Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Self-stigma and quality of life in patients with depressive disorder: a cross-sectional study
Authors Holubova M, Prasko J , Ociskova M , Marackova M, Grambal A, Slepecky M
Received 1 August 2016
Accepted for publication 24 August 2016
Published 19 October 2016 Volume 2016:12 Pages 2677—2687
DOI https://doi.org/10.2147/NDT.S118593
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Michaela Holubova,1,2 Jan Prasko,1 Marie Ociskova,1 Marketa Marackova,1 Ales Grambal,1 Milos Slepecky3
1Department of Psychiatry, Faculty of Medicine and Dentistry, Palacky University Olomouc, University Hospital Olomouc, Olomouc, 2Department of Psychiatry, Hospital Liberec, Liberec, Czech Republic; 3Department of Psychology Sciences, Faculty of Social Science and Health Care, Constantine the Philosopher University, Nitra, Slovak Republic
Background: Self-stigma is a maladaptive psychosocial phenomenon that can affect many areas of patients’ lives and have a negative impact on their quality of life (QoL). This study explored the association between self-stigma, QoL, demographic data, and the severity of symptoms in patients with depressive disorder.
Patients and methods: Patients who met the International Classification of Diseases, 10th revision, research criteria for depressive disorder were enrolled in this cross-sectional study. All outpatients completed the following measurements: the Quality of Life Enjoyment and Satisfaction Questionnaire, the Internalized Stigma of Mental Illness Scale, demographic questionnaire, and the objective and subjective Clinical Global Impression-Severity scales that measure the severity of disorder. A total of 81 depressive disorder patients (with persistent affective disorder – dysthymia, major depressive disorder, or recurrent depressive disorder) and 43 healthy controls participated in this study.
Results: Compared with the healthy control group, a lower QoL was observed in patients with depressive disorder. The level of self-stigma correlated positively with total symptom severity score and negatively with QoL. Multiple regression analysis revealed that the overall rating of objective symptom severity and score of self-stigma were significantly associated with QoL.
Conclusion: This study suggests a lower QoL in patients with depressive disorder in comparison with healthy controls and a negative impact of self-stigma level on QoL in patients suffering from depressive disorders.
Keywords: self-stigma, quality of life, depressive disorder
Introduction
Psychiatric diagnoses are often disappointing news for patients and their families.1 Prejudgment and discrimination by the public against people with psychiatric disorders are common and socially harmful, and they are a part of more general stigmatization. Several biased opinions, emotions, and behaviors cause discrimination against people labeled as mentally ill. It is not surprising that patients often deny the presence of symptoms and delay seeking psychiatric care because of the fear of people’s prejudices and their impact.2 Self-stigma is an adverse psychosocial issue upsetting a considerable number of psychiatric patients.1 Similarly, self-stigma is associated with non-adherence to various medical procedures.3,4 People with a high level of self-stigma agree on the societal preconceptions about individuals with psychiatric disorders and thus are convinced of their inferiority or untreatability of their mental problems.5 Self-stigma frequently leads to dysphoria and decline in self-esteem and quality of life (QoL).6 Social avoidance or other forms of potentially maladaptive behavior are also common. Self-stigma might also lead to suicide.6,7 Self-stigma may also have a deleterious impact on the treatment efficacy in mental disorders.8–13
According to the World Health Organization (WHO), QoL characterizes the individual’s subjective evaluation of physical, psychological, and social areas of life.14,15 Depressive disorder, which is the prominent basis of disability affecting ~350 million people worldwide, is associated with a significant decrease in QoL.15–17 Notably, QoL insufficiencies have been shown to continue beyond the clinical resolution of depressive symptoms,18 retaining patients at an increased possibility of relapse.19 A reduced QoL often corresponds to the severity of depressive symptoms.20 Nevertheless, some investigations have shown that the seriousness of the symptoms explained only a minor amount of the variance in QoL.16,17,21 These results show that measuring only the symptom reduction may not be the best way to gage the efficacy of antidepressant strategies. Despite being gradually documented as an imperative measure of health in medical and psychiatric patients, the QoL of patients with depressive disorder needs more attention in research and clinical efforts.22,23
Self-assessed approaches to measure QoL and health status have been linked to the severity of the disorder, disability, and the development of disorder, and they are now reflected as the fundamental aspect of the process of policy creation, distribution of services, and provision of care.24,25 These evaluations capture a multidimensional vision of a personalized state of well-being and health and therefore incorporate a wide-ranging description of health, as well defined by the WHO.15 Different studies have suggested that self-assessed QoL and health status are modified by various factors including age, education, physical activity, and depressive symptoms.24,26–28
A study by Rapaport et al16 reported that ~63% of patients with major depressive disorder (MDD) and 85% of patients with chronic/double depression (ie, a major depressive episode on top of dysthymia) entering clinical trials had uncompromising QoL deficiencies. Several investigations have shown that impairments in QoL often continue beyond the medical resolution of the depressive symptoms, engaging patients at a higher risk of relapse.18,19 Notably, the severity of depressive symptoms has been found to explain only partially the impairment of QoL.16,18,29–31 Papakostas et al32 reviewed studies concentrating on the relationship between depression and QoL, particularly focusing on the impact of the treatment of depression on QoL.
IsHak et al31 analyzed the complete data of 2,280 adult outpatients with MDD at entry/exit of each level of antidepressant treatments and after 12 months of entry to follow-up from the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial. The QoL was assessed using the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q). Some patients scoring “within-normal” QoL (within 10% of Q-LES-Q community norms) and those with “severely impaired” QoL (>2 SD below Q-LES-Q community norms) were analyzed. At the start of the treatment, only ~3% of the depressive patients experienced “within-normal” QoL. After treatment, significant improvements were identified. However, the percentage of the patients reaching “within-normal” QoL did not go above 30%, with >50% of the patients experiencing “severely impaired” QoL. Although remitted patients had greater improvements compared to non-remitters, 32%–60% of the individuals continued to experience reduced QoL. The 12-month follow-up data revealed that the patients experiencing “within-normal” QoL showed a statistically significant decrease in QoL compared to non-remitters. The authors concluded that symptom-focused treatments of MDD may leave a misleading impression that the patients have recovered when, in fact, they may be experiencing ongoing QoL deficits.
The aim of this study was to measure QoL and self-stigma in outpatients with depressive disorder. The second objective was to find how QoL and self-stigma are related to each other and which clinical and demographic data could influence them. The following three main research hypotheses were defined:
- The probands from the healthy control group will have a higher level of QoL in comparison with the patients with depressive disorder.
- The degree of self-stigma and QoL will be related to demographic data such as age, relationship, family burden, and education.
- The self-stigma and QoL will correlate negatively with each other.
Patients and methods
A total of 25 experienced outpatient psychiatrists, who participated in this study, confirmed the diagnoses using the inclusion and exclusion criteria of the study and ensured the collection of questionnaires from their outpatients who were also treated by them. The study was performed between March 2014 and November 2015. In addressing psychiatrists to collaborate on data collection, a sheet of outpatient psychiatrists in the Czech Republic was compiled. Based on this data sheet and the available email addresses, an application was sent to >200 psychiatrists to participate in the study, of whom 25 participated in the study. Inclusion criteria were a) the diagnosis of depressive disorder according to the criteria of the International Classification of Diseases, 10th revision; b) adult age; c) current mental state was stabilized; d) signing of the consent form; and e) both sexes. Exclusion criteria were acute symptomatology, <18 years of age, current hospitalization, intellectual disability, severe physical illness, and comorbid substance abuse disorder. A physical examination was performed in all outpatients, and they were treated with standard medication for the depressive disorder according to the guidelines and principles of Good Clinical Practice. The controls with acute symptomatology were excluded from the study by the psychiatrists, who knew the patients for a long time. Patients who attended the outpatient psychiatric facilities were in stable condition; thus, according to the psychiatrists, it meant that they had a reduced acute symptomatology, did not require hospitalization, and did not need changes in medication or other therapeutic intervention, and the medication was the same as in the last 3 months. The University Hospital Olomouc ethics committee approved the study. All patients signed an informed consent. The investigation was carried out according to the latest version of the Declaration of Helsinki and the Guidelines for Good Clinical Practice.33 Subjects received no monetary compensation for participation in the study.
Healthy controls were selected from the general population in the Czech Republic using the “snowball technique”.34 Mail was sent to them with a request to fill out the questionnaire (in the case of absence of a history of mental illness or previous examination by a psychiatrist). We asked a group of employees from the University Department of Psychiatry to invite their relatives and friends to participate in the study. Controls anonymously filled out the Q-LES-Q and an anonymous demographic questionnaire with questions about their age, sex, employment, level of education, and past and actual psychiatric or somatic illnesses. No individuals with a history of psychiatric disorder and/or a serious somatic disorder were included. No other personal data were gathered.
Assessment instruments
The patients completed the following questionnaires during the routine psychiatric examination:
- The Q-LES-Q: This questionnaire with 93 items is divided into eight domains to assess.35 The patients assess each domain by choosing one number from a 5-point Likert scale according to their level of satisfaction in the item. The completion takes 20–30 minutes. Patients fill out the domains of physical health, feelings, leisure, household, work, school/study, social relations, general, and a sum of Q-LES-Q. The Czech version of the Q-LES-Q was validated by Müllerova.36 The analyses indicated the high internal consistency (Cronbach’s α=0.8–0.9) and proved the stability of the answers over time (test–retest).36
- The Internalized Stigma of Mental Illness (ISMI) scale: This questionnaire has 29 items that evaluate five areas of the internalized stigma.37 The scale assesses five facets of self-stigma, alienation, perceived discrimination, stereotype endorsement, social withdrawal, and resistance to the stigma.37–39 Internal consistency of the scale is excellent.37 The same goes for the Cronbach’s α of the Czech translation of the scale (α=0.91), which also has a very good reliability analyzed by the split-half method (Spearman–Brown coefficient =0.93) and test–retest after 3 weeks of the first measurement (r=0.90, P<0.001).40
- Clinical Global Impression (CGI): This scale represents a global assessment of severity of psychopathology.41 The CGI severity score is based on symptoms, behaviors, and functioning over the last 7 days, both reported and observed. It is evaluated on the 7-point scale extending from 1 (normal) to 7 (most extremely ill). The evaluation is performed by the professional rater (psychologist or psychiatrist) using the objective version (objCGI) of the scale. The patient also assesses himself/herself by the subjective version (subCGI) of the scale, which includes seven levels of severity of the psychopathology.41 The measure may be completed by a physician (objCGI) or a patient (subCGI). Internal consistency of the scale is satisfactory.42 The intra-class correlations lie in the interval 0.88–0.92.
- Demographic questionnaire: This questionnaire concerns sex, age, employment status, education, marital status, heredity, type of pension, the number of siblings, the age at the onset of disorder, the length of attendance at outpatient clinic, duration of attendance at the outpatient clinic, the number of psychiatric hospitalizations, and current medication.
Statistical analysis
The statistical package software Prism3 and SPSS 24.0 were used for statistical analysis. Demographic data and mean total scores of the particular scales were assessed using descriptive statistics. The mean, median, standard deviation, and distribution of data were defined. The Shapiro–Wilk W-test was used to determine the Gaussian distribution of the data. The unpaired t-test and the Mann–Whitney (MW) tests were used for the comparisons of the mean values. The relationship between particular categories was analyzed using the correlation coefficients (Pearson or Spearman according to the distribution of data) and linear regression. The Fisher’s exact test or chi-squared test was used to verify the relationship between alternative variables (sex, education, marital status, partnership). Multiple stepwise regression analysis was used to calculate the significance of correlations of certain factors. The 5% level of significance was considered to be satisfactory for all statistical tests.
Results
Sample characteristics
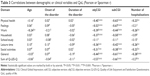
A total of 81 outpatients with depressive disorder (persistent affective disorder – dysthymia, MDD, or recurrent depressive disorder) agreed to participate in the study and completed the scales (76.5% were women). Out of them, 76 patients completed all the questionnaires (only a few demographic data were missed). Mean age was 52.08±13.57 years. Most patients were married (54.3%). Nearly half of the patients achieved a secondary education (49.4%; Table 1). Family psychiatric history was found in 29 patients (35.8%). The healthy control group and the clinical group did not show any statistical differences in age, sex ratio, education, and marital status (Table 1).
Approximately 56.8% of patients were employed. Of the 75 patients who completed these questionnaires, 42 (56.0%) patients received disability benefits; the most frequent were complete disability benefits (n=10; 13.3%), followed by partial disability benefits (n=10; 13.3%) and retirement (n=22; 29.3%). Among the controls, 82.9% were employed. There was a statistically significant difference between the groups in the ratio of employed and unemployed people (Table 1).
The number of hospitalized patients in the past years was 22 (the remaining patients were not hospitalized yet, who stated this figure, were treated in the outpatient clinic), and the average number of hospitalizations was 0.51±1.05. Out of 56 (71.8%) patients, 22 (28.2%) were hospitalized once at least, and 10 patients (12.8%) were hospitalized twice or more (Table 1).
Current medication
A total of 76 patients (93.8%) reported that they used prescribed antidepressive medication. Most of the patients indicated that they were using the medication in prescribed dosages regularly (91.3%), and four patients (4.9%) reported taking the medication irregularly (sometimes they had forgotten to use it). The precise dosages of medication taken were not monitored in this study.
Severity of the disorder
Psychiatrists evaluated the actual severity of the depressive syndrome in their patients using objCGI severity scores. On average, the objCGI score was 3.16±1.25. The average rating of subCGI was 2.50±1.16. The average difference between objCGI severity rating and subCGI rating was 0.66±1.01 (Table 1). There was a statistically significant difference between objective and subjective assessment of the severity of the disorder (MW U-test =2,257; P<0.001); psychiatrists evaluated the severity as more severe than the patients themselves.
Self-stigma
A total of 80 patients completed the ISMI questionnaire. Only one patient did not fully complete this questionnaire, so his/her data were not used in the analysis.
Relationship between self-stigma and demographic and clinical variables
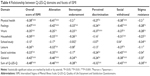
The overall score of ISMI did not statistically significantly correlate with the age of patients, the age at the onset of the disorder, the length of the disorder, and the number of hospitalizations. However, self-stigma highly significantly correlated with the objCGI and subCGI severity of the disorder in all subscales of ISMI (Table 2).
There were no differences between the sexes in the overall score of ISMI (Table 2). However, the employed and unemployed patients significantly differed in self-stigma, where those without a job had a higher degree of stigmatization of themselves. The overall rating of ISMI also depended on the different amounts of education; patients with a secondary school education stigmatized themselves more than patients with a university education (Table 2). Regarding marital status or having a partner, the comparison of the overall score of ISMI did not show any differences between the groups (Table 2).
Quality of life
A total of 80 patients completed the Q-LES-Q. From the maximum of 465 possible points, patients received 280.9±59.87; the mean relative sum of Q-LES-Q was 60.41%±12.88%. The healthy controls received 316.10±45.04 points on average, and the relative sum of Q-LES-Q was 67.99%±9.69% of the maximum. This difference in QoL between outpatients and healthy controls was highly significant (Table 1).
The QoL of patients with depression was lower especially in the domains of feelings, work, leisure time, social activities, and general of Q-LES-Q compared with the control group. This difference was not found in the domains of physical health, household, and school (Table 1).
Relationship between QoL and demographic and clinical variables
The sum of Q-LES-Q and most of the domains of Q-LES-Q correlated negatively only with the objective and subjective assessment of severity of the disorder (objCGI and subCGI) but not with other demographic or clinical features such as the age at the onset of the disorder and duration of the disorder. If the patients feel that they are severely depressed, then there will be a negative impact mainly on their physical health, feelings, and functioning in the household (Table 3). The age of the patients correlated negatively with the domain of work, and the number of hospitalizations correlated significantly negatively with the domains of physical health, work, leisure time, social activities, general, and the sum of Q-LES-Q (Table 3).
Relationship between self-stigma and demographic and clinical factors
The overall score of self-stigma correlated significantly with the objCGI and subCGI (Table 2), but not with the age, the age at the onset of the disorder, duration of the disorder, or the number of hospitalizations. From the subscales of ISMI, it was found that the results of the correlation analysis were the same as of the overall score of ISMI (Table 2), where all of them correlated with objCGI and subCGI.
Relationship between QoL and self-stigma
The overall rating of ISMI and ISMI subscales correlated highly significantly with all the domains of Q-LES-Q except school/study (Table 4). “Stereotype endorsement” correlated with the domains of feelings, work, household, general, and the sum of Q-LES-Q but not with physical health, school/study, leisure, and social activities. The subscale “stigma resistance” correlated with the domains of feelings, work, household, school, and the sum of Q-LES-Q but not with physical health, leisure time, social activities, and general (Table 4).
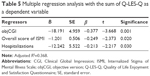
Regression analysis
Because several factors were significantly related to the sum of Q-LES-Q, the multiple stepwise regression analysis was performed to identify the most important factors associated with QoL in the outpatients with depressive disorder. The multiple regression analysis was performed only on the patient group. The dependent variable was the sum of Q-LES-Q. The independent variables were the factors, which significantly correlated, in the previous analysis, with the sum of Q-LES-Q (objCGI, the number of hospitalizations, the overall score of ISMI, and the ISMI domains of alienation, stereotype endorsement, discrimination experience, and withdrawal). The most significant factors associated with the sum of Q-LES-Q were objCGI, the overall rating of ISMI, and the number of hospitalizations, which totally explained 36.8% of the sum of Q-LES-Q scores (F=15.545, df=75; P<0.001; Table 5).
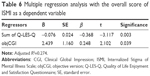
Self-stigma in outpatients with depressive disorder measured by ISMI (dependent variable) was significantly related to many factors; therefore, the multiple regression analysis was performed. Between independent factors, variables significantly associated with the degree of self-stigma, such as objCGI, the sum of Q-LES-Q, all domains of Q-LES-Q except school activities, were included. The most significant factors associated with self-stigma measured by the overall score of ISMI were objCGI and the sum of Q-LES-Q, which totally explained 27.4% of the overall rating of ISMI (F=14.585, df=72; P<0.001; Table 6).
Discussion
This study assessed the associations between self-stigma, QoL, and demographic and clinical data in outpatients suffering from depressive disorder. Similar to other investigations on different psychiatric disorders, the sum of Q-LES-Q in patients was lower than that in healthy controls.28,43–45 Statistical analysis revealed differences in all the Q-LES-Q domains, except household and school/study domains. This result was partly in agreement with the outcome of the study by Sidlova et al46 in schizophrenia, where patients with schizophrenia reported lower QoL in the domains of physical health, feelings, leisure, and general. The authors did not report the differences in the domains of social activities, which demonstrated contrasting findings in our study. The different diagnoses could explain the discrepancies in the results be because of higher mean age of the patients in the current study (but in the linear regression analysis, there was no significant correlation between the age of our patients and their level of Q-LES-Q) and the lower level of education in the patients reported in the study by Sidlova et al.46 A comparable study by Holubova et al47 conducted with patients with schizophrenia showed practically the same results in comparison with healthy controls as those of the current study with depressive disorder patients. The question for further research consideration is whether this type of mental disorder affects the level of QoL or the diagnosis have no impact on the outcome.
The level of self-stigma in the depressive disorder patients was similar to that of patients suffering from other mental disorders, such as patients with anxiety spectrum disorders and schizophrenia spectrum disorders.46–48 This result can be explained by the fact that the degree of self-stigma is probably not influenced as much by a diagnosis of the mental illness. Maybe, just the fact of being a person who needs treatment because of mental health problems and who has been hospitalized or visited a psychiatrist can be problematic for a patient’s self-image.
The second aim of this study was to focus on the demographics in association with self-stigma, wherein we found no evidence of a relationship between age, sex, marital status, having a partner, the age at the onset of the disorder, duration of the disorder, the number of hospitalizations, and self-stigma. These findings partly correspond to the results of Vrbová et al49 and Gerlinger et al50 in a population of schizophrenic patients, who showed that sex, marital status, and partnership are not statistically significantly related to the degree of self-stigma. On the other hand, our results showed that patients with secondary school education showed a higher level of self-stigma than patients with university level of education, which is different in comparison with the abovementioned studies of schizophrenia. Kamaradova et al51 found that the degree of self-stigma among men and women does not differ, which was also confirmed in the current study. The rate of self-stigma was significantly associated with employment. Unemployed patients showed a higher degree of self-stigma than the employed patients. The same results were described in our previous study in schizophrenia.47 An important association was found between subjectively or objectively assessed severity of the illness and all subscales of ISMI.
The third aim was to assess the relationship between QoL and self-stigma. The results showed that the level of self-stigma significantly negatively correlated with QoL. A similar result was described by Tang and Wu52 and Holubova et al47 in a population of patients with schizophrenia and by Ocisková et al48 in patients with anxiety spectrum disorders. Yen et al53 examined the association between QoL and self-stigma, and found that depressive individuals had lower QoL on the physical, psychological, and social relationship domains than the nondepressed control group. These results are in agreement with our conclusion. Patients with depression, who had more severe self-stigma, had lower QoL. The question is whether self-stigma changes QoL or leads to a decrease in QoL, or whether the low QoL predicts a higher level of self-stigma.
The results of this study also showed that self-stigma of the patients with depressive disorder negatively correlated with all the domains of QoL. It is also possible that the symptomatology affects QoL, as well as the readiness to develop self-stigma. QoL also highly depended on the degree of severity of the disorder. The stepwise regression analysis showed that objCGI, the overall score of ISMI, and the number of hospitalizations correlated with a Q-LES-Q score to the greatest extent. The objective and subjective severities of the disorder contribute to a significant proportion of the overall QoL in depression. Depressive disorders are characterized by distorted negative and pessimistic view of the person itself and also by the negative view on other people; hence, it is understandable that the perception of their life circumstances and qualities will be reduced according to the nature of this mental illness. It is possible, that after depressive episode remitted, the severity of the disorder could not have such impact on the QoL. The same consideration applies to self-stigma, which was also mainly influenced by the objective and subjective severity of the disorder. The rate of self-stigmatization may also be different after a reduction in depressive symptoms. Prospective studies are needed to answer this question.
These findings are similar to our study of schizophrenia patients,47 where the most significant factors associated with QoL were self-stigma, objective and subjective severity, and the age at the onset of the disorder, which totally explained 49.2% of the Q-LES-Q scores. The only difference is that the regression model of these variables in depression explained 36.8% of the sum of Q-LES-Q scores.
Because of the cross-sectional design of this study, it is difficult to make a conclusion about the causative factors. Hence, prospective studies are needed to answer this question.
Limitations
The main limitation of this study is using the self-report scales and questionnaires, since filling out the questionnaire can be significantly affected by the current state of the patient. This applies mainly to the questionnaire evaluating the QoL. In addition, the severity of the disorder was assessed only by the overall clinical rating, rather than a more specific assessment instrument. The other limitation is that patients showed various severities of the disorder, which highly influence the results. The small sample size is also a limitation of the study. The mental health of the healthy control group was not evaluated by any diagnostic assessment, but only by own reports, and hence we should not be confidently convinced of their comprehensive mental health. The engagement of the healthy control using relatives is also problematic to the research, because an individual’s QoL could affect his/her decision to participate in the study. In addition, this cross-sectional study does not allow us to explore the causality of the study phenomena, which requires a prospective study.
Conclusion
Self-stigma and QoL could be reflected as significant features for patients, who suffer from depressive disorders. The outcomes of the investigation presented a lower level of QoL in patients compared with healthy controls in almost all measured domains. Patients with a higher level of self-stigma reported a lower standard of QoL and a greater degree of severity of the disorder. Our data suggest the importance of a subsequent study and longitudinal assessment of the symptoms and their influence on the subjectively perceived QoL during the disorder. In addition, answering the question, whether and how the QoL could change after the therapy, remains the significant challenge for research in the future.
The implications of the findings into practice should be important because of the message for the clinicians that the self-stigma and QoL are interrelated. Talking with the patients about their experiences how to be a psychiatric patient and how to be a person treated in psychiatry, needs empathy to his/her fears of the changes in life roles and empathy how painful is his/her self-stigma itself, and encouraging him/her to modify this view of himself or herself, can be quite important for patients and their mental recovery.
Depressed disorder patients had lower QoL on the physical, psychological, and social relationship domains than that of the nondepressed control group. These results are in agreement with our conclusion. The patients with depression, who had more severe self-stigma, had lower QoL.
The results of this study showed that self-stigma of patients with depressive disorder negatively correlated with all the domains of QoL.
Acknowledgments
The authors appreciate the willing cooperation of Dr Jiří Rozkoš from Prostějov, Dr Jan Flídr from Kralupy nad Vltavou, Dr Jana Matějková from Prague, Dr Simona Papežové from Prague, Dr Pavel Tautermann from Prague, Dr Markéta Zemanová from Havlíčkův Brod, Dr Markéta Dobrá from Hrabyně, Dr Zuzana Kozáková from Trutnov, Dr Tibor Miklóš from Prague, Dr Michaela Zapletalová from Chomutov, Dr Jana Novosadová from Blansko, Dr Jiří Trska from Týn nad Vltavou, Dr Zdeněk Holoubek from Nymburk, Dr Iva Ondráčková from Prague, Dr Andrea Bryčková from Hořice, Dr Jindřiška Masnerová from Beroun, Dr Petr Pastucha from Prostějov, and Dr Hana Lemanová from Brno.
Disclosure
The authors report no conflicts of interest in this work.
References
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–2161. | ||
Camp DL, Finlay WML, Lyons E. Is low self-esteem an inevitable consequence of stigma? An example of women with chronic mental health problems. Soc Sci Med. 2002;55(5):823–834. | ||
Fung KMT, Tsang HWH, Corrigan PW. Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatr Rehabil J. 2008;32(2):485–495. | ||
Ustündağ MF, Kesebir S. Internalized stigmatization in bipolar patients: relationship with clinical properties, quality of life and treatment compliance. Turk Psikiyatri Derg. 2013;24(4):231–239. | ||
Corrigan PW, Rafacz J, Rüsch N. Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Res. 2011;189(3):339–343. | ||
Latalova K, Prasko J, Kamaradova D, et al. Self-stigma and suicidality in patients with neurotic spectrum disorder – a cross sectional study. Neuro Endocrinol Lett. 2014;35(6):474–480. | ||
Schulze B, Angermeyer MC. Subjective experiences of stigma: a focus group study of schizophrenic patients, their relatives, and mental health professionals. Soc Sci Med. 2003;56(2):299–312. | ||
Ritsher JB, Phelan JC. Internalized stigma predicts the erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257–265. | ||
Tsang HW, Fung KM, Chung RC. Self-stigma and stages of change as predictors of treatment adherence of individuals with schizophrenia. Psychiatry Res. 2010;180(1):10–15. | ||
Ociskova M, Prasko J, Vrbova K, Kamaradova D, Jelenova D, Latalova K. Stigma and self-stigma in patients with schizophrenia. Ceska Slov Psychiatr. 2014;110(5):250–258. | ||
Ociskova M, Prasko J, Kamaradova D. Relationship between personality and self-stigma in mixed neurotic spectrum and depressive disorders – cross sectional study. Act Nerv Super Rediviva. 2015;57(1–2):22–29. | ||
Ociskova M, Prasko J, Kamaradova D, Grambal A, Sigmundova Z. Individual correlates of self-stigma in patients with anxiety disorders with and without comorbidities. Neuropsychiatr Dis Treat. 2015;11:1767–1779. | ||
Ociskova M, Prasko J, Latalova K, Kamaradova D, Grambal A. Psychological factors and treatment effectiveness in resistant anxiety disorders in highly comorbid inpatients. Neuropsychiatr Dis Treat. 2016;12:1539–1551. | ||
WHO. Preamble to the Constitution of the World Health Organization as Adopted by the International Health Conference; June 19–22, 1946; New York. Signed on 22 July 1946 by the representatives of 61 states (official records of the World Health Organization, Vol 2, 100) and entered into force on 7 April 1948. | ||
WHOQOLG. Measuring Quality of Life. 1997. Available from: http://www.who.int/mental_health/media/68.pdf. Accessed September 23, 2016. | ||
Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–1178. | ||
Ishak WW, Christensen S, Sayer G, et al. Sexual satisfaction and quality of life in major depressive disorder before and after treatment with citalopram in the STAR*D study. J Clin Psychiatry. 2013;74(3):256–261. | ||
Angermeyer MC, Holzinger A, Matschinger H, Stengler-Wenzke K. Depression and quality of life: results of a follow-up study. Int J Soc Psychiatry. 2002;48(3):189–199. | ||
Hirschfeld RM, Dunner DL, Keitner G, et al. Does psychosocial functioning improve independent of depressive symptoms? A comparison of nefazodone, psychotherapy, and their combination. Biol Psychiatry. 2002;51(2):123–133. | ||
Mcknight PE, Kashdan TB. The importance of functional impairment to mental health outcomes: a case for reassessing our goals in depression treatment research. Clin Psychol Rev. 2009;29(3):243–259. | ||
Berlim MT, Mcgirr A, Fleck MP. Can sociodemographic and clinical variables predict the quality of life of outpatients with major depression? Psychiatry Res. 2008;160(3):364–371. | ||
Linzer M, Spitzer R, Kroenke K, et al. Gender, quality of life, and mental disorders in primary care: results from the PRIME-MD 1000 study. Am J Med. 1996;101(5):526–533. | ||
Langlieb AM, Guico-Pabia CJ. Beyond symptomatic improvement: assessing real-world outcomes in patients with major depressive disorder. Prim Care Companion J Clin Psychiatry. 2010;12(2). | ||
Clifton J, Gingrich N. Are citizens of the world satisfied with their health? Health Aff (Millwood). 2007;26(5):w545–w551. | ||
Wannamethee G, Shaper AG. Self-assessment of health status and mortality in middle-aged British men. Int J Epidemiol. 1991;20(1):239–245. | ||
Lahelma E, Arber S, Kivela K, Roos E. Multiple roles and health among British and Finnish women: the influence of socioeconomic circumstances. Soc Sci Med. 2002;54(5):727–740. | ||
Unden AL, Elofsson S. Do different factors explain self-rated health in men and women? Gend Med. 2006;3(4):295–308. | ||
Ten Doesschate MC, Koeter MW, Bockting CL, Schene AH; DELTA Study Group. Health-related quality of life in recurrent depression: a comparison with a general population sample. J Affect Disord. 2010;120(1–3):126–132. | ||
Ishak WW, Balayan K, Bresee C, et al. A descriptive analysis of quality of life using patient-reported measures in major depressive disorder in a naturalistic outpatient setting. Qual Life Res. 2013;22(3):585–596. | ||
IsHak WW, Greenberg JM, Balayan K, et al. Quality of life: the ultimate outcome measure of interventions in major depressive disorder. Harv Rev Psychiatry. 2011;19(5):229–239. | ||
IsHak WW, Mirocha J, James D, et al. Quality of life in major depressive disorder before/after multiple steps of treatment and one-year follow-up. Acta Psychiatr Scand. 2015;131(1):51–60. | ||
Papakostas GI, Petersen T, Mahal Y, Mischoulon D, Nierenberg AA, Fava M. Quality of life assessments in major depressive disorder: a review of the literature. Gen Hosp Psychiatry. 2004;26(1):13–17. | ||
EMEA. 2002. Available from: http://www.ema.europa.eu/pdfs/human/ich/013595en.pdf. Accessed March 20, 2009. | ||
Burgess RG. In the Field: An Introduction to Field Research. London: Routledge; 1991. | ||
Ritsner M, Kurs R, Gibel A, Ratner Y, Endicott J. Validity of an abbreviated Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-18) for schizophrenia, schizoaffective, and mood disorder patients. Qual Life Res. 2005;14(7):1693–1703. | ||
Müllerova H. Transcultural transmission and validation of the quality life questionnaire Q-LES-Q (in Czech: Mezikulturní přenos a validace dotazníku kvality života Q-LES-Q). Psychiatrie. 2001;5:80–87. | ||
Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121(1):31–49. | ||
Boyd JE, Adler EP, Otilingam PG, Peters T. Internalized Stigma of Mental Illness (ISMI) Scale: a multinational review. Compr Psychiatry. 2014;55(1):221–231. | ||
Ritsner M, Ben-Avi I, Ponizovsky A, Timinsky I, Bistrov E, Modai I: Quality of life and coping with schizophrenia symptoms. Qual Life Res. 2003;12(1):1–9. | ||
Ociskova M, Prasko J, Dostalova L, et al. Self-stigma in psychiatric patients – standardization of the ISMI scale. Neuro Endocrinol Lett. 2014;35(7):624–632. | ||
Guy W, editor. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: DHEW; 1976. Available from: https://archive.org/details/ecdeuassessmentm1933guyw. | ||
Zaider TI, Heimberg RG, Fresco DM, Schneier FR, Liebowitz MR. Evaluation of the clinical global impression scale among individuals with social anxiety disorder. Psychol Med. 2003;33(4):611–622. | ||
Jansen K, Campos Mondin T, Azevedo Cardoso TD, et al. Quality of life and mood disorder episodes: community sample. J Affect Disord. 2013;147(1–3):123–127. | ||
Lenox-Smith A, Macdonald MT, Reed C, et al. Quality of life in depressed patients in UK primary care: the FINDER study. Neurol Ther. 2013;2(1–2):25–42. | ||
Sivertsen H, Bjørkløf GH, Engedal K, Selbæk G, Helvik AS. Depression and quality of life in older persons: a review. Dement Geriatr Cogn Disord. 2015;40(5–6):311–339. | ||
Sidlova M, Prasko J, Jelenova D, et al. The quality of life of patients suffering from schizophrenia – a comparison with healthy controls. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2011;155(2):173–180. | ||
Holubova M, Prasko J, Latalova K, et al. Are self-stigma, quality of life, and clinical data interrelated in schizophrenia spectrum patients? A cross-sectional outpatient study. Patient Prefer Adherence. 2016;10:265–274. | ||
Ocisková M, Praško J, Kamarádová D, et al. Self-stigma in psychiatric patients – standardization of the ISMI scale. Neuro Endocrinol Lett. 2014;35(7):624–632. | ||
Vrbová K, Kamarádová D, Látalová K, et al. Self-stigma and adherence to medication in patients with psychotic disorders – cross-sectional study. Neuro Endocrinol Lett. 2014;35(7):645–652. | ||
Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU. Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry. 2013;12(2):155–164. | ||
Kamaradova D, Latalova K, Prasko J, et al. Connection between self-stigma, adherence to treatment, and discontinuation of medication. Patient Prefer Adherence. 2016;10:1289–1298. | ||
Tang IC, Wu HC. Quality of life and self-stigma in individuals with schizophrenia. Psychiatr Q. 2012;83(4):497–507. | ||
Yen CF, Lee Y, Tang TC, Yen JY, Ko CH, Chen CC. Predictive value of self-stigma, insight, and perceived adverse effects of medication for the clinical outcomes in patients with depressive disorders. J Nerv Ment Dis. 2009;197(3):172–177. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.