Back to Journals » Cancer Management and Research » Volume 16
Serum Biochemical Markers for Medullary Thyroid Carcinoma: An Update
Received 15 September 2023
Accepted for publication 21 March 2024
Published 8 April 2024 Volume 2024:16 Pages 299—310
DOI https://doi.org/10.2147/CMAR.S440477
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Shuzhou Liu,1,* Hao Zhao,2,* Xiaoyi Li2
1Department of Head & Neck Surgery, Hainan General Hospital, Haikou, 570311, People’s Republic of China; 2Department of General Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, 100010, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoyi Li, Department of General Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, No. 1 Shuai Fu Yuan, Dongcheng District, Beijing, 100730, People’s Republic of China, Email [email protected]
Introduction: Medullary thyroid carcinoma (MTC), a rare malignancy, requires early diagnosis for optimal patient outcomes. An important aspect of MTC diagnosis is the assessment of serum biomarkers. This review aimed to evaluate the use of serum biomarkers in the diagnosis, prognosis, and follow-up of MTC.
Methods: A thorough search of PubMed covering 1975 to 2022 was conducted to identify English-language articles on MTC serum biomarkers.
Results: The review revealed that calcitonin (Ctn) and carcinoembryonic antigen (CEA) remain the most important serum biomarkers for MTC diagnosis and management. Despite limited studies on procalcitonin (PCT), its stability and ability to exclude interference from inflammation make it a valuable potential marker of MTC. Although the positive rate of serum CA19-9 levels in MTC patients was not high, it can be used as an indicator of poor prognosis in advanced MTC. Other serum markers, including chromogranin A, gastrin-releasing peptide precursor, and neurospecific enolase, did not show any unique value in MTC diagnosis and management.
Conclusion: Taken together, this review emphasized the importance of serum biomarkers, particularly Ctn and CEA, in the diagnosis and management of MTC. PCT shows promise as a valuable potential marker, whereas CA19-9 can be used as a prognostic indicator of advanced MTC. Further research is needed to validate the significance of these serum biomarkers in MTC and determine the effects of confounding factors on their levels. Clinicians should consider using these markers in MTC diagnosis, prognosis, and follow-up, particularly for patients with advanced disease.
Keywords: medullary thyroid carcinoma, serum biochemical markers, calcitonin, carcinoembryonic antigen, procalcitonin
Introduction
Medullary thyroid carcinoma (MTC) is a neuroendocrine neoplasm that originates from the parafollicular cells (C cells) of the thyroid gland and accounts for approximately 2% of all thyroid cancers.1,2 Approximately 75% of MTCs are sporadic, with the remaining 25% inherited. C cells originate from the neuroectoderm and belong to the family of amine precursor uptake and decarboxylation cells, which secrete endocrinologically active substances, including calcitonin (Ctn), calcitonin gene-related peptide (CGRP), neuro-specific enolase (NSE), adrenocorticotropic hormone, gastrin-related peptide (GRP), chromogranin A (CgA), and 5-hydroxytryptamine.3 Furthermore, neoplastic C cells produce carcinoembryonic antigen (CEA) and carbohydrate antigen 19–9 (CA19-9).1 Among these, Ctn is a highly specific and sensitive biomarker of MTC. CEA is less specific but more convenient and less expensive. Both of these biomarkers play an important role in the diagnosis, evaluation, and follow-up of MTC. In this review article, a comprehensive summary of the diagnostic and prognostic value of the common and some newly emerged serum biomarkers of MTC has been presented.
Search Strategy
A search of PubMed using the following terms was conducted: “medullary thyroid carcinoma”[tiab] AND “calcitonin”[All fields] AND ((“1975/01/01” [PDAT]: “2022/12/31” [PDAT]) AND English [lang]). The keyword calcitonin was then replaced by other markers (carcinoembryonic antigen/procalcitonin/carbohydrate antigen 19–9/gastrin-related peptide/neuro-specific enolase/chromogranin A) separately and searched with the same search strategy. From the 2350 records returned, the most relevant articles were selected, giving priority to more recent publications. The reference lists of key papers were scanned for additional relevant articles.
CTN
Ctn, a peptide hormone secreted by C cells, whose normal upper limit is assay-dependent, has varying normal upper limits across sex and age, with females having slightly lower levels than males and children having higher levels than adults.4 The detection of serum Ctn primarily relies on various immunoassays, the most widely used of which in clinical practice are immunochemiluminometric assays. Serum Ctn stability can be affected by environmental factors, causing inaccurate outcomes. Serum Ctn levels decrease by 7%–18%, 20%–35%, and 28%–65% when stored at room temperature for >2, >6, and >12 h, respectively, and by 6%–8% and 21%–23% at 6 and 12 hours when stored at 4–8°C.5
Diagnosis
Fine-needle aspiration (FNA) is routinely utilized to differentiate benign and malignant for nodules that are suspected to be MTC. However, its sensitivity for MTC diagnosis is only approximately 50%.6 On the other hand, routine serum Ctn screening has been revealed that can detect MTC at an early stage with higher sensitivity (83.3%–100%) and specificity (95.3%–100%), outperforming FNA.6–11 Nevertheless, the Ctn-positive rate in thyroid nodule screenings is extremely low (0.3%–5.9%), with only 0.1%–1.1% of Ctn-positive patients eventually diagnosed with MTC.6–11
The cutoff value of basal Ctn (bCtn) is a key factor affecting the diagnostic efficiency. With a cutoff at 10 pg/mL, sensitivity was almost 100%, rarely missed MTC patients. However, the reported positive predictive value (PPV) varied widely among studies (Table 1).6–11 For bCtn >100 pg/mL, nearly all studies indicated a PPV close to 100%, which confirmed the diagnosis with almost no exception.8,10,11 When bCtn was in the range of 10–100 pg/mL, PPV varied in a large range (0%–68.8%, Table 1),8–11 making the diagnosis difficult. Ctn provocation test, despite enhancing stimulated Ctn levels in MTC patients and C-cell hyperplasia, failed to significantly improve PPVs for those with bCtn between 10 and 100 pg/mL.8,12
 |
Table 1 The Diagnostic Efficiency of the Common Biomarkers in MTC |
In 2007, Boi et al19 reported a 100% sensitivity and specificity for MTC diagnosis based on Ctn levels in FNA wash-out fluid (Ctn-FNA). Many subsequent studies, although with small patient samples, replicated high sensitivity (90%–100%) and specificity (86.7%–100%) of Ctn-FNA.13–18 Its accuracy for lymph node metastasis (LNM) was even higher, with 100% sensitivity and specificity.19–21 The diagnostic cutoff value remains an important factor affecting the results (Table 1). However, Ctn-FNA levels could be influenced by bCtn levels.30 Accordingly, false-positive Ctn-FNA results were likely to occur in cases of C-cell hyperplasia with mildly elevated bCtn levels.14,15 Thus, combining cytology and Ctn immunohistochemistry could further improve diagnostic accuracy in such situations to achieve 100% sensitivity and specificity.31,32 Of note, nonsecretory MTCs, a rare subset of MTC patients with normal basal Ctn levels, accounting for approximately 0.83%–5.5% of all MTC cases, presenting a diagnostic challenge preoperatively, with definitive diagnosis primarily relying on postoperative pathology.11,33
Tumor Burden
Preoperative serum Ctn levels can reflect the tumor burden and correlate with MTC disease extent, which are positively correlated with tumor size.34 The tumor diameter is usually <1 cm with Ctn <100 pg/mL and often >2 cm when the Ctn level is >1000 pg/mL.34–38 While few studies have explored the correlation between Ctn levels and LNM extent, and no definitive Ctn level has been identified for accurately indicating LNM or metastasis extent, all reports suggest a positive association between bCtn levels and LNM.
In a cohort of 300 MTC patients, Machens et al36 reported no central or lateral LNM when the Ctn level was <20 pg/mL. However, when the Ctn level was >200 pg/mL, more than one-third of patients presented with central and ipsilateral lateral LNM, and the contralateral lateral LNM rate was >10% when Ctn >500 pg/mL. Similar findings were obtained by Park et al.38 Furthermore, a recent multicenter study proposes an ipsilateral lateral neck dissection for patients with bCtn >240 pg/mL and a contralateral lateral neck dissection for those with bCtn >600 pg/mL.39 As MTC patients with bCtn <100 pg/mL rarely have LNM in the ipsilateral lateral compartments,36,38 lateral neck dissection should be carefully evaluated in these patients. To date, however, the practice of determining the extent of surgery based on the preoperative bCtn level has not been widely endorsed.40–42 Nevertheless, preoperative bCtn levels have shown good predictive value for distant metastases (Table 2). Most study observed no distant metastasis in patients with Ctn levels <500 pg/mL.35,36,38 It is clear that the bCtn level is closely correlated with the tumor burden. It was revealed that biochemical cure after surgery was nearly unattainable for MTC patients with preoperative Ctn was >1000 pg/mL, while 97.8% of patients with Ctn <50 pg/mL achieved it.34,43 Of note, in hereditary MTC (hMTC), Ctn level is crucial for predicting tumor progression, reflecting tumor burden, and determining surgical timing. As all hMTC patients may eventually require surgical intervention, optimal timing is essential for satisfactory outcomes and minimizing complications. In MTC family members with moderate (MOD) and high (H) risk of germline RET mutations, 39%–61% and 77%–100% of patients with normal and elevated Ctn levels, respectively, were pathologically diagnosed with MTC after prophylactic thyroidectomy.44–47 When the Ctn level was <30 pg/mL, the tumors were usually enclosed in the thyroid gland without LNM or distant metastasis, whereas more than one-third of patients with Ctn levels >30 pg/mL were predicted to develop LNM.44,45 A recent study indicated that the prognosis for both MOD and H groups is primarily driven by tumor burden, not genetic risk outcomes.48 All patients with hMTC may be biochemically cured postoperatively when preoperative Ctn does not exceed 30 pg/mL.45,49,50 For members of the hMTC family with germline RET mutations at the highest class risk, the key factor in determining surgical treatment is the genetic risk class and age at diagnosis. Research has shown that 83% of the such patients who underwent prophylactic surgery under 1 year of age were pathologically diagnosed with MTC and had a significantly higher rate of biochemical cure than those who received surgery after the age of 1 year (83% vs 15%, p < 0.0001).51
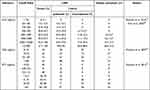 |
Table 2 The Ability of Reflecting Tumor Burden of Common Biomarkers in MTC |
Follow-Up
According to the postoperative Ctn level and imaging studies, Tuttle et al54 defined the dynamic risk stratification of MTC. Studies indicate that 27%–70% of MTC patients with ER (Excellent response) exhibit a favorable prognosis with a 10-year disease-specific survival (DSS) of up to 95%–100% and a low recurrence rate of 1%–4%. Moreover, 23%–35% of MTC patients with BIR (biochemical incomplete response) showed a decreased 10-year DSS of 90%–95% and an elevated recurrence rate of 14%–37%. The prognosis was even worse for MTC patients with SIR (structural incomplete response), accounting for 7%–38% of all cases, with a mortality rate of 20%–79% within an average follow-up period of 6.2 to 12.8 years.55–59 This indicates that the initial postoperative Ctn level can reflect the prognosis of the disease when no structural lesions are present.
The prognosis of patients with different Ctn levels may vary even if their postoperative Ctn is below the upper limit of the reference range. Theoretically, when the thyroid and MTC lesions are completely removed, the Ctn level should be reduced to an undetectable level (below the lower detection limit).60 In a recent study involving 334 MTC patients over an 8.5-year median follow-up, the biochemical cure rate was significantly higher in the Ctn undetectable group than in the detectable control group (90.1% vs 9.2%, p < 0.001), with no incidence of structural recurrence or death in the undetectable group.61 In addition, Fanget et al62 drew a similar conclusion in 127 MTC patients (recurrence rate: 3% vs 25%, p = 0.001) after a median follow-up period of 47 months. Likewise, different Ctn levels may indicate different outcomes in patients with BIR. In a study enrolling 120 MTC patients, Ctn level ≥29 pg/mL could predict structural recurrence with 100% sensitivity, 90.5% specificity, 59.1% PPV, and 100% negative predictive value (NPV) at the assessment of response to initial therapy.56 Saltiki et al,63 however, suggested a Ctn level of >14.5 pg/mL as a cutoff value for predicting structural recurrence. In patients with SIR, there is no consensus on whether Ctn levels can be used as a precise indicator of local and distant metastases. Pellegriti et al64 and Cho et al56 both observed postoperative MTC patients that higher Ctn levels (>150 pg/mL) were often associated with distant metastases at the time of relapse, suggesting that this threshold could serve as an indicator of postoperative distant metastasis.1,65 Further exploration of the value of different postoperative Ctn levels to predict prognosis is needed.
The Ctn doubling time (Ctn-dt), which is adversely linked to the proliferation grade of MTC, is an additional critical prognostic marker for patients with postoperative Ctn abnormalities. Patients with Ctn-dt >2 years were reported to have 5- and 10-year overall survival (OS) rates of 100% (Table 3),66 while those with Ctn-dt between 0.5 and 2 years had OS rates of 92% and 37% at 5 and 10 years, respectively. When Ctn-dt was <0.5 years, the 5-year and 10-year OS rates were only 25% and 8%. Similar findings were obtained by Hassan et al67 and Miyauchi et al.68 A meta-analysis by Meijer et al69 revealed that a Ctn-dt of <1 year was an indicator of poor prognosis. However, the utility of Ctn-dt in clinical practice is limited due to its time-consuming and costly nature and its inability to predict disease progression or recurrence at an early stage. A more recent study proposed using the Ctn ratio (CR, postoperative Ctn level/preoperative Ctn level) as an early indicator for predicting structural recurrence; the ratio has a recurrence rate of 41.0% and mortality rate of 4.5% (median follow-up = 3.25 years) when CR ≥ 0.15 at 3 postoperative days.70
 |
Table 3 Predictive Capacity of Common Biomarkers for Prognosis in MTC |
Dynamic risk stratification is a good indicator of MTC prognosis, but the optimal time for postoperative Ctn detection and its accuracy in predicting prognosis at an early stage remain uncertain. The half-life of Ctn is the most important factor that affects its clearance time after complete tumor resection. The half-life of exogenous salmon Ctn is approximately 30 min in humans.73,74 Therefore, it has been hypothesized that the serum Ctn of MTC patients can drop to normal levels within a very short time after complete resection. Faggiano et al75 reported that the Ctn levels could drop to <50% of the preoperative levels 30 min after surgery in six patients who all achieved a biochemical cure. After a mean follow-up period of 14.6 months, none of these patients relapsed. Similar results were obtained in the Brauckhoff study with a median follow-up period of 21 months.76 Of note, the half-life of Ctn in MTC patients can be significantly prolonged to 30 h, which is probably due to the high preoperative tumor burden and the longer time required for “calcitonin-enriched lymphatic fluid” to enter the circulatory system and be cleared after surgery. Furthermore, extremely high preoperative Ctn (>1000 pg/mL) may prolong the time to Ctn normalization to 1–2 weeks or even 8 weeks.77 Therefore, it is recommended that the response to initial therapy should be performed at 2–3 months or 6–12 months after surgery.1,55–59 However, whether an earlier assessment can produce an earlier and more precise indication of prognosis deserves further investigation. A study showed that 41 out of 42 patients who achieved an undetectable Ctn level 1 year after surgery had also reached an undetectable Ctn level as soon as 1 month after surgery.78
CEA
CEA, initially known as an intercellular adhesion glycoprotein, is expressed by the neuroendocrine tissues of the gastrointestinal tract during fetal development. However, it was also found to be expressed in both normal and tumor tissues, including C cells.79,80 Healthy populations typically have CEA levels ranging from 2.5 to 5 ng/mL, and a higher level in men than women.81 Elevated CEA (>5 ng/mL) indicates various malignancies, including digestive tract and respiratory tumors, and can also be found in ulcerative colitis, pancreatitis, and liver cirrhosis and among heavy smokers. This suggests that CEA is not a specific tumor marker for MTC. However, previous studies reported that approximately 60%–70% of MTC patients present with elevated serum CEA levels.52,82,83 While CEA is not a specific biomarker, its convenience and low test cost make it an important and commonly used serum biomarker of MTC.
Preoperative CEA levels may also reflect the tumor burden and are positively correlated with tumor size. For CEA levels of 10, 10–100, and >100 ng/mL, the sizes of the tumors were 6.5–12.5, 9.3–29.3, and 25.3–47.7 mm, respectively.36 Moreover, varied elevated levels of basal CEA may be an indicator of LNM and distant metastasis. Machens et al52 reported that while not statistically significant, the rate of LNM and distant metastases in the CEA normal group (n = 23) was much lower than in the CEA elevated group (n = 54) (26.1% vs 61%, p = 0.09; 8.7% vs 30%, p = 0.08) [69]. In the elevated CEA group, more than two-thirds of patients had central and ipsilateral lateral LNM when CEA was >30 ng/mL. Furthermore, when CEA was >100 ng/mL, 73% of patients had contralateral lateral cervical LNM and 75% had distant metastases.52 Likewise, it was reported that LNM rate increased significantly when CEA was >30 ng/mL.84 The sensitivity and specificity of this cutoff value as a predictor of lateral LNM were 75.0% and 81.6%, respectively.85 All of these studies showed that CEA is a sensitive marker of tumor progression and invasion. A study involving 899 MTC patients suggested that preoperative CEA levels correlated with tumor stage, with 80.9% of stage I patients having normal CEA levels and 79.8%/97.5% of stage III/IV patients having elevated CEA levels.83
CEA is also useful for the assessment of response to initial therapy in MTC patients. However, the sensitivity of CEA to indicate prognosis is lower than that of Ctn, as only a subset of MTC have elevated serum CEA levels.56,64,86 Postoperative CEA levels >5 ng/mL had a 65%, sensitivity and 79% specificity for predicting recurrence, whereas postoperative CEA levels >12.66 ng/mL had up to 100% specificity to predict recurrence, but its sensitivity decreased to 57.9%.87 Certain studies have considered CEA as a marker of dedifferentiation in MTC,88,89 and CEA doubling time (CEA-dt) was found to be a better prognostic factor than Ctn-dt in MTC.66,69 Barbet et al66 reported that patients with a CEA-dt of 0.5–2 years and <0.5 years had worse OS than those with the same Ctn-dt and that the 5- and 10-year OS rates were 0% when CEA-dt was <0.5 years (Table 3). Furthermore, CEA-dt was found to be more accurate than Ctn-dt in predicting MTC disease recurrence.69 However, owing to the low sensitivity of CEA, CEA-dt values could be calculated in only approximately half of the patients. Therefore, it is usually recommended to combine CEA-dt and Ctn-dt for postoperative follow-up.1,90 Other studies revealed that 94% of patients had disease progression when Ctn/CEA-dt was <25 months, that their 5- and 10-year OS rates were 66.3% and 29.1%, and that the 5- and 10-year recurrence-free survival (RFS) rates were 34.9% and 13%, respectively, when Ctn/CEA-dt was <2 years.71,72
CEA can be produced in both normal and tumor tissues in humans, thereby making it difficult to assess the half-life of serum CEA in vivo. It was reported that in patients with colorectal cancer with elevated preoperative CEA levels who achieved clinical remission after surgery, the serum CEA level halved in 3–5 days after surgery; the same was observed in 3.2 days in patients with lung cancer.91,92 Andrade et al78 found that of 56 patients with normal CEA one year post-surgery, 63% and 97% had normal levels at one and six months postoperatively. At present, it is advised that CEA testing for response to initial therapy should be performed 2–3 months after surgery.1
Procalcitonin (PCT)
PCT is a precursor peptide of calcitonin without hormonal activity. It is synthesized and secreted by C cells or other neuroendocrine cells of the lung and intestine. Typically, all PCTs produced in C cells transform into mature Ctn and circulate, rendering PCT levels undetectable in healthy individuals (<0.1 ng/mL in adults).24,93 In 2003, Bihan et al94 detected intact PCT in the serum of all MTC patients at a mean level 7.6 times higher than the Ctn level. Moreover, after the administration of pentagastrin, PCT levels were stimulated and elevated. Since 2023, further investigations on PCT in the diagnosis and treatment of MTC have gradually developed.
It has been suggested that the diagnostic efficiency of PCT and Ctn for MTC is similar when excluding inflammatory disruptions. A study showed that using a cutoff value of PCT > 0.1 ng/mL for the diagnosis of MTC resulted in a sensitivity of 100%, specificity of 99.9%, PPV of 77.8%, and NPV of 100%23 (Table 1). A recent meta-analysis also yielded similar results.95 Remarkably, PCT can improve the diagnostic efficiency in patients with mildly elevated Ctn (10–100 pg/mL).26,29,96,97 In a study involving 60 such patients, all 9 patients with confirmed MTC showed PCT levels >0.1 ng/mL, whereas 46 of 51 non-MTC patients had PCT <0.1 ng/mL, resulting in a 100% NPV.96 Giovanella et al97 and Lim et al26 also showed that the NPV of PCT in patients with mildly elevated Ctn was up to 100% and 96.3%, respectively. Evidently, the diagnosis of MTC can be excluded when PCT is not elevated. One study showed that PPV with PCT > 0.07 ng/mL was 100% in such patients.29
Similarities between PCT and Ctn have been observed, which may indicate the tumor extent preoperatively and predict recurrence postoperatively.22,25,28,53,98 Machens et al53 discovered the association between PCT levels and the presence of LNM. When PCT was <0.25 ng/mL, LNM was rare, and at PCT >0.5 ng/mL, approximately 38% and 23% of patients developed central and ipsilateral lateral LNM, respectively (Table 2). Moreover, when the PCT level exceeded 1.0 ng/mL, 4% of patients developed contralateral lateral LNM, and when above 5.0 ng/mL, the rate of contralateral lateral LNM and distant metastasis were 36% and 18%, respectively. A postoperative study of 158 MTC patients (median follow-up period of 16 years) revealed significantly higher PCT level in the metastatic and minimal residual disease group compared to the cured group at the last follow-up (109 ± 202 vs 0.511 ± 0.800 vs <0.06 ng/mL, p < 0.001).28 Similar results were obtained in the studies of Giovanella et al98 and Trimbolie et al.22 Moreover, Walter et al25 suggested that MTC may produce less Ctn during the process of dedifferentiation and that the PCT/Ctn ratio can be used as a predictor of recurrence or distant metastasis, with a sensitivity of 72.2% and specificity of 73.5% when the PCT/Ctn ratio is >2.4. The PCT/Ctn ratio can be measured at any time postoperatively, which is more convenient for clinical application than the Ctn/CEA-dt index. Thus, the PCT/Ctn ratio may be an effective indicator of MTC prognosis and deserves further exploration and investigation.
PCTs originating from different cells are structurally different but highly analogous and indistinguishable by current assays.28 Consequently, the currently detectable serum PCT levels are susceptible to inflammation and trauma, thereby limiting their utility in the diagnosis and treatment of MTC.27 However, compared with Ctn, PCT has several advantages. It is stable at room temperature, and PCT levels are highly consistent under different assays. Moreover, there is no sex-based variation in the reference values of PCR, and no false negatives due to the “hook effect” are observed.5,24,99,100 As a result, PCT is expected to be a promising biomarker for diagnosing MTC by indicating tumor extent and prognosis. However, further research with larger samples is necessary to completely evaluate the utility of PCT in MTC.
CA19-9
The glycoantigen CA19-9 is a type of Lewis A blood group-determining cluster of mucin antigens that are glycolipids expressed from or secreted on the tumor cell surface. The level of serum CA19-9 in the normal population is <37 U/mL. However, it should be noted that CA19-9 is a nonspecific tumor marker and is usually used as an indicator of pancreatic cancer. In 2011, Milman et al101 reported that one patient with MTC with distant metastases had significantly elevated serum CA19-9 levels. In 2013, Elisei et al102 found that liver metastatic lesions also expressed CA19-9. These findings led to the hypothesis that elevated serum CA19-9 is a marker of progression and poor prognosis in advanced MTC. It was later confirmed that positive CA19-9 expression in MTC tissue was associated with distant metastasis.103,104 Furthermore, a study in 100 patients with recurrent MTC and LNM or distant metastases showed that serum CA19-9 was elevated in 16% of patients and that the distant metastasis rate and mortality were higher in the group with elevated serum CA19-9.105 Similar results were found by Lorusso et al106 and Alencar et al107 who showed a higher mortality rate in patients with elevated CA19-9 than in those without elevated CA19-9 (60% vs 19%, p < 0.0001). Moreover, the mortality rate was 100% in those with a CA19-9 doubling time of <1 year.106 Although the rate of positive serum CA19-9 in MTC patients is low, it can be used as an indicator of poor prognosis in advanced MTC.
Other Biomarkers
In MTC patients, the levels of certain neuroendocrine substances, such as GRP, CgA, and NSE, may be elevated. These substances may serve as potential markers of MTC. GRP is a 27-amino-acid peptide with gastrin-releasing effects, but it is not suitable for clinical testing, as its half-life is 2 min in plasma.108 The gastrin-releasing peptide precursor (proGRP), the precursor to GRP, however, is stable and can reflect GRP levels. In the normal population, serum proGRP levels are typically <50 pg/mL. Elevated serum proGRP, which is a common marker for small-cell lung cancer, is also detected in some benign diseases and gastrointestinal tumors. Elevated proGRP was reported in approximately 80% of MTC patients.109,110 Liang et al110 showed that the diagnostic sensitivity and specificity were 53.85% and 96.98%, respectively, with a cutoff value of serum proGRP >68.3 pg/mL in MTC. Likewise, the level of proGRP in FNA wash-out fluid (FNA-proGRP) was also a valid index with a sensitivity of 94.12% and specificity of 98.27% when FNA-proGRP was >22.77 pg/mL.110 Furthermore, few studies have examined the association of serum proGRP levels with tumor burden and prognosis in MTC. A study on 78 postoperative MTC patients revealed that proGRP levels were higher in the evidence of structural disease (ESD) group (n = 49) than in the no evidence of structural disease (NESD) group (880.0 vs 74.8 pg/mL, p < 0.05). The proGRP levels had a sensitivity of 75.9% and specificity of 97.9% for differentiating NESD from ESD using a cutoff value of 72.2 pg/mL. The sensitivity was 100%, and the specificity was 96.3% for predicting local recurrence and distant metastasis using a cutoff value of 167 pg/mL.111
CgA is a protein comprising 439 amino acids and is widely distributed in neuroendocrine cells. In the normal population, serum CgA levels are <100 ng/mL. Elevated CgA levels are detected in various neuroendocrine tumors, including MTC.112 It was reported that approximately 23%–50% of MTC patients, mostly advanced cases, had elevated serum CgA levels.113–117 Therefore, serum CgA is not a suitable diagnostic marker and has been shown to have limited usefulness as a prognostic indicator of MTC.87,116,117 Wolinski et al87 found that CgA had a sensitivity of 55% and specificity of 83.8% for predicting MTC recurrence postoperatively.
In addition to CgA, NSE is a commonly used neuroendocrine tumor marker. The upper limit of normal of serum NSE is 12.5 ng/mL.118 However, few studies are available on NSE in MTC. Several studies have reported that serum NSE was elevated in approximately 21%–42% of MTC patients.114,118 It was also shown that when serum NSE was >13.95 ng/mL, the sensitivity of predicting lateral LNM was 55.6%, and the specificity was 94.7% in MTC patients.85
Conclusions
In clinical practice, Ctn and CEA remain the most important serum biomarkers of MTC. While few studies have been conducted on PCT, it has shown great value when excluding the interference of inflammation. No other markers have shown a more comprehensive role and unique value in the diagnosis and treatment of MTC.
Acknowledgments
The authors would like to thank MogoEdit for its English editing during the preparation of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by National High-Level Hospital Clinical Research Funding (No. 2022-PUMCH-B-003).
Disclosure
All authors have declared no conflicts of interest in this work.
References
1. Wells SA, Asa SL, Dralle H, et al. Revised American Thyroid Association Guidelines for the Management of Medullary Thyroid Carcinoma. Thyroid. 2015;25(6):567–610. doi:10.1089/thy.2014.0335
2. Pereira M, Williams VL, Hallanger Johnson J, Valderrabano P. Thyroid Cancer Incidence Trends in the United States: association with Changes in Professional Guideline Recommendations. Thyroid off J Am Thyroid Assoc. 2020;30(8):1132–1140. doi:10.1089/thy.2019.0415
3. Oberg K, Modlin IM, De Herder W, et al. Consensus on biomarkers for neuroendocrine tumour disease. Lancet Oncol. 2015;16(9):e435–e446. doi:10.1016/S1470-2045(15)00186-2
4. Basuyau JP, Mallet E, Leroy M, Brunelle P. Reference intervals for serum calcitonin in men, women, and children. Clin Chem. 2004;50(10):1828–1830. doi:10.1373/clinchem.2003.026963
5. Kratzsch J, Petzold A, Raue F, et al. Basal and stimulated calcitonin and procalcitonin by various assays in patients with and without medullary thyroid cancer. Clin Chem. 2011;57(3):467–474. doi:10.1373/clinchem.2010.151688
6. Elisei R, Bottici V, Luchetti F, et al. Impact of routine measurement of serum calcitonin on the diagnosis and outcome of medullary thyroid cancer: experience in 10,864 patients with nodular thyroid disorders. J Clin Endocrinol Metab. 2004;89(1):163–168. doi:10.1210/jc.2003-030550
7. Vierhapper H, Niederle B, Bieglmayer C, Kaserer K, Baumgartner-Parzer S. Early diagnosis and curative therapy of medullary thyroid carcinoma by routine measurement of serum calcitonin in patients with thyroid disorders. Thyroid off J Am Thyroid Assoc. 2005;15(11):1267–1272. doi:10.1089/thy.2005.15.1267
8. Costante G, Meringolo D, Durante C, et al. Predictive value of serum calcitonin levels for preoperative diagnosis of medullary thyroid carcinoma in a cohort of 5817 consecutive patients with thyroid nodules. J Clin Endocrinol Metab. 2007;92(2):450–455. doi:10.1210/jc.2006-1590
9. Rink T, Truong PN, Schroth HJ, Diener J, Zimny M, Grünwald F. Calculation and validation of a plasma calcitonin limit for early detection of medullary thyroid carcinoma in nodular thyroid disease. Thyroid off J Am Thyroid Assoc. 2009;19(4):327–332. doi:10.1089/thy.2008.0102
10. Schneider C, Kobe C, Schmidt M, et al. Calcitonin screening in patients with thyroid nodules. Diagnostic value. Nukl Nucl Med. 2012;51(6):228–233. doi:10.3413/Nukmed-0494-12-04
11. Weber T, Poplawski A, Vorländer C, et al. Preoperative calcitonin testing improves the diagnosis of medullary thyroid carcinoma in female and male patients. Eur J Endocrinol. 2022;186(2):223–231. doi:10.1530/EJE-21-1015
12. Niederle MB, Scheuba C, Riss P, Selberherr A, Koperek O, Niederle B. Early Diagnosis of Medullary Thyroid Cancer: are Calcitonin Stimulation Tests Still Indicated in the Era of Highly Sensitive Calcitonin Immunoassays? Thyroid off J Am Thyroid Assoc. 2020;30(7):974–984. doi:10.1089/thy.2019.0785
13. Kudo T, Miyauchi A, Ito Y, Takamura Y, Amino N, Hirokawa M. Diagnosis of medullary thyroid carcinoma by calcitonin measurement in fine-needle aspiration biopsy specimens. Thyroid off J Am Thyroid Assoc. 2007;17(7):635–638. doi:10.1089/thy.2006.0338
14. Massaro F, Dolcino M, Degrandi R, et al. Calcitonin assay in wash-out fluid after fine-needle aspiration biopsy in patients with a thyroid nodule and border-line value of the hormone. J Endocrinol Invest. 2009;32(4):308–312. doi:10.1007/BF03345717
15. Diazzi C, Madeo B, Taliani E, et al. The diagnostic value of calcitonin measurement in wash-out fluid from fine-needle aspiration of thyroid nodules in the diagnosis of medullary thyroid cancer. Endocr Pract off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2013;19(5):769–779. doi:10.4158/EP12420.OR
16. Trimboli P, Cremonini N, Ceriani L, et al. Calcitonin measurement in aspiration needle washout fluids has higher sensitivity than cytology in detecting medullary thyroid cancer: a retrospective multicentre study. Clin Endocrinol. 2014;80(1):135–140. doi:10.1111/cen.12234
17. Kihara M, Hirokawa M, Kudo T, et al. Calcitonin measurement in fine-needle aspirate washout fluid by electrochemiluminescence immunoassay for thyroid tumors. Thyroid Res. 2018;11:15. doi:10.1186/s13044-018-0059-4
18. Liu Z, Zhou W, Han R, et al. Cytology versus calcitonin assay in fine-needle aspiration biopsy wash-out fluid (FNAB-CT) in diagnosis of medullary thyroid microcarcinoma. Endocrine. 2021;74(2):340–348. doi:10.1007/s12020-021-02759-1
19. Boi F, Maurelli I, Pinna G, et al. Calcitonin measurement in wash-out fluid from fine needle aspiration of neck masses in patients with primary and metastatic medullary thyroid carcinoma. J Clin Endocrinol Metab. 2007;92(6):2115–2118. doi:10.1210/jc.2007-0326
20. Abraham D, Gault PM, Hunt J, Bentz J. Calcitonin estimation in neck lymph node fine-needle aspirate fluid prevents misinterpretation of cytology in patients with metastatic medullary thyroid cancer. Thyroid off J Am Thyroid Assoc. 2009;19(9):1015–1016. doi:10.1089/thy.2009.0011
21. Marques B, Cunha N, Martins RG, et al. Lymph Node Metastases of Medullary Thyroid Cancer: role of Calcitonin in the Washout Fluid of Fine-Needle Aspiration. Int J Endocrinol. 2020;2020:9267972. doi:10.1155/2020/9267972
22. Trimboli P, Lauretta R, Barnabei A, et al. Procalcitonin as a postoperative marker in the follow-up of patients affected by medullary thyroid carcinoma. Int J Biol Markers. 2018;33(2):156–160. doi:10.1177/1724600817747518
23. Giovanella L, Imperiali M, Piccardo A, et al. Procalcitonin measurement to screen medullary thyroid carcinoma: a prospective evaluation in a series of 2705 patients with thyroid nodules. Eur J Clin Invest. 2018;48(6):e12934. doi:10.1111/eci.12934
24. Algeciras-Schimnich A, Preissner CM, Theobald JP, Finseth MS, Grebe SKG. Procalcitonin: a marker for the diagnosis and follow-up of patients with medullary thyroid carcinoma. J Clin Endocrinol Metab. 2009;94(3):861–868. doi:10.1210/jc.2008-1862
25. Walter MA, Meier C, Radimerski T, et al. Procalcitonin levels predict clinical course and progression-free survival in patients with medullary thyroid cancer. Cancer. 2010;116(1):31–40. doi:10.1002/cncr.24738
26. Lim SK, Guéchot J, Vaubourdolle M. Negative predictive value of procalcitonin in medullary thyroid carcinoma. Ann Biol Clin. 2016;74(2):213–218. doi:10.1684/abc.2015.1115
27. Kaczka K, Mikosiński S, Fendler W, Celnik A, Pomorski L. Calcitonin and procalcitonin in patients with medullary thyroid cancer or bacterial infection. Adv Clin Exp Med off Organ Wroclaw Med Univ. 2012;21(2):169–178.
28. Kratzsch J, Willenberg A, Frank-Raue K, Kempin U, Rocktäschel J, Raue F. Procalcitonin measured by three different assays is an excellent tumor marker for the follow-up of patients with medullary thyroid carcinoma. Clin Chem Lab Med. 2021;59(11):1861–1868. doi:10.1515/cclm-2021-0428
29. Censi S, Di Stefano M, Repaci A, et al. Basal and Calcium-Stimulated Procalcitonin for the Diagnosis of Medullary Thyroid Cancers: lights and Shadows. Front Endocrinol. 2021;12:754565. doi:10.3389/fendo.2021.754565
30. Giovanella L, Ceriani L, Bongiovanni M. Calcitonin measurement on fine needle washouts: preanalytical issues and normal reference values. Diagn Cytopathol. 2013;41(3):226–229. doi:10.1002/dc.22804
31. Ahmed M, Abi-Raad R, Fu L, Holt EH, Adeniran AJ, Cai G. Performing Calcitonin Immunocytochemistry on an Additional ThinPrep Slide in Fine-Needle Aspiration Diagnosis of Medullary Thyroid Carcinoma. Am J Clin Pathol. 2022;157(3):426–433. doi:10.1093/ajcp/aqab141
32. Rossi ED, Raffaelli M, Mulè A, et al. Relevance of immunocytochemistry on thin-layer cytology in thyroid lesions suspicious for medullary carcinoma: a case-control study. Appl Immunohistochem Mol Morphol AIMM. 2008;16(6):548–553. doi:10.1097/PAI.0b013e3181690ca3
33. Frank-Raue K, Machens A, Leidig-Bruckner G, et al. Prevalence and clinical spectrum of nonsecretory medullary thyroid carcinoma in a series of 839 patients with sporadic medullary thyroid carcinoma. Thyroid off J Am Thyroid Assoc. 2013;23(3):294–300. doi:10.1089/thy.2012.0236
34. Cohen R, Campos JM, Salaün C, et al. Preoperative calcitonin levels are predictive of tumor size and postoperative calcitonin normalization in medullary thyroid carcinoma. Groupe d’Etudes des Tumeurs a Calcitonine (GETC). J Clin Endocrinol Metab. 2000;85(2):919–922. doi:10.1210/jcem.85.2.6556
35. Filimon S, Payne RJ, Black MJ, et al. Calcitonin secretory index and unsuspected nodal disease in medullary thyroid carcinoma. Endocr Pract off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2018;24(5):460–467. doi:10.4158/EP-2017-0236
36. Machens A, Dralle H. Biomarker-based risk stratification for previously untreated medullary thyroid cancer. J Clin Endocrinol Metab. 2010;95(6):2655–2663. doi:10.1210/jc.2009-2368
37. Opsahl EM, Akslen LA, Schlichting E, et al. The Role of Calcitonin in Predicting the Extent of Surgery in Medullary Thyroid Carcinoma: a Nationwide Population-Based Study in Norway. Eur Thyroid J. 2019;8(3):159–166. doi:10.1159/000499018
38. Park H, Park J, Choi MS, et al. Preoperative Serum Calcitonin and Its Correlation with Extent of Lymph Node Metastasis in Medullary Thyroid Carcinoma. Cancers. 2020;12(10):E2894. doi:10.3390/cancers12102894
39. Juez LD, Mercader E, Amunategui I, et al. Extension of Prophylactic Surgery in Medullary Thyroid Carcinoma. Differences Between Sporadic and Hereditary Tumours According to Calcitonin Levels and Lymph Node Involvement. World J Surg. 2022;46(4):820–828. doi:10.1007/s00268-022-06448-6
40. Szabo Yamashita T, Rogers RT, Foster TR, et al. Medullary thyroid cancer: what is the optimal management of the lateral neck in a node negative patient at index operation? Surgery. 2022;171(1):177–181. doi:10.1016/j.surg.2021.04.052
41. Spanheimer PM, Ganly I, Chou JF, et al. Prophylactic Lateral Neck Dissection for Medullary Thyroid Carcinoma is not Associated with Improved Survival. Ann Surg Oncol. 2021;28(11):6572–6579. doi:10.1245/s10434-021-09683-8
42. Ito Y, Miyauchi A, Kihara M, Higashiiyama T, Fukushima M, Miya A. Static Prognostic Factors and Appropriate Surgical Designs for Patients with Medullary Thyroid Carcinoma: the Second Report from a Single-Institution Study in Japan. World J Surg. 2018;42(12):3954–3966. doi:10.1007/s00268-018-4738-z
43. Machens A, Lorenz K, Dralle H. Prediction of biochemical cure in patients with medullary thyroid cancer. Br J Surg. 2020;107(6):695–704. doi:10.1002/bjs.11444
44. Niccoli-Sire P, Murat A, Rohmer V, et al. When should thyroidectomy be performed in familial medullary thyroid carcinoma gene carriers with non-cysteine RET mutations? Surgery. 2003;134(6):1029–1036. doi:10.1016/j.surg.2003.07.019
45. Elisei R, Romei C, Renzini G, et al. The timing of total thyroidectomy in RET gene mutation carriers could be personalized and safely planned on the basis of serum calcitonin: 18 years experience at one single center. J Clin Endocrinol Metab. 2012;97(2):426–435. doi:10.1210/jc.2011-2046
46. Pelizzo MR, Torresan F, Boschin IM, et al. Early, Prophylactic Thyroidectomy in Hereditary Medullary Thyroid Carcinoma: a 26-year Monoinstitutional Experience. Am J Clin Oncol. 2015;38(5):508–513. doi:10.1097/COC.0b013e3182a78fec
47. Febrero B, Rodríguez JM, Ríos A, et al. Prophylactic thyroidectomy in multiple endocrine neoplasia 2 (MEN2) patients with the C634Y mutation: a long-term follow-up in a large single-center cohort. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2019;45(4):625–630. doi:10.1016/j.ejso.2018.09.002
48. Voss RK, Feng L, Lee JE, et al. Medullary Thyroid Carcinoma in MEN2A: ATA Moderate- or High-Risk RET Mutations Do Not Predict Disease Aggressiveness. J Clin Endocrinol Metab. 2017;102(8):2807–2813. doi:10.1210/jc.2017-00317
49. Rohmer V, Vidal-Trecan G, Bourdelot A, et al. Prognostic factors of disease-free survival after thyroidectomy in 170 young patients with a RET germline mutation: a multicenter study of the Groupe Francais d’Etude des Tumeurs Endocrines. J Clin Endocrinol Metab. 2011;96(3):E509–518. doi:10.1210/jc.2010-1234
50. Opsahl EM, Brauckhoff M, Schlichting E, et al. A Nationwide Study of Multiple Endocrine Neoplasia Type 2A in Norway: predictive and Prognostic Factors for the Clinical Course of Medullary Thyroid Carcinoma. Thyroid off J Am Thyroid Assoc. 2016;26(9):1225–1238. doi:10.1089/thy.2015.0673
51. Castinetti F, Waguespack SG, Machens A, et al. Natural history, treatment, and long-term follow up of patients with multiple endocrine neoplasia type 2B: an international, multicentre, retrospective study. Lancet Diabetes Endocrinol. 2019;7(3):213–220. doi:10.1016/S2213-8587(18)30336-X
52. Machens A, Ukkat J, Hauptmann S, Dralle H. Abnormal carcinoembryonic antigen levels and medullary thyroid cancer progression: a multivariate analysis. Arch Surg Chic Ill. 2007;142(3):289–293. doi:10.1001/archsurg.142.3.289
53. Machens A, Lorenz K, Dralle H. Utility of serum procalcitonin for screening and risk stratification of medullary thyroid cancer. J Clin Endocrinol Metab. 2014;99(8):2986–2994. doi:10.1210/jc.2014-1278
54. Tuttle RM, Ganly I. Risk stratification in medullary thyroid cancer: moving beyond static anatomic staging. Oral Oncol. 2013;49(7):695–701. doi:10.1016/j.oraloncology.2013.03.443
55. Lindsey SC, Ganly I, Palmer F, Tuttle RM. Response to initial therapy predicts clinical outcomes in medullary thyroid cancer. Thyroid off J Am Thyroid Assoc. 2015;25(2):242–249. doi:10.1089/thy.2014.0277
56. Cho YY, Jang HW, Jang JY, et al. Clinical outcomes of patients with hypercalcitoninemia after initial treatment for medullary thyroid cancer and postoperative serum calcitonin cutoffs for predicting structural recurrence. Head Neck. 2016;38(10):1501–1508. doi:10.1002/hed.24469
57. Kwon H, Kim WG, Jeon MJ, et al. Dynamic risk stratification for medullary thyroid cancer according to the response to initial therapy. Endocrine. 2016;53(1):174–181. doi:10.1007/s12020-015-0849-6
58. Jung KY, Kim SM, Yoo WS, et al. Postoperative biochemical remission of serum calcitonin is the best predictive factor for recurrence-free survival of medullary thyroid cancer: a large-scale retrospective analysis over 30 years. Clin Endocrinol. 2016;84(4):587–597. doi:10.1111/cen.12852
59. Choi JB, Lee SG, Kim MJ, et al. Dynamic risk stratification in medullary thyroid carcinoma: single institution experiences. Medicine. 2018;97(3):e9686. doi:10.1097/MD.0000000000009686
60. Rosario PW, Calsolari MR. Influence of chronic autoimmune thyroiditis and papillary thyroid cancer on serum calcitonin levels. Thyroid off J Am Thyroid Assoc. 2013;23(6):671–674. doi:10.1089/thy.2012.0564
61. Duval MA, Ferreira CV, Marmitt L, et al. An undetectable postoperative calcitonin level is associated with long-term disease-free survival in medullary thyroid carcinoma: results of a retrospective cohort study. Thyroid off J Am Thyroid Assoc. 2022. doi:10.1089/thy.2022.0295
62. Fanget F, Demarchi MS, Maillard L, Lintis A, Decaussin M, Lifante JC. Medullary thyroid cancer outcomes in patients with undetectable versus normalized postoperative calcitonin levels. Br J Surg. 2021;108(9):1064–1071. doi:10.1093/bjs/znab106
63. Saltiki K, Rentziou G, Stamatelopoulos K, et al. Small medullary thyroid carcinoma: post-operative calcitonin rather than tumour size predicts disease persistence and progression. Eur J Endocrinol. 2014;171(1):117–126. doi:10.1530/EJE-14-0076
64. Pellegriti G, Leboulleux S, Baudin E, et al. Long-term outcome of medullary thyroid carcinoma in patients with normal postoperative medical imaging. Br J Cancer. 2003;88(10):1537–1542. doi:10.1038/sj.bjc.6600930
65. Costante G, Meringolo D. Calcitonin as a biomarker of C cell disease: recent achievements and current challenges. Endocrine. 2020;67(2):273–280. doi:10.1007/s12020-019-02183-6
66. Barbet J, Campion L, Kraeber-Bodéré F, Chatal JF, GTE Study Group. Prognostic impact of serum calcitonin and carcinoembryonic antigen doubling-times in patients with medullary thyroid carcinoma. J Clin Endocrinol Metab. 2005;90(11):6077–6084. doi:10.1210/jc.2005-0044
67. Hassan A, Siddique M, Riaz S, Khan AI, Nawaz MK, Bashir H. Medullary Thyroid Carcinoma: prognostic Variables And Tumour Markers Affecting Survival. J Ayub Med Coll Abbottabad JAMC. 2018;30(Suppl 1):798.
68. Miyauchi A, Onishi T, Morimoto S, et al. Relation of doubling time of plasma calcitonin levels to prognosis and recurrence of medullary thyroid carcinoma. Ann Surg. 1984;199(4):461–466. doi:10.1097/00000658-198404000-00014
69. Meijer JAA, le Cessie S, van den Hout WB, et al. Calcitonin and carcinoembryonic antigen doubling times as prognostic factors in medullary thyroid carcinoma: a structured meta-analysis. Clin Endocrinol. 2010;72(4):534–542. doi:10.1111/j.1365-2265.2009.03666.x
70. Chen L, Sun W, Qian K, et al. High Ratio of Early Postoperative Calcitonin to Preoperative Calcitonin Could be a Novel Indicator of Poor Prognosis in Patients with Biochemical Incomplete Responses in Sporadic Medullary Thyroid Cancer. Endocr Pract off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2020;26(7):738–747. doi:10.4158/EP-2019-0404
71. Gawlik T, d’Amico A, Szpak-Ulczok S, et al. The prognostic value of tumor markers doubling times in medullary thyroid carcinoma - preliminary report. Thyroid Res. 2010;3(1):10. doi:10.1186/1756-6614-3-10
72. Laure Giraudet A, Al Ghulzan A, Aupérin A, et al. Progression of medullary thyroid carcinoma: assessment with calcitonin and carcinoembryonic antigen doubling times. Eur J Endocrinol. 2008;158(2):239–246. doi:10.1530/EJE-07-0667
73. Beveridge T, Niederer W, Nüesch E, Petrin A. Pharmacokinetic study with synthetic salmon calcitonin (Sandoz). Z Gastroenterol Verh. 1976;2(10):12–15.
74. West TET, O’riordan JLH, Care AD. The clearance of homologous calcitonin. J Endocrinol. 1969;45(4):495–504. doi:10.1677/joe.0.0450495
75. Faggiano A, Milone F, Ramundo V, et al. A decrease of calcitonin serum concentrations less than 50 percent 30 minutes after thyroid surgery suggests incomplete C-cell tumor tissue removal. J Clin Endocrinol Metab. 2010;95(9):E32–36. doi:10.1210/jc.2010-0045
76. Brauckhoff M, Gimm O, Brauckhoff K, Ukkat J, Thomusch O, Dralle H. Calcitonin kinetics in the early postoperative period of medullary thyroid carcinoma. Langenbecks Arch Surg. 2001;386(6):434–439. doi:10.1007/s004230100252
77. Machens A, Lorenz K, Dralle H. Time to calcitonin normalization after surgery for node-negative and node-positive medullary thyroid cancer. Br J Surg. 2019;106(4):412–418. doi:10.1002/bjs.11071
78. Andrade F, Rondeau G, Boucai L, et al. Serum calcitonin nadirs to undetectable levels within 1 month of curative surgery in medullary thyroid cancer. Arch Endocrinol Metab. 2019;63(2):137–141. doi:10.20945/2359-3997000000112
79. H S. The carcinoembryonic antigen (CEA) family: structures, suggested functions and expression in normal and malignant tissues. Semin Cancer Biol. 1999;9(2). doi:10.1006/scbi.1998.0119
80. Kodama T, Fujino M, Endo Y, et al. Identification of carcinoembryonic antigen in the C-cell of the normal thyroid. Cancer. 1980;45(1):98–101. doi:10.1002/1097-0142(19800101)45:1<98::aid-cncr2820450117>3.0.co;2-c
81. Herbeth B, Bagrel A. A study of factors influencing plasma CEA levels in an unselected population. Oncodevelopmental Biol Med J Int Soc Oncodevelopmental Biol Med. 1980;1(4–5):67.
82. Correia-Deur JEM, Toledo RA, Imazawa AT, et al. Sporadic medullary thyroid carcinoma: clinical data from a university hospital. Clin Sao Paulo Braz. 2009;64(5):379–386. doi:10.1590/s1807-59322009000500002
83. Modigliani E, Cohen R, Campos JM, et al. Prognostic factors for survival and for biochemical cure in medullary thyroid carcinoma: results in 899 patients. The GETC Study Group. Groupe d’étude des tumeurs à calcitonine. Clin Endocrinol. 1998;48(3):265–273. doi:10.1046/j.1365-2265.1998.00392.x
84. Fan W, Xiao C, Wu F. Analysis of risk factors for cervical lymph node metastases in patients with sporadic medullary thyroid carcinoma. J Int Med Res. 2018;46(5):1982–1989. doi:10.1177/0300060518762684
85. Ye L, Zhou X, Lu J, Wang Y, Xie X, Zhang J. Combining serum calcitonin, carcinoembryonic antigen, and neuron-specific enolase to predict lateral lymph node metastasis in medullary thyroid carcinoma. J Clin Lab Anal. 2020;34(7):e23278. doi:10.1002/jcla.23278
86. Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E. Nonparallel patterns of calcitonin and carcinoembryonic antigen levels in the follow-up of medullary thyroid carcinoma. Cancer. 1984;53(2):278–285. doi:10.1002/1097-0142(19840115)53:2<278::aid-cncr2820530216>3.0.co;2-z
87. Woliński K, Kaznowski J, Klimowicz A, et al. Diagnostic value of selected biochemical markers in the detection of recurrence of medullary thyroid cancer - comparison of calcitonin, procalcitonin, chromogranin A, and carcinoembryonic antigen. Endokrynol Pol. 2017;68(4):434–437. doi:10.5603/EP.a2017.0038
88. Ishikawa N, Hamada S. Association of medullary carcinoma of the thyroid with carcinoembryonic antigen. Br J Cancer. 1976;34(2):111–115. doi:10.1038/bjc.1976.133
89. Mendelsohn G, Wells SA, Baylin SB. Relationship of tissue carcinoembryonic antigen and calcitonin to tumor virulence in medullary thyroid carcinoma. An immunohistochemical study in early, localized, and virulent disseminated stages of disease. Cancer. 1984;54(4):657–662. doi:10.1002/1097-0142(1984)54:4<657::aid-cncr2820540412>3.0.co;2-v
90. Raue F, Frank-Raue K. Long-Term Follow-up in Medullary Thyroid Carcinoma. Recent Results Cancer Res Fortschritte Krebsforsch Progres Dans Rech Sur Cancer. 2015;204:207–225. doi:10.1007/978-3-319-22542-5_10
91. Ito K, Hibi K, Ando H, et al. Usefulness of analytical CEA doubling time and half-life time for overlooked synchronous metastases in colorectal carcinoma. Jpn J Clin Oncol. 2002;32(2):54–58. doi:10.1093/jjco/hyf011
92. Verhelst J, Vanden Broecke E, Van Meerbeeck J, De Backer W, Blockx P, Vermeire P. Calculation of half-life of carcinoembryonic antigen after lung tumour resection: a case report. Eur Respir J. 1991;4(3):374–376.
93. Maruna P, Nedelníková K, Gürlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000;49 Suppl 1:S57–S61.
94. Bihan H, Becker KL, Snider RH, et al. Calcitonin precursor levels in human medullary thyroid carcinoma. Thyroid off J Am Thyroid Assoc. 2003;13(8):819–822. doi:10.1089/105072503768499716
95. Giovanella L, Garo ML, Ceriani L, Paone G, Campenni’ A, D’Aurizio F. Procalcitonin as an Alternative Tumor Marker of Medullary Thyroid Carcinoma. J Clin Endocrinol Metab. 2021;106(12):3634–3643. doi:10.1210/clinem/dgab564
96. Rosario PW, Mourão GF. Diagnostic Utility of Procalcitonin for Sporadic Medullary Thyroid Carcinoma in Patients with Nodular Disease and Mild or Moderate Hypercalcitoninemia. Horm Metab Res Horm Stoffwechselforschung Horm Metab. 2022;54(4):220–223. doi:10.1055/a-1773-1127
97. Giovanella L, Verburg FA, Imperiali M, Valabrega S, Trimboli P, Ceriani L. Comparison of serum calcitonin and procalcitonin in detecting medullary thyroid carcinoma among patients with thyroid nodules. Clin Chem Lab Med. 2013;51(7):1477–1481. doi:10.1515/cclm-2012-0610
98. Giovanella L, Fontana M, Keller F, Verburg FA, Ceriani L. Clinical performance of calcitonin and procalcitonin Elecsys® immunoassays in patients with medullary thyroid carcinoma. Clin Chem Lab Med. 2021;59(4):743–747. doi:10.1515/cclm-2020-1424
99. Meisner M, Schmidt J, Hüttner H, Tschaikowsky K. The natural elimination rate of procalcitonin in patients with normal and impaired renal function. Intensive Care Med. 2000;26 Suppl 2:S212-216. doi:10.1007/BF02900740
100. Machens A, Hoffmann F, Sekulla C, Dralle H. Importance of gender-specific calcitonin thresholds in screening for occult sporadic medullary thyroid cancer. Endocr Relat Cancer. 2009;16(4):1291–1298. doi:10.1677/ERC-09-0136
101. Milman S, Whitney KD, Fleischer N. Metastatic medullary thyroid cancer presenting with elevated levels of CA 19-9 and CA 125. Thyroid off J Am Thyroid Assoc. 2011;21(8):913–916. doi:10.1089/thy.2010.0425
102. Elisei R, Lorusso L, Romei C, et al. Medullary thyroid cancer secreting carbohydrate antigen 19-9 (Ca 19-9): a fatal case report. J Clin Endocrinol Metab. 2013;98(9):3550–3554. doi:10.1210/jc.2013-1940
103. Milman S, Arnold JL, Price M, et al. Medullary thyroid cancer that stains negative for ca 19-9 has decreased metastatic potential. Endocr Pract off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2015;21(6):590–594. doi:10.4158/EP14357.OR
104. Vargas CVF, Ceolin L, Scheffel RS, Benini AF, Graudenz MS, Maia AL. The tissue expression pattern of CA 19.9 is associated with oncological features in medullary thyroid carcinoma. Endocrine. 2020;70(3):544–551. doi:10.1007/s12020-020-02377-3
105. Elisei R, Lorusso L, Piaggi P, et al. Elevated level of serum carbohydrate antigen 19.9 as predictor of mortality in patients with advanced medullary thyroid cancer. Eur J Endocrinol. 2015;173(3):297–304. doi:10.1530/EJE-15-0304
106. Lorusso L, Romei C, Piaggi P, et al. Ca19.9 Positivity and Doubling Time Are Prognostic Factors of Mortality in Patients with Advanced Medullary Thyroid Cancer with No Evidence of Structural Disease Progression According to Response Evaluation Criteria in Solid Tumors. Thyroid off J Am Thyroid Assoc. 2021;31(7):1050–1055. doi:10.1089/thy.2020.0060
107. Alencar R, Kendler DB, Andrade F, et al. CA19-9 as a Predictor of Worse Clinical Outcome in Medullary Thyroid Carcinoma. Eur Thyroid J. 2019;8(4):186–191. doi:10.1159/000497201
108. Yamaguchi K, Abe K, Kameya T, et al. Production and molecular size heterogeneity of immunoreactive gastrin-releasing peptide in fetal and adult lungs and primary lung tumors. Cancer Res. 1983;43(8):3932–3939.
109. Parra-Robert M, Orois A, Augé JM, Halperin I, Filella X, Molina R. Utility of proGRP as a tumor marker in the medullary thyroid carcinoma. Clin Chem Lab Med. 2017;55(3):441–446. doi:10.1515/cclm-2016-0572
110. Liang X, Zhu J, Cai M, et al. Progrp as a novel biomarker for the differential diagnosis of medullary thyroid carcinoma in patients with thyroid nodules. Endocr Pract off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2020;26(5):514–522. doi:10.4158/EP-2019-0396
111. Giovanella L, Fontana M, Keller F, Campenni’ A, Ceriani L, Paone G. Circulating pro-gastrin releasing peptide (ProGRP) in patients with medullary thyroid carcinoma. Clin Chem Lab Med. 2021;59(9):1569–1573. doi:10.1515/cclm-2021-0361
112. O’Connor DT, Deftos LJ. Secretion of chromogranin A by peptide-producing endocrine neoplasms. N Engl J Med. 1986;314(18):1145–1151. doi:10.1056/NEJM198605013141803
113. Blind E, Schmidt-Gayk H, Sinn HP, O’Connor DT, Raue F. Chromogranin A as tumor marker in medullary thyroid carcinoma. Thyroid off J Am Thyroid Assoc. 1992;2(1):5–10. doi:10.1089/thy.1992.2.5
114. Nobels FR, Kwekkeboom DJ, Coopmans W, et al. Chromogranin A as serum marker for neuroendocrine neoplasia: comparison with neuron-specific enolase and the alpha-subunit of glycoprotein hormones. J Clin Endocrinol Metab. 1997;82(8):2622–2628. doi:10.1210/jcem.82.8.4145
115. Franke WG, Pinkert J, Runge R, Bredow J, Wunderlich G, Koch R. Chromogranin A: an additional tumor marker for postoperative recurrence and metastases of medullary thyroid carcinomas? Anticancer Res. 2000;20(6D):56.
116. Guignat L, Bidart JM, Nocera M, Comoy E, Schlumberger M, Baudin E. Chromogranin A and the alpha-subunit of glycoprotein hormones in medullary thyroid carcinoma and phaeochromocytoma. Br J Cancer. 2001;84(6):808–812. doi:10.1054/bjoc.2000.1677
117. de Groot JWB, Kema IP, Breukelman H, et al. Biochemical markers in the follow-up of medullary thyroid cancer. Thyroid off J Am Thyroid Assoc. 2006;16(11):1163–1170. doi:10.1089/thy.2006.16.1163
118. Baudin E, Gigliotti A, Ducreux M, et al. Neuron-specific enolase and chromogranin A as markers of neuroendocrine tumours. Br J Cancer. 1998;78(8):1102–1107. doi:10.1038/bjc.1998.635
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
