Back to Journals » Infection and Drug Resistance » Volume 15
Septic Shock After Kidney Transplant: A Rare Bloodstream Ralstonia mannitolilytica Infection
Authors Tian X, Jing N, Duan W, Wu X, Zhang C, Wang S, Yan T
Received 10 April 2022
Accepted for publication 29 June 2022
Published 19 July 2022 Volume 2022:15 Pages 3841—3845
DOI https://doi.org/10.2147/IDR.S370170
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Xiangyong Tian,1,* Nan Jing,2,* Wenjing Duan,3 Xiaoqiang Wu,1 Chan Zhang,1 Shanmei Wang,2 Tianzhong Yan1
1Department of Urology, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Henan University People’s Hospital, Zhengzhou, People’s Republic of China; 2Department of Clinical Microbiology, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Henan University People’s Hospital, Zhengzhou, People’s Republic of China; 3Department of the Clinical Research Center, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Henan University People’s Hospital, Zhengzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tianzhong Yan, Department of Urology, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Zhengzhou, Henan Province, 450003, People’s Republic of China, Email [email protected] Wenjing Duan, Department of the Clinical Research Center, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Zhengzhou, Henan Province, 450003, People’s Republic of China, Email [email protected]
Background: Ralstonia mannitolilytica, an emerging opportunistic pathogen, can infect immunocompromised patients but is a rare cause of severe sepsis and septic shock in kidney transplant recipients (KTRs).
Case Presentation: We present a case of septic shock after renal transplant in a 41-year-old male, which was finally proven to be caused by Ralstonia mannitolilytica through blood cultures and mass spectrometric analysis following the negative result of metagenomic next-generation sequencing (mNGS). He was finally cured after the application of sensitive antibiotics (sulfamethoxazole-trimethoprim, amikacin and piperacillin-tazobactam) based on the drug sensitivity test results. The patient had a satisfactory recovery with no complications during a 6-month follow-up period.
Conclusion: This study highlights that Ralstonia mannitolilytica is an easily overlooked cause of septic shock in KTRs requiring a detailed inquiry of medical history with inflammatory markers monitored closely. Traditional blood cultures still should be taken seriously. It also provides a cautionary tale that negative results of mNGS have to be interpreted with caution.
Keywords: Ralstonia mannitolilytica, kidney transplant, sepsis, metagenomic next-generation sequencing, mNGS, blood cultures
Introduction
Ralstonia mannitolilytica (R. mannitolilytica) is one of the most prevalent species of the Ralstonia genus.1 It refers to a gram-negative, oxidase-positive, non-fermentative rods typically distributed in environmental habitats such as water, soil and plants.1–3 The incidence of R. mannitolilytica opportunistic infection is relatively low, but it can cause health lesions, such as pneumonia, abdominal infection, bacteremia, cystic fibrosis infection and meningitis, etc, especially in immunocompromised patients.2,4–8 Two reports have described it as a pathogen of infection in kidney transplant recipients, who need maintenance immunosuppression indefinitely after transplantation to prevent chronic rejection and promote long-term allograft survival. The clinical manifestations of them were mild and they were finally cured after giving sensitive antibiotics, such as cefoperazone-sulbactam or cefepime.9,10 Here, we describe a rare case with rapidly progressive sepsis caused by R. mannitolilytica after kidney transplantation. The pathogen, R. mannitolilytica, was identified by conventional blood culture rather than metagenomic next-generation sequencing (mNGS).
Case Presentation
A 41-year-old male haemodialysis patient underwent a live-related donor kidney transplantation in our hospital. His healthy father aged 64 years volunteered to donate a kidney after a careful evaluation of potential living kidney donors. Both of them were evaluated preoperatively with complete clinical examination and imaging workup showing no surgical contraindication and no signs of inflammation or infection during hospitalization. Standard-dose tacrolimus, mycophenolate mofetil and prednisone were given to the recipient for immunosuppression following the transplant. Although the third-generation cephalosporin (ceftizoxime) was given to prevent infection, the patient experienced transient fever (38 °C) on the first postoperative night. Therefore, routine blood tests and inflammatory indexes were immediately performed and the antibiotic was upgraded to biapenem (0.3g, q8h). However, on the next night, the fever returned and the temperature was as high as 39.5°C after sudden chills. We immediately performed laboratory tests again including blood culture, blood routine, coagulation function, inflammatory indexes and other related tests before administration of dexamethasone (10mg, i.v.). The body temperature lowered somewhat by giving dexamethasone. However, an hour later he suddenly developed chest tightness, dyspnea and altered consciousness. Meanwhile, his blood pressure decreased to 76/40 mmHg, accompanied by tachycardia (140–160 beats/min) and decreased urine output (20 mL/h). Intravenous biapenem antibiotics, albumin and rehydration fluids were given immediately with oxygen support. The patient’s vital signs gradually returned to normal and urine output also improved after 20 minutes of administration.
Immediately afterwards, color Doppler ultrasound showed good blood flow to the transplanted kidney with no significant perinephric effusion. Bleeding disorders were excluded. The laboratory tests were used to continuously monitor the treatment outcomes. The results of tests previous mentioned were timely reported as showed in Table 1. Thus we believed that he was suffering from severe septic shock with suspected pulmonary embolism. In the third postoperative day, the patient underwent a chest computed tomography (CT) to rule out the pulmonary embolism. The maintenance dosages of immunosuppressant were adjusted to the minimum effective dose. And the antibiotics were also empirically adjusted to biapenem (0.3g, q8h), linezolid (0.6g, q12h), and caspofungin (50mg, qd). His blood samples, urine samples and the post-surgical fluids (PSF) samples collected from perirenal surgical drains were sent for mNGS and traditional bacterial culture, respectively. But no clear pathogen was found in results of mNGS on the fifth postoperative day. With the exception of the positive blood culture on sixth postoperative day, all other pathogen tests were negative. The aerobic and anaerobic bottles of all four standard blood culture sets grew R. mannitolilytica (Figure 1). The cultured isolate was confirmed by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS; Bruker, Germany). So we adjusted the antibiotic to compound sulfamethoxazole-trimethoprim (960mg, q8h), amikacin (0.2g, q12h) and piperacillin-tazobactam (4.5g, q8h) according to the results of drug sensitivity tests (Table 2). This regimen was continued for 8 days. Blood cultures were persistently negative for bacterial growth over the period, and the inflammatory indicators (including procalcitonin (PCT), C-reactive protein (CRP), neutrophils, white blood cells, etc.) decreased significantly or returned to normal. The patient was no longer febrile. Then only sulfamethoxazole-trimethoprim (480mg, q12h) was carried on for 3 weeks as consolidation therapy. The patient was cured thereafter. No other infectious foci were found anywhere else in the body. Transient impairment of renal function were associated with hypoperfusion during septic shock and application of large quantity of antibiotics. Fortunately, creatinine levels returned to normal values before hospital discharged on the 27th postoperative day (Table 1). After 6 months of follow-up, all his lab test indicators returned to normal.
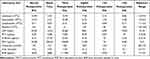 |
Table 1 Laboratory Findings |
 |
Table 2 Susceptibility of Antibiotics to the Ralstonia mannitolilytica Isolate |
Supplementary intensive inquiry of patient’s history after controlling for septic shock revealed that the patient had similar episodes of chills and fever three times during the two-year dialysis period before kidney transplantation. Because of the mild symptoms and fast relief after empirical treatment, the course of the infection did not attracted sufficient attention. The patient did not consider such mild events as important enough to mention to his doctor before transplantation. Considering the potential nosocomial infection, we tested 16 samples from the patient and his surroundings in the hospital, including central venous catheter, skin, drinking water and water cups, etc. Each sample was swabbed by pre-moistened sterile cotton swabs and inoculated into broth medium for incubation. But no R. mannitolilytica was found, indicating that it did not come from these sites. Based on these two points, we believe that R. mannitolilytica may be a chronic colonization state.
Discussion and Conclusions
The species of Ralstonia genus, in order from most to least common, were R. pickettii, R. mannitolilytica, R. solanacearum (Previously Burkholderia pickettii and B. solanacearum), R. insidiosa, and R. syzygii.11 There were some reports caused by R. mannitolilytica, such as cystic fibrosis with infection, pneumonia, bacteremia, dialysis tube infection and burn wound infection, etc.2,5,11 So far, in kidney transplant recipients (KTRs), there are only two reports about R. mannitolilytica infection from urine samples. They showed only mild symptoms of fever and were quickly cured with the application of sensitive antibiotics.9,10 But this is the first case of severe septic shock after kidney transplantation due to hematogenous infection of R. mannitolilytica, considered to be colonizer reactivation after transplant. The colonization may be related to long-term dialysis and the site of colonization may be his former tunneled hemodialysis catheter. Medical water is considered as a high risk factor for R. mannitolilytica infection, and there have been several reports of nosocomial infection outbreaks of R. mannitolilytica due to water contamination.12,13 We tested 16 samples in the surrounding environment of the patient and no R. mannitolilytica was detected, indicating that the bacteria did not come from our hospital and did not spread to the surroundings.
R. mannitolilytica is an opportunistic pathogen. ICU inpatients and immunodeficiency patients are high-risk groups.1 This case was frail after transplantation, and the concurrent application of immunosuppressive agents led to the re-activation of R. mannitolilytica, which caused severe septic shock. So R. mannitolilytica can impell opportunistic infection in immune-compromised patients ensuing from asymptomatic or mildly symptomatic colonization to severely pathogenic forms. Although mNGS has played an important role in the diagnosis of infectious diseases in recent years, especially in rare pathogenic infections,14 it failed to effectively identify R. mannitolilytica this time. We checked the raw data of mNGS, and found that there were 33, 26 and 5 reads of R. mannitolilytica nucleic acid fragments in blood, urine and PSF samples, respectively. Due to the low number of reads, the bacterium did not attract the attention of examiners and was excluded from subsequent analysis. R. mannitolilytica was finally diagnosed by traditional blood culture, suggesting blood culture still plays a huge role in diagnosis infectious disease sometimes.
Daxboeck et al15 showed that there were obvious genotypic and phenotypic differences among R. mannitolilytica strains from different sources, and therefore differences in antibiotic susceptibility. The treatment and management of R. mannitolilytica infection is often challenging, because it is frequently resistant to numerous different types of antibiotics, including several β-lactams, carbapenems and most of the aminoglycosides. It has also been shown in the literature that, R. mannitolilytica may be susceptible to cefepime, ciprofloxacin, sulfanilamide, amikacin, cefoperazone-sulbactam and piperacillin-tazobactam.9,10,15 In this case, drug susceptibility testing showed that R. mannitolilytica was resistant to carbapenems, but sensitive to sulfamethoxazole-trimethoprim, piperacillin-tazobactam and amikacin. Immediately afterwards, we promptly adjusted empiric coverage to sensitive antibiotics and the infection was controlled in time. We treated the patient with the three sensitivity drugs for 8 days and confirmed the significant efficacy with continuous negative blood cultures, significant decrease or reduction to normal in inflammatory indexes (including PCT, CRP, neutrophils, white blood cells, etc.), and no re-fever in the patient. The prolonged use of sulfamethoxazole-trimethoprim alone for three weeks was intended not only to consolidate treatment as a sensitive antibiotic for R. mannitolilytica, but also as a prophylactic measure for pneumocystis carinii pneumonia. In this case, PCT was very high at onset and dropped significantly after effective treatment, so PCT might be helpful in assessing the severity of R. mannitolilytica infection and the treatment efficacy.
This case provides a cautionary tale for working on kidney transplant. Uremic patients should be asked carefully before transplant about the detailed history of prior infections, such as recurrent fever and sudden chills. Heightened alert regarding R. mannitolilytica infection is needed to allow early diagnosis and treatment, especially for live donor kidney transplantation because of its controllability. A negative mNGS result needs to be interpreted with caution. The low yield of mapped reads may cause false-negative mNGS results, even in those culturable pathogens. Traditional blood cultures still need to be taken seriously. In this case, the blood cultures were not performed at the time of the first postoperative fever because it was a transient low fever without accompanying symptoms, which was considered likely to be a physiologic pyrexia after operation. This has taught us a lesson that early postoperative fevers should not be underestimated for KTRs. The combination of the mNGS and traditional methods can increase the detection rate.
In conclusion, this paper reports a case of severe septic shock after kidney transplant caused by R. mannitolilytica infection, which was finally diagnosed by blood culture. For KTRs who suffer from R. mannitolilytica infection, detailed medical history, early detection, timely targeted anti-infection and symptomatic supportive treatment can bring more favorable outcomes.
Ethics Approval and Informed Consent
Ethical approval was granted by Henan Provincial People’s Hospital ethics committee. Written informed consent was obtained from the study participants for publication of this case report and any accompanying images. The transplanted kidney was from the case’s father, and it was donated voluntarily with written informed consent. This study was conducted in accordance with the Declaration of Istanbul.
Funding
This work was supported by the Project of Science and Technology of Henan Province (No. 202102310438), the 23456 Talent Project Foundation of Henan Provincial People’s Hospital (No. ZC23456127), Joint Construction Project of Henan Medical Science and Technology Research Plan (No. LHGJ20210042) and Foundation of Henan Educational Committee (No. 22A320012).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ryan MP, Adley CC. Ralstonia spp.: emerging global opportunistic pathogens. Eur J Clin Microbiol Infect Dis. 2004;33(3):291–304. doi:10.1007/s10096-013-1975-9
2. Lim CTS, Lee SE. A rare case of Ralstonia mannitolilytica infection in an end stage renal patient on maintenance dialysis during municipal water contamination. Pak J Med Sci. 2017;33(4):1047–1049. doi:10.12669/pjms.334.13112
3. Yabuuchi E, Kosako Y, Yano I, et al. Transfer of two Burkholderia and an Alcaligenes species to Ralstonia gen. Nov.: proposal of Ralstonia pickettii (Ralston, Palleroni and Doudoroff 1973) comb. Nov., Ralstonia solanacearum (Smith 1896) comb. Nov. and Ralstonia eutropha (Davis 1969) comb. Nov. Microbiol Immunol. 1995;39(11):897–904. doi:10.1111/j.1348-0421.1995.tb03275.x
4. Xie P, Liu J, Wu L, Liu D. Pulmonary Cavitation: a Hint of Ralstonia mannitolilytica Infection through Imaging. Am J Respir Crit Care Med. 2021;203(12):1569–1570. doi:10.1164/rccm.202009-3616IM
5. Coenye T, Goris J, Spilker T, LiPuma JJ. Characterization of unusual bacteria isolated from respiratory secretions of cystic fibrosis patients and description of Inquilinus limosus gen. J Clin Microbiol. 2002;40(6):2062–2069. doi:10.1128/JCM.40.6.2062-2069.2002
6. Dotis J, Printza N, Orfanou A, et al. Peritonitis due to Ralstonia mannitolilytica in a pediatric peritoneal dialysis patient. New Microbiol. 2012;35(4):503–506.
7. Tu J, Tu L, Jiang Y, et al. Sepsis Due to Bloodstream Ralstonia mannitolilytica Infection After Surgical Treatment of Perianal Abscess: a Case Report. Infect Drug Resist. 2021;14:4441–4445. doi:10.2147/IDR.S329588
8. Vaneechoutte M, De Baere T, Wauters G, et al. One case each of recurrent meningitis and hemoperitoneum infection with Ralstonia mannitolilytica. J Clin Microbiol. 2001;39(12):4588–4590. doi:10.1128/JCM.39.12.4588-4590.2001
9. Mukhopadhyay C, Bhargava A, Ayyagari A. Ralstonia mannitolilytica infection in renal transplant recipient: first report. Indian J Med Microbiol. 2003;21(4):284–286. doi:10.1016/S0255-0857(21)03017-6
10. Boattini M, Bianco G, Biancone L, Cavallo R, Costa C. Ralstonia mannitolilytica bacteraemia: a case report and literature review. Infez Med. 2018;26(4):374–378.
11. Lin TC, Wu RX, Chiu CC, et al. The clinical and microbiological characteristics of infections in burn patients from the Formosa Fun Coast Dust Explosion. J Microbiol Immunol Infect. 2018;51(2):267–277. doi:10.1016/j.jmii.2016.08.019
12. Said M, van Hougenhouck-Tulleken W, Naidoo R, Mbelle N, Ismail F. Outbreak of Ralstonia mannitolilytica bacteraemia in patients undergoing haemodialysis at a tertiary hospital in Pretoria, South Africa. Antimicrob Resist Infect Control. 2020;9(1):117. doi:10.1186/s13756-020-00778-7
13. Shankar M, Rampure S, Siddini V, Ballal HS. Outbreak of Ralstonia mannitolilytica in Hemodialysis Unit: a Case Series. Indian J Nephrol. 2018;28(4):323–326. doi:10.4103/ijn.IJN_77_17
14. Gu W, Deng X, Lee M, et al. Rapid pathogen detection by metagenomic next-generation sequencing of infected body fluids. Nat Med. 2021;27(1):115–124. doi:10.1038/s41591-020-1105-z
15. Daxboeck F, Stadler M, Assadian O, et al. Characterization of clinically isolated Ralstonia mannitolilytica strains using random amplification of polymorphic DNA (RAPD) typing and antimicrobial sensitivity, and comparison of the classification efficacy of phenotypic and genotypic assays. J Med Microbiol. 2005;54(1):55–61. doi:10.1099/jmm.0.45656-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

