, SARS-CoV-2, COVID-19, recovery
Introduction
The long-term impact of SARS-CoV2 infection on function is currently an area of interest and investigation. The CDC reports that 1 in 13 adults in the US (7.5%) have “long COVID”, defined as novel symptoms lasting three or more months after first contracting the virus. However, this definition is not universally accepted, contributing to difficulties in developing treatment guidelines.1 Naming conventions for “long COVID” also vary and include post-acute SARS-CoV2 COVID (PASC), post-COVID syndrome, long COVID, and others.1,2 Further, the condition appears to lack an identified, cohesive biosignature.1,2 However, there does seem to be general agreement that this emergent condition is a significant medical concern, and one that substantively impacts daily life and function.2,3 For purposes of consistency, we will refer to post-COVID sequelae as PASC.
PASC is rarely a single organ-system problem and presents with many signs and symptoms, different risk factors, and thus different outcomes.4,5 Progress has been made to help identify some risks, but the variation presents challenges when seeking to and classify severity, and identify treatment target. Additionally, progression of the condition may include periods of remission and relapses before symptom resolution, and some may not return to full function.
There is disagreement in the literature about which populations are at greatest risk for PASC. Some previous studies have suggested that the risk of developing PASC was higher for persons of older age, female sex, with COVID-19 related hospitalization (including the need for oxygen therapy), with greater symptom load (especially dyspnea at presentation and chest pain), abnormal auscultation findings, and with comorbidities such as asthma.6–8 However, the Household Pulse Study reported by the CDC and another study indicated that older adults (≥70 years) were less likely to have PASC than younger adults (18–69 years) and that women were more likely than men to have CDC defined long COVID across all surveillance time points.9,10
Hospitalization has been an indicator of severity for SARS-CoV-2 but is not necessarily a risk factor for PASC. In one report, 45% of COVID-19 survivors, regardless of prior hospitalization, experienced a range (32–45 categories) of unresolved symptoms at ∼ 4 months.11,12 Some studies do identify prior hospitalization and history of severe COVID-19 infection as being a risk factor for PASC, and specifically a risk for increased dyspnea, anxiety, myalgia, and hair loss.8,13 By contrast, vaccination has been shown to potentially reduce the likelihood of developing PASC.14
Sociodemographic and behavioral factors seem to be important indicators of risk for PASC. Social determinants of health and health behaviors appear to correlate significantly with PASC, notably with its persistence, severity, and symptom clustering.15–17 Further investigation into these correlates may reveal mechanisms and mitigation strategies in the emergent chronic illness crisis presented by PASC. Several studies report no correlations, clearly different from SARS-CoV-2 infection, hospitalization, and death, in which ethnic differences and limited healthcare access were significant.18 Timing of the analysis (before versus after October 2021 availability of “Post COVID-19 condition, unspecified” in US healthcare coding) and increased sample size available for analysis as cases accumulate over time may both play roles in this disparate reporting.17,18 A recent study found that African-American/Black and Hispanic/Latino adults who were hospitalized for COVID-19 were more likely to develop PASC.17,19 In the months after infection, African-American/Black and Hispanic/Latino adults were also more likely to have diabetes and to report novel incidence of headaches, chest pain, and joint pain but were less likely to have sleep disorders, cognitive problems, or fatigue than White adults. Patient characteristics that indicate the risk of PASC, including persistence, severity and symptomology, remain to be well described, and greater evaluation is needed.
The prevalence of PASC and its various manifestations pose a significant challenge to patients and health care teams. Some evidence suggests that lifestyle health behaviors such as food and beverage choices, smoking, exercise, and sleep could help influence the progression of PASC. However, more evidence is needed to understand whether these factors are more influential in the development of PASC, and to what extent they can moderate recovery. Intervention strategies are needed to lessen the burden of PASC and may include diet, exercise/activity, and possible cognitive/behavioral treatments. In this longitudinal study, we report 6-months of observation for patients with a documented SARS-CoV-2 infection assessed for physical and cognitive function as well as PROs. This study documents both resolution and persistence of symptoms and attempts to characterize sub-populations at greatest risk for the impact of these symptoms on function, cognition, and quality of life.
Materials and Methods
Study Design
Participants, as well as the local SARS-CoV-2 population treated within our health system, were described in previous publications.12,19–23 This study conforms to all STROBE guidelines, was reviewed and approved ethically by the Inova Institutional Review Board (IRB# U20-09-4279) and Western Institutional Review Board (WIRB; IRB# 1294366) as human subjects research, complies with the Declaration of Helsinki, and informed consent was obtained from all participants. Written consent was obtained for in-person participants, and verbal consent was obtained for participants opting for virtual participation. Briefly, participants who were treated for SARS-CoV-2 between March 2020 and July 2022 within Inova Health System – a large, metropolitan, community health system in the northeastern U.S. – were invited to enroll in a post-acute SARS-CoV-2 (PASC) follow-up study examining post-COVID-19 recovery. Once enrolled, 323 participants’ data was collected at baseline and 6 months and continuing annual follow-ups with those experiencing persistent symptoms. Participants had their choice to participate either in-person or virtually, and in these sessions were asked about symptoms, including fatigue and other aspects of recovery relevant to PASC. Additional efforts made to remove language barriers to enrollment and promote inclusive enrollment were also described previously.19
Study Measures
We extracted information on the severity of acute SARS-CoV-2 infection and its treatment, as well as laboratory values, which were extracted from our electronic health record system (EPIC). In this prospective study, we collected data from participants in person and virtual interviews. These included sociodemographic status, past medical history (PMH), participation in (remote and current) regular exercise (30 minutes, 5x/week or a total of 150 minutes/week), measures of cognition (Color Word interference Test (CWIT), Coding, Arithmetic, Matrix Reasoning), a clinical assessment of health behavior change, and a variety of PROs (eg, Edmonton Symptom Assessment System (ESAS), EuroQol-5 dimension health-related quality of life instrument (EQ5D)) Full protocol and instrument description can be found in our prior publications.12,20
Fatigue Symptoms
A special emphasis was also placed upon assessing fatigue – one of the most commonly reported symptoms in assessed PASC patients using the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F). The FACIT-F includes 4 subscales of well-being: physical (PWB, range 0–28), emotional (EWB, 0–24), social (SWB, 0–28) and functional (FWB, 0–28); and a fatigue subscale domain (FS, 0–52), which adds up to a total FACIT-F score (0–160). For all domains, greater values are designed to reflect better health status.24 Using the general population norm and standard deviation (SD) for FS, we defined severe fatigue as FS lower than the norm by at least one SD which yields the cutoff of 29.7 (population norm 40.1, SD 10.4). Symptom categorization for free responses can also be found in Supplement 1 of our previous publications.12,19 FACIT-F score and Symptom Reporting were also analyzed using chi-square with odds ratio and confidence interval reporting.
Symptom Severity Reports
Participants were initially asked to name persistent symptoms that developed after the onset of SARS-CoV-2, along with the symptom severity (eg, mild, moderate, and severe). This self-report measure was repeated during subsequent visits in order to assess change and was recorded as better, worse, or resolved.
Statistical Analysis
Analyses used SAS 9.4 (SAS Institute, Cary, NC) and Jamovi 2.3.21. Prior to data analysis, the study database was reviewed for variable completeness and consistency with hard-copy case report forms.19 Any instance of missing data collection for variables was marked “unknown” and excluded from analysis.19 Additionally, cases longitudinally lost to follow-up were cross-sectionally analyzed for time points collected and excluded from time point comparisons.19 Between groups categorical comparisons used chi-square. Mann Whitney U and rank biserial correlation were used to compare severe to non-severe fatigue. Frequencies and relative reporting of symptoms by fatigue severity, along with chi-square odds ratios and confidence intervals were also included in the fatigue analyses.
Results
Symptom Burden
At baseline, 41.3% of 303 with complete symptom information reported being symptom-free. The frequency of persistent symptoms is reported to be in the order of prevalence at baseline and 6 months (reported in Table 1). Among the 58.2% reporting persistent symptoms, the nine top symptoms reported were fatigue (20.5%), memory difficulties (15.5%), shortness of breath (12.2%), general neurological symptoms (10.9%), loss of smell and/or taste (10.2%), musculoskeletal symptoms (8.6%), headache (8.3%), rash (7.6%), and mood disturbance (6.9%). At 6 months, 46.3% of 300 participating subjects report being symptom-free, fatigue (10.7%), memory difficulties (8.7%), shortness of breath (7.3%), general neurological symptoms (5.3%), musculoskeletal symptoms (5.0%), loss of smell and/or taste (4.7%), rash (4.0%), mood disturbance (3.7%), and headache (3.0%). A full list of reported symptoms can be found in Figure 1 (Figure 1).
 |
Table 1 Severe Fatigue (FACIT-F ≤27.9) and Symptom Reporting at Baseline and 6 Months |
By 6 months, only one symptom (nasal congestion) was resolved entirely, 17 symptoms were reported by <1% of those responding, and only 157 participants reported persistence for the top nine symptoms listed above. 81 participants completed the FACIT-F at 6 months, including 77 of the 157 instances of the top 9 symptoms. 18 of the 81 (22.2%) with completed FACIT-F scored within the severe fatigue range at baseline, and the number of cases of severe fatigue reported was cut in half as well (62 baseline vs 32 at 6 months) and just over half of the participants reporting severe fatigue completed the FACIT-F, a similar percentage of reporting to baseline.
The number of participants reporting individual symptoms decreased over the observation period – sometimes by nearly half. However, complete resolution of symptoms was uncommon, even among acute symptoms such as anosmia which reduced by half from 37 cases at baseline to 18 cases at 6 months). Approximately half of those evaluated at baseline completed detailed patient-reported outcomes data and the FACIT-F fatigue measures.
 |
Figure 1 Symptom Reporting Categorization. |
Severe Fatigue per FACIT-F Subset Analysis
Across timepoints, fatigue was the most commonly reported symptom. However, only half of those with baseline measurements provided detailed self-reports, including the FACIT-F fatigue measurements at the 6-month follow-up (Figure 2). 177 of 305 participants reported persistence of the top nine symptoms reported at baseline, and 37 of these 177 had FACIT-F scores (<27.9) indicating severe fatigue. In agreement with this finding, many participants reported persistence of clinically significant fatigue (37.8%), followed by shortness of breath (32.4%), memory difficulties (29.7%), and headache (24.3%) (Figure 3). Additional patient-reported outcome measure responses at baseline due to the presence or absence of severe fatigue reporting can be found in Table 2.
 |
Table 2 Severe/Non-Severe Fatigue at Baseline by Mann–Whitney U and Rank Biserial Correlation |
 |
Figure 2 Percentage of patients with severe fatigue among all those completing the Functional Assessment of Chronic Illness Therapy - Fatigue (FACIT-F). |
 |
Figure 3 Percentage of participants with severe fatigue at baseline by self-reported symptoms. |
Fatigue at Baseline After Enrollment
Those severely fatigued at baseline were more than 3 times as likely to report shortness of breath (32.4% vs 10.6%), almost 3 times more likely to report fatigue as a specific symptom (37.8% vs 14.4%), over 5 times more likely to report headache (24.3% vs 4.8%), nearly twice more likely to report memory difficulties (29.7% vs 15.4%), slightly more likely to report musculoskeletal symptoms (13.5 vs 9.6), slightly more general neurological symptoms (18.9% vs 14.4%), and over twice as likely to report neurological symptoms (16.2% vs.7.7%). There were similar reporting rates of rash (8.1% vs 7.7%). Those not severely fatigued were slightly more likely to report loss of taste or smell (16.3% vs 13.5%).
Fatigue After Six Months Follow-Up
Compared to those with less fatigue at baseline, those with severe fatigue reported greater persistence of the top nine symptoms at 6 months, reporting almost 3 times as much shortness of breath (27.8% vs 9.5%), twice as many general neurological symptoms (22.2% vs 11.1%), more fatigue (16.7% vs 9.5%), memory difficulties (16.7% vs 15.9%), mood disturbance (16.7% vs 4.8%), headaches (11.1% vs 4.8%), and rash (11.1 vs 6.3%) (Figure 4). However, these groups have the same levels of persistence for loss of smell and/or taste (11.1% vs 11.1%) and musculoskeletal problems (11.1% vs 11.1%) at 6 months. Additional information on FACIT-F severe fatigue versus not severe fatigue scores by fatigue symptom reporting at 6 months can be found in Table 3.
 |
Table 3 Frequencies of 6-Month Fatigue Severity Symptom Reporting Compared to FACIT-F Fatigue Severity Scores |
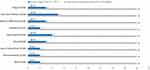 |
Figure 4 6-month symptoms frequency in the severely fatigued per Functional Assessment of Chronic Illness Therapy - Fatigue (FACIT-F). |
Association of Fatigue and Mood
The group reporting severe fatigue overlapped with those reporting worse well-being, depression, and stress, and this group also had greater persistence of the top nine PASC symptoms. Of those reporting severe fatigue, 27% had a past medical history of anxiety, and 32.4% depression. This group also reported less regular pre-infection physical activity, and less regular post-infection physical activity and represents almost 1/3 of the group.
Association of Fatigue and Health Behaviors
At baseline, patients reporting severe fatigue at baseline also reported having a significantly worse diet compared to before their acute SARS-CoV-2 infection (37.8% versus 13.6%, p < 0.002); worse weight status (44.4% versus 20.0%, p < 0.005), and worse sleep quality (63.9% versus 28.3%, p < 0.0013).
FACIT-F by Symptom Reporting
Those severe fatigue per FACIT-F at baseline were over 5 times more likely to report headache (24.3% vs 4.8%, p < 0.001, OR 6.36, CI 1.97–20.5), more than 3 times as likely to report shortness of breath (32.4% vs 10.6%, p < 0.003, OR 4.06, CI 1.60–10.03), and almost 3 times more likely to report fatigue as a specific symptom (37.8% vs 14.4%, p < 0.003, OR 3.61, CI 1.53–8.64). Memory difficulties (29.7% vs 15.4%, p < 0.057, OR 2.33, CI 0.962–5.63), mood disturbances (16.2% vs.7.7%, p < 0.136, OR 2.32, CI 0.748–7.21), musculoskeletal symptoms (13.5 vs 9.6, p < 0.509, OR 1.47, CI 0.467–4.62), general neurological symptoms (18.9% vs 14.4%, p < 0 0.517, OR 1.38, CI 0.515–3.72), rash (8.1% vs 7.7%, p < 0 0.935), and loss of taste or smell (16.3% vs 13.5%, p < 0.683) also had differences in reported, however were not statistically significant.
Among the symptoms, only shortness of breath remained statistically significant at 6 months of study follow-up by FACIT-F fatigue severity. The severely fatigued continued to report the major symptoms at higher percentages at 6 months, reporting almost 3 times as much shortness of breath (27.8% vs 9.5%, chi-square = 0.046), 3.5 times more mood disturbance (16.7% vs 4.8%, chi-square = 0.089), twice as many general neurological symptoms (22.2% vs 11.1%, chi-square = 0.225), more than twice the percentage of headaches (11.1% vs 4.8%, chi-square = 0.324), more fatigue as a symptom (16.7% vs 9.5%, chi-square = 0.395), almost twice as much rash (11.1 vs 6.3%, chi-square = 0.496), and slightly more memory difficulties (16.7% vs 15.9%, chi-square = 0.936). Both groups report the same percentage of loss of smell and/or taste (11.1% vs 11.1%, chi-square = 1.000) and musculoskeletal problems (11.1% vs 11.1%, chi-square = 1.000) at 6 months.
Discussion
Remarkable progress has been made in preventing and treating SARS-CoV-2, and acute infection remains a subject of ongoing research.25,26 The Centers for Disease Control of the United States (CDC) reports the prevalence of persistent symptoms following SARS-CoV-2 infection (PASC) as 7.5%. Global prevalence of PASC is estimated at approximately 65 million people, and growing, worldwide. This presents an important challenge to the health care community.9,17,24 The prevalence of PASC, its myriad of symptoms, its persistence, impact on function and life roles presents a significant health risk for domestic and global populations. Assessing which are modifiable should be a high priority. In our view, data collected from prospective, natural history studies using standard, reliable assessments, including PROs are critical to understanding this novel and emergent condition.
Using a prospective design, we confirm the work of others, in which existing data set analyses were performed, that fatigue is a common PASC symptom and is importantly, associated with less well-being and poor function. Fatigue can be associated with loss of work productivity and its associated indirect costs to the society.27 In this study, participants with clinically severe fatigue were younger, female, and have a past medical history of anxiety, depression, kidney disease, and are unlikely to exercise regularly. The finding that fatigue, and severe fatigue in 15% of this group, is the most common symptom is of significant concern, in part because it is difficult to measure and determine its cause(s). Further, the strong associations between fatigue and mood and shortness of breath (SOB) suggest fatigue is complex requires careful further assessments.
Our study did not measure breathing mechanics or include imaging of the lungs, so its etiology remains to be further explored. Currently, the American Lung Association identifies the following as the top causes of long-term SOB: poorly controlled asthma, chronic obstructive pulmonary disease (COPD), or pulmonary fibrosis.28 The National Health Service of the United Kingdom states that SOB is frequently a symptom of heart and lung problems in addition to asthma, allergies, and anxiety.29 Our data support the view that SOB may not solely be associated with pulmonary disease or cardio-respiratory dysfunction.19
Consistent with prior studies, we have identified that fatigue is prevalent among people reporting persistent symptoms, both in the months immediately following acute infection, and persistent through 6 months of diagnosed PASC.19 Symptom persistence and intensity are difficult to predict in PASC. Only shortness of breath predicted fatigue severity at 6 months. One of the specific aims of this study was to determine risk profiles for those recovering from PASC over 6 months and to identify which symptoms were most likely to persist among which sub-groups. Most patients had a reduction in symptom burden during the observation period, many symptoms lingered, and only one symptom, nasal congestion, fully resolved after 6 months.
PASC has a significant impact on quality of life and perceived well-being, and thus soliciting open-ended reports from patients may reveal highly relevant, especially bothersome, or the most subjectively disruptive symptoms impacting their daily routines. While these unstructured comments may not be complete or as reliable, they may indicate opportunities for intervention led by patient-led goals. However, the use of standardized measures whose psychometric properties have been validated may be more diagnostically informative and thus should not be omitted in lieu of symptom self-reporting alone.
Despite improvement in fatigue and other symptoms over the follow-up period, severe, disruptive fatigue seems to linger in a substantial number of patients with PASC. Our analysis suggests that the group likely to report severe, persistent fatigue are younger female patients who have a high symptom burden and especially report anxiety and depressive symptoms in addition to their fatigue. Additionally, the most impacted seem to be those with lower pre-COVID exercise behaviors, and those for whom the acute infection highly disrupted previously functional healthy diet and exercise habits. Impacts such as these may disproportionately impact the lives of those who report fatigue (ie, young women) because of their life stage and demands, including education, work, and family-related responsibilities.
Lingering fatigue is not unique to PASC. Post-viral fatigue has been reported in patients with Hepatitis C, Lyme Disease, and E-B virus among others and is often referred to as Chronic Fatigue/Myalgic Encephalomyelitis Syndrome (ME/CFS).30–33 Fatigue unrelated to exercise or post-exercise fatigue has also been seen in patients with non-alcoholic fatty liver disease (NAFLD).34,35 Future research may wish to look at similarities of fatigue among different patient groups to ascertain clues about the mechanisms and common pathways of fatigue. Fatigue is a highly prevalent symptom across a wide variety of viral and metabolic conditions, can be debilitating, has high frequency “co-traveler” conditions of significant concern (eg, anxiety and depression), and yet its underlying physiological pathways and mechanism involvement are still unclear. Looking at past medical history of anxiety and depression in more detail may also give us some understanding whether these diagnoses are overrepresented in our post-viral population with severe, persistent fatigue.
There is no consensus regarding the evaluation and treatment of fatigue. Our data support the finding of many other studies that fatigue is not an isolated symptom and may be associated with negative mood/affect, sedentary lifestyle, and metabolic dysregulation. This may compound the diminished social participation/social isolation that many reported during the pandemic, resulting in significant and extremified disparities in the work and social lives of persons with fatigue resulting from infection with COVID-19.30,36
These data may help inspire clinicians to include assessment of patient exercise and health behavior history in routine visits and especially in visits where patients seek treatment after viral infections. The association between regular exercise (30 minutes, 5x/week or a total of 150 minutes/week) and fewer symptoms and faster symptom resolution is striking. Targeting a manageable activity, such as pacing, may provide appropriate guidance for populations at risk and offer clinicians a recommendation for patients seeking medical attention for reasons other than SARS-CoV2 infection and its sequelae. As reported in our previous paper, this effect was also seen in mAb-treated patients.37 While our study did not include comprehensive assessments of diet and eating behavior, patient reports regarding the quality of their diet indicated that disruptions to diet may be associated with worse PASC symptom persistence.
The study had some significant challenges. The surge of the delta and then omicron variants significantly impacted the willingness of patients to come for in-person evaluations and led to a reduced sample for follow-up. We used Figure 1 self-reported symptoms, freely volunteered by participants without prompts, to capture the current symptom burden. This may not be a comprehensive assessment of all remaining symptoms. However, a significant strength of our study was the inclusion of patient-reported outcomes (PROs) at all visits -including fatigue via FACIT-F- which were both standardized and quantifiable.38 This study documents an association between patient reports of fatigue as a new symptom developed post-acute SARS-CoV-2 but does not establish causality. While our analysis identified that younger working age adults and specifically younger women were at higher risk for fatigue, our study also cannot speak to the magnitude and roles of fatigue, depression, and anxiety in the youngest of adults (age 18–20s), due to their low representation within our study cohort. This follows the Household Pulse Study reported by the CDC, where younger adults (18–69) and women were more likely to have CDC-defined long COVID across all surveillance time points.9,10
While documentation of persistent fatigue as a phenomenon in SARS-CoV-2 has been established, prospective and careful measurement of fatigue using validated measures versus just symptom reporting is lacking in the literature. There is a difference between identifying fatigue and understanding fatigue. An added strength of our prospective, multi-visit, in-depth cohort study with face-to-face discussion of symptomatology is that the features of interest within our cohort – possible confounding variables also assessed using validated measures – provide clarity in differentiating fatigue from frequent co-traveling conditions. Unique to the literature, we are also trying to determine phenomenon that go along with fatigue with patient-reported outcomes to understand what may be impactful in people’s lives, including behavioral milieu, depression, sleep, and quality of life. This is informed by our experience examining both viral and metabolic drivers of fatigue prior to the advent of SARS-CoV-2 and PASC.
Conclusion
Among patients with post-acute sequalae of SARS-CoV-2 (PASC) fatigue was the most common lingering symptom, followed by headache and shortness of breath. Severe fatigue was highly correlated with almost all patient-reported symptoms and notably the highest with comorbid depressive symptoms and anxiety. Young women were more likely to report severe, persistent, and disruptive fatigue and to also report low pre-COVID activity/exercise levels. Fatigue is prevalent in the PASC population and should be regarded as an important indicator of condition persistence and severity. Evaluation of mood and quality of life should be routinely performed, taken seriously, and treated medically when appropriate. Recommendation for regular exercise prior to infection, and to maintain a healthy diet during recovery, is likely to be associated with fewer and milder post-infection symptoms.
Acknowledgments
The research team would like to acknowledge the support of our organization Inova Health System, through the Betty & Guy Beatty Center for Integrated Research and the Department of Medicine, and for internal URAP support granted to the primary investigator for conduct of this study. The authors would also like to gratefully acknowledge our colleagues and their support for our research efforts: James Michael Estep, Pegah Golabi, Manisha Verma, Patrick Austin, Kathy Terra, Carey Escheik, Manirath Srishord, Mariam Afendy, Fatema Nader, Sean Felix, and Rebecca Cable.
Disclosure
In addition to the internal funding received for this study reported in acknowledgements, some authors have received funding for other research endeavors. Specifically, AAW cites institutional payments by the Health Resources and Services Administration (HRSA), and ZMY has consulted for Bristol Myers Squibb, Gilead, Intercept, Novo Nordisk, Novartis, Terns, Merck, Quest, and Siemens, and Madrigal. The authors declare that they have no other competing interests in this work.
References
1. Ledford H. How common is long COVID? Why studies give different answers. Nature. 2022;606(7916):852–853. doi:10.1038/d41586-022-01702-2
2. Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterization of post-COVID-19 manifestations. Int J Clin Pract. 2021;75(3):e13746. doi:10.1111/ijcp.13746
3. Carter SJ, Baranauskas MN, Raglin JS, Pescosolido BA, Perry BL. Functional status, mood state, and physical activity among women with post-acute COVID-19 syndrome. Int J Public Health. 2022;67:1604589. doi:10.3389/ijph.2022.1604589
4. Munipalli B, Seim L, Dawson NL, Knight D, Dabrh AMA. Post-acute sequelae of COVID-19 (PASC): a meta-narrative review of pathophysiology, prevalence, and management. SN Compr Clin Med. 2022;4(1):90. doi:10.1007/s42399-022-01167-4
5. Chippa V, Aleem A, Anjum F. Post-Acute Coronavirus (COVID-19) Syndrome. Treasure Island (FL): StatPearls Publishing; 2023.
6. Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. doi:10.1038/s41591-021-01292-y
7. Jacobs LG, Paleoudis EG, Lesky-di bari D, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020;15(12):e0243882. doi:10.1371/journal.pone.0243882
8. Subramanian A, Nirantharakumar K, Hughes S. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28(8):1706–1714. doi:10.1038/s41591-022-01909-w
9. National Center for Health Statistics. U.S. Census Bureau, Household Pulse Survey, 2022–2023. Long COVID. [Internet, generated interactively] Available from: https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm.
10. Qasmieh SA, Robertson MM, Teasdale CA, et al. The prevalence of SARS-CoV-2 infection and long COVID in U.S. adults during the BA.4/BA.5 surge, June-July 2022. Prev Med. 2023;169:107461. doi:10.1016/j.ypmed.2023.107461
11. O’Mahoney LL, Routen A, Gillies C, et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine. 2022;55:101762. doi:10.1016/j.eclinm.2022.101762
12. de Avila L, Price JK, Stepanova M, et al. Regular exercise is associated with low fatigue levels and good functional outcomes Post-COVID-19: a prospective observational study. Am J Phys Med Rehabil. 2023;102(5):433–443. doi:10.1097/PHM.0000000000002197
13. Malik P, Patel K, Pinto C, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis. J Med Virol. 2022;94(1):253–262. doi:10.1002/jmv.27309
14. Ayoubkhani D, Bosworth ML, King S, et al. Risk of long COVID in people infected with severe acute respiratory syndrome coronavirus 2 after 2 doses of a coronavirus disease 2019 vaccine: community-based, matched cohort study. Open Forum Infect Dis. 2022;9(9):ofac464. doi:10.1093/ofid/ofac464
15. NIH. NIH RECOVER research identifies potential long COVID disparities. Available from: https://www.nih.gov/news-events/news-releases/nih-recover-research-identifies-potential-long-covid-disparities.
16. Pfaff ER, Madlock-Brown C, Baratta JM, et al. N3C Consortium; RECOVER Consortium. Coding long COVID: characterizing a new disease through an ICD-10 lens. BMC Med. 2023;21(1):58. doi:10.1186/s12916-023-02737-6
17. Khullar D, Zhang Y, Zang C, et al. Racial/ethnic disparities in post-acute sequelae of SARS-CoV-2 infection in New York: an EHR-based cohort study from the RECOVER Program. J Gen Intern Med. 2023;38:1127–1136. doi:10.1007/s11606-022-07997-1
18. Yoo SM, Liu TC, Motwani Y, et al. Factors associated with post-acute sequelae of SARS-CoV-2 (PASC) after diagnosis of symptomatic COVID-19 in the inpatient and outpatient setting in a diverse cohort. J Gen Intern Med. 2022;37(8):1988–1995. doi:10.1007/s11606-022-07523-3
19. Price JK, Gerber LH, Stepanova M, et al. Post-acute SARS-CoV-2 symptoms are fewer, less intense over time in people treated with mono-clonal antibodies for acute infection. Int J Gen Med. 2023;16:1479–1490. doi:10.2147/IJGM.S406571
20. Mannan A, Sutingco N, Djurkovic S, et al. Service line care delivery model for COVID-19 patient-centric care. Am J Manag Care. 2022;28(3):e80–e87. doi:10.37765/ajmc.2022.88731
21. Verderese JP, Stepanova M, Lam BP. Neutralizing monoclonal antibody treatment reduces hospitalization for mild and moderate coronavirus disease 2019 (COVID-19): a real-world experience. Clin Infect Dis. 2022;74(6):1063–1069. doi:10.1093/cid/ciab579
22. Stepanova M, Lam BP, Younossi E, et al. The impact of variants and vaccination on the mortality and resource utilization of hospitalized patients with COVID-19. BMC Infect Dis. 2022;22(1):702. doi:10.1186/s12879-022-07657-z
23. Lam BP, Stepanova M, Venkatesan C, et al. Outcomes of hospitalized patients with COVID-19 during the course of the pandemic in a fully integrated health system. PLoS One. 2022;17(2):e0263417. doi:10.1371/journal.pone.0263417
24. Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133–146. doi:10.1038/s41579-022-00846-2
25. Priyanka CH, Choudhary OP. mRNA vaccines as an armor to combat the infectious diseases. Travel Med Infect Dis. 2023;52:102550. doi:10.1016/j.tmaid.2023.102550
26. Dhawan M, Parmar M, Angural S. Convalescent plasma therapy against the emerging SARS-CoV-2 variants: delineation of the potentialities and risks. Int J Surg. 2022;97:106204. doi:10.1016/j.ijsu.2021.106204
27. Maya S, Kahn JG, Lin TK, et al. Indirect COVID-19 health effects and potential mitigating interventions: cost-effectiveness framework. PLoS One. 2022;17(7):e0271523. doi:10.1371/journal.pone.0271523
28. Lung. Learn about shortness of breath. Available from: https://www.lung.org/lung-health-diseases/warning-signs-of-lung-disease/shortness-of-breath/learn-about-shortness-of-breath.
29. NHS Inform. Shortness of breath. Available from: https://www.nhsinform.scot/illnesses-and-conditions/lungs-and-airways/shortness-of-breath.
30. Rasa S, Nora-Krukle Z, Henning N, et al. European Network on ME/CFS (EUROMENE). Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med. 2018;16(1):268. doi:10.1186/s12967-018-1644-y
31. Price J, Escheik C, Azim Y, et al. Sustained virologic response (SVR) in hepatitis C (HCV) patients does not demonstrate differences in physical performance, fatigue, sleep, and health-related quality of life (HRQL). Am J Gastroenterol. 2013;108:S122. doi:10.14309/00000434-201310001-00410
32. Monaghan AM. An examination of physical activity, cardiorespiratory fitness and cardio-metabolic health through the modern hepatitis C continuum, Trinity College Dublin. School of Medicine. 2019.
33. Cortes Rivera M, Mastronardi C, Silva-Aldana CT, Arcos-Burgos M, Lidbury BA. Myalgic encephalomyelitis/chronic fatigue syndrome: a comprehensive review. Diagnostics. 2019;9(3):91. doi:10.3390/diagnostics9030091
34. Weinstein AA, Escheik C, Oe B, Price JK, Gerber LH, Younossi ZM. Perception of effort during activity in patients with chronic hepatitis C and nonalcoholic fatty liver disease. Pm&r. 2016;8(1):28–34. doi:10.1016/j.pmrj.2015.06.001
35. Austin P, Gerber L, Paik JM, Price JK, Escheik C, Younossi ZM. Aerobic capacity and exercise performance in nonalcoholic fatty liver disease. J Sports Med Phys Fitness. 2019;59(8):1376–1388. doi:10.23736/S0022-4707.19.09231-4
36. Gerber L, Estep M, Stepanova M, Escheik C, Weinstein A, Younossi ZM. Effects of viral eradication with ledipasvir and sofosbuvir, with or without ribavirin, on measures of fatigue in patients with chronic hepatitis C virus infection. Clin Gastroenterol Hepatol. 2016;14(1):156–164.e3. doi:10.1016/j.cgh.2015.07.035
37. Twomey R, DeMars J, Franklin K, Culos-Reed SN, Weatherald J, Wrightson JG. Chronic fatigue and post exertional malaise in people living with long COVID: an observational study. Phys Ther. 2022;102(4):zac005. doi:10.1093/ptj/pzac005
38. Webster K, Cella D, Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1(79):1–7. doi:10.1186/1477-7525-1-79
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
