Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Serum β2-Microglobulin is Associated with Mortality in Hospitalized Patients with Exacerbated Chronic Obstructive Pulmonary Disease
Authors Mao W , Wang J, Zhang L, Wang Y , Wang W , Zeng N, Zhang J, li Q, Jiao F, Li J, Cui N, Mi S, Xue Y, Wang Z, Ying S, Huang K
Received 23 January 2020
Accepted for publication 15 March 2020
Published 7 April 2020 Volume 2020:15 Pages 723—732
DOI https://doi.org/10.2147/COPD.S243905
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chunxue Bai
Wenping Mao,1,2 Jing Wang,1,2 Liming Zhang,1,2 Ying Wang,1,2 Wenjun Wang,1,2 Na Zeng,3 Jun Zhang,1,2 Qian li,1,2 Fengwei Jiao,1,2 Jie Li,1,2 Na Cui,1,2 Song Mi,1,2 Yi Xue,1,2 Zhaomei Wang,1,2 Sun Ying,4 Kewu Huang1,2
1Beijing Key Laboratory of Respiratory and Pulmonary Circulation Disorders, Department of Pulmonary and Critical Care Medicine, Beijing Chao-Yang Hospital, Capital Medical University, Beijing 100020, People’s Republic of China; 2Beijing Institute of Respiratory Medicine, Beijing 100020, People’s Republic of China; 3Clinical Epidemiology and EBM Unit, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, People’s Republic of China; 4Department of Immunology, School of Basic Medical Sciences, Capital Medical University, Beijing 100069, People’s Republic of China
Correspondence: Kewu Huang
Department of Pulmonary and Critical Care Medicine, Beijing Chao-Yang Hospital, Capital Medical University, No. 8, Gongti South Road, Chaoyang District, Beijing 100020, People’s Republic of China
Tel + 86-10-85231167
Email [email protected]
Purpose: We hypothesized that increased level of serum β 2-microglobulin (β 2M) is an independent factor associated with higher mortality in hospitalized patients with exacerbated chronic obstructive pulmonary disease (COPD).
Patients and Methods: We retrospectively analyzed 488 hospitalized patients with exacerbated COPD as the first diagnosis at Beijing Chao-Yang hospital, P. R. China between December 31st, 2012 and December 28th, 2017. Concentrations of serum β 2M and other clinical indexes were measured or collected on admission, and all patients were followed up to 90 days. The relationship between β 2M and 30- and 90-day all-cause mortality was explored by Cox regression analysis adjusted for age, C-reactive protein values, N-terminal pro-brain natriuretic peptide/100, respiratory failure [RF, defined as partial arterial oxygen pressure (PaO2) < 60 mmHg on room air or PaO2 over the fraction of inspired oxygen (PaO2/FiO2) < 300], eosinopenia, consolidation, and acidaemia.
Results: Median concentrations of β 2M were significantly higher in non-survivals compared to survivals within 30 days (4.11 mg/L (IQR 3.10– 6.60) vs 2.79mg/L (IQR 2.13– 3.76), P < 0.001) and 90 days (3.79 mg/L (IQR 2.61– 6.69) vs 2.79 mg/L (IQR 2.13– 3.73), P < 0.001). Serum levels of β 2M were correlated with 30-day and 90-day mortality in overall exacerbated COPD patients, with hazard ratios (HRs) of 1.09 (95% CI 1.04– 1.14, P = 0.001) and 1.09 (95% CI 1.05– 1.14, P < 0.001). In exacerbated COPD patients without RF and with RF, the HRs were 1.06 (95% CI 0.995– 1.137, P = 0.069) and 1.14 (95% CI 1.02– 1.27, P = 0.021) for 30-day mortality, 1.09 (95% CI 1.02– 1.15, P = 0.010) and 1.14 (95% CI 1.03– 1.26, P = 0.014) for 90-day mortality, respectively.
Conclusion: Our data showed that concentrations of serum β 2M were associated with an increased risk of mortality, suggesting that β 2M might be a valuable predictor of poor prognosis for hospitalized patients with exacerbated COPD.
Keywords: β 2-microglobulin, COPD, exacerbation, predictor, prognosis
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable and treatable disease characterized by persistent respiratory symptoms and airflow limitation.1 COPD is the primary cause for morbidity and mortality worldwide, which also causes a great socio-economic burden. According to the report of WHO, COPD will become the third leading cause of death worldwide in 2030.2 The China Pulmonary Health (CPH) study shows that the prevalence of spirometry-defined COPD is 13.7% for people aged 40 years or older.3 Exacerbations of COPD are important events in the course of the disease because these impacts on health status negatively increase rates of hospitalization and readmission, and cause disease progression.4–6 It has been identified that some prognostic factors are significantly associated with the increase in short-term mortality in hospitalized patients with exacerbated COPD, including age, cardiac failure, chronic renal failure, long-term oxygen therapy, cor pulmonale, academia, etc.7 Previous studies have shown that numerous events, such as concentrations of plasma soluble urokinase plasminogen activator receptor,8 C-reactive protein (CRP),8 serum D-dimer,9 N-terminal pro-brain natriuretic peptide (NT-proBNP),10 the neutrophil–lymphocyte ratio (NLR),11 and the DECAF Score (composed of extended MRC Dyspnea Score, eosinopenia, consolidation, acidaemia, and atrial fibrillation),12,13 might be independent risk factors for short-time mortality in admitted patients with exacerbated COPD.
β2-microglobulin (β2M) is a 11.8 kD protein consisting of 100 amino acids encoded by a gene located in chromosome15 in humans. It has been known that β2M, associated with both classical and non-classical MHC Class I molecules on the surface of all nucleated cells, is crucial for antigen presentation, immunoglobulin transport and iron metabolism.14 It has been also known that β2M is continuously generated by all nucleated cells, and freely filtered by the glomerulus, with more than 99.9% reabsorbed and metabolized in the proximal tubule.15 Numerous studies have shown that β2M is not only used in assessing renal function by estimating glomerular filtration rate and monitoring the effects of treatment16,17 but also associated with a number of clinic status, including chronic inflammatory diseases, malignancies, poor outcome of chronic diseases and so on.15
Our previous study has shown that concentrations of serum β2M are significantly elevated in patients with COPD compared to those of the healthy population and that β2M might contribute to the pathogenesis of lung emphysema through inducing epithelial cell senescence.18 These findings suggest that β2M might reflect the chronic inflammatory status and also be a molecule related to aging. Recently, a large cohort study has also shown that aging and chronic inflammation are associated with an increasing mortality of exacerbated COPD.19 However, to our knowledge, the value of β2M, as a prognostic index for short time all-cause death of exacerbated COPD, has not been investigated so far. In the present study, we hypothesized that concentrations of serum β2M at the time of admission in hospitalized patients with exacerbated COPD are a prognostic predictor for short time all-cause death.
Materials and Methods
Study Design and Patients
We retrospectively enrolled patients with exacerbated COPD who were admitted in Beijing Chao-Yang Hospital, Capital Medical University, Beijing, P. R. China, from December 31st, 2012 to December 28th, 2017. For patients with repeated hospital admissions, only the last hospitalized data were recorded. Patients were followed up to 30 days or 90 days from admission by telephone or by hospital electronic information system. All-cause death was the outcome. The Institutional Review Board for Beijing Chao-Yang Hospital approved the study with a waiver of informed consent (2014-ke-115), which was conducted in accordance with the Declaration of Helsinki.
Patients with exacerbated COPD including both acute exacerbation of COPD (AECOPD) defined as an acute change from baseline in one or more of symptoms including dyspnea, cough and sputum, beyond normal day-to-day variation19 and pneumonic COPD defined as patients complicated by radiographic consolidation12 were recruited in the present study. For inclusion, primary diagnosis of all patients was exacerbated COPD. In addition, inclusive criteria also included as following: age ≥40 years; post-bronchodilator forced expiratory volume in 1s (FEV1) and forced vital capacity (FVC) of less than 0.70 according to the diagnostic criteria of Global Initiative for Chronic Obstructive Lung Disease (GOLD). Furthermore, serum level of β2M, creatinine (Cr), CRP, NT-proBNP, routine blood test, arterial blood gas analysis, electrocardiography and chest image were measured or took on admission within 24 hours. Primary exclusion criteria: patients were excluded for those primary diagnoses for hospitalization was not exacerbated COPD.
In the present study, respiratory failure (RF) was defined as partial arterial oxygen pressure (PaO2) < 60 mmHg on room air or PaO2 over the fraction of inspired oxygen (PaO2/FiO2) <300 according to arterial blood gas analysis for patients on oxygen regardless of partial carbon dioxide pressure (PaCO2) and pH value.20,21 In this case, patients with exacerbated COPD were further divided into exacerbated COPD with RF and without RF. The flow chart is shown in Figure 1.
 |
Figure 1 Flow chart of the study for recruiting and grouping participants. Abbreviations: COPD, chronic obstructive pulmonary disease; RF, respiratory failure. |
Data Collection
Demographic and clinical data were collected from all subjects on admission within 24 hours, including age, sex, height, weight, smoking history, history of oxygen therapy, comorbidities, concentrations of serum β2M, Cr, CRP, NT-proBNP, eosinophil count, arterial blood gas analysis, electrocardiography and chest image.
Concentrations of serum β2M and Cr were measured using Latex immune turbidity and Oxidase method by Beckman Coulter UniCel DXC800 (Beckman Coulter, Inc., USA). NT-proBNP was measured using fluorescence immunoassay by TZ-310 Dry fluorescence immunoassay (ReLIA Biotechnologies Ltd., China). CRP was measured using solid-phase sandwich format immunometric assay by NycoCardTM READER II (Alere Technologies AS, Norway).
Eosinopenia and acidaemia were determined according to eosinophil count < 0.05×109/L and pH < 7.3.12 Atrial fibrillation (AF) was diagnosed by electrocardiography at the time of hospital admission.
The severity of comorbid diseases, such as coronary heart disease, diabetes mellitus, cerebrovascular disease, dementia, connective tissue disease, cancer, congestive heart failure, kidney disease, etc., was recorded and scored according to the Charlson comorbidity index (CCI) updated by Quan et al.22,23 We estimated creatinine clearance rate (Ccr) (mL/min) with the Cockroft-Gaultequation: Ccr = ([140 – age in years] × bodyweight in kg)/(72 × serum creatinine in mg/dL). For women, the calculated values were multiplied by 0.85.
Death from any cause within 30 or 90 days started from admission was recorded.
Statistical Analysis
Continuous variables were presented as median and interquartile range (IQR) or mean (standard deviation). Categorical variables were presented as numbers (n) and percentages (%). Differences of β2M values and other variables between groups were compared by Mann–Whitney U-tests or Chi-squared test. Both univariate and multivariate Cox regression analyses were applied to evaluate the relationship between concentrations of serum β2M and the time to death. Results were presented as hazard ratios (HRs) with 95% confidence intervals (CIs). Concentration of serum β2M was adjusted for age, CRP, NT-proBNP/100, RF, eosinopenia, consolidation and acidaemia in multivariate Cox regression analysis. Subgroups were further divided according to whether patients were with or without RF. The differences in the mortality rates were grouped by β2M median in overall exacerbated COPD, while subgroups were also analyzed by Chi-squared test. Survivals by β2M median in overall exacerbated COPD patients were presented in accumulative survival curves adjusted by above-mentioned variables. ROC curve analyses for diagnostic accuracy of β2M on 30-day and 90-day mortality in overall patients with exacerbated COPD was also performed. The areas under receiver operating curves (ROC-AUC) were used to assess the prognostic value of biomarkers. SPSS 23.0 was used for statistical analysis. P < 0.05 was considered to be statistically significant.
Results
Characteristics of Included Subjects
In the present study, total of 488 hospitalized patients with exacerbated COPD (340 men, 148 women, with a median age of 77 years old) were enrolled from 685 patients chosen and 197 of those patients were excluded from the final analysis because of the missing of variables. Among 488 patients, 307 patients had no RF and 181 patients had RF. The median concentrations of serum β2M were 2.90 mg/L (IQR: 2.16–3.88), 2.82 mg/L (IQR: 2.15–3.80) and 3.08 mg/L (IQR: 2.17–3.98) in overall subjects with exacerbated COPD, subjects with exacerbated COPD but without RF and subjects with exacerbated COPD and RF, respectively (Table 1).
 |
Table 1 Demographic and Clinical Characteristics of Patients with Exacerbated COPD |
Analysis of Mortality Rate of Overall Exacerbated COPD Patients and of Exacerbated COPD Patients Grouped by RF
Median concentration of serum β2M was significantly higher among non-survivals within 30 days of follow-up compared to survivals in overall exacerbated COPD, exacerbated COPD without RF and exacerbated COPD with RF (P < 0.01 for all). The similar results were also observed in the subjects involved within 90 days of follow-up (P < 0.01 for all). When the subjects were grouped by median of β2M, the mortality rates of 30 or 90 days were significantly increased in the group of patients with higher concentrations of serum β2M compared to those with lower serum β2M, except that 90-day mortality rate in exacerbated COPD with RF (Table 2). The differences of other data between the subgroups are shown in Supplemental Table 1.
 |
Table 2 Mortality Rates and Concentrations of Serum β2M in Hospitalized Patients with Exacerbated COPD |
Analysis of β2M and Other Variables by Rank Correlation
Furthermore, the concentrations of serum β2M were positively correlated with age (Spearman correlation coefficient 0.409), CCI updated (Spearman correlation coefficient 0.195), serum CRP (Spearman correlation coefficient 0.255), NT-proBNP (Spearman correlation coefficient 0.270) and lower Ccr (Spearman correlation coefficient −0.524) in overall exacerbated COPD (P <0.001 for all) (Supplementary Table 2).
Univariate and Multivariate Survival Analyses
Univariate Cox regression analysis showed that concentration of serum β2M was a mortality risk factor for both 30-day and 90-day mortalities in overall exacerbated COPD patients because the HRs and 95% CIs were 1.14 (95% CI 1.10–1.18) for 30-day mortality and 1.15 (95% CI 1.11–1.18) for 90-day mortality, respectively, in overall exacerbated COPD patients (P < 0.001 for both). In addition, age, serum CRP, RF, CCI updated, Ccr, serum NT-proBNP, eosinopenia, consolidation and acidaemia were also risk factors for both 30-day and 90-day mortalities in overall exacerbated COPD and exacerbated COPD without RF. The similar results were also observed in exacerbated COPD with RF except for CCI updated (Table 3).
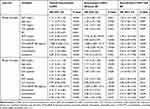 |
Table 3 Univariate Survival Analysis of 30-Day and 90-Day Mortality Risk in Hospitalized Patients with Exacerbated COPD |
In the multivariate Cox analysis, concentration of serum β2M was an independent mortality risk factor for both 30-day (HR, 1.09, 95% CI: 1.04–1.14, P = 0.001) and 90-day mortalities (HR, 1.09, 95% CI: 1.05–1.14, P < 0.001) in overall exacerbated COPD patients. In addition, age, CRP, NT-proBNP/100, RF, eosinopenia, consolidation, acidaemia were also independent mortality risk factors for 30-day and 90-day mortalities in overall exacerbated COPD (P < 0.05 for all). Subgroup analysis showed that concentration of serum β2M was still an independent mortality risk factor in exacerbated COPD patients, regardless with or without RF, but with the exception of 30-day mortality in exacerbated COPD without RF (P = 0.069) (Table 4).
 |
Table 4 Multivariate Survival Analysis of 30-Day and 90-Day Mortality Risk in Hospitalized Patients with Exacerbated COPD |
The data analysis stratified by β2M median showed that the mortality risks were significantly increased in the higher category groups of serum β2M concentration for 30-day in overall exacerbated COPD (>2.9 mg/L) (HR, 2.95, 95% CI 1.26–6.91; P = 0.013) compared to the groups with lower levels of serum β2M (≤2.9 mg/L) when the data were adjusted for age, CRP, NT-proBNP/100, RF, eosinopenia, consolidation, and acidaemia, but higher level of serum β2M was not observed to be associated with 90-day mortality in overall patients with exacerbated COPD when stratified by β2M median adjusted for the above variables (HR, 1.61, 95% CI 0.89–2.91; P = 0.115). (Figure 2A and B).
The Prognostic Value of β2M on 30-Day and 90-Day Mortality in Hospitalized Patients with Exacerbated COPD
The ROC curve analyses showed that the sensitivity and specificity of β2M levels on 30-day and 90-day mortality in overall exacerbated COPD were 72.1% and 65.4%, 62.9% and 65.7%, respectively, when the cutoff value of β2M was 3.27mg/L, and the areas of the ROC curve were 0.732 (95% CI 0.643~0.821, P <0.001) and 0.683 (95% CI 0.602~0.764, P <0.001) for the prediction of 30-day and 90-day mortality, respectively. Similar results were also observed in the sensitivity and specificity of β2M levels on 30-day and 90-day mortality in exacerbated COPD without RF or with RF (Supplemental Table 3).
Discussion
The present study showed that the concentrations of serum β2M were higher in patients who died within 30 days and 90 days on admission compared to those who survived until the data analysis. Furthermore, the concentrations of serum β2M were independently associated with higher 30-day and 90-day all-cause mortality in overall hospitalized patients with exacerbated COPD. To our knowledge, this is the first report suggesting that concentrations of serum β2M might have a predict value in the mortality of all-cause in these patients.
Exacerbations of COPD account for the greatest proportion of the total COPD burden on the healthcare, which causes a substantial economic burden on individuals and society, often requires hospitalization and is continuatively to be correlated with a high mortality rate.1,6 In the present study, mortality rates were 8.8% within 30 days and 12.7% within 90 days in overall hospitalized patients with exacerbated COPD, which are similar to previous reports in which the 30-day and 90-day mortality rates were 6.4% and 13.4%, respectively.8 Thus, early identification of poor prognosis in hospitalized patients with exacerbated COPD may aid in clinical measurements, treatment intervention, resource allocation and improvement of prognosis.
COPD is an age-associated disease and is often accompanied by multiple comorbidities.24 Inflammation plays important role in the pathogenesis of COPD in the peripheral airway, lung parenchyma, pulmonary vessels and even in the circulation, suggesting that systemic inflammation might also exist.25 To support this, a previous study has also shown that systemic inflammation has significant correlation with comorbidities, such as cardiovascular diseases, diabetes and osteoporosis.25 Most importantly, the systemic inflammation could further worsen during exacerbations, which might significantly contribute to the all-cause mortality.26 In addition, it has been known that β2M produced by nucleated cells could reflect multiple aspects of a variety of diseases. Several previous studies have shown that concentrations of serum β2M are higher in patients with Behçet’s disease, inflammatory bowel diease (IBD) and systemic lupus erythematosus (SLE) than those of healthy controls, suggesting that it might be also a useful biomarker for assessment of these autoimmune disease activities.27–29 Elevated concentrations of serum β2M have been also observed in patients with hemato-oncological pathology despite these patients with the preserved renal function and solid cancers.15 It has also shown that concentrations of serum β2M are independently and significantly associated with major cardiovascular events in patients with isolated systolic hypertension (ISH) without severe renal insufficiency,30 and in patients with acute coronary syndromes who underwent successful percutaneous coronary intervention.31
Our data showed that concentrations of serum β2M were associated with advanced age, higher CCI updated, lower Ccr, higher levels of serum CRP and NT-proBNP, which are consistent with the observations of several previous reports.32,33 Taken together, these findings suggest that β2M is a useful predictor associated with aging and inflammation. Furthermore, these might also imply that β2M is a potential indicator in predicting the mortality in some population, such as elderly population, or population with some chronic diseases, or both. This speculation has also been supported by several previous studies, including in elderly population,34 elderly ISH patients,30 heart failure patients35 and chronic kidney disease patients.36
As mentioned above, β2M, as a predictor related to aging and inflammation might not only participate in the pathogenesis of lung emphysema but also play role in the pathophysiological processes during exacerbations of COPD. It has been known that AECOPD patients with respiratory failure, chronic renal failure and cardiac dysfunction normally have poor prognosis.7,37,38 Among these, respiratory failure is the common complication of COPD exacerbation and is the most especially common risk factor causing the death of patients with COPD exacerbation.7,37 Multivariate Cox regression analysis of the present study revealed that the elevated concentration of serum β2M was an independent prognostic factor for all-cause mortality in overall exacerbated COPD patients when adjusted for age, CRP, NT-proBNP/100, RF, eosinopenia, consolidation and acidaemia. These further indicate that concentration of serum β2M is a potential valuable predictor for the poor outcome of exacerbated COPD patients in hospital.
We also found NT-proBNP was an independent risk factor for 30-day and 90-day mortalities, which is consistent with a report from a meta-analysis for both short-time mortality and long-time mortality.7 Another study has also shown that the elevated concentration of NT-proBNP is a prognostic indicator for early mortality, indicating that cardiac involvement may be an important predictor in admitted AECOPD without heart failure.10
Although univariate Cox regression analysis showed that Ccr and CCI updated were also associated with the increasing mortality, there was no correlation between these two variables and mortality observed in multivariate Cox regression analyses, suggesting that concentrations of serum β2M might have a stronger association with 30-day and 90-day mortality than that of Ccr and CCI. This also supports the concept that β2M might be a comprehensive biomarker reflecting renal function and comorbidity severity.
CRP, as a classical inflammatory marker is correlated with the systemic inflammation and has been used to evaluate the prognosis of patients with COPD. Although a previous study derived from a pooled analysis has shown that there was no significant correlation between CRP and early mortality in AECOPD,39 however, another Meta-analysis indicates that individuals with higher levels of CRP measured at baseline have an association with early mortality in stable COPD.40 The differences in criteria of inclusion and data collections might contribute to this inconsistency. In the present cohort, CRP was also an independent prognostic predictor for short-time mortality in overall exacerbated COPD patients, which is consistent with the previous studies conducted in admitted AECOPD patients.8,11
The DECAF score, reported in a prospective study by Steer et al,12 is a simple yet effective predictor of mortality in hospitalized patients with exacerbated COPD. We also collected the clinical variables related DECAF score, including eosinopenia, consolidation, acidaemia and atrial fibrillation, but not stable-state dyspnea assessed using the eMRCD (extended Medical Research Council (MRC) dyspnea) score,41 which was not available in the present retrospective study. After the multivariate Cox regression, we observed that eosinopenia, consolidation, acidaemia were independent predictors for shot-time mortality in our study in overall exacerbated COPD patients. In the present study, atrial fibrillation was not a prognostic factor for exacerbated COPD patients, which is not consistent with the previous study.12,13 The different study designs and variety of baseline characteristics of recruited patients might contribute to the inconsistency.
It is also worth mentioning that there are several limitations in the present study. First, it is a retrospective single-center study, although single-center study has better homogeneity of treatment though reducing the confounding factors caused by the inconsistency of therapeutic regime, which is common in multi-center retrospective study. Secondly, the sample size is relatively small. For example, we did not observe that higher level of serum β2M was associated with 30-day mortality in exacerbated COPD patients without RF after multivariate Cox regression analyses, which might be partly due to relatively few death cases in this group and more adjusted variables. A larger prospective study from multi-center should be taken into account in future. Finally, there were 197 patients among 685 hospitalized patients with exacerbated COPD were excluded from the final analysis due to missing data on CRP or NT-proBNP, which might lead to a selection bias. However, a comparison conducted between the final analysis group and those of 197 patients excluded, showed that there was no significant difference in mortality and other clinical characteristics except for the sex between the two groups (Supplemental Table 4). These results suggest that there was no significant selection bias occurred even though 197 patients were excluded from the final analysis.
Conclusion
The elevated concentrations of serum β2M are associated with higher 30-day and 90-day mortality in overall hospitalized patients with exacerbated COPD. This might be as an independently considerate predictor for evaluating prognosis of these patients. It is obvious, however, that prospective studies are warranted to further investigate the prognostic value of serum β2M for all-cause mortality in hospitalized patients with exacerbated COPD in the future.
Abbreviations
β2M, β2-microglobulin; COPD, chronic obstructive pulmonary disease; AECOPD, acute exacerbation of chronic obstructive pulmonary disease; RF, respiratory failure; BMI, body mass index; CCI, Charlson comorbidity index; CRP, C-reactive protein; FEV1, forced expiratory volume in 1s; FVC, forced vital capacity; GOLD, global initiative for chronic obstructive lung disease; NT-proBNP, N-terminal pro-brain natriuretic peptide, DECAF Score, composed of extended MRC Dyspnea Score, eosinopenia, consolidation, acidaemia and atrial fibrillation; AF, atrial fibrillation.
Acknowledgments
This work was supported by the National Key R&D Program of China, Ministry of Science and Technology of China (2016YFC0901102), the Project of “Deng Feng” Talent Training, Beijing Municipal Administration of Hospitals (DFL20190301) and the National Natural Science Foundation of China (81870032, 81670032).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Chapter 1: definition and overview. 2019; 4. Available from: http://goldcopd.org.
2. World Health Organization. World Health Organization (WHO) website. Available from: www.who.int/respiratory/copd/burden/en/.
3. Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. doi:10.1016/S0140-6736(18)30841-9
4. Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–1422. doi:10.1164/ajrccm.157.5.9709032
5. Ozkaya S, Findik S, Atici AG. The costs of hospitalization in patients with acute exacerbation of chronic obstructive pulmonary disease. Clinicoecon Outcomes Res. 2011;3:15–18. doi:10.2147/CEOR
6. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8
7. Singanayagam A, Schembri S, Chalmers JD. Predictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10(2):81–89. doi:10.1513/AnnalsATS.201208-043OC
8. Godtfredsen NS, Jorgensen DV, Marsaa K, et al. Soluble urokinase plasminogen activator receptor predicts mortality in exacerbated COPD. Respir Res. 2018;19(1):97. doi:10.1186/s12931-018-0803-2
9. Fruchter O, Yigla M, Kramer MR. D-dimer as a prognostic biomarker for mortality in chronic obstructive pulmonary disease exacerbation. Am J Med Sci. 2015;349(1):29–35. doi:10.1097/MAJ.0000000000000332
10. Chang CL, Robinson SC, Mills GD, et al. Biochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPD. Thorax. 2011;66(9):764–768. doi:10.1136/thx.2010.155333
11. Yao C, Liu X, Tang Z. Prognostic role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2285–2290. doi:10.2147/COPD.S141760
12. Steer J, Gibson J, Bourke SC. The DECAF score: predicting hospital mortality in exacerbations of chronic obstructive pulmonary disease. Thorax. 2012;67(11):970–976. doi:10.1136/thoraxjnl-2012-202103
13. Echevarria C, Steer J, Heslop-Marshall K, et al. Validation of the DECAF score to predict hospital mortality in acute exacerbations of COPD. Thorax. 2016;71(2):133–140. doi:10.1136/thoraxjnl-2015-207775
14. Zijlstra M, Bix M, Simister NE, Loring JM, Raulet DH, Beta JR. 2-microglobulin deficient mice lack CD4-8+ cytolytic T cells. Nature. 1990;344(6268):742–746. doi:10.1038/344742a0
15. Argyropoulos CP, Chen SS, Ng YH, et al. Rediscovering beta-2 microglobulin as a biomarker across the spectrum of kidney diseases. Front Med. 2017;4:73. doi:10.3389/fmed.2017.00073
16. Viberti GC, Keen H, Beta MD. 2-microglobulinaemia: a sensitive index of diminishing renal function in diabetics. Br Med J (Clin Res Ed). 1981;282(6258):95–98. doi:10.1136/bmj.282.6258.95
17. Inker LA, Tighiouart H, Coresh J, et al. GFR estimation using beta-trace protein and beta2-microglobulin in CKD. Am J Kidney Dis. 2016;67(1):40–48. doi:10.1053/j.ajkd.2015.07.025
18. Gao N, Wang Y, Zheng CM, et al. Beta2-microglobulin participates in development of lung emphysema by inducing lung epithelial cell senescence. Am J Physiol Lung Cell Mol Physiol. 2017;312(5):L669–L677. doi:10.1152/ajplung.00516.2016
19. Mullerova H, Maselli DJ, Locantore N, et al. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest. 2015;147(4):999–1007. doi:10.1378/chest.14-0655
20. Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374(9685):250–259. doi:10.1016/S0140-6736(09)60496-7
21. Martin-Gonzalez F, Gonzalez-Robledo J, Sanchez-Hernandez F, Moreno-Garcia MN, Barreda-Mellado I. Effectiveness and predictors of failure of noninvasive mechanical ventilation in acute respiratory failure. Med Intensiva. 2016;40(1):9–17. doi:10.1016/j.medin.2015.01.007
22. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
23. Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. doi:10.1093/aje/kwq433
24. Miller J, Edwards LD, Agusti A, et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med. 2013;107(9):1376–1384. doi:10.1016/j.rmed.2013.05.001
25. Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi:10.1016/j.jaci.2016.05.011
26. Hurst JR, Donaldson GC, Perera WR, et al. Use of plasma biomarkers at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;174(8):867–874. doi:10.1164/rccm.200604-506OC
27. Aygunduz M, Bavbek N, Ozturk M, Kaftan O, Kosar A, Kirazli S. Serum beta 2-microglobulin reflects disease activity in behcet’s disease. Rheumatol Int. 2002;22(1):5–8. doi:10.1007/s00296-002-0180-4
28. Yilmaz B, Koklu S, Yuksel O, Arslan S. Serum beta 2-microglobulin as a biomarker in inflammatory bowel disease. World J Gastroenterol. 2014;20(31):10916–10920. doi:10.3748/wjg.v20.i31.10916
29. Kim HA, Jeon JY, Yoon JM, Suh CH. Beta 2-microglobulin can be a disease activity marker in systemic lupus erythematosus. Am J Med Sci. 2010;339(4):337–340. doi:10.1097/MAJ.0b013e3181d26dfb
30. Wang HJ, Si QJ, Shi Y, Guo Y, Li Y, Wang YT. The prognostic values of beta-2 microglobulin for risks of cardiovascular events and mortality in the elderly patients with isolated systolic hypertension. J Res Med Sci. 2018;23(1):82. doi:10.4103/jrms.JRMS_135_17
31. Mockel M, Muller R, Searle J, et al. Usefulness of beta2-microglobulin as a predictor of all-cause and nonculprit lesion-related cardiovascular events in acute coronary syndromes (from the PROSPECT study). Am J Cardiol. 2015;116(7):1034–1040. doi:10.1016/j.amjcard.2015.07.017
32. Evrin PE, Wibell L. The serum levels and urinary excretion of 2 -microglobulin in apparently healthy subjects. Scand J Clin Lab Invest. 1972;29(1):69–74. doi:10.3109/00365517209081057
33. Stanga Z, Nock S, Medina-Escobar P, Nydegger UE, Risch M, Risch L. Factors other than the glomerular filtration rate that determine the serum beta-2-microglobulin level. PLoS One. 2013;8(8):e72073. doi:10.1371/journal.pone.0072073
34. Shinkai S, Chaves PH, Fujiwara Y, et al. Beta2-microglobulin for risk stratification of total mortality in the elderly population: comparison with cystatin C and C-reactive protein. Arch Intern Med. 2008;168(2):200–206. doi:10.1001/archinternmed.2007.64
35. Kawai K, Kawashima S, Miyazaki T, et al. Serum beta2-microglobulin concentration as a novel marker to distinguish levels of risk in acute heart failure patients. J Cardiol. 2010;55(1):99–107. doi:10.1016/j.jjcc.2009.10.003
36. Foster MC, Coresh J, Hsu CY, et al. Serum beta-trace protein and beta2-microglobulin as predictors of ESRD, mortality, and cardiovascular disease in adults with CKD in the chronic renal insufficiency cohort (CRIC) study. Am J Kidney Dis. 2016;68(1):68–76. doi:10.1053/j.ajkd.2016.01.015
37. MacIntyre N, Huang YC. Acute exacerbations and respiratory failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):530–535. doi:10.1513/pats.200707-088ET
38. Pavasini R, Tavazzi G, Biscaglia S, et al. Amino terminal pro brain natriuretic peptide predicts all-cause mortality in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis. Chron Respir Dis. 2017;14(2):117–126. doi:10.1177/1479972316674393
39. Leuzzi G, Galeone C, Taverna F, Suatoni P, Morelli D, Pastorino U. C-reactive protein level predicts mortality in COPD: a systematic review and meta-analysis. Eur Respir Rev. 2017;26(143):160070. doi:10.1183/16000617.0070-2016
40. Fermont JM, Masconi KL, Jensen MT, et al. Biomarkers and clinical outcomes in COPD: a systematic review and meta-analysis. Thorax. 2019;74(5):439–446. doi:10.1136/thoraxjnl-2018-211855
41. Steer J, Norman EM, Afolabi OA, Gibson GJ, Bourke SC. Dyspnoea severity and pneumonia as predictors of in-hospital mortality and early readmission in acute exacerbations of COPD. Thorax. 2012;67(2):117–121. doi:10.1136/thoraxjnl-2011-200332
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

