Back to Journals » Infection and Drug Resistance » Volume 16
Serodiagnosis of Abdominal Abscess Caused by Burkholderia pseudomallei: Case Report and Literature Review
Authors Li Y, He X, Deng L, Chen H, Chen X, Mao X, Xiang Y
Received 18 June 2023
Accepted for publication 16 August 2023
Published 25 August 2023 Volume 2023:16 Pages 5613—5625
DOI https://doi.org/10.2147/IDR.S421739
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Yuanli Li,1,* Xiaoyi He,2,* Ling Deng,2 Hai Chen,1 Xi Chen,1 Xuhu Mao,2 Yang Xiang2
1Department of Clinical Laboratory, Sanya People’s Hospital, Sanya, Hainan, People’s Republic of China; 2Department of Clinical Microbiology and Immunology, College of Pharmacy and Laboratory Medicine Science, Third Military Medical University (Army Medical University), Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yang Xiang, Email [email protected]
Abstract: Burkholderia pseudomallei, the causative agent of melioidosis can be responsible for a wide spectrum of clinical manifestations and heterogeneous prognoses, with a high mortality in the acute onset. We report a case of a deep abdominal abscess with sepsis secondary to melioidosis in a young farmer from a non-high-risk population. Emergency medical treatment was administered according to the detection of serum antibodies against Hcp1, the results of which provided etiological evidence of B. pseudomallei infection for the timely and properly antimicrobial therapy in the absence of direct evidence of melioidosis. To our knowledge, this is the first reported case of serodiagnosis of acute exacerbation of melioidosis in China.
Keywords: melioidosis abscess, serodiagnosis, Burkholderia pseudomallei, antibody detection, Hcp-1
Introduction
Melioidosis is a potentially life-threatening infectious disease caused by Burkholderia pseudomallei, which is prevalent in southest Asia and northern Australia. In China, it is endemic in sub tropical area such as Hainan.1,2 The disease is transmitted by contact with contaminated soil or water through percutaneous inoculation, aerosol inhalation, ingestion of contaminated water or food. Person-to-person mode of transmission is rare and till date, sexual transmission of melioidosis remains unproven.3 It often presents as subclinical infections, asymptomatic or minor localized abscesses, severe pneumonia, and fulminant sepsis.4 The most common risk factors include diabetes mellitus, alcoholism, chronic diseases, long-term steroid use and immunosuppression, and exposure to environmental contaminants.5 The characteristics of diverse clinical symptoms, high fatality, and recurrence if not treated regularly bring great difficulty to clinical diagnosis and treatment.6 Early and accurate diagnosis is essential to improve the ability of clinicians to provide timely and appropriate therapy for serious infections, because B. pseudomallei is intrinsically resistant to many antibiotics used for empirical treatment.7 Empirical antibiotics may carry a risk of resistance to bacteria other than B. pseudomallei, even in suspected cases with high risk factors in endemic areas. Bacterial culture from a specimen is considered as an imperfect gold standard for laboratory diagnosis of B. pseudomallei infection, taking 3–7 days and requiring a bio-safety Level 2+ laboratory.8 The current standard serological assay is the indirect hemagglutination assay (IHA), but the rapid onset and high mortality of acute melioidosis require a more sensitive serological diagnostic method at the time of presentation. Serodiagnosis, based on the detection of serum antibodies against B. pseudomallei specific antigen hemolysin co-regulated protein 1 (Hcp1), can provide etiological evidence to institute appropriate antibiotic therapy. In particular, it has demonstrated an excellent ability to detect blood culture-negative melioidosis sepsis that may otherwise be difficult to find. Here, we report a case of a deep abdominal abscess with unknown pyrexia in a non-high-risk patient caused by B. pseudomallei, and hope to raise awareness of early and accurate diagnosis supported by serological detection.
Case Report
A 30-year-old male Sanya local farmer with symptoms of emaciation (unintentional loss of 3 kg in 1 month), left lower abdominal pain of unknown cause associated with posture and aggravated by turning, went to the nearby health service center for medical treatment with no apparent improvement. Five days later, on 7th July 2021 (Day 1), he was admitted to Sanya People’s Hospital with fever of unknown origin (Tmax 38°C) and complications of hypoproteinemia, electrolyte imbalance and hyperglycemia (Table 1). Medical history: denied hepatitis, tuberculosis, hypertension, diabetes, heart disease, cancer, etc. On 8th July (Day 2), the patient underwent a computed tomography (CT) plain scan of the upper abdomen, which revealed the enlarged spleen with low-density from the splenic and left psoas major, showing a possible abscess with inflammatory exudate (Figure 1). Spleen puncture was not performed due to the poor location of the abscess and the poor patient compliance. The patient was started on symptomatic treatment for sepsis and hyperglycemia. However, the patient deteriorated rapidly and remained febrile with worsening abdominal pain and tendency to ketoacidosis. Cefoperazone-tazobactam was promptly administered to the patient based on the detection of serum anti- Hcp1 antibodies to B. pseudomallei, which were determined to be strongly positive for IgG strip (Figure 2). After intravenous antibiotic and supportive therapy, the relief of symptoms on 16th July (Day 10) provided the window of opportunity for the ultrasound-guided puncture aspiration of the left psoas major abscess. The lesion recovered well on the second day after the abscess was aspirated. The diagnosis of splenic and psoas major abscess due to melioidosis was finally confirmed on 20th July (Day 14) by pus culture as shown in Figure 3 (blood cultures taken prior to antibiotics were negative), and anti-infective therapy was continued. On 27th July (Day 21) the patient gradually improved from sepsis with stable blood glucose. Inflammatory indicators returned to normal, lesion exudation decreased, and the patient was discharged from hospital on oral cefixime eradication therapy for TMP-SMZ resistance. Follow-up imaging with contrast-enhanced abdominal CT on 20th October 2021 (3 months after discharge) showed abscess resolution.
 |
Table 1 Laboratory Data on Admission |
 |
Figure 1 CT plain scan of the patient’s abdomen. The red arrow indicates the low-density region, considering possible abscess (left, left psoas major; right, spleen). |
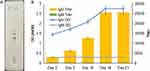 |
Figure 2 Serum antibody detection of the patient. (A) B. pseudomallei IgG showed strongly positive by GICA; (B) Hcp1 IgG and IgM ELISA reactivity (OD) and titre of serum collected after admission. |
Serum Antibody Detection
The antigen reagents for the serological detection, including the recombinant Hcp1 were prepared in our laboratory. Hcp-1 enzyme-linked immunosorbent assay (ELISA), and Hcp-1 gold immunochromatography assay (GICA) were performed to detect IgG and IgM directed against B. pseudomallei in the patient’s serum. The sera were collected at five different time points during the days of hospitalization (Figure 2B). Two replicates of the negative control, two replicates of the positive control, one blank control and two replicates of samples were included in each ELISA. After the reaction, the optical density (OD) was measured at a single wavelength of 450 nm. The antibody titres were determined by ELISA method (the maximum dilution multiple of the antibody with OD value above the cut-off). The OD value of the patient’s first serum IgG was 1.471 (cut-off 0.105) at a titre of 1:3200; the OD value of the fifth sample was 2.761 at a titre of 1:25,600. The OD value of the patient’s first serum IgM was 0.2915 (cut-off 0.29) at a titre of 1:100; the OD value of the fifth sample was 0.23 at a titre of 1:20. For GICA, the diluted serum was added to the strip and read after 15 minutes, only IgG was positive (Figure 2A). According to the Hcp1 ELISA, the patient showed a more than 4-fold increase in IgG titre, while the IgM remained low.
Isolates Identification and Antimicrobial Susceptibility Testing
The patient’s blood was collected and inoculated into both aerobic and anaerobic blood culture bottles and placed in BACT/ALERT® 3D (BioMérieux, France), which showed no growth after 5 days. The aspirated pus from the puncture was thick yellow fluid. Direct smear and Gram stain showed tiny numbers of Gram-negative rods with WBC (Figure 3A). The pus was inoculated onto Columbia blood agar, non-inhibitor chocolate agar, and China blue agar and cultured in a constant temperature incubator in a CO2 enhanced atmosphere at 35°C. After 24 hours of culture, small, smooth, creamy white, neatly edged, milky and slightly sticky colonies were seen on the blood plates. 72 hours later, pale white-yellow, subcircular, dry, wrinkled, and opaque “daisy-like” colonies were observed (Figure 3B–D). No growth was observed on other culture media including anaerobic, mycobacterial, and fungal cultures. The selected single colony stained was showed as Gram--negative bacilli and acid-fast staining was negative. The isolated strain was then subjected to BD Phoenix-100 Automated Microbiology System (BD Biosciences, Franklin Lakes, NJ), and identified as B. pseudomallei. In addition, genomic DNA extracted from the isolated strain using a Bacterial DNA Kit (TIANGEN, Beijing), and amplified using a 16S rDNA Bacterial Identification PCR Kit (Sangon, Shanghai), was sent to BGI company for sequencing. Direct sequencing and phylogenetic analysis of the PCR amplification products showed that the isolate (named BP-HS) was unequivocally clustered with B. pseudomallei (Figure 3E). The scale bar of the evolutionary distance divergence is 0.001.
The strains isolated from this case were also subjected to antimicrobial susceptibility testing using the microbroth dilution method according to CLSI guidelines. The CLSI M45 susceptible/resistant breakpoints were used. Briefly, the isolate was cultured in Columbia blood plate for 24 hours at 35 °C in 5% CO2, and the turbidity was adjusted to 0.5 McFarland, then the bacterial suspension was diluted with Mueller Hinton broth. Ceftazidime, imipenem, cefoperazone-sulbactam (CFP-S) and trimethoprim-sulfamethoxazole (TMP-SMZ) were then applied. After incubation in a 5% CO2 incubator at 35°C for 16–24 hours, the clinical isolate of B. pseudomallei showed a susceptibility and resistance profile with susceptibility to ceftazidime (MIC=2μg/mL), cefoperazone-sulbactam (MIC≤16/8μg/mL), imipenem (MIC≤1μg/mL), and resistance to trimethoprim- sulfamethoxazole (MIC=4/76μg/mL).
Discussion and Literature Review
In this case, despite the lack of blood culture confirmation and the delay in obtaining pus culture, we were able to quickly find the clue of sepsis caused by B. pseudomallei infection based on the antibody directed against the in vivo expressed B. pseudomallei Hcp1, saving the patient in time. Additionally, the significant change of more than 4-fold in anti-Hcp1 IgG titer further identified the infection by retrospective diagnosis. However, in this case, the IgM level measured by Hcp-1 ELISA was always low, whereas it was undetected by Hcp-1 GICA. This was probably due to the properties of IgM test reagents, or that the serum samples were not collected in the infection process for detectable IgM. B. pseudomallei usually invades the epithelial cells of the mucosal surface or skin from the soil and stagnant water in endemic regions.9 Diabetes mellitus is the most common predisposing factor of melioidosis, and more than 50% of the melioidosis patients worldwide are diabetic.10 In this case, the patient was found to be a farmer living in the endemic area, and although he was hyperglycemic on admission, he had normal fasting plasma glucose on discharge, suggesting that he had stress hyperglycemia on admission. The likely exposure of our patient was during the farming activities. Phylogenetic analysis showed that this patient’s isolate appeared to cluster with isolates from Malaysia, probably revealing the origin of B. pseudomallei in the local area. However, whether this isolate is related to B. pseudomallei isolates from the local region should be further investigated.
Most regions of mainland China are outside the endemic range of B. pseudomallei, but the regional distribution of melioidosis in China is asymmetric, with most cases in recent decades occurring in local hospitals in Hainan Province, the most tropical area of the country with limited medical resources. Between 2002 and 2013, with an increasing trend of melioidosis incidence in Hainan, 170 cases of melioidosis were documented, and the most common presentations were pneumonia and bacteraemia.11 Melioidosis is characteristic of various manifestations and is often misdiagnosed as tuberculosis or space-occupying lesion as cancer, which is known as the “great imitator”, causing diagnostic dilemma in prevalent districts.5 Among the 3 billion people living in areas likely to be exposed to B. pseudomallei, the incidence of melioidosis is estimated to be 165,000 cases per year with a predicted mortality of 89,000 per year.6 Due to human activities and environmental changes, as well as improvements in laboratory detection and reporting, the increase in sporadic cases suggests that the disease has spread beyond the tropics and subtropics and that the risk of a melioidosis epidemic is greatly underestimated.12–15 However, the greater public safety risk of latent melioidosis of abscess with subsequent reactivation can occur at any time after the first exposure, which may lead to rapid disease escalation and fatal sepsis.16 Sepsis of unknown origin is a particularly challenging. Given the heterogeneous presentation of melioidosis and the fact that empiric sepsis therapy is likely to exclude the antimicrobial agents used to treat melioidosis, intrinsic resistance of B. pseudomallei would result in failed radical cure, persistent infection or recurrence. Differences in the initial assessment of infection would lead to different clinical outcomes.17 Therefore, timely and effective diagnosis can be life-saving, especially in cases where there has been a delay in confirming the diagnosis from the initial blood culture.
IHA is the most widely used serological test for the detection of antibodies to B. pseudomallei, but its clinical utility has been limited by persistently negativity in culture-confirmed cases of melioidosis, cumbersome performance, and high background seropositivity in endemic locations. ELISA represent a potentially superior method for detecting B. pseudomallei when antigens are carefully selected and properly validated. B. pseudomallei O-polysaccharide (OPS) and capsular polysaccharide (CPS) have long been used as antigens recognized by antibodies in sera of melioidosis patients.18 However, some non-pathogenic, environmental near-neighbor species express OPS moieties that are the same or similar to B. pseudomallei OPS potentially yielding false-positive results. Meanwhile, the predominant antigen of type A OPS could lead to false-negative results when using type A-specific assays to identify individuals exposed to B. pseudomallei strains expressing type B OPS.19 Besides, CPS-based diagnostic tests were reported to have limited sensitivity when used alone. To help address this concern, Hcp1, an effector protein of the type VI secretion system, has been developed as serodiagnostic tools. B. pseudomallei Hcp1 is immunogenic and stimulates high antibody titres in melioidosis patients.20,21 Many studies, including ours, have shown that the Hcp1 ELLISA can provide higher specificity in discriminating between B. pseudomallei and neighboring species even in the endemic area, where the positive cut-off OD of Hcp1 ELLISA was evaluated using the receiver operator characteristic curve.22–24 Although it is still unclear whether the tends of melioidosis antibodies is different than or similar to that of other infectious diseases, which can be used as excellent indicators for disease diagnosis and prognostic assessment. Moreover, to increase the reliability of serological tests, multi-antigen reagents combined detection was better to avoid false negative results.23 In this individual case, the results of serological tests were consistent with expected. However, more samples should be included to further optimize the OD cut-off value according to the local exposure to B. pseudomallei.
To better understand the features of melioidosis in China, we searched the MEDLINE database (https://www.ncbi.nlm.nih.gov/pubmed), which revealed that the early case reports of melioidosis in China were mainly from Hongkong and Taiwan regions since 1983.25 However, the first case reports from mainland China were observed in Guangxi province in 2006.26 A total of 32 cases of melioidosis had been documented in China’s inner regions, including 3 cases we reported,13,14,27 which are summarized in Table 2. The subjects were all males and aged from 17 days to 69 years. 27 cases resided within endemic areas (Hainan, Guangdong, Guangxi). Of the 5 cases living in areas where B. pseudomallei is considered currently absent, 4 returned from endemic areas. The main predisposing risk factors, according to the available literature data, mainly involved diabetes (15/32, 46.9%) and history of travel/exposure (13/32, 40.6%). According to available data, 26 patients were febrile on admission and 27 cases had symptoms of systemic infection. The overall case-fatality rate was 16.7% (5/30, data for two cases unavailable). Most of these cases occurred with imaging findings based on CT scanning (29/32). Even so, the bedside ultrasound is extremely important to facilitate the diagnosis of melioidosis in patient presenting with acute sepsis.28 Pneumonia was reported in 17 cases and abscesses were found in 15 cases. The presence of abdominal abscesses in predicting melioidosis is especially important in areas where melioidosis is endemic.29 The most commonly used antibiotics were TMP-SMZ (15/25), Ceftazidime (11/25) and Imipenem (11/25). Microorganisms were initially misidentified by an automated microbiology system in 5 cases. Diagnosis was delayed in almost all of the cases because the culture usually takes time to confirm. However, in none of the cases was antibody detection used to perform serodiagnosis for evidence-based effective treatment. Lack of medical resources in endemic areas and low awareness in non-endemic areas, make diagnosis difficult. Moreover, reactivation of latent melioidosis may represent as a source of infection in non-endemic areas and is responsible for causing severe opportunistic infections with a high mortality rate in susceptible populations. Even in non-resource-limited settings, the reported mortality of acutely diagnosed melioidosis ranges from 9–18%.30 Thus, the insufficient knowledge of melioidosis diagnosis in both endemic and non-endemic regions, makes it widespread as an emerging public health problem.
 |
Table 2 Characteristics of the Melioidosis Case Reports in the Inner Regions of China |
Conclusion
We report a case of deep abdominal abscess associated with sepsis caused by B. pseudomallei in a young man. In this case, the patient’s condition deteriorated dramatically, and no underlying disease was found other than stress hyperglycaemia on admission. Exacerbation of a visceral organ abscess can be rapidly fatal. Given the strategy of mitigating the potential risk, the detection of serum antibodies specific to B. pseudomallei using an Hcp1-based assay reinforces the need to improve diagnostic capabilities in melioidosis management when the other diagnostic tests for melioidosis were helpless. Moreover, because of the risk of exposure to laboratory staff, clinical laboratories may be advised to perform serological testing on suspected isolates before referring them to a professional bio-safety laboratory for more definitive testing. Furthermore, with the increasing number of melioidosis cases reported in mainland China, especially in those without a travel history, physicians and laboratories in both endemic and non-endemic areas should be aware of this clinical entity and the diagnostic challenges. We suggest the use of specific antibody detection for timely serodiagnosis of unexplained abscesses with a tendency to deteriorate, especially in the search for etiological clues to improve clinical outcomes by early implementation of appropriate therapeutic interventions.
Informed Consent and Ethics Approval
Patient provided informed consent for the case details and images to be published. No ethics committee approval was required for this study as the data had been analyzed in a retrospective manner.
Patient Consent and Ethics Statement
Patient provided informed consent for the case details and images to be published. No ethics committee approval was required for this study as the data had been analyzed in a retrospective manner.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was funded by National Natural Science Foundation of China (81601832), Natural Science Foundation of Hainan Province (820QN429), and Technological Innovation Foundation of Army Medical University (2019XYY02).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zheng X, Xia Q, Xia L, Li W. Endemic melioidosis in Southern China: past and present. Trop Med Int Health. 2019;4(1):39. doi:10.3390/tropicalmed4010039
2. Yang S. Melioidosis research in China. Acta Trop. 2000;77(2):157–165. doi:10.1016/S0001-706X(00)00139-X
3. Chang CY, Lau NLJ, Currie BJ, Podin Y. Disseminated melioidosis in early pregnancy - an unproven cause of foetal loss. BMC Infect Dis. 2020;20(201):4. doi:10.1186/s12879-020-4937-8
4. Mao XH, Lin R, Fang Y. Expert consensus on diagnosis and treatment of melioidosis. Chin J Infect Dis. 2022;40(10):7.
5. Wiersinga WJ, Currie BJ, Peacock SJ. Melioidosis. N Engl J Med. 2012;367(11):1035–1044. doi:10.1056/NEJMra1204699
6. Limmathurotsakul D, Golding N, Dance DA, et al. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol. 2016;1(1):1–5. doi:10.1038/nmicrobiol.2015.8
7. Rhodes KA, Schweizer HP. Antibiotic resistance in Burkholderia species. Drug Resist Updat. 2016;28:82–90. doi:10.1016/j.drup.2016.07.003
8. Hemarajata P, Baghdadi JD, Hoffman R, Humphries RM, Kraft CS. Burkholderia pseudomallei: challenges for the clinical microbiology laboratory. J Clin Microbiol. 2016;54(12):2866–2873. doi:10.1128/JCM.01636-16
9. Wiersinga WJ, van der Poll T, White NJ, et al. Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei. Nat Rev Microbiol. 2006;4(4):272–282. doi:10.1038/nrmicro1385
10. Wiersinga WJ, Virk HS, Torres AG, et al. Melioidosis. Nat Rev Dis Primers. 2018;4(1):17107. doi:10.1038/nrdp.2017.107
11. Fang Y, Chen H, Li Y-L, et al. Melioidosis in Hainan, China: a restrospective study. Trans R Soc Trop Med Hyg. 2015;109(10):636–642. doi:10.1093/trstmh/trv065
12. Gee JE, Bower WA, Kunkel A, et al. Multistate outbreak of melioidosis associated with imported aromatherapy spray. N Engl J Med. 2022;386(9):861–868. doi:10.1056/NEJMoa2116130
13. Fang Y, Zhu X, Chen H, Mao XH. Fatal melioidosis in a newborn from Hainan, China. Am J Trop Med Hyg. 2016;95(2):444–446. doi:10.4269/ajtmh.15-0899
14. Kong Z, Fang Y, Zhang M, et al. Melioidosis acquired by a traveler from Papua New Guinea. Travel Med Infect Dis. 2016;14(3):267–270. doi:10.1016/j.tmaid.2015.12.010
15. Xiao L, Zhou T, Chen J, et al. Paravertebral abscess and bloodstream infection caused by Burkholderia pseudomallei after acupuncture: a case report. BMC Complement Med Ther. 2022;22(1):95. doi:10.1186/s12906-022-03563-8
16. Patterson MC, Darling CL, Blumenthal JB. Acute melioidosis in a soldier home from South Vietnam. JAMA. 1967;200(6):447–451. doi:10.1001/jama.1967.03120190073010
17. Chien JM, Saffari SE, Tan AL, Tan TT. Factors affecting clinical outcomes in the management of melioidosis in Singapore: a 16-year case series. BMC Infect Dis. 2018;18(1):482. doi:10.1186/s12879-018-3393-1
18. Suttisunhakul V, Wuthiekanun V, Brett PJ, et al. Development of rapid enzyme-linked immunosorbent assays for detection of antibodies to Burkholderia pseudomallei. J Clin Microbiol. 2016;54(5):1259–1268. doi:10.1128/JCM.02856-15
19. Win ZZ, Phokrai P, Aung Z, et al. Use of rapid enzyme-linked immunosorbent assays for serological screening of melioidosis in Myanmar. Am J Trop Med Hyg. 2018;98(5):1300–1302. doi:10.4269/ajtmh.17-0791
20. Wagner GE, Föderl-Höbenreich E, Assig K, et al. Melioidosis DS rapid test: a standardized serological dipstick assay with increased sensitivity and reliability due to multiplex detection. PLoS Negl Trop Dis. 2020;14(7):e0008452. doi:10.1371/journal.pntd.0008452
21. Phokrai P, Karoonboonyanan W, Thanapattarapairoj N, et al. A rapid immunochromatography test based on Hcp1 is a potential point-of-care test for serological diagnosis of melioidosis. J Clin Microbiol. 2018;56(8):10–1128. doi:10.1128/JCM.00346-18
22. Zhang MJ, Hu ZQ, Xia YP, et al. Recombinant expression and immunological characterization of hemolysin coregulated protein 1, Burkholderia pseudomallei type VI secretion system protein. J Third Mil Med Univ. 2020;42(23):2296–2301.
23. Amornchai P, Hantrakun V, Wongsuvan G, et al. Evaluation of antigen-detecting and antibody-detecting diagnostic test combinations for diagnosing melioidosis. PLoS Negl Trop Dis. 2021;15(11):e0009840. doi:10.1371/journal.pntd.0009840
24. Pumpuang A, Dunachie SJ, Phokrai P, et al. Comparison of O-polysaccharide and hemolysin co-regulated protein as target antigens for serodiagnosis of melioidosis. PLoS Negl Trop Dis. 2017;11(3):e0005499. doi:10.1371/journal.pntd.0005499
25. So SY, Chau PY, Leung YK, et al. Successful treatment of melioidosis caused by a multiresistant strain in an immunocompromised host with third generation cephalosporins 1. Am Rev Respir Dis. 1983;127(5):650–654. doi:10.1164/arrd.1983.127.5.650
26. Liu GN, Yang ML, Deng JM, et al. The clinical manifestations of three cases with melioidosis. Zhonghua Jie He He Hu Xi Za Zhi. 2010;33(6):422–426.
27. Chen H, Hu ZQ, Fang Y, et al. A case report: splenic abscess caused by Burkholderia pseudomallei. Medicine. 2018;97(26):e11208. doi:10.1097/MD.0000000000011208
28. Chang CY. Bedside ultrasonography for rapid detection of splenic abscess in melioidosis. Rev Soc Bras Med Trop. 2023;56:e0097. doi:10.1590/0037-8682-0097-2023
29. Chang CY. Burkholderia pseudomallei as the predominant cause of splenic abscess in Kapit, Sarawak, Malaysian Borneo. J Ayub Med Coll Abbottabad. 2023;35(2):348–350. doi:10.55519/JAMC-02-11390
30. Pang L, Harris PNA, Seiler RL, et al. Melioidosis, Singapore, 2003–2014. Emerg Infect Dis. 2018;24(1):140–143. doi:10.3201/eid2401.161449
31. Zong Z, Wang X, Deng Y, Zhou T. Misidentification of Burkholderia pseudomallei as Burkholderia cepacia by the VITEK 2 system. J Med Microbiol. 2012;61(Pt 10):1483–1484. doi:10.1099/jmm.0.041525-0
32. Cai XJ, Huang YJ, Fu YH. A case on acute Burkholderia pseudomallei pericarditis. Chin Med J. 2016;129(18):2256–2257. doi:10.4103/0366-6999.189912
33. Zong Z, Wang X, Deng Y. An imported case of acute melioidosis caused by st881 Burkholderia pseudomallei. Southeast Asian J Trop Med Public Health. 2016;47(2):219–222.
34. Zhan Y, Wu Y, Li Q, Yu A. Neuromelioidosis: a series of seven cases in Hainan province, China. J Int Med Res. 2017;45(2):856–867. doi:10.1177/0300060516685967
35. Huang L, Yang Z, Zhou XP, Wu JR. Burkholderia pseudomallei infection presenting with a lung abscess and osteomyelitis in an adult man: a case report. Medicine. 2018;97(35):e12145. doi:10.1097/MD.0000000000012145
36. Huang WY, Wu G, Chen F, et al. Multi-systemic melioidosis: a clinical, neurological, and radiological case study from Hainan Province, China. BMC Infect Dis. 2018;18(1):649. doi:10.1186/s12879-018-3569-8
37. Li XY, Ke BX, Chen CN, et al. First co-infection case of melioidosis and Japanese encephalitis in China. BMC Infect Dis. 2018;18(1):452. doi:10.1186/s12879-018-3364-6
38. Wu H, Huang D, Wu B, et al. Fatal deep venous thrombosis and pulmonary embolism secondary to melioidosis in China: case report and literature review. BMC Infect Dis. 2019;19(1):984. doi:10.1186/s12879-019-4627-6
39. Yuan Y, Yao Z, Xiao E, et al. The first imported case of melioidosis in a patient in central China. Emerg Microbes Infect. 2019;8(1):1223–1228. doi:10.1080/22221751.2019.1654839
40. Liu Y, Zong Z, Torres AG. Prolonged intermittent fever and massive splenomegaly in a miner working in the tropical jungle, China. PLoS Negl Trop Dis. 2020;14(7):e0008278. doi:10.1371/journal.pntd.0008278
41. Shi L, Chen J, Yi G. Burkholderia pseudomallei was identified in a melioidosis aneurysm using polymerase chain reaction targeting 23S rRNA. Ann Vasc Surg. 2020;68:
42. Wu H, Wang X, Zhou X, et al. Mycotic aneurysm secondary to melioidosis in China: a series of eight cases and a review of literature. PLoS Negl Trop Dis. 2020;14(8):e0008525. doi:10.1371/journal.pntd.0008525
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

