Back to Journals » International Journal of General Medicine » Volume 14
Sero-Prevalence and Associated Factors of Hepatitis B Virus Among Pregnant Women at North West Ethiopia: An Institution-Based Cross-Sectional Study
Authors Demeke G , Ayalneh GM , Shiferaw AA , Toru M , Dilnessa T
Received 18 May 2021
Accepted for publication 14 June 2021
Published 24 June 2021 Volume 2021:14 Pages 2799—2805
DOI https://doi.org/10.2147/IJGM.S320711
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Gebreselassie Demeke, Getachew Mengistu Ayalneh, Abtie Abebaw Shiferaw, Milkiyas Toru, Tebelay Dilnessa
Department of Medical Laboratory Science, College of Health Science, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Milkiyas Toru Email [email protected]
Background: Hepatitis B virus is a public health problem in the world. It is a major cause of chronic hepatitis, cirrhosis, and hepatic cellular carcinoma. The presence of a confirmed HBsAg result is indicative of ongoing HBV infection. This study aims to assess the sero-prevalence and associated factors of the hepatitis B virus among pregnant women in North West Ethiopia.
Methods and Materials: An institution-based cross-sectional study was conducted at Debre Markos Referral Hospital from January to July 2017. A consecutive 338 pregnant women attending the antenatal clinic were included. A structured questionnaire was used to assess hepatitis B virus infection associated factors and some socio-demographic characteristics. A 5 mL of venous blood was collected from each study participant and plasma was separated and analyzed using a rapid HBsAg kit and further confirmed by double sandwich ELISA. The data were analyzed using SPSS software version 24.
Results: The mean age of the study participants was 27 (SD ± 4.75) years. The sero-prevalence of hepatitis B virus in pregnant women was 28 (8.3%). Body tattooing practice (AOR = 4.94 95% CI, 1.87– 13.0), multi-partner sexual intercourse (AOR = 4.48 95% CI, 1.89– 10.5) and family hepatitis B history (AOR = 7.40 95% CI, 2.23– 24.5) were statistically significantly associated with HBV infection (p = 0.001).
Conclusion: The prevalence of hepatitis B infection is very high among pregnant women in the study area. Awareness creation on modes of transmission and early screening of all pregnant women attending antenatal care must be strengthened to minimize and control infection.
Keywords: prevalence, pregnant women, hepatitis B virus, ELISA, Ethiopia
Background
Hepatitis B virus (HBV) is an enveloped virus with a viral genome of partially double-stranded circular DNA which belongs to the family Hepadnaviridae.1,2 HBV causes acute and chronic infections of the liver. It is a major cause of chronic hepatitis, cirrhosis, and hepatic cellular carcinoma. HBV infection in pregnancy comes with attendant effects on both mother and child.3 It has been reported that 10–20% of HBsAg-positive pregnant women transmit the virus to their babies, and women who are positive for both HBsAg and HBeAg have a nearly 100% chance of transmitting HBV to their newborns at birth. Up to 90% of the newborns born to these mothers go on to develop chronic hepatitis B if they do not receive hepatitis B immune globulin and hepatitis B vaccine at birth.4
There are three possible routes of transmission of HBV from infected mothers to infants: Trans-placental transmission of HBV in utero natal transmission during delivery or postnatal transmission during care of an infant or through breast milk. In patients with acute hepatitis B infection, vertical transmission occurs in up to 10% and 80−90% of neonates when infection occurs in the first and third trimester, respectively.4,5 Perinatal transmission mainly occurs through maternal blood and body fluid contact.6,7
The main intervention to reduce hepatitis B infection is by increasing the coverage of infant vaccination. Vaccination reduces the risk of developing hepatitis B infection among infants of hepatitis B-positive mothers by 3.5 times.8,9
At least one serologic marker is present during the different phases of HBV infection. The presence of a confirmed HBsAg result is indicative of ongoing HBV infection, so all HBsAg-positive persons should be considered infectious. In newly infected persons, HBsAg is the only serologic marker detected during the first 3–5 weeks after infection, and it persists for variable periods at very low levels. The average time from exposure to the detection of HBsAg is 30 days (range: 6–60 days). Chronic HBV infection occurs when HBsAg persists for >6 months in the presence of HBeAg or anti-HBc or detection of IgG-anti-HBc, whereas acute HBV infection occurs within 6 months of infection. The possible risk factors for hepatitis virus infections are intravenous drug use, blood transfusion, multi-sexual practice, traditional practice, mother to child transmission, etc.10–14 Ethiopia is one of the sub-Saharan countries with a high endemicity of HBV. But the diagnosis (screening) of pregnant mothers during attending antenatal care clinics with highly sensitive diagnostic tools is not common in Ethiopia. Additionally, to our knowledge there is no published data on burden of hepatitis B infection among pregnant mothers in the study area. Therefore, this study attempted to assess the sero-prevalence and associated risk factors of hepatitis B virus among pregnant women at Debre Markos Referral Hospital.
Materials and Methods
Study Area, Design and Period
The study was conducted with women attending antenatal care clinic (ANC) at Debre Markos Referral Hospital (DMRH) located in Debre Markos town, the capital of East Gojjam Zone. DMRH is a tertiary level hospital that provides services for East Gojjam Zone and surrounding areas. A hospital-based cross-sectional study design was employed among pregnant women attending antenatal care clinic from January to July 2017.
Study Population
All pregnant women who visited ANC at Debre Markos Referral Hospital during the study period and fulfilled selection criteria were our source populations. All pregnant women with confirmed pregnancy by urine HCG test and ultrasound and attending ANC for the first visit were included and pregnant women who were critically sick and unable to respond to questions were excluded from the study.
Sample Size Determination and Sampling Technique
The sample size for the study was determined by using a single population proportion formula. With the assumption of 95% confidence interval, the previous prevalence rate (p = 7.8%) from a study conducted in Hawassa, South Ethiopia15 and by considering a 10% non-response rate, a total of 338 pregnant women were consecutively included in this study.
Data Collection
Data on socio-demographic characteristics (age, residence, occupation, educational status and marital status) and associated factors for HBV infection (trimester, previous delivery place, abortion, history of hospital admission, history of surgical procedure, history of blood transfusion, sharp injury, accidental needle stick injuries, splash of body fluids, family history of hepatitis B infection, genital mutilation, tooth extraction, body tattooing, intravenous drug use, history of multiple sexual practice, hepatitis B vaccination and blood group type) were collected by trained nurses using a structured questionnaire.
Blood Specimen Collection and Processing
Five milliliters (5mL) of venous blood was drawn from each study participant under aseptic conditions in disposable vacutainer tubes by laboratory technicians. Then collected blood was allowed to clot for 30 minutes under room temperature. The clotted blood specimen was centrifuged at 3000 revolutions per minute (RPM) for 10 minutes to separate serum. The rapid test was performed using hepatitis B rapid test kit from separated serum and the remaining serum was collected in Eppendorf tubes and stored at −20°C at Debre Markos Referral Hospital and transported to Debre Markos blood bank in a cold box to confirm by the gold standard test (enzyme -linked immuno-sorbent assay (ELISA) test).
Laboratory Detection of HBsAg
Rapid HBsAg detection was done using a SD Bioline HBsAg one-step hepatitis B virus test strip (Abbott, China) following manufacturers instruction. The test has sensitivity and specificity of greater than 99%. The 100 μL of serum was added to the test device left at room temperature for 20 minutes. The serum sample reacts with the coated dye conjugate (mouse anti-HBsAg antibody colloidal gold conjugate) that was coated in the test strip. Then the mixture reacts by capillary action with anti-HBsAg antibodies on the membrane. The presence of a red band indicates a positive result while its absence indicates a negative result.
Rapid HBsAg test result was further confirmed by using the Dialab® HBsAg ELISA kit (DIALAB, Wiener Neudorf, Austria), which has a sensitivity of 100% and specificity of 99.87% and uses an antibody sandwich ELISA method.
Data Quality Assurance
To ensure the quality of data, the data collectors were trained and the instruments was also pre-tested on at least 5% of the sample size prior to actual data collection. Standard operating procedures were strictly followed during blood specimen collection, transportation, storage and analytical process. Storage conditions and expired date of reagents were checked before use. Quality control test was done before each step in laboratory tests and the necessary modification was done based on the findings. The principal investigator and supervisors frequently supervised the data collection process by checking completeness of the required type of data to correct faults, if any, on the site of data collection. The data collection form (questionnaire) was checked for completeness and consistency before data entry by the principal investigator.
Data Analysis
Data was double-entered into Epi data software version 4.2 and exported to SPSS software version 24 to compute statistical analysis. Chi-square and bivariate and multivariate logistic regressions were used to determine the association between associated factors and the outcome variables. The odds ratio (OR) and 95% confidence intervals (CI) were calculated. Finally, variables with p<0.05 were considered statistically significant. The data were expressed by tables.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 338 pregnant women participated in this study. The mean age of study participants was 27 (SD ± 4.75) years, ranging 15 to 46 years. The age category distributions showed that the highest number of participants, 58.3% (197/338), were in the age group of 25–34 years. About 69.5% (235/338) of study participants were from an urban setting and 20.7% (70/338) cannot read and write. The majority 81.4% (275/338) were married and 32.8% (111/338) were governmental employees (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Pregnant Women Attending Antenatal Care at Debre Markos Referral Hospital, Debre Markos, Ethiopia, January to July 2017 |
Sero-Prevalence of Hepatitis B Virus Infection
Among 338 pregnant women attending antenatal care at Debre Markos Referral Hospital the overall prevalence of hepatitis B virus infection was 8.3% (28/338). The highest prevalence, 10.6% (22/207), was seen among pregnant women at third trimester and there was a 10.9% (5/46) prevalence among single mothers (Table 1).
Comparison of Rapid HBsAg Test Result with ELISA Test Result
Out of 338 blood samples tested on rapid HBsAg test kit, 26 samples were positive and 321 samples were negative for HBsAg. On further testing for confirmation with ELISA, 3 false positive and 5 false negative samples were detected (Table 2).
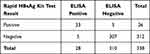 |
Table 2 Comparison of Rapid HBsAg Kit Test with ELISA Test Result |
Factors Associated with Hepatitis B Virus Infection
The results of multivariate logistic regression analysis showed that there is no statistically significant difference between HBV infection and socio-demographic and some clinical characteristics such as age, residence, occupation, level of education, trimester, abortion history, blood contamination, sharp material injury and history of blood transfusion (p-value >0.05). However, other variables such as tattooing, multi-partner sexual intercourse and family history of HBV infection were significantly associated with HBV sero-status (p <0.05). Pregnant women who had traditional tattooing practice had five times higher risk of being sero-positive for HBV infection than pregnant women who had not practiced tattooing (AOR = 4.94, 95% CI, 1.87–13.0, p = 0.001). Regarding multi-partner sexual intercourse, pregnant women who had multi-partner sexual intercourse were almost five times more likely to be sero-positive for HBV infection than those pregnant women who had not (AOR = 4.48; 95% CI, 1.89–10.5; p = 0.001). Based on family history of hepatitis B, study participants who had family history of HBV infection were seven times more likely to be sero-positive for HBV than those who had no history (AOR = 7.40; 95% CI, 2.23–24.5; p = 0.001) (Table 3).
 |
Table 3 Risk Factors Associated with Sero-Prevalence of Hepatitis B Virus Among Pregnant Women Attending ANC at the Debre Markos Referral Hospital, Debre Markos, Ethiopia, July 2017 |
Discussion
HBV infection is one of the serious public health problems worldwide.16 Based on HBsAg carrier, WHO categorizes hepatitis B endemicity into high endemicity, intermediate endemicity and low endemicity.9
In this study the overall prevalence of hepatitis B virus among pregnant women was 8.3%, which is categorized as high endemicity.9 This finding is in line with the study conducted in Gambia and Mali where the sero-prevalence of hepatitis B virus was 9.2%17 and 8%,18 respectively. But our finding is higher than other studies conducted in Tigray 5.5%,19 in Debre Tabor hospital 5.3%,20 and in Gondar 7.3%.21 In contrast to our finding, studies from different countries indicated that the hepatitis B virus prevalence was higher in Ghana 12.3%,12 in Uganda 11.8%22 and in Yemen 10.8%.23 The possible explanation for variations in the prevalence of HBV infection within different parts of the world might be due to differences in socio-cultural practice, geographical area, laboratory technique used and test kit sensitivity.
In this study, pregnant women who had multi-partner sexual intercourse were almost five times more likely to be positive for HBV infection compared to those pregnant women who had not (AOR = 4.48; 95% CI, 1.89–10.5; p = 0.001). This is similar with study findings from Tigray,19 Bahirdar24,25 and Nigeria.11 Hepatitis is usually transmitted through blood and body fluid contact with an infected person. Semen contains high amounts of virus, so the virus can be easily transmitted.
In our study, hepatitis B virus infection is strongly associated with family history of HBV infection (AOR = 7.40; 95% CI, 2.23–24.5; p = 0.001). Close contact with hepatitis B virus-infected individuals within family members may result in contamination of family members through various ways. Our study finding is concordant with most previous studies from Arba Minch26 and Tigray.19
In our study, a traditional practice, body tattooing, is also significantly associated with HBV infection in our study area. A similar finding with our study result is reported from a previous study from Bahir Dar.24 This may be due to sharing a single sharp material for different people without disinfection and sterilization. Similarly, unvaccinated individuals are at higher risk for HBV infection if they are tattooed under unsterile conditions.27 However, there was no significant association observed between previous history of abortion, sharp material injury, blood transfusion and HBsAg sero-status (p >0.05) in our study.
Conclusion
The findings of this study indicated the high prevalence of hepatitis B virus infection among pregnant women attending antenatal care clinic in the study area. Having unprotected multiple partner sexual intercourse, family history of HBV infection and traditional tattooing practice were significantly associated with HBV infection. Therefore, awareness creation on modes of transmission and early screening of all pregnant women attending antenatal care must be strengthened to minimize and control the spread of infection.
Abbreviations
ANC, antenatal clinic; DNA, deoxyribo nucleic acid; ELISA, enzyme-link immunosorbent assay; HBsAg, hepatitis B surface antigen; HBV, hepatitis B virus.
Data Sharing Statement
Research data can be presented upon a reasonable request.
Ethical Approval and Consent to Participate
Ethical approval of the study was obtained after the study protocol was reviewed and approved by Debre Markos University, College of Health Science Research Ethics Review Committee. An official letter of cooperation obtained from College of Health Science was submitted to Debre Markos Referral Hospital and permission was secured from hospital administration. Written consent was taken after explaining the purpose and importance of the study to each participant. For participants under 18 years old, written informed consent was obtained from each participant's parents or guardians prior to inclusion in the study (as per the Declaration of Helsinki 1975, as revised in 2013). Any information concerning the patients was kept confidential and the specimen collected from the patients was only analyzed for the intended purposes.
Acknowledgments
We wish to express our deepest gratitude to Debre Markos University for financial input, materials and other valuable logistic supports that were extremely important for the achievement of this research. Additionally, we would like to thank study participants.
Funding
The research was funded by Debre Markos University. The funder covered materials, reagents, and personnel costs required during the study only.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Seeger C, Mason WS. Hepatitis B virus biology. Microbiol Mol Biol Rev. 2000;64:51–68. doi:10.1128/MMBR.64.1.51-68.2000
2. Uyar Y, Cabar C, Balci A. Seroprevalence of Hepatitis B virus among pregnant women Northern Turkey. 2009.
3. Pennap G, Osanga E, Ubam A. Seroprevalence of hepatitis B surface antigen among pregnant women attending antenatal clinic in federal medical center Keffi, Nigeria. Res J Med Sci. 2011;5:80–82. doi:10.3923/rjmsci.2011.80.82
4. Apuzzio J, Block JM, Cullison S, et al. OBSTETRICS REPORT-Chronic Hepatitis B in pregnancy-a workshop consensus statement on screening, evaluation, and management, part 1. Female Patient. 2012;37:22.
5. American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 86: viral hepatitis in pregnancy. Obstet Gynecol. 2007;110:941. doi:10.1097/01.AOG.0000263930.28382.2a
6. World Health Organization. Preventing Mother-To-Child Transmission of Hepatitis B: Operational Field Guidelines for Delivery of Birth Dose of Hepatitis B Vaccine. World Health Organization; 2006.
7. Lavanchy D, Kane M. Global epidemiology of hepatitis B virus infection. In: Hepatitis B Virus in Human Diseases. Springer; 2016:187–203.
8. World Health Organization. Practices to Improve Coverage of the Hepatitis B Birth Dose Vaccine. World Health Organization; 2012.
9. Nelson NP, Easterbrook PJ, McMahon BJ. Epidemiology of hepatitis B virus infection and impact of vaccination on disease. Clin Liver Dis. 2016;20:607–628. doi:10.1016/j.cld.2016.06.006
10. Hoofnagle JH, Di Bisceglie AM. Serologic diagnosis of acute and chronic viral hepatitis. In: Seminars in Liver Disease. © 1991 by Thieme Medical Publishers, Inc.; 1991:73–83.
11. Obi S, Onah H, Ezugwu F. Risk factors for hepatitis B infection during pregnancy in a Nigerian obstetric population. J Obstet Gynaecol. 2006;26:770–772. doi:10.1080/01443610600963986
12. Candotti D, Danso K, Allain J-P. Maternofetal transmission of hepatitis B virus genotype E in Ghana, west Africa. J Gen Virol. 2007;88:2686–2695. doi:10.1099/vir.0.83102-0
13. Belyhun Y, Maier M, Mulu A, Diro E, Liebert UG. Hepatitis viruses in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2016;16:761. doi:10.1186/s12879-016-2090-1
14. Amsalu A, Ferede G, Eshetie S, Tadewos A, Assegu D. Prevalence, infectivity, and associated risk factors of hepatitis B virus among pregnant women in Yirgalem hospital, Ethiopia: implication of screening to control mother-to-child transmission. J Pregnancy. 2018;2018. doi:10.1155/2018/8435910
15. Metaferia Y, Dessie W, Ali I, Amsalu A. Seroprevalence and associated risk factors of hepatitis B virus among pregnant women in southern Ethiopia: a hospital-based cross-sectional study. Epidemiol Health. 2016;38:38. doi:10.4178/epih.e2016027
16. Adibi P, Akbari L, Kahangi LS, Abdi F. Health-state utilities in liver cirrhosis: a cross-sectional study. Int J Prev Med. 2012;3:S94.
17. Bittaye M, Idoko P, Ekele BA, Obed SA, Nyan O. Hepatitis B virus sero-prevalence amongst pregnant women in the Gambia. BMC Infect Dis. 2019;19:19. doi:10.1186/s12879-019-3883-9
18. MacLean B, Hess RF, Bonvillain E, et al. Seroprevalence of hepatitis B surface antigen among pregnant women attending the Hospital for Women & Children in Koutiala, Mali. South Afri Med J. 2012;102.
19. Araya Mezgebo T, Niguse S, Gebrekidan Kahsay A, Hailekiros H, Berhe N, Asmelash Dejene T. Hepatitis B virus infection and associated risk factors among pregnant women attending antenatal care in health facilities of Tigray, Northern Ethiopia. J Med Virol. 2018;90:503–509. doi:10.1002/jmv.24987
20. Walle F, Asrat D, Alem A, Tadesse E, Desta K. Prevalence of hepatitis B surface antigen among pregnant women attending antenatal care service at Debre-Tabor Hospital, Northwest Ethiopia. Ethiop J Health Sci. 2008;17:13–20.
21. Tiruneh M. Seroprevalence of multiple sexually transmitted infections among antenatal clinic attendees in Gondar Health Center, northwest Ethiopia. Ethiop Med J. 2008;46:359–366.
22. Bayo P, Ochola E, Oleo C, Mwaka AD. High prevalence of hepatitis B virus infection among pregnant women attending antenatal care: a cross-sectional study in two hospitals in northern Uganda. BMJ Open. 2014;4:e005889. doi:10.1136/bmjopen-2014-005889
23. Murad EA, Babiker SM, Gasim GI, Rayis DA, Adam I. Epidemiology of hepatitis B and hepatitis C virus infections in pregnant women in Sana’a, Yemen. BMC Pregnancy Childbirth. 2013;13:127. doi:10.1186/1471-2393-13-127
24. Zenebe Y, Mulu W, Yimer M, Abera B. Sero-prevalence and risk factors of hepatitis B virus and human immunodeficiency virus infection among pregnant women in Bahir Dar city, Northwest Ethiopia: a cross sectional study. BMC Infect Dis. 2014;14:118. doi:10.1186/1471-2334-14-118
25. Gedefaw G, Waltengus F, Akililu A, Gelaye K. Risk factors associated with hepatitis B virus infection among pregnant women attending antenatal clinic at Felegehiwot referral hospital, Northwest Ethiopia, 2018: an institution based cross sectional study. BMC Res Notes. 2019;12:509. doi:10.1186/s13104-019-4561-0
26. Yohanes T, Zerdo Z, Chufamo N. Seroprevalence and predictors of hepatitis B virus infection among pregnant women attending routine antenatal care in Arba Minch Hospital, South Ethiopia. Hepat Res Treat. 2016;2016. doi:10.1155/2016/9290163
27. Jafari S, Buxton JA, Afshar K, Copes R, Baharlou S. Tattooing and risk of hepatitis B: a systematic review and meta-analysis. Can J Public Health. 2012;103:207–212. doi:10.1007/BF03403814
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
