Back to Journals » International Journal of General Medicine » Volume 16
Serum Magnesium Level as a Biomarker to Predict the Risk of Labor Epidural Anesthesia Associated Fever
Authors Chen Z , Zhu C, Huang L, Qi Y, Guo X, Xie L, Li H
Received 31 July 2023
Accepted for publication 27 October 2023
Published 6 November 2023 Volume 2023:16 Pages 5131—5138
DOI https://doi.org/10.2147/IJGM.S431731
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Luca Testarelli
Zhiwei Chen,1,* Chuling Zhu,2,* Lingna Huang,1,* Yuanjie Qi,1 Xiaoyao Guo,1 Li Xie,1 Hua Li1
1Department of Gynecologic, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, People’s Republic of China; 2Department of Women’s health Department, QuanZhou Women and Children’s Hospital, Quanzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hua Li, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, 18 Daoshan Road, Fuzhou, Fujian, 350001, People’s Republic of China, Tel +86-18005016206, Email [email protected] Li Xie, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, 18 Daoshan Road, Fuzhou, Fujian, 350001, People’s Republic of China, Tel +86-13635281861, Email [email protected]
Objective: Excessive pain will have adverse effects on the mother and fetus. Labor epidural analgesia greatly reduces the pain, which is widely carried out abroad. Labor epidural anesthesia-associated fever (LEAF) is the biggest problem for labor epidural anesthesia. This study aimed to evaluate the clinical value of serum magnesium levels to predict the LEAF.
Methods: Overall 528 singleton term-pregnant women who underwent labor epidural anesthesia in Fujian Provincial Maternity and Children’s Health Hospital, affiliated hospital of Fujian Medical University from January 2019 to June 2019, were analyzed retrospectively. The serum magnesium level was detected using venous blood samples. The relationship between the serum magnesium level and LEAF was interpreted, and the optimal cut-off values of the serum magnesium level to predict LEAF were calculated.
Results: Overall, 65 (12.30%) participants had LEAF. And a higher rate of the bulging membrane, gestational hypertension, neonatal intensive care unit (NICU) admission, and the different mode of delivery was significantly associated with LEAF. Also, the serum magnesium level demonstrated higher significantly in presence of LEAF than absence (P< 0.05). What is more, it indicated that the area under the receiver operating characteristic curve (AUC) for the serum magnesium level was 0.825, and an optimal cut-off of the serum magnesium level was 0.855 mg/dl. Furthermore, it demonstrated that the serum magnesium level had the highest OR (OR= 7.49; 95% CI (4.58– 14.35)) (P< 0.001). The bulging membrane is an independent risk factor presence of LEAF (OR = 1.55; 95% CI (1.01– 2.43)) (P=0.038).
Conclusion: This study demonstrated that the baseline of serum magnesium can provide a suitable biomarker to predict LEAF. It can help to provide a useful target for LEAF treatment and enhance surveillance before fever.
Keywords: serum magnesium level, labor epidural anesthesia associated fever, inflammation, risk, therapy
Introduction
Childbirth pain is a process of intertwining physical and psychological. Excessive pain will have adverse effects on the mother and fetus. With the advancement of society and the development of anesthesia technology, labor epidural analgesia has been recognized and accepted by more pregnant women.1 In the United States, it is reported that labor epidural analgesia was used by more than 70% of women undergoing childbirth.2 A 25% in The United Kingdom of Great Britain and Northern Ireland (UK) and 68% in Spanish delivery with epidural analgesia as an available intervention to relieve pain in labor.1
However, relevant research shows that the rate of labor analgesia is less than 10% in China, closely related to the increase in the cesarean section rate.3 Therefore, it is essential to promote labor analgesia vigorously in China, which is beneficial for pregnant women and babies.
At present, the clinically used labor epidural analgesia method is mainly intraspinal block, labor epidural associated, which has the advantages of good analgesic effect and little impact on mother and baby.4 Although labor epidural anesthesia is worthy of vigorous clinical promotion in China, it still faces many practical applications. One of the most significant issues is that the rate of labor epidural-associated fever (LEAF) is significantly higher than that without labor epidural anesthesia. Studies have shown that 26% of delivery women receiving labor epidural anesthesia have LEAF.5 Subsequently, many observational studies and prospective studies have also confirmed this clinical phenomenon.6 Intrapartum fever may have potential adverse effects on mothers and babies. Parturients who suffer from epidural analgesia-related intrapartum fever are more likely to receive vaginal device-assisted labor and cesarean section.7 Intrapartum fever also increases the possibility of infection screening and antibiotic use. In most cases, these obstetric interventions are unnecessary, and there is a suspicion of overtreatment of the parturient.8 Besides, a prospective cohort study conducted by Impey et al9 on 4915 participants showed that intrapartum fever is closely related to neonatal encephalopathy (OR=10.8, 95% CI: 4.0–29.3). The outcome model of intrapartum fever related to epidural labor analgesia showed that injection of IL-6 induced non-infectious fever in pregnant mice can lead to fetal neuritis.10 Therefore, it is urgent to find an effective method to reduce LEAF.
Understanding LEAF’s mechanism can help to adopt safe and effective prevention measures to reduce the fever rate during childbirth. Unfortunately, the exact pathogenesis of LEAF is not yet clear. Initially, LEAF was attributed to infection, but the mothers’ placental histological examination and blood culture with LEAF did not reveal microbes. Preoperative prophylactic antibiotics did not reduce the incidence of LEAF. However, parturients receiving labor epidural analgesia have significantly increased expression of IL-6 and other inflammatory factors.11–14 Therefore, the etiology of LEAF is most likely a non-infectious inflammatory reaction.13 Some clinical studies can support this theory. Kopsky DJ et al15 reported that the use of dexamethasone could reduce the LEAF. And this effect on the reduction of IL-6 levels caused by dexamethasone. However, LEAF’s pathogenesis is still in the exploratory stage, and there are limited clinical indicators. Therefore, it is meaningful to find newer and more convenient biomarkers to predict LEAF’s risk and provide new treatment options for the treatment of LEAF.
Studies have shown that magnesium sulfate has a protective effect on newborns’ brains. The use of magnesium sulfate before delivery can reduce cerebral palsy probability in preterm infants.16,17 Interestingly, a retrospective cross-sectional study18 showed that intrapartum fever incidence with and without magnesium sulfate was 6% and 10.2%, respectively, indicating magnesium sulfate can significantly reduce the incidence of intrapartum fever, but the mechanism is not precise. Further prospective studies are needed to confirm and evaluate the dose–effect relationship between them. In the rat model, magnesium sulfate inhibited the increase in maternal temperature caused by IL-6.10 Besides, in a small clinical study, it was found that when magnesium sulfate was injected intravenously, it was observed that pregnant women’s central core temperature decreased.19 Therefore, magnesium may also have a role in maternal fever. However, there are a few studies about the relationship between the serum magnesium level and LEAF. Here, we investigate whether the serum magnesium level is predictive of LEAF and becomes a potential target for LEAF treatment.
Materials and Methods
Patients and Study Design
This is a retrospective study in the west of China. We analyzed 528 participants who underwent labor epidural anesthesia from the Fujian Provincial Maternity and Children’s Health Hospital, affiliated hospital of Fujian Medical University, from January 2019 to June 2019. All populations must meet the following criteria: 1) Singleton head pregnancy; 2) age above 18 years; 3) 37–42 weeks of pregnancy; 4) basal body temperature is less than 37.5°C, no prenatal fever. Patients were excluded if pregnant women with upper respiratory tract infection, urinary tract infection, and postpartum placental umbilical cord pathological examination suggesting placental umbilical cord infection. The study was approved by the Hospital Ethics Committee (FMCH20181003), and all individuals participating in this study provided written informed consent. Detailed data on pregnancy health information and neonatal data were collected from computerized obstetric records, neonatal databases, and handwritten records.
Biomarker Assessment
Patients’ venous blood samples were obtained after at least 12 h of fasting after admission and stored at –80°C. Serum magnesium level is tested immediately by standardized methods using an automatic blood analyzer (7600–020; Hitachi, Ltd., Tokyo, Japan) following clinical laboratory guidelines.
Maternal LEAF Assessment
The primary outcome was the presence of LEAF, which was defined as a basal body temperature of ≥37.5°C (99.5°F) while getting labor epidural analgesia. Women who had at least one recorded temperature ≥of 37.5°C (99.5°F) were considered to have LEAF. As noted previously, participants without an adequate record of intrapartum temperatures were excluded. In an epidural catheter placement, the temperature measurement was defined as being taken within 2 hours before or 1 hour after labor epidural analgesia.
Statistical Analysis
T-tests analyzed the counting data, and the measurement data were used Chi-square tests. To evaluate the association between the serum magnesium level and LEAF, linear by linear analysis was performed. The data were calculated using the IBM SPSS statistical package version 22.0 (IBM Corporation, Armonk, NY, USA). The data were analyzed using GraphPad Prism 6.0. Diagnostic accuracy of serum magnesium level for LEAF was expressed as the area under the receiver operating characteristic (ROC) curve (AUC). The odd’s ratios (ORs) with 95% confidence intervals (CIs) were analyzed to estimated different risks. In all statistical tests, the differences were considered statistically significant at P-values <0.05.
Result
Patient Characteristics
Finally, a total of 528 patients were included in the study period. Demographic and clinical data from the study participants are presented in Table 1. Overall, 65 (12.30%) participants had the presence of LEAF and the mean serum magnesium was 0.76± 0.11 (mg/dl). The mean age was 28.21 ± 4.07 years, and the mean gestational age at delivery was 39.32±1.21 weeks. Furthermore, the mean gravity was 1.54± 0.72 times, and the mean parity was 0.37± 0.56 times, the mean height was 160.74± 4.83 cm, the mean weight was 67.63± 7.82 kg, the mean body mass index (BMI) was 26.24± 2.71 kg/m2. Of the patients, 180 (34.10%) had bulging membrane, 89 (16.90%) had gestational diabetes mellitus (GDM), 23 (4.40%) had gestational hypertension, and 41 (7.80%) had a postpartum hemorrhage. Also, 67 (12.70%) suffered cesarean delivery, 38 (7.20%) needed assisted vaginal delivery, and the rest (80.10%) was vaginal delivery successfully. The mean birth weight was 3327.64±370.12g, and 44 (8.30%) of the newborns needed neonatal intensive care unit (NICU).
 |
Table 1 Baseline Characteristics of Participants in the Study |
The Associations Between Risk Factors and LEAF
As shown in Table 2, all participants (N=528) were composed of those with LEAF (N=65) or without (N=463). This study revealed that the women with LEAF, versus without, were more likely to present for bulging membrane (43.08% vs 32.83%) (P=0.013) and had a higher incidence of gestational hypertension (9.23% vs 3.67%) (P=0.004). Furthermore, the mode of delivery (P=0.032), NICU admission (P=0.002), and the serum magnesium level (P<0.001) were significantly different between the two groups. We realized a significant difference in means of serum magnesium level in two groups (P<0.001, ANOVA test) (Figure 1A). There were no differences between the two groups when comparing age, gestational age, gravity, parity, height, weight, BMI, GDM, postpartum hemorrhage, and fetus’s birth weight during labor.
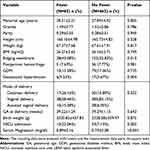 |
Table 2 The Correlation Between Clinical Factors and LEAF |
The Serum Magnesium Level is a Predictive Factor for the Presence of LEAF
ROC analyses of the serum magnesium level were performed (Figure 1B). We observed that AUC for the serum magnesium level was 0.825. Also, an optimal cut-off of the serum magnesium level was 0.855 mg/dl.
As shown in Table 3, the independent factors associated with the diagnosis of presence of LEAF were identified in the multiple logistic regressions. It is demonstrated that the serum magnesium level had the highest OR (OR = 7.49; 95% CI (4.58–14.35)) (P<0.001). The bulging membrane is an independent risk factor presence of LEAF (OR = 1.55; 95% CI (1.01–2.43)) (P=0.038).
 |
Table 3 Multiple Logistic Regression Analysis of Factors Associated with LEAF |
Discussion
This study indicated that the serum magnesium level showed a significant association with the presence of LEAF. Hence, our study may provide information with a new and possible biomarker to predict the presence of LEAF and offer a potential target for the treatment of the presence of LEAF.
Childbirth is a complex and highly individualized process. Long-term pain will have adverse effects on pregnant women’s physiology and psychology, which will affect the delivery process and the safety of the fetus. In recent years, with the advancement of anesthesiology and the change of people’s fertility awareness, more and more pregnant women have begun to adopt necessary analgesic measures to relieve labor pain and improve labor outcomes. However, the presence of LEAF seriously affects the promotion and application of labor analgesia technology.
In this study, 65 (12.30%) participants had the presence of LEAF, which was lower than that reported in the previous study.5 In clinical studies, LEAF incidence varies greatly, ranging from 1.6% to 46.3%,6 which may be due to different epidural drug concentrations or dose, infusion mode, and too long epidural sedation. Zhou X et al20 compared the different amounts with 0.075% ropivacaine and 0.125% ropivacaine combined with a 0.25 μg/mL sufentanil labor epidural analgesia, and the results showed a higher concentration of ropivacaine, the higher body temperature, and serum IL-6 level. Moreover, this study revealed that the mode of delivery (P=0.032) and NICU admission (P=0.002) were significantly different between the women with LEAF and without, which was similar to the previous study. Greenwell EA et al21 found that neonatal conditions including 1 min and 5 min Apgar scores were lower in women with LEAF than women without LEAF, and in women with LEAF, the incidence of fetal distress, intrauterine death, acidosis or hypoxemia, the rates of neonatal asphyxia, convulsions, assisted ventilation or cardiopulmonary resuscitation, oxygen therapy, and transfer to the NICU after delivery are all higher than those women without LEAF.
Currently, the mechanism of fever during childbirth has not been fully revealed. Presence of LEAF likely has multiple causes. The non-infection response is now the most likely mechanism for triggering LEAF because intrapartum fever has inflammation and cytokine production, but there is no acute infection evidence.22 The non-infection response occurs in the absence of pathogenic bacteria and is caused by some endogenous molecules released after tissue injury. These endogenous molecules can act through pattern recognition receptors, such as toll-like receptors, and ultimately lead to increased secretion of pro-inflammatory factors and fever-inducing cytokines in the body.5 In many kinds of research11–14 about presence of LEAF, the increase of IL-1, IL-6, and cytokines are involved. Therefore, the growth of IL-6 secretion is closely related to the presence of LEAF. However, the level of IL-6 in women during pregnancy gradually increases with the increase of gestational age and the progress of labor. It plays a vital role in maintaining normal pregnancy and labor initiation and is closely related to the intensity and frequency of contractions.14 Therefore, IL-6 cannot be used as a specific indicator in clinical practice.
As we are known, pregnant women with presence of LEAF increase adverse pregnancy outcomes for pregnant women and newborns. In this study, we demonstrated that the women with LEAF, versus those without, were more likely to had a higher incidence of gestational hypertension (9.23% vs 3.67%) (P=0.004) and a higher rate of cesarean delivery (P=0.032), which is similar to previous research.7 Therefore, there is an urgent need to clarify the specific pathophysiological mechanism of non-infectious inflammation caused by labor epidural analgesia to solve the presence of LEAF possible adverse clinical outcomes. Tian et al23 proposed that the maternal serum IL-6 level can be reduced to reduce the rate of LEAF presence. Kopsky DJ et al15 used an intraspinal injection of dexamethasone to observe its effect on fever in delivery patients. The results showed that intraspinal injection of dexamethasone had a significant impact on preventing the presence of LEAF. However, these research methods have medical deficiencies, so they have not been certified and recommended, and further research is needed.
Furthermore, this study demonstrated that the serum magnesium level showed a significant association with the presence of LEAF. Magnesium sulfate has antispasmodic, vasodilatory, and direct inhibition of uterine smooth muscle contraction to prevent premature birth, so it is widely used in pregnant women with obstetric pathological pregnancy. The therapeutic dose of magnesium sulfate has no apparent adverse reactions to pregnant women and fetuses.24 Clinical studies and animal model studies show that magnesium sulfate can lower body temperature.10,18 However, how magnesium sulfate affects body temperature regulation is not entirely known.
Magnesium-induced peripheral vasodilation may be thought to accelerate the drop in core temperature observed in healthy volunteers in research experimental settings.25 In a study of 3713 healthy postmenopausal women,26 it was found that high-magnesium dietary intake was associated with reduced systemic levels of inflammatory cytokines (such as IL-6). Therefore, magnesium may weaken the systemic inflammatory cascade, thereby decreasing the fever response during delivery.
As we knew, these are a few studies to describe this negative association between the serum magnesium level and the presence of LEAF. However, there are some limitations to this research. First, the specimen’s size was not big enough. For a more accurate evaluation, increasing the sample size may be necessary for future studies. Second, in our research, we did not further study the relationship between the serum magnesium level and maternal and neonatal outcome, which is worth further studying.
In conclusion, our results demonstrate that the serum magnesium level demonstrated higher significantly in presence of LEAF than absence. We advocate serum magnesium level as a suitable biomarker to predict the presence of LEAF. Our products may offer a useful target for the treatment of the presence of LEAF and promote the further development of labor epidural analgesia.
Ethics Approval
The Hospital Ethics Committee of Fujian Provincial Maternity and Children’s Hospital, an affiliated hospital of Fujian Medical University, approved the study (FMCH2017J01232) and complied with Helsinki’s Declaration.
Consent to Participate and Consent for Publication
All individuals participating in this study provided written informed consent.
Acknowledgments
The study was supported by grants from the Fujian Provincial Health Technology Project (grant no. 2019-CX-8). The authors want to thank the patients who made this study possible.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was supported by grants from the Fujian Provincial Health Technology Project (grant no. 2019-CX-8).
Disclosure
The authors declare that they have no competing interests.
References
1. Zheng H, Zheng BX, Lin XM. The Trend of Labor Analgesia in the World and China: a Bibliometric Analysis of Publications in Recent 30 Years. J Pain Res. 2020;13:517–526. doi:10.2147/JPR.S232132
2. Butwick AJ, Bentley J, Wong CA, et al. United States State-Level Variation in the Use of Neuraxial Analgesia During Labor for Pregnant Women. JAMA network open. 2018;1(8):e186567. doi:10.1001/jamanetworkopen.2018.6567
3. Lumbiganon P, Laopaiboon M, Gulmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet. 2010;375(9713):490–499. doi:10.1016/S0140-6736(09)61870-5
4. Li MJ, Xu Q, Li MY. The mechanism of labor pain and the usual methods of labor analgesia. Int Obstet Gynecol. 2018;45:125–129.
5. Sultan P, David AL, Fernando R, et al. Inflammation and epidural-related maternal fever: proposed mechanisms. Anesth Analg. 2016;122(5):1546–1553. doi:10.1213/ANE.0000000000001195
6. Sharpe EE, Arendt KW. Epidural Labor Analgesia and Maternal Fever[J]. Clin Obstet Gynecol. 2017;60(2):365–374. doi:10.1097/GRF.0000000000000270
7. Segal S. Labor epidural analgesia and maternal fever. Anesth Analg. 2010;111(6):1467–1475. doi:10.1213/ANE.0b013e3181f713d4
8. White A, Olson D, Messacar K. A statewide assessment of the association between epidural analgesia, maternal fever, and neonatal antibiotics in Colorado, 2007- 2012. Arch Dis Child Fetal Neonatal Ed. 2017;102(2):F120–F125 . doi:10.1136/archdischild-2015-309985
9. Impey L, Greenwood C, McQuillan K, et al. Fever in Labour and Neonatal Encephalopathy: a Prospective Cohort Study. BJOG. 2001;108(6):594–597. doi:10.1111/j.1471-0528.2001.00145.x
10. Segal S, Pancaro C, Bonney I, et al. Non-infectious Fever in the Near- Term Pregnant Rat Induces Fetal Brain Inflammation: a Model for the Consequences of Epidural- associated Maternal Fever. Anesth Analg. 2017;125(6):2134–2140. doi:10.1213/ANE.0000000000002479
11. Sharma SK, Rogers BB, Alexander JM, et al. A Randomized Trial of the Effects of Antibiotic Prophylaxis on Epidural- Related Fever in Labor. Anesth Analg. 2014;118(3):604–610. doi:10.1213/ANE.0b013e3182a5d539
12. Goetzl L, Evans T, Rivers J, et al. Elevated maternal and fetal serum interleukin- 6 levels are associated with epidural fever. Am J Obstet Gynecol. 2002;187(4):834–838. doi:10.1067/mob.2002.127135
13. Riley LE, Celi AC, Onderdonk AB, et al. Association of Epidural- Related Fever and Non-infectious Inflammation in Term Labor. Obstet Gynecol. 2011;117(3):588–595. doi:10.1097/AOG.0b013e31820b0503
14. Mantha VR, Vallejo MC, Vimala R, et al. Maternal and Cord Serum Cytokine Changes with Continuous and Intermittent Labor Epidural Analgesia: a Randomized Study. Sci World J. 2012;2012:607938. doi:10.1100/2012/607938
15. Kopsky DJ. Phenytoin cream for the treatment for neuropathic pain: case series. Pharmaceuticals. 2018;11(2):53. doi:10.3390/ph11020053
16. Chollat C, Sentilhes L, Market S. Protection of brain development by antenatal magnesium sulfate for infants born preterm. Dev Med Child Neurol. 2019;61(1):25–30. doi:10.1111/dmcn.14038
17. Burd I, Breen K, Friedman A, et al. Magnesium sulfate reduces inflammation- associated brain injury in fetal mice. Am J Obstet Gynecol. 2010;202(3):292.e1–292.e9. doi:10.1016/j.ajog.2010.01.022
18. Lange EMS, Segal S, Pancaro C, et al. Association between Intrapartum Magnesium Administration and the Incidence of Maternal Fever: a Retrospective Cross-sectional Study. Anesthesiology. 2017;127(6):942–952. doi:10.1097/ALN.0000000000001872
19. Parsons MT, Owens CA, Spellacy WN. Thermic effects of tocolytic agents: decreased temperature with magnesium sulfate. Obstet Gynecol. 1987;69(1):88–90.
20. Zhou X, Li J, Deng S, et al. Ropivacaine at different concentrations on intrapartum fever, IL- 6 and TNF- α in a parturient with epidural labor analgesia. Exp Ther Med. 2019;17(3):1631–1636. doi:10.3892/etm.2018.7121
21. Greenwell EA, Wyshak G, Ringer SA, et al. Intrapartum Temperature Elevation, Epidural Use, and Adverse Outcome in Term Infants. PEDIATRICS. 2012;129(2):e447–e454 . doi:10.1542/peds.2010-2301
22. Del Arroyo AG, Sanchez J, Patel S, et al. Role of leucocyte caspase-1 activity in epidural-related maternal fever: a single-center, observational, mechanistic cohort study. Br J Anaesth. 2019;122(1):92–102. doi:10.1016/j.bja.2018.09.024
23. Tian F, Wang K, Hu J, et al. Continuous spinal anesthesia with sufentanil in labor analgesia can induce maternal febrile responses in puerpera. Int J Clin Exp Med. 2013;6(5):334–341.
24. Doyle LW, Crowther CA, Middleton P, et al. Antenatal magnesium sulfate and neurologic outcome in preterm infants: a systematic review. Obstet Gynecol. 2009;113:1327–1333. doi:10.1097/AOG.0b013e3181a60495
25. Zweifler RM, Voorhees ME, Mahmood MA, et al. Magnesium sulfate increases the rate of hypothermia via surface cooling and improves comfort. Stroke. 2004;35:2331–2334. doi:10.1161/01.STR.0000141161.63181.f1
26. Chacko SA, Song Y, Nathan L, et al. Relations of dietary magnesium intake to biomarkers of inflammation and endothelial dysfunction in an ethnically diverse cohort of postmenopausal women. Diabetes Care. 2010;33:304–310. doi:10.2337/dc09-1402
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

