Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Serum Calcium Levels and in-Hospital Infection Risk in Patients with Acute Ischemic Stroke
Authors Chen X, Liang X, Zhang J, Chen L, Sun J, Cai X
Received 5 January 2022
Accepted for publication 7 April 2022
Published 3 May 2022 Volume 2022:18 Pages 943—950
DOI https://doi.org/10.2147/NDT.S354447
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jun Chen
Xueping Chen,1,2 Xiaoxue Liang,2 Jun Zhang,1,2 Liujing Chen,1,2 Jingping Sun,2 Xueli Cai2
1Zhejiang University, School of Medicine, Hangzhou, Zhejiang, 310005, People’s Republic of China; 2Department of Neurology, Lishui Hospital of Zhejiang University (Lishui Municipal Central Hospital), Lishui, Zhejiang, 323000, People’s Republic of China
Correspondence: Xueli Cai; Jingping Sun, Department of Neurology, Lishui Hospital of Zhejiang University (The Central Hospital of Lishui), No. 289, KuoCang Street, Lishui, Zhejiang, 323000, People’s Republic of China, Tel +8613967059836 ; +860578-2285330, Email [email protected]; [email protected]
Purpose: Stroke-associated infection (SAI) is one of the most common post-stroke complications, which may lead to a relatively poor prognosis. This study aims to explore the potential relationship between serum calcium levels and SAI.
Patients and Methods: This is a cross-sectional study involving 395 participants. SAI is a term that covers stroke-associated pneumonia (SAP), urinary tract infection (UTI), as well as other infections diagnosed during the first week after a stroke. Serum calcium levels were measured within 24 hrs of admission. To determine the association of serum calcium levels with the SAI, logistic regression models were calculated. An adjusted spline regression model was used to further confirm the relationship between the two.
Results: Among the total patients, SAI occurred in 107 (27.1%) patients. Serum calcium was associated with SAI and was independent of the SAI risk factors for age, admission NIHSS score, and intravascular therapy [adjusted OR 0.040 (95% CI = 0.005– 0.291), p = 0.002]. Remarkably, this trend applies predominantly to serum calcium levels less than 2.25mmol/L (p= 0.005 for linearity).
Conclusion: Serum calcium levels are associated with the risk of SAI, when serum calcium is below normal (2.25mmol/L), the risk of SAI increases as serum calcium levels decrease.
Keywords: calcium homeostasis, stroke-associated infection, pneumonia, risk factors
Introduction
Stroke, characterised by a high morbidity, high disability rate and high mortality rate.1 According to the data from the Ministry of Health China Stroke Prevention Project Committee (CSPPC), from 2012 to 2018, stroke prevalence in China increased at an average annual rate of 12% (95% CI: 10.9% - 13.3%), placing a heavy burden on society and families.2 Recently, a large-scale domestic epidemiological study data shows that in China, even in the current situation of continuous improvement of acute ischemic stroke (AIS) diagnosis and treatment process and continuous improvement of prognosis, the mortality rate during the first hospitalization with AIS is still as high as 0.9% (95% CI: 0.8%-1.1%).3 Prevention and treatment of stroke-related complications is an important measure to improve stroke prognosis. SAI is one of the most common complications after experiencing a stroke. Studies have shown that the incidence of SAI in hospitals is as high as 30%, with stroke-associated pneumonia (SAP) being the most common type.4 However, in the early stages of stroke, common diagnostic features of pneumonia, such as fever, cough, and purulent sputum, are not obvious. This means that there is greater need for more sensitive and easily accessible SAI markers to help in its early detection. The occurrence of SAI is associated with post-stroke stress and immunosuppression,5 and severe neurological deficiencies, dysphagia, as well as underlying lung disease are all risk factors associated with SAI.6 Studies have found that many indicators related to inflammation and stress may help to predict the occurrence of SAI, but these indicators are not routine, large-scale clinical popularization is a bit tricky.7
Calcium ions are involved in a variety of physiological and pathological functions of the human body and play an important role in immunity. As a second messenger, this cation has been central in expanding our understanding of various physiological functions of immune cells, including proliferation, receptor-induced activation, secretion, phagocytosis, and cell death.8 Studies have shown that calcium deficiency in the body can cause abnormal calcium signals9; furthermore, chronic hypocalcemia can significantly affect the intracellular concentrations of calcium.10 Therefore, hypocalcemia may lead to immune dysfunction in the body, further leading to an increased incidence of infection. This has been confirmed in some animal studies.11 So far, however, there has been a lack of studies to explore the correlation between serum calcium and SAI. In this study, we aim to uncover this relationship.
Materials and Methods
Study Design
We enrolled patients from a retrospective clinical database that included consecutive patients who were admitted to the Lishui City Center Hospital, within 24 hrs after the onset of ischemic stroke between January 2020 to January 2021.
Inclusion and Exclusion Criteria
The inclusion criteria were for patients who suffered from ischemic stroke within 24 hours of the onset of the disease at the age of 18 or greater. Exclusion criteria were: 1) those who were prescribed calcium channel blockers or antibiotics during hospitalization within 2 weeks prior to hospitalisation; 2) any infection or pyrexia within 2 weeks prior to hospitalisation; 3) signs or symptoms suggestive of infection at admission; 4) if immunosuppressants or glucocorticoids were used within 3 months of admission; and 5) if tracheal intubation is required to assist in ventilation. Ultimately, a total of 395 patients were included in the analyses (Figure 1).
 |
Figure 1 Flow Diagram of the Participant Selection. SAI, stroke-associated infection; CCB, calcium channel blockers. |
Infectious Endpoints
The observed outcome of the study was the presence of SAP within 7 days of hospitalization. SAI refers to SAP, UTI, as well as other infections, which are diagnosed during the first week after a stroke. Or the diagnostic criteria for infections refer to the US Centers for Disease Control and Prevention standards.12 Briefly, SAI is defined as any form of infection that occurs within 7 days of onset of a stroke and is manifested by a fever (>37.5°C) or an elevated white blood cell count (≥1.2×109/L), with clinical manifestations of the corresponding organ infection (including purulent sputum, pulmonary infiltrate, or abnormal urine sediment). The definition requires that pneumonia be confirmed by a chest CT.
Data Collection
After obtaining consent, patients’ data were collected from their medical records, including age and gender, smoking, alcohol consumption, in addition to risk factors. Patients’ medical backgrounds were also collected including, diabetes, hypertension, chronic obstructive pulmonary disease, and fatty liver disease. Furthermore we obtained National Institutes of Health Stroke Scale (NIHSS) scores and previous evidence of intravascular therapy. The baseline laboratory examinations were derived directly from the hospital laboratory database based on the patient’s admission number, including fasting blood glucose (FBG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TC), cholesterol, and absolute values of lymphocytes within 24 hours of admission. Serum calcium levels in all patients were obtained within 24 hours of admission, and was tested for by a professional from the laboratory department of Lishui Hospital of Zhejiang University. The stroke severity was assessed by well-trained neurologists using NIHSS score, within 24 hrs of hospital admission.
Statistical Analysis
Continuous variables with normal distributions are expressed in mean±SD, while the remaining measurement data are shown as the median + interquartile range. Categorical variables are presented as frequency and percentage. Continuous variables were compared with the Student’s t-test or Mann Whitney U-test as appropriate, and the chi-square test and Fisher exact test were used for categorical variables. All reported p-values were 2-sided with p<0.05 considered significant. Logistic regression analyses were performed to estimate the Odds Ratio (OR) and the resulting 95% confidence intervals (CI) of the association between serum calcium levels and SAI risk. Variables with p < 0.05 in univariate analysis were candidates for inclusion in multivariate logistic regression analysis. We further evaluated the pattern and magnitude of associations between the serum calcium levels and the risk of SAI using an adjusted spline regression model, fitting a restricted cubic spline function with 3 knots (10th, 50th, and 90th percentiles). All analyses were conducted with R for Windows (version 4.1.0; http://www.r-project.org/).
Results
Baseline Characteristics of the Patients with and without SAP
The study ultimately included 395 patients, of whom 271 (68.6%) were men, with an average age of 68.3±12.5 years. Of these, 107 (27.1%) patients were diagnosed with in-hospital SAI. The baseline characteristics of the patients with and without SAP are presented in Table 1. There were no statistical differences between the two groups relating to their backgrounds of smoking, alcohol consumption, hypertension, diabetes, and COPD. Patients with SAI suffered from relatively severer neurological deficits [higher NIHSS score, 3 (1–5) versus 10 (3–15); p<0.001], tended to be older in age (66.6±12.5 versus 72.8±11.4; p<0.001) and were more likely to undergo intravascular therapy [19 (6.60%) versus 38 (35.5%); p<0.001]. The values of serum calcium in non-SAI and SAI patients were 2.23±0.14 and 2.14±0.14, respectively. Compared to patients without SAP, those with SAP had significantly lower serum calcium levels (p<0.0001). Meanwhile, the baseline free fatty acid, fasting blood sugar, triglyceride, and cholesterol levels were higher in patients with SAP (Table 1).
 |
Table 1 Patient Characteristics Stratified by Infections |
Association Between Serum Calcium and SAI
In our univariate analysis, the risk of SAI was negatively correlated with serum calcium levels [0.006 (95% CI =0.001–0.038), p = 0.035], as shown in Table 2. Age, history of intravascular therapy, admission NIHSS score, fasting blood sugar level, free fatty acid level and white blood cell count, were all significantly associated with the risk of SAP (all p <0.05). In our multivariable logistic regression analysis, serum calcium levels remained significant after adjusting for confounders [model 2:0.037 (95% CI = 0.004–0.270), p = 0.002; model 3: 0.040 (95% CI = 0.005–0.291), p = 0.002]. Age [1.03 (95% CI = 1.01–1.05), p = 0.01] and admission NIHSS score [1.14 (95% CI = 1.08–1.20), p <0.001] are also standalone risk factors for SAI. The risk of SAI is higher when the blood calcium concentration is less than 2.25mmol/L, within 24 hours of admission [adjusted OR 3.009 (95% CI = 1.629–5.803), p <0.001].
 |
Table 2 Multivariate Adjusted Odds Ratios for the Association Between Serum Calcium Levels and SAI |
Furthermore, multiple-adjusted cubic spline regressions confirmed the association between SAI risk and serum calcium levels (Figure 2). Within the range of serum calcium less than 2.25mmol/L, the risk of SAI increases with the decrease of serum calcium (P = 0.005 for linearity). When serum calcium is greater than 2.25mmol/L, there is no statistically significant relationship between SAI risk and serum calcium.
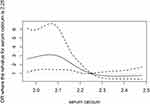 |
Figure 2 Association Between Serum Calcium Levels and Risk of SAI. The reference serum calcium levels were 2.25 mmol/L. The two dotted lines represent 95% confidence intervals. And the solid gray curve is the ORs value. ORs and 95% confidence intervals derived from restricted cubic spline regression, adjusting for the same variables as model 3 in Table 2. |
Discussion
This study involved 395 patients, of whom 27.1% developed SAI, which is consistent with previously published studies.4 We found that serum calcium was associated with SAI and was independent of the SAI risk factors for age, admission NIHSS score, and intravascular therapy [adjusted OR 0.040 (95% CI = 0.005–0.291), p = 0.002]. Remarkably, this trend is predominantly related to when the serum calcium level is less than 2.25mmol/L. This illustrates that serum calcium is a reliable and easily detectable risk factor for SAI.
Until now, there has been a lack of research that explores the relationship between serum calcium and SAI, although some animal studies suggest a possible link between serum calcium and infection.11 As a second messengers, calcium ions are involved in the realization of various physiological functions of immune cells, including proliferation, receptor-induced activation, secretion, phagocytosis, convergization, and programmed cell death.8 We speculate that on the one hand, the concentration of extracellular calcium ions may affect the key calcium signalling channels within immune cells, which in turn affects the body’s immune function. Some studies have found that serum calcium levels can affect calcium signals within cells9,10 and that changes in calcium ion levels can affect the body’s immune function.11,13 In addition, evidence from a cohort study suggests that adequate serum calcium levels are associated with low levels of chronic inflammation.14 Calcium ions involved in the immune defences against bacterial infections can be complex. The internal flow of calcium ions is considered to be an important part of the pathophysiology of sepsis.15 Meanwhile, the use of calcium channel blockers can reduce the probability of severe sepsis [adjusted OR 0.466 (95% CI = 0.412–0.798), p < 0.001].16 Notably, due to the distribution of serum calcium levels in this group of patients, we cannot confirm the relationship between serum calcium and SAI risk when it exceeds the normal range.
On the other hand, deficiency of vitamin D (<25nmol/L), an important hormone that regulates calcium homeostasis, has been shown to be an independent risk factor for SAP [adjusted OR 2.997 (95% CI = 1.185–7.584), p = 0.020].17 Similar to the study on vitamin D levels and the relationship between SAP, our study identified an increased risk of SAI when the serum calcium concentration was less than 2.25mmol/L [adjusted OR 3.009 (95% CI = 1.629–5.803), p <0.001]. Low serum calcium levels may be associated with low vitamin D levels in stroke patients at high risk of SAI. Vitamin D and serum calcium have complex interactions in the regulation of immunity. One in vitro study found that 1,25-(OH)2D produced striking up-regulation of genes involved in immune responses, inflammation, extracellular matrix, and cell adhesion, which was almost eliminated by the addition of calcium ions.18
In addition, another hypothesis is that serum calcium may reflect post-stroke stress and immunosuppression. Stroke-induced immunodepression syndrome (SIIS) is characterised by post-stroke monocyte dysfunction and lymphopenia, and its main mechanisms include impaired immune system function due to dysfunction of the autonomic nervous system in acute post-stroke stress.19 Activation of the hypothalamic-pituitary-adrenal cortex axis (HPA) leads to the production of large amounts of glucocorticoids, further inducing lymphopenia and altering the level of inflammatory/anti-inflammatory mediators. It is worth noting that the increase of glucocorticoids, in addition to affecting the function of the immune system, can also antagonize parathyroid hormones, resulting in an imbalance in calcium regulation, resulting in a decrease in blood calcium levels.
In this study, the average serum calcium levels of the included participants were lower than normal (overall 2.20±0.14mmol/L, infected 2.14±0.14mmol/L, non-infected 2.23±0.14mmol/L). Some studies have found that the incidence of hypocalcemia is higher in hospitalized patients.20 Therefore, hypocalcemia may be one of the common manifestations in hospitalized cerebral infarction patients. In addition, low calcium intake is one of the risk factors for stroke in specific populations.21 This may be another reason why stroke patients in our study showed lower serum calcium levels.
Many new blood indicators have been shown to predict the risk of SAI or SAP. Recently, for the first time, Xabier Urra et al22 confirmed through clinical studies, that high levels of cortisol are an independent risk factor for SAI. Zonneveld et al23 found that a blood glucose >7.8 mmol/L upon admission was an independent risk factor for post-stroke infection (aOR 2.31, 95% CI 1.31–4.07); however, for patients with confirmed diabetes, a high blood glucose level could not predict post-stroke infection (aOR 0.49, 95% CI 0.15–1.58). In our study we also discovered patients who eventually developed SAI had higher blood glucose levels during admission compared with the SAI-free group (mean 5.93 mmol/L vs 6.84 mmol/L, p = 0.03).
In addition, CPus, PCTus24 and neutrophil-to-lymphocyte ratio (NLR),25 have all been proven to be independent predictors of SAP. Moreover, serum amyloid A is considered a new independent predictor of SAI.26 Compared with some SAI prediction markers, serum calcium detection is more popular in primary hospitals, and can be better applied in hospitals with relatively backward testing equipment. In the future, more research is needed to integrate these indicators of post-stroke infection, to assess whether SAI and SAP forecasts can be further improved. We believe this study highlights how calcium levels may be one of the possible candidates for this improved predictive capacity. On the other hand, the correlation between serum calcium and SAI has been demonstrated, which may provide new ideas for studying the mechanism of SAI occurrence.
Our study has several limitations. First, due to the lack of data, we were forced to neglect the symptom of dysphagia, which has been proven to be an independent risk factor for SAP. Second, because our study analysis is retrospective and single-centered in nature, it’s unclear if low serum calcium concentration is an early manifestation of infection or if low calcium leads to an increased risk of infection. Thus, additional large-scale, prospective clinical cohorts are needed to confirm our findings. Finally, the infection rates after hospitalization were also not accounted for, which means some potentially infected people may be included in non-infected groups. However, this is more likely to lead to a bias toward the null hypothesis and thus underestimate the correlation between serum calcium and SAI.
Conclusion
In summary, our study is the first to report that reduced serum calcium levels are associated with the occurrence of SAI in inpatient stroke patients. In the future, if our findings are validated in a larger prospective cohort, serum calcium levels may help select patients who are susceptible to infection.
Abbreviations
COPD, chronic obstructive pulmonary disease; CHO, cholesterin; IQR, interquartile range; mRS, modified Rankin Scale; SAI, stroke-associated infection; SAP, stroke-associated pneumonia; FPG, Fasting blood sugar; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; FFA, free fatty acid; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio; TC, triglyceride; WBC, white blood cell; UTI, urinary tract infection.
Data Sharing Statement
The data and R codes that was used to generate the results can be made available upon request from the corresponding author.
Ethics Approval and Informed Consent
This study complies with the Declaration of Helsinki and was approved by the LiShui Central Hospital Ethics Committee (No. 172 of 2020). All participants provided written informed consent forms when they registered for the current study. The data that support the findings of this study are available from the corresponding author on reasonable request.
Consent for Publication
We hereby transfer, assign, or otherwise convey all copyright ownership, including any and all rights incidental thereto, exclusively to the journal, in the event that such work is published by the journal.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants from the Zhejiang Medical and Health Science and Technology Program in 2021 (No.2,021,452,054), Training for Innovation Talent Support Program in the Health Commission of Zhejiang Province, China. The funding organization had no role in the study or in the preparation of this report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi:10.1016/S0140-6736(19)30427-1
2. Chao BH, Yan F, Hua Y, et al. Stroke prevention and control system in China: CSPPC-Stroke Program. Int J Stroke. 2021;16(3):265–272. doi:10.1177/1747493020913557
3. Tu WJ, Chao BH, Ma L, et al. Case-fatality, disability and recurrence rates after first-ever stroke: a study from bigdata observatory platform for stroke of China. Brain Res Bull. 2021;175:130–135. doi:10.1016/j.brainresbull.2021.07.020
4. Westendorp WF, Nederkoorn PJ, Vermeij JD, Dijkgraaf MG. Post-stroke infection: a systematic review and meta-analysis. BMC Neurol. 2011;11(1):110. doi:10.1186/1471-2377-11-110
5. Liu DD, Chu SF, Chen C, Yang PF, Chen NH, He X. Research progress in stroke-induced immunodepression syndrome (SIDS) and stroke-associated pneumonia (SAP). Neurochem Int. 2018;114:42–54. doi:10.1016/j.neuint.2018.01.002
6. Hoffmann S, Harms H, Ulm L, et al. Stroke-induced immunodepression and dysphagia independently predict stroke-associated pneumonia – the PREDICT study. J Cereb Blood Flow Metab. 2017;37(12):3671–3682. doi:10.1177/0271678X16671964
7. Wästfelt M, Cao Y, Ström JO. Predictors of post-stroke fever and infections: a systematic review and meta-analysis. BMC Neurol. 2018;18(1):49. doi:10.1186/s12883-018-1046-z
8. Massullo P, Sumoza-Toledo A, Bhagat H, Partida-Sánchez S. TRPM channels, calcium and redox sensors during innate immune responses. Semin Cell Dev Biol. 2006;17(6):654–666. doi:10.1016/j.semcdb.2006.11.006
9. Breitwieser GE, Gama L. Calcium-sensing receptor activation induces intracellular calcium oscillations. Am J Physiol Cell Physiol. 2001;280(6):C1412–C1421. doi:10.1152/ajpcell.2001.280.6.C1412
10. Mailhot GV, Petit JL, Demers C, Gascon-Barre M. Influence of the in Vivo Calcium Status on Cellular Calcium Homeostasis and the Level of the Calcium- Binding Protein Calreticulin in Rat Hepatocytes. Endocrinology. 2000;141(3):891-900. doi:10.1210/endo.141.3.7398
11. Kimura K, Reinhardt TA, Goff JP. Parturition and Hypocalcemia Blunts Calcium Signals in Immune Cells of Dairy Cattle. J Dairy Sci. 2006;89(7):2588–2595. doi:10.3168/jds.S0022-0302(06)72335-9
12. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi:10.1016/j.ajic.2008.03.002
13. Zhuang Z, Wang X, Huang M, Luo Y, Yu H. Serum calcium improved systemic inflammation marker for predicting survival outcome in rectal cancer. J Gastrointest Oncol. 2021;12(2):568–579. doi:10.21037/jgo-20-479
14. Shridhar K, Kinra S, Gupta R, et al. Serum Calcium Concentrations, Chronic Inflammation and Glucose Metabolism: a Cross-Sectional Analysis in the Andhra Pradesh Children and Parents Study (APCaPS). Curre Dev Nutrition. 2019;3:3. doi:10.1093/cdn/nzy085
15. Song SK, Karl IE, Ackerman JJ, Hotchkiss RS. Increased intracellular Ca2+: a critical link in the pathophysiology of sepsis? Proce National Acad Sci. 1993;90(9):3933–3937. doi:10.1073/pnas.90.9.3933
16. Zheng L, Hunter K, Gaughan J, Poddar S. Preadmission Use of Calcium Channel Blockers and Outcomes After Hospitalization With Pneumonia: a Retrospective Propensity-Matched Cohort Study. Am J Ther. 2017;24(1):e30–e38. doi:10.1097/MJT.0000000000000312
17. Huang GQ, Cheng HR, Wu YM, et al. Reduced Vitamin D Levels are Associated with Stroke-Associated Pneumonia in Patients with Acute Ischemic Stroke. CIA. 2019;14:2305–2314. doi:10.2147/CIA.S230255
18. Protiva P, Pendyala S, Nelson C, Augenlicht LH, Lipkin M, Holt PR. Calcium and 1,25-dihydroxyvitamin D 3 modulate genes of immune and inflammatory pathways in the human colon: a human crossover trial. Am J Clin Nutr. 2016;103(5):1224–1231. doi:10.3945/ajcn.114.105304
19. Urra X, Laredo C, Zhao Y, et al. Neuroanatomical correlates of stroke-associated infection and stroke-induced immunodepression. Brain Behav Immun. 2017;60:142–150. doi:10.1016/j.bbi.2016.10.004
20. Zivin JR, Gooley T, Zager RA, Ryan MJ. Hypocalcemia: a pervasive metabolic abnormality in the critically ill. Am J Kidney Dis. 2001;37(4):689–698. doi:10.1016/S0272-6386(01)80116-5
21. Iso H, Stampfer MJ, Manson JE, et al. Prospective Study of Calcium, Potassium, and Magnesium Intake and Risk of Stroke in Women. Stroke. 1999;30(9):1772–1779. doi:10.1161/01.STR.30.9.1772
22. Urra X, Cervera Á, Obach V, Climent N, Planas AM, Chamorro Á. Monocytes Are Major Players in the Prognosis and Risk of Infection After Acute Stroke. Stroke. 2009;40(4):1262–1268. doi:10.1161/STROKEAHA.108.532085
23. Zonneveld TP, Nederkoorn PJ, Westendorp WF, et al. Hyperglycemia predicts poststroke infections in acute ischemic stroke. Neurology. 2017;88(15):1415–1421. doi:10.1212/WNL.0000000000003811
24. Hotter B, Hoffmann S, Ulm L, et al. Inflammatory and stress markers predicting pneumonia, outcome, and etiology in patients with stroke. 2020;7(3). doi:10.1212/NXI.0000000000000692
25. Nam KW, Kim TJ, Lee JS, et al. High Neutrophil-to-Lymphocyte Ratio Predicts Stroke-Associated Pneumonia. Stroke. 2018;49(8):1886–1892. doi:10.1161/STROKEAHA.118.021228
26. Schweizer J, Bustamante A, Lapierre-Fétaud V, et al. SAA (Serum Amyloid A): a Novel Predictor of Stroke-Associated Infections. Stroke. 2020;51(12):3523–3530. doi:10.1161/STROKEAHA.120.030064
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
