Back to Journals » Psychology Research and Behavior Management » Volume 15
Serum CC Chemokines as Potential Biomarkers for the Diagnosis of Major Depressive Disorder
Authors Gao W, Xu Y, Liang J, Sun Y, Zhang Y, Shan F, Ge J, Xia Q
Received 29 July 2022
Accepted for publication 5 October 2022
Published 11 October 2022 Volume 2022:15 Pages 2971—2978
DOI https://doi.org/10.2147/PRBM.S384267
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Wenfan Gao,1– 4,* Yayun Xu,5– 7,* Jun Liang,1– 4 Yanhong Sun,1– 4 Yuanyuan Zhang,1– 4 Feng Shan,1– 4 Jinfang Ge,6– 8 Qingrong Xia1– 4
1Affiliated Psychological Hospital of Anhui Medical University, Hefei, People’s Republic of China; 2Department of Pharmacy, Hefei Fourth People’s Hospital, Hefei, People’s Republic of China; 3Psychopharmacology Research Laboratory, Anhui Mental Health Center, Hefei, People’s Republic of China; 4Anhui Clinical Research Center for Mental Disorders, Hefei, People’s Republic of China; 5Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, People’s Republic of China; 6Inflammation and Immune Mediated Diseases Laboratory of Anhui Province, Anhui Institute of Innovative Drugs, Anhui Medical University, Hefei, People’s Republic of China; 7The Key Laboratory of Anti-Inflammatory and Immune Medicines, Ministry of Education, Hefei, People’s Republic of China; 8School of Pharmacy, Anhui Medical University, Hefei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jinfang Ge, School of Pharmacy, Anhui Medical University, 81 Meishan Road, Hefei, 230000, People’s Republic of China, Email [email protected] Qingrong Xia, Department of Science and Education, Hefei Fourth People’s Hospital, Affiliated Psychological Hospital of Anhui Medical University, Anhui Mental Health Center, 316 Huangshan Road, Hefei, 230000, People’s Republic of China, Email [email protected]
Objective: Evidence indicates a potential role of chemokines in depression-like behavior and depression-related pathophysiological processes. In the present study, we examined the serum levels of multiple chemokines, focusing on CC chemokines, in patients with major depressive disorder (MDD), with the aim to discover and identify serum chemokines-based biomarkers for MDD diagnosis.
Methods: Participants included 24 patients with MDD and 24 healthy controls. The 24-item Hamilton Depression Rating Scale (HAMD-24) was administered to assess the disease severity of patients with MDD. A total of 9 serum CC chemokines including MCP-1 (CCL-2), MIP-1α (CCL-3), MIP-1β (CCL-4), eotaxin-1 (CCL-11), MCP-4 (CCL-13), TARC (CCL-17), MIP-3α (CCL-20), MDC (CCL-22), and Eotaxin-3 (CCL-26) were measured using electrochemiluminescence immunoassays. The levels of serum CC chemokines between MDD group and control group were compared, and diagnostic values of different CC chemokines were evaluated using the receiver operating characteristic (ROC) curve method for discriminating MDD patients from healthy controls. Correlations between the levels of serum CC chemokines and depression severity (HAMD-24 scores) were evaluated using Pearson’s correlation test.
Results: Patients with MDD had higher levels of serum MIP-1α and MIP-1β and lower levels of serum MCP-1, MCP-4, TARC, MDC, and Eotaxin-3 compared to controls (all P < 0.05). Moreover, ROC curve analysis showed that the Area Under Curve (AUC) values of MIP-1α, MCP-4, TARC, and Eotaxin-3 were > 0.7 in discriminating patients with MDD from healthy controls. Furthermore, no significant relationship was found between the levels of serum CC chemokines and HAMD-24 scores in MDD group.
Conclusion: These results suggested that circulating CC chemokines may hold promise in the discovery of biomarkers for diagnosing MDD.
Keywords: chemokines, biomarker, diagnosis, serum, major depressive disorder
Introduction
Major depressive disorder (MDD) is one of the most common psychiatric disorders.1 According to the latest nationwide survey of mental disorders in China, MDD has a lifetime prevalence of 3.4%, affecting approximately 44 million people.2 Characterized by high morbidity, mortality and disability rates, MDD impose a heavy burden on individuals and society.3 Currently, the diagnosis of depression primarily depends on subjective symptoms/manifestations, with uncertainties as high as 40% as a consequence.4 Therefore, an urgent but unmet need exists to identify objective biomarkers of depression, especially MDD.
Chemokines, a group of small (8–14 kDa) polypeptides, are divided into four subfamilies: C, CC, CXC and CX3C, based on the number and spacing of cysteine residues within their N-terminal regions.5 Among them, CC and CXC chemokines have been identified as the two largest groups of chemokines in mammals.6 Numerous evidence has demonstrated chemokines as an important group of molecules in both the immune system and the nervous system.7 In the immune system, chemokines act to coordinate immune cells and attract them to sites of ongoing inflammation. In the nervous system, chemokines play a role in neuron-glia communication, synaptic transmission, neurogenesis, neurodevelopment and plasticity. Due to their role in cellular migration and immune coordination, chemokines are prime candidates for linking peripheral and central inflammation and orchestrating neuroinflammatory crosstalk.6 It is worth noting that chemokines have been implicated in depression by facilitating migration of peripheral immune cells into the central nervous system.8 Preclinical studies revealed abnormal expression of chemokines in animal models of depression.9 For example, it has been reported that the levels of CCL2 and CXCL12 in the hippocampus and frontal cortex were significantly increased in prenatally stressed rats.10 On the contrary, chemokine disturbance can induce depression-like behavioral changes in animals. Indeed, intraperitoneal injection of CXCL1 showed the reduced spontaneous exploratory activity and burrowing behavior in rats.11 Consistently, distorted levels of chemokines can also be found in peripheral blood of patients with depression in clinical studies.12,13 It has been demonstrated that MDD patients with suicidal ideation had lower level of CCL2 compared to control subjects.14 Taken together, these findings suggest a close link between chemokines and depression.
In the present study, we examined the serum levels of multiple chemokines, focusing on CC chemokines, in patients with MDD, with the aim to discover and identify serum chemokines-based biomarkers for MDD diagnosis.
Materials and Methods
Study Design and Participants
This study was conducted at Anhui Mental Health Center between August 2020 and June 2022. Twenty-four patients with MDD were screened via psychiatric interviews by an experienced researcher in accordance with the guidelines of the structured clinical interview according to the Diagnostic and Statistical Manual for Psychiatric Disorders-Fifth Version (DSM-V). The common criteria for inclusion were as follows: (1) being between the ages of 18–65; (2) meeting the diagnostic criteria of depression listed in the DSM-V; (3) Hamilton Depression Rating Scale-24 (HAMD-24) scores > 20; and (4) receiving no treatment with antidepressants, anti-inflammatory agents or other psychotropic drugs in the previous 3 months. The exclusion criteria were as follows: (1) other major psychiatric disorders or neurodegenerative illness history; (2) substance abuse (drug, caffeine, nicotine, alcohol, or others); (3) serious heart, brain, liver, kidney, immune disorders, obesity, poor nutrition, acute and chronic infection. Health subjects received HAMD-24 assessment and a total of 24 subjects met the requirement of a HAMD-24 score of < 8 were enrolled in the present study. This procedure was approved by the ethics committee of Hefei Fourth People’s Hospital (registration number HFSY-IRB-PJ-XQR-2020001) and was conducted according to the principles of the Declaration of Helsinki. Informed consent was obtained from all the participants.
Blood Sample Collection and Measurement of Serum Cytokines
Blood samples from the subjects were collected from the participants’ vein between 7:00 A.M. and 8:00 A.M., and immediately centrifuged at 1, 200 × g for 10 min at 4°C. The supernatant was extracted as a serum sample. In order to avoid the time effect, all the samples were stored at −80°C until detection. Moreover, the control samples were matched as closely as possible to the MDD group with respect to the time period of sample collection. A total of 9 serum CC chemokines including MCP-1 (CCL-2), MIP-1α (CCL-3), MIP-1β (CCL-4), eotaxin-1 (CCL-11), MCP-4 (CCL-13), TARC (CCL-17), MIP-3α (CCL-20), MDC (CCL-22), and eotaxin-3 (CCL-26) were measured using a commercially available multiplex electrochemiluminescence immunoassay (a V-PLEX Human Biomarker 54-Plex Kit; Meso Scale Discovery [MSD], Rockville, MD, USA; kit number: K15248D). To ensure that the results were not unduly influenced by a single data point and as is the convention, outliers (datapoint >3 SD above or below the mean) were removed from the dataset.
Statistical Analysis
The data were analyzed using SPSS (version 17.0; IBM Corp., Armonk, NY, USA). The data are expressed as mean ± standard error of the mean (SEM), and the statistical significance was set at P < 0.05. A one-sample Kolmogorov–Smirnov test showed a normal distribution of continuous variables. Student’s t-test for independent samples was used to compare the age, BMI, serum chemokines between control group and MDD group. Sex differences between the groups were tested using the chi-square test. Correlation analyses were performed using Pearson correlation tests. Receiver operating characteristic (ROC) curve analysis was used to evaluate the area under the curve (AUC) of serum chemokines in discriminating MDD patients from healthy controls. Given the small sample size, we computed the post-hoc power of two-sample t-test (two groups) using G*Power (version 3.1.9.2, University of Kiel, Kiel, Germany).
Results
Demographic and Clinical Characteristics of the Participants
Table 1 summarizes the demographic and clinical characteristics of participants. There was no statistically significant difference in age (t = 1.373, P = 0.176), sex (χ2 = 0.000, P = 1.000), or BMI (t = 1.214, P = 0.232) between patients with MDD and healthy controls. The mean HAMD-24 scores of the MDD group were significantly higher than those of the control group (t = −19.014, P < 0.001).
 |
Table 1 Clinical Characteristics of Control Group and MDD Group |
Comparison of Serum CC Chemokines Between Patients with MDD and Healthy Controls
The levels of serum CC chemokines of MDD patients and healthy controls are shown in Table 2. Compared to controls, patients with MDD exhibited higher levels of MIP-1α and MIP-1β and lower levels of MCP-1, MCP-4, TARC, MDC, and eotaxin-3 (Table 2 and Figure 1; all P < 0.05). No significant differences in other cytokines levels including eotaxin-1 and MIP-3α were found between groups. Post hoc power analyses demonstrated that the power of our study was sufficient (power > 0.80) for MIP-1α, MCP-4, TARC, MDC, and Eotaxin-3 (Table 2).
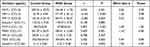 |
Table 2 Comparison of Serum Cytokines Between Control Group and MDD Group |
Diagnostic Values of Different CC Chemokines in Discriminating Patients with MDD from Healthy Controls
The diagnostic performance of different CC chemokines in discriminating patients with MDD from healthy controls were performed by ROC curve analysis (Figure 2). The results showed that the AUC values of MCP-1, MIP-1α, MIP-1β, MCP-4, TARC, MDC, and eotaxin-3 were 0.673, 0.891, 0.650, 0.980, 0.854, 0.699, and 0.779, respectively. Among them, the AUCs of MIP-1α, MCP-4, TARC, and eotaxin-3 were > 0.7, indicating that these 4 CC chemokines had good diagnostic value (Table 3). At a cut-off point of 34.92 pg/mL for MIP-1α, the sensitivity and specificity were 87.5% and 87.5%, respectively; at a cut-off point of 46.31 pg/mL for MCP-4, the sensitivity and specificity were 95.5% and 89.5%, respectively; at a cut-off point of 136.30 pg/mL for TARC, the sensitivity and specificity were 72.7% and 84.2%, respectively; at a cut-off point of 3.20 pg/mL for eotaxin-3, the sensitivity and specificity were 63.6% and 84.2%, respectively. A combined panel of MIP-1α, MCP-4, TARC, and Eotaxin-3 achieved a high accuracy in discriminating patients with MDD from healthy controls (AUC = 1.000).
 |
Table 3 ROC Analysis of Different Cytokines in Discriminating Patients with MDD from Healthy Volunteers |
Correlation Between HAMD-24 Scores and the Levels of Serum CC Chemokines in MDD Group
Figure 3 shows the relationship between serum CC chemokines levels and HAMD-24 scores. No significant relationship was found between the levels of serum CC chemokines and HAMD-24 scores in MDD group (all P > 0.05; Figure 3A). The data of serum CC chemokines levels were log (base 2) transformed, and the result of Pearson correlation test showed that there was still no correlations between serum CC chemokines and HAMD-24 scores in MDD group (all P > 0.05; Figure 3B).
Discussion
The present study compared the levels of 9 CC chemokines in patients with MDD and healthy controls, with the aim to identify serum chemokines-based biomarkers for MDD. Three main findings emerged in the present study. Firstly, patients with MDD had higher levels of serum MIP-1α and MIP-1β and lower levels of serum MCP-1, MCP-4, TARC, MDC, and Eotaxin-3 compared to controls. Secondly, ROC curve analysis showed that the AUC values of MIP-1α, MCP-4, TARC, and Eotaxin-3 were > 0.7 in discriminating patients with MDD from healthy controls. Thirdly, no significant relationship was found between the levels of serum CC chemokines and HAMD-24 scores in MDD group.
The CC class chemokines are most abundant chemokines, and this class includes 27 proteins: CCL1-CCL28 (CCL9 and CCL10 correspond to the same protein). Among them, MCP-1 (CCL-2), MIP-1α (CCL-3), MIP-1β (CCL-4), and eotaxin-1 (CCL-11) are thought to be closely linked to depression.6 Given that Meso Scale Discovery (MSD) has several advantages over classical ELISA, including greater sensitivity and dynamic range, the potential for multiplexing, and smaller quantities of sample used during testing,15 this method was performed to measure the levels of the above 4 CC chemokines. For the simultaneous detection of MCP-1 (CCL-2), MIP-1α (CCL-3), MIP-1β (CCL-4), and eotaxin-1 (CCL-11), a V-PLEX Human Biomarker 54-Plex Kit (MSD; kit number: K15248D) was selected. The kit contains the detection of a total of 9 CC chemokines including MCP-1 (CCL-2), MIP-1α (CCL-3), MIP-1β (CCL-4), eotaxin-1 (CCL-11), MCP-4 (CCL-13), TARC (CCL-17), MIP-3α (CCL-20), MDC (CCL-22), and eotaxin-3 (CCL-26). Therefore, these 9 CC chemokines were used to identify serum chemokines-based biomarkers for MDD diagnosis.
In this study, patients with MDD exhibited higher levels of MIP-1α (CCL-3) and MIP-1β (CCL-4). Consistently, another two studies have also found a increase in circulating MIP-1α in depressed patients.13,16 In terms of MIP-1β, studies concerning MIP-1β levels in the peripheral blood of patients with depression have been inconsistent. It has been reported that the serum levels of MIP-1β were significantly increased in pregnant women with anxiety and depression compared to the control group, and a positive relationship was found between MIP-1β levels and severity of depressive symptoms.17 However, another study have shown that the serum levels of MIP-1β was significantly decreased in patients with MDD compared to healthy controls.18 The source of the contradictions between these reports remains unclear. Considering that MIP-1α and MIP-1β are both pro-inflammatory chemokines,19 up-regulations of their levels in patients with MDD in the present study are supportive of the mainstream opinion that depression is accompanied by activation of the inflammatory system.20,21
Lower levels of MCP-1, MCP-4, TARC, MDC, and Eotaxin-3 were found in MDD group compared to control group in the present study. MCP-1 (CCL2), known as one of the inflammatory chemokines, critically regulate leukocyte recruitment during inflammatory responses.22 Several studies have explored the circulating levels of MCP-1 in depressed patients and reported conflicting results. On the one hand, an increased MCP-1 levels in serum were observed in patients with depression.23 On the other hand, there are also studies reported a decreased or unchanged level of this chemokine.24,25 In terms of MCP-4 (CCL13) and TARC (CCL17), only one study found significant decreases in cerebrospinal fluid levels of MCP-4 and TARC in patients who attempted suicide compared to with healthy control subjects.26 To the best of our knowledge, the present study firstly investigated the serum levels of MDC (CCL22) and Eotaxin-3 (CCL26) in patients with MDD. Therefore, these abnormally expressed chemokines may provide more possibilities for the selection of diagnostic markers for depression.
In order to explore the potential values of these aberrant chemokines as diagnostic biomarkers of MDD, ROC analysis was further applied. Given that AUC value in ROC analysis should be > 0.7 to be of clinical value for screening,27 a total of 4 chemokines including MIP-1α, MCP-4, TARC, and Eotaxin-3 meet this condition. Among them, MCP-4 showed outstanding discrimination ability with a AUC value of 0.978, and MIP-1α, TARC, and Eotaxin-3 showed excellent discrimination ability with AUCs > 0.7 in discriminating patients with MDD from healthy controls. It has been shown that combined detection of multiple serum proteins as a single panel can increase the sensitivity or specificity of a single biomarker.28 Therefore, we have added a combination of MIP-1α, MCP-4, TARC, and Endotoxin-3 for the diagnosis of MDD. The results showed that the AUC value of this panel increased to 1.000, indicating that this panel hold significant promise as biomarkers for identification of patients with MDD.
HAMD-24 is the most widely used interview scale for the selection of patient with depression.29,30 Thus, the occurrence and severity of depression were evaluated by HAMD-24 in the present study. Correlations between the levels of serum CC chemokines and HAMD-24 scores in MDD group were evaluated. The results showed that there was no significant relationship between the levels of serum CC chemokines and HAMD-24 scores in MDD group.
There are some limitations to this study. Firstly, the present study is a single-center study with a relatively small sample size, which might represent sampling bias. Secondly, this cross-sectional study cannot explore the causal relationship between depression and these aberrant chemokines. Thirdly, not all CC chemokines were analyzed due to the limitations in detection technology. Fourthly, another limitation of our study is the long period (almost 2 years) over which the samples were collected.
In summary, the present study reveals that 4 CC chemokines including MIP-1α, MCP-4, TARC, and Eotaxin-3 may be of potential to be used as diagnostic biomarkers in discriminating patients with MDD. Multicentric studies are clearly required to validate the potential of these chemokines as novel biomarkers for MDD, and longitudinal studies examining the causal relationship between aberrant chemokines and depression are warranted.
Data Sharing Statement
All the data can be requested from the corresponding author upon reasonable request.
Ethics and Approval and Consent to Participate
This study was approved by the ethics committee of Hefei Fourth People’s Hospital (registration number HFSY-IRB-PJ-XQR-2020001). Individual written consent was required.
Consent for Publication
Informed consent was obtained from all subjects involved in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was provided by the National Natural Science Foundation of China (81870403), Key Research and Development Program of Anhui Province (202004j07020001), Hefei Sixth cycle Key Medical Specialty, and Anhui Province Medical and Health Key Specialty Construction Project.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Li Z, Ruan M, Chen J, Fang Y. Major depressive disorder: advances in neuroscience research and translational applications. Neurosci Bull. 2021;37:863–880. doi:10.1007/s12264-021-00638-3
2. Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211–224. doi:10.1016/S2215-0366(18)30511-X
3. Vos T, Allen C, Arora M. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi:10.1016/S0140-6736(16)31678-6
4. Mogi T, Toda H, Yoshino A. Clinical characteristics of patients with diagnostic uncertainty of major depressive disorder. Asian J Psychiatr. 2017;30:159–162. doi:10.1016/j.ajp.2017.10.001
5. Chen K, Bao Z, Tang P, Gong W, Yoshimura T, Wang J. Chemokines in homeostasis and diseases. Cell Mol Immunol. 2018;15:324–334.
6. Leighton S, Nerurkar L, Krishnadas R, Johnman C, Graham G, Cavanagh J. Chemokines in depression in health and in inflammatory illness: a systematic review and meta-analysis. Mol Psychiatry. 2018;23:48–58. doi:10.1038/mp.2017.205
7. Campuzano S, Yáñez-Sedeño P, Pingarrón J. Revisiting Electrochemical Biosensing in the 21st Century Society for Inflammatory Cytokines Involved in Autoimmune, Neurodegenerative, Cardiac, Viral and Cancer Diseases. Sensors. 2020;1;21.
8. Wohleb E, McKim D, Sheridan J, Godbout J. Monocyte trafficking to the brain with stress and inflammation: a novel axis of immune-to-brain communication that influences mood and behavior. Front Neurosci. 2014;8:447. doi:10.3389/fnins.2014.00447
9. Ślusarczyk J, Trojan E, Chwastek J, Głombik K, Basta-Kaim A, Potential A. Contribution of Chemokine Network Dysfunction to the Depressive Disorders. Curr Neuropharmacol. 2016;14:705–720. doi:10.2174/1570159x14666160219131357
10. Ślusarczyk J, Trojan E, Głombik K, et al. Prenatal stress is a vulnerability factor for altered morphology and biological activity of microglia cells. Front Cell Neurosci. 2015;9:82. doi:10.3389/fncel.2015.00082
11. Campbell S, Meier U, Mardiguian S, et al. Sickness behaviour is induced by a peripheral CXC-chemokine also expressed in multiple sclerosis and EAE. Brain Behav Immun. 2010;24:738–746. doi:10.1016/j.bbi.2010.01.011
12. Powell T, McGuffin P, D’Souza U, et al. Putative transcriptomic biomarkers in the inflammatory cytokine pathway differentiate major depressive disorder patients from control subjects and bipolar disorder patients. PLoS One. 2014;9:e91076. doi:10.1371/journal.pone.0091076
13. Simon N, McNamara K, Chow C, et al. A detailed examination of cytokine abnormalities in Major Depressive Disorder. Eur Neuropsychopharmacol. 2008;18:230–233. doi:10.1016/j.euroneuro.2007.06.004
14. Grassi-Oliveira R, Brieztke E, Teixeira A, et al. Peripheral chemokine levels in women with recurrent major depression with suicidal ideation. Rev brasileira de psiquiatria. 2012;34:71–75. doi:10.1590/s1516-44462012000100013
15. Kiris E, Kota K, Burnett J, Soloveva V, Kane C, Bavari S. Recent developments in cell-based assays and stem cell technologies for botulinum neurotoxin research and drug discovery. Expert Rev Mol Diagn. 2014;14:153–168. doi:10.1586/14737159.2014.867808
16. Merendino R, Di Pasquale G, De Luca F, et al. Involvement of fractalkine and macrophage inflammatory protein-1 alpha in moderate-severe depression. Mediators Inflamm. 2004;13:205–207. doi:10.1080/09511920410001713484
17. Camacho-Arroyo I, Flores-Ramos M, Mancilla-Herrera I, et al. Chemokine profile in women with moderate to severe anxiety and depression during pregnancy. BMC Pregnancy Childbirth. 2021;21:807. doi:10.1186/s12884-021-04225-2
18. Lehto S, Niskanen L, Herzig K, et al. Serum chemokine levels in major depressive disorder. Psychoneuroendocrinology. 2010;35:226–232. doi:10.1016/j.psyneuen.2009.06.007
19. Ko H, Lim S. Production of macrophage inflammatory protein (MIP)-1alpha and MIP-1beta by human polymorphonuclear neutrophils stimulated with Porphyromonas endodontalis lipopolysaccharide. J Endod. 2002;28:754–757. doi:10.1097/00004770-200211000-00002
20. Petralia M, Mazzon E, Fagone P, et al. The cytokine network in the pathogenesis of major depressive disorder. Autoimmunity Rev. 2020;19:102504. doi:10.1016/j.autrev.2020.102504
21. Lee C, Giuliani F. The Role of Inflammation in Depression and Fatigue. Front Immunol. 2019;10:1696.
22. Zhu S, Liu M, Bennett S, Wang Z, Pfleger K, Xu J. The molecular structure and role of CCL2 (MCP-1) and C-C chemokine receptor CCR2 in skeletal biology and diseases. J Cell Physiol. 2021;236:7211–7222. doi:10.1002/jcp.30375
23. Piletz J, Halaris A, Iqbal O, et al. Pro-inflammatory biomakers in depression: treatment with venlafaxine. World J Biol Psychiatry. 2009;10:313–323. doi:10.3109/15622970802573246
24. Black C, Miller B. Meta-Analysis of Cytokines and Chemokines in Suicidality: distinguishing Suicidal Versus Nonsuicidal Patients. Biol Psychiatry. 2015;78:28–37. doi:10.1016/j.biopsych.2014.10.014
25. Brietzke E, Anna M, Teixeira A, Kapczinski F. Abnormalities in serum chemokine levels in euthymic patients with bipolar disorder. Brain Behav Immun. 2009;23:1079–1082. doi:10.1016/j.bbi.2009.04.008
26. Janelidze S, Ventorp F, Erhardt S, et al. Altered chemokine levels in the cerebrospinal fluid and plasma of suicide attempters. Psychoneuroendocrinology. 2013;38:853–862. doi:10.1016/j.psyneuen.2012.09.010
27. Swets J. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–1293.
28. Luo P, Yin P, Hua R, et al. A Large-scale, multicenter serum metabolite biomarker identification study for the early detection of hepatocellular carcinoma. Hepatology. 2018;67:662–675. doi:10.1002/hep.29561
29. Wang X, Zhou X, Dai Q, Ji B, Feng Z. The Role of Motivation in Cognitive Reappraisal for Depressed Patients. Front Hum Neurosci. 2017;11:516. doi:10.3389/fnhum.2017.00516
30. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi:10.1136/jnnp.23.1.56
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



