Back to Journals » International Journal of General Medicine » Volume 13
Self-Reported Morbidity and Health-Seeking Behavior and its Predictors Among a Geriatric Population in Western Ethiopia: Community-Based Cross-Sectional Study
Authors Feyisa BB , Deyaso SF, Tefera GM
Received 28 September 2020
Accepted for publication 23 November 2020
Published 7 December 2020 Volume 2020:13 Pages 1381—1393
DOI https://doi.org/10.2147/IJGM.S283906
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Beshadu Bedada Feyisa,1 Seble Fekadu Deyaso,2 Gosaye Mekonen Tefera3
1Department of Public Health, College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia; 2Department of Sociology, College of Social Sciences and Humanities, Ambo University, Ambo, Ethiopia; 3Department of Pharmacy, College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia
Correspondence: Beshadu Bedada Feyisa Email [email protected]
Background: Planning for health care services provision depends on the morbidity profile, health-seeking behavior (HSB), and its predictors. Thus, this study aimed to identify the level of self-reported morbidity, HSB and its predictors.
Patients and Methods: A community-based cross-sectional study was conducted among the geriatric (≥ 60 years) population in West Shoa Zone. A multi-stage systematic sampling technique was employed to select the study participants. After testing for collinearity, variables with p-value < 0.25 on binary logistic regression were entered into backward multivariate logistic regression analysis with statistical significance at p-value < 0.05.
Results: With a response rate of 98%, 779 study participants were recruited. The median (IQR) age of the respondents was 70 (70– 78) years. Five hundred eighty-four (3/4) of the study participants reported that they experienced morbidity at least once in the year before interview. Of 584 study participants, 53.9% had poor HSB. Living in village (p-value = 0.034), being housewife (p-value = 0.048), wealth index [being rich (p-value = 0.033), being in moderate economic status (p-value= 0.001), and being poor (p-value= 0.049) relative to richest], being head of polygamous household (p-value= 0.019), non-smoker (P-value = 0.012), not having community-based health insurance coverage (CBHI) (p-value< 0.0001), having ≤ 3 times number of illness (p-value < 0.0001), self-medication (p-value < 0.0001), not having hypertension (p-value=0.016), not having diabetes mellitus (DM) (p-value=0.012), and not having oro-dental problem (p-value= 0.043) were positively associated with poor HSB. Nevertheless, self-perceived mild severity of illness (p-value= < 0.0001), good health status (p-value= 0.001), and not having musculoskeletal problem (p-value< 0.0001) were negatively associated with poor HSB.
Conclusion: There was a high prevalence of self-reported morbidity and poor HSB. There should be an effort to improve the HSB and CBHI utilization of the geriatric population by all stakeholders. Moreover, modifiable predictors of HSB needs to be improved.
Keywords: self-reported morbidity, geriatrics, health-seeking behavior; HSB, predictor, Ethiopia
Introduction
Aging is a natural process, which is associated with physiological and biological changes. It is associated with diseases, the cumulative effect of multiple exposures to psychological, physical, and social conditions that are frequently unfavorable and increase the risk of health problems. Morbidity rates are highest in the aged populations, due to lack of availability and accessibility of health services related to the older population.1
Globally, the proportion of the elderly has been rising steadily, more than the number of people in all younger age groups. It increased from 7% in 1950 to 11% in 2007 and is expected to rise by 22% in 2050. In the same manner, between 2017 and 2050, the number of elderly living in developing countries is expected to rise from 652 million to 1.7 billion.2 This projection indicates that nearly 80% of the world’s elderly populations will live in developing countries in 2050.2 Moreover, in Ethiopia, the elderly population accounts for about 5% of the total population in 2007 and is expected to rise to 7.3% of the total population by 2037.3
The rise in the number of elderly people increases the burden of providing social services, including health care services for these populations.4 However, inequality in health, education, and income levels of older people is increasing between developed and developing countries. Policies that support the elderly such as pensions, free health care, and treatments of chronic disease have been slow to evolve in developing countries compared with the fast rise in the numbers of those people.5 A similar situation was found in Ethiopia as most have no constant sources of income, no adequate public sector pension for employed,6 and absence/lack of social security system among unemployed rural elderly people.7,8 This might affect health-seeking behavior (HSB) of the elderly population; thus, they could be obliged to visit alternative care rather than seeking modern health care.9 HSB has been defined as any action performed by individuals to search for remedy owing to manifestation of symptoms for self-perceived health problems or illness.10
There is increasing literature on HSB and its determinants in many developing countries. These studies revealed that the determinants for HSB were not similar for all elderly populations. It may vary based on the cultural belief and practice as well as the economic status of the countries.11–13 As we understand from the above literature, the factors that determine the HSB of the geriatric population were different for different nations. Thus, country or community-specific data is mandatory for planning health intervention for those populations.
However, in Ethiopia, there is limited literature on the level of morbidity, HSB, and its determinant among geriatric populations. Even the limited literature had its own limitation to identify the level of morbidity and HSB among the geriatric population. For instance, a study done in the Wolaita zone, Ethiopia, included only the elderly who experience illness in the month before the survey. This may fail to address the level of self-reported morbidity and the time duration is too short.14 Again, this study was conducted in the South Nation Nationalities and People (SNNP) region of Ethiopia where the socio-economic and cultural beliefs of the study participants were different from the current study participants. Another two studies conducted in Ethiopia were done in a very small study area and on a small sample size, which may be difficult to generalize the result for a large community. Again these studies failed to clearly define HSB among the study participants in relation to the number of their illness in a specified period of time.15,16
Planning for health care services provision depends on the morbidity profile and HSB of the population. Data on HSB is essential to provide need-based health care services to the population. A community-based study reflects the HSB and its determinant. Thus, this study aimed to fill the literature gap and identify the level of self-reported morbidity, HSB and its determinant among the geriatric population of Western Ethiopia. The results of this study will be used as baseline information for the researcher and for policymakers to make decisions and use available evidence-based interventions to improve the HSB of the elderly population in the country.
Patients and Methods
Study Area, Design, and Period
A community-based cross-sectional study was conducted from April 1 to June 1, 2018. The study was conducted at Oromia regional state, West Shoa Zone using a multi-stage random sampling of geriatric (≥60 years) populations. The West Shoa zone is located in west Ethiopia and covers 14,921.19 km2 with a total population of 2,058,676 (Ethiopian 2007 census report). The geriatric population was estimated to be 102,934 depending on the proportion set by the Central Statistical Agency of Ethiopia.3 West Shoa Zone has 23 woredas and 526 kebeles of which 486 are rural. Out of 23 weredas, eight woredas (Ambo, Bako Tibe, Dandi, Ilu Gelan, Jibat, Ilfeta, Ambo, and Toke Kutaye) and 26 kebeles were included in the study.
Source Population
All elderly ≥ 60 years who were residents in the West Shoa zone were the source population.
Study population:All elderly in the West Shoa zone who were selected by systematic random sampling technique.
Exclusion criteria: Elderly with the following impairments will be excluded from this study.
- Elderly who were severely ill and unable to respond
- Elderly who were unable to speak and hear
- Elderly who were away from home during data collection for three consecutive visits
- Elderly who were diagnosed with dementia or memory loss (to avoid recall bias).
Study Variables, Sample Size, and Sampling Technique
Dependent variable: HSB of the geriatric population.
Independent variable: Socio-demographic variable; gender, residence, occupation of respondents, wealth index, family size, head of the household, decision-maker on how to use the money earned in the household, decision-maker on health service utilization, the pattern of cigarette smoking, living conditions, educational status, ownership of land, availability of bank accounts, ownership of the living house, age and marital status, and decision-maker on a household major purchase, seeking medical care, and how to expend money earned in the household. Health care and morbidity related variable: availability of health insurance, self-rating health, number of illnesses in a year before the interview, distance from the health facility, self-rating severity of illness, self-medication, and morbidity profile.
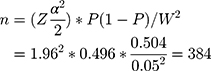
The minimum sample size (n) required for estimation of true proportion was calculated by using a single population proportion formula as follows,
Where
P=0.496, the proportion of elderly who utilize health service17
Z= is the standard normal score = 1.961 at 95% CI
Considering the design effect of 2 and non-response rate =3%,
A multi-stage sampling technique was employed to select the study participant. The first eight woredas were selected by the lottery method from 23 woredas in the West Shoa zone. Then 26 kebeles were selected randomly after proportional allocation for each selected woreda. Then the final sample was allocated to each kebeles proportionally to the size of the study participants in each kebeles. A systematic sampling technique without a sampling frame was used to identify the study participants. The data collector makes the Kebeles office as the center of the kebeles and goes to the four directions of the kebeles. They contact any household and count the first house that they got geriatric population as one. They continue the same procedure until they reach k value for each kebeles. The first household with the geriatric population to be included in the study was selected by the lottery method from the first household to k for each kebeles. Then they interview the study participant in the household in every kthvalues for each kebeles. K values vary for each kebeles. If there are two or more geriatric people in the same household, one of them was selected by lottery method.
Data Collection Tool, Process and Quality Management
A semi-structured questioner was used for collecting data from the study participants. The questioner has two main parts socio-demographic part adopted from Ethiopian Demographic and HealthSurvey18 and health care- and morbidity-related questions were adopted from a previous study conducted for a similar purpose with slight modification, which was available elsewhere.12,14,15 The interview tool was prepared first in English, then translated into Afaan Oromo, and re-translated to English to maintain its consistency by different persons. It was pre-tested on 40 elderly who were comparable with actual study participants in one non-sampled kebele. Ten graduating medical students after training were given on the purpose, objective, and the content of the questioner for three days did data collection.
A face-to-face interview was employed with the study participant at their residence on socio-economic factors, health status, morbidity status, HSB and decision-making status. Data on health status, morbidity pattern and HSB were collected through self-reported history. To reduce recall bias, a local calendar was used with memorable occasions to probe number of illnesses and any health care seeking in the previous year. Those participants who visit the health facilities reported the morbidity pattern they told the facility. For the participant who does not seek medical care, the morbidity pattern was assessed through the provisional diagnosis of diseases based on reported symptoms and clinical evaluation by investigators. The elderly who reported that they had health problems were asked for HSB. The principal investigator and supervisor rechecked for completeness and consistency of the questionnaire immediately after the interview at the field level and during submission.
Statistical Analysis
Ahead of data analysis using Statistical Package for Social Science (SPSS) version 21, the data were cleaned, coded, and entered into the Epi data 3.1 version. Continuous variables were presented using mean with standard deviation (SD) or median with inter-quartile range (IQR) after testing for normality using the kurtosis test. Categorical variables were presented using frequencies and percentages. Moreover, variables with collinearity coefficients of ≥ 0.8 were excluded from the model. Then variables with a p-value of < 0.25 on binary logistic regression were entered into backward multivariate logistic regression analysis with statistical significance atp-value <0.05 to search for independent predictors of HSB.
The wealth index was assessed to estimate the economic status of the participant. It was calculated using the household assets and ownership of farm animal data via a principal component analysis (PCA). All variables used as an indicator of wealth Index were transformed into dichotomous (0, 1) indicators. The variables were coded no if the respondents have no particular variable and yes if they have. After transforming all variables into a dichotomous indicator, it was examined using a PCA to produce a common factor score for each household. Variable with zero variance were dropped. After completion of PCA, the component that accounts for the largest proportion of the variance is used as the wealth index. Finally, the ranking of this component was made to obtain wealth quintile.
Operational Definition
Morbidity: is defined as having any type of illness or perceived health problem and/or informed by a physician ahead of data collection period.
Self-rating health status: The participants were asked to rate their current health status as very good, good, moderate, bad, and very bad. Then very good and good were recorded as good and very bad and bad were recorded as bad.
Self-rating severity of illness: The participants were asked how they rate the severity of their illness using a scale of very severe, severe, and mild.
Seeking modern medical care: Choosing to use any modern health service resource, i.e., government hospitals, private hospitals or clinics, health centers, or health posts to get a remedy for their illness.
Seeking alternative care: Choosing non-modern medical care services like a religious place/holy water, traditional healer, herbal medication, and home remedies to get remedy for their illness.
HSB has been defined as any action performed by individuals to search for a remedy due to the manifestation of symptoms for self-perceived health problems or illness.10 In previous studies,11–16 it refers to visiting modern medical care for any of their need at least once in a given period. However, this may overestimate HSB because somebody may have ten needs (illness), but may visit only once. Thus, these individuals did not seek medical care for nine of his/her illness but were labeled as he/she sought medical care for his/her illness. In this study, HSB is estimated by the ratio of the number of times that the participants seek medical care for the number of their illnesses (need) in the year before the interview. Then, an individual’s score was labeled as having good HSB if the ratio is above the median and poor HSB if the ratio is below the median.
Ethical Considerations
Ethical clearance was obtained from Ambo University, Research, and Ethics Committee with the reference number of AU/T1035/2/17/018 on 21February 2018. Confidentiality was kept and informed verbal consent was obtained from each study participants after explaining the purpose of the study. Verbal informed consent was approved by the Ambo University Research and Ethics Committee. This study was conducted in accordance with the ethical guidelines of the Helsinki Declaration.
Results
Socio-Demographic Characteristics of the Respondents
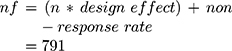
A total of 779 participants were included in the study with a response rate of 98%. The median (IQR) age of the respondents was 70 (70–78) years. The majority of them were male (53.4%), follow orthodox religion (70.0%), Oromo ethnic group (93.2%), married (52.8%), and had no formal education (91.7%. About 44.5% of the respondents were farmers and 34.4% of them were retired).
About 23.5% of the respondents were in the medium wealth quintiles followed by the richest and poorest 20.0% each. About 88.0% of the respondents were living with their family, 52.9% were from the rural areas and 83.0% were living in their own house during data collection. About 64.1% and 32.2% of the study participant had farming land and a bank account, respectively (Table 1).
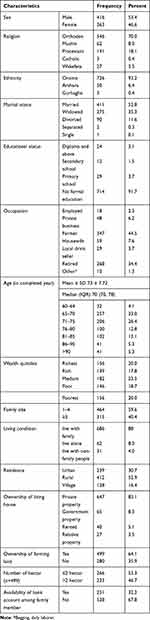 |
Table 1 Socio-Demographic Characteristics of Geriatric Population in West Shoa Zone, Ethiopia, 2018 (n=779) |
Decision Making of the Study Participant
About 49.8% of the geriatric population included in this study had final say on how to spend money earned in the household. Half (50.7%) of the respondents can decide on their own health service utilization and 47.8% of them can decide on household major purchase (Table 2).
 |
Table 2 Decision Making of the Respondent (N= 779) |
Health Care and Morbidity-Related Characteristics
The median ratio of HSB (number of times health seeking compared to number of illness) was 0.5 with minimum of 0 to 1. The majority (62.6%) of the respondents were in good health status (per-self-rating health status) during data collection. Five hundred eighty-four of 779 (3/4) of the participants reported that they experienced morbidity at least once in the year before the interview. Of 584, more than half (53.9%) had poor HSB for their illness. About 45.2% and 24.0% of the respondents had co-morbid conditions and practiced self-medication, respectively. A few (14.5%) of the respondents had community-based health insurance (CBHI) coverage. Among those who had the CBHI coverage, 11.5% did not use the insurance for the health service costs (Table 3).
 |
Table 3 Health Care and the Pattern of Self-Reported Morbidity Characteristics |
Number of Morbidities, Seeking Alternative Care, and Seeking Medical Care
The median (IQR) number of morbidity was 3 (3–5) times in the year before the interview. The mean ± SD number of time that the participants sought medical care for their illness was 1.85 ± 1.8. The median (IQR) number of time that participant choose alternative care to treat their illness was 0 (0–1)
Morbidity Profile of the Geriatric Population in West Shoa
Most (230) of the study participants experience musculoskeletal-related health problems in one year before the interview; followed by neurologic problems (100). A few (5) study participants complain oro-dental problem (Figure 1).
Predictors of Health-Seeking Behavior
Binary and backward multiple logistic regression analysis were done to assess the predictor of HSB among the geriatric population. Accordingly, gender (p-value = 0.242), religion (p-value= 0.69), head of household (p-value = 0.038), residence (p-value = 0.119), having health insurance (p-value <0.001), self-rating severity of illness (p-value <0.001), self-medication (p-value = 0.002) hypertension (p-value =0.070), DM (p-value = 0.022), musculoskeletal problem (p-value = 0.004), oro-dental problem (p-value = 0.104), genitor-urinary problem (p-value = 0.147), wealth index (p-value= 0.206), family size (p-value = 0.107), self rating health (p-value < 0.001) number of illness (p-value < 0.001), and occupation of the participants (p-value = 0.145) were found to be the candidate variable for backward multivariate logistic regression analysis (Table 4).
 |  |  |
Table 4 Determinant of Health-Seeking Behavior Among Geriatric Population in West Shoa, 2018 |
The residence of the participants was found to be the independent predictor of HSB. Living in the village contributes to poor HSB among the geriatric population by two times (AOR= 2.076 at 95% CI 1.057 to 4.077, p-value = 0.034) relative to living in urban. Being a housewife increases the chance of poor HSB by five times (AOR= 5.312 at 95% CI 1.017 to 27.741, p-value = 0.048) relative to employed. The wealth index is an economic status that was found to be an independent predictor of HSB; [being rich increase the probability of poor HSB by two times (AOR=2.238 at 95% CI 1.066 to 4.699, p-value = 0.033), being in moderate economic status increase chance of poor HSB by four-time (AOR= 3.573 at 95% CI 1.672 to 7.632, p-value= 0.001), and being poor increases chance of poor HSB by two times (AOR= 2.156 at 95% CI 1.003 to 4.632, p-value= 0.049)] as compared to richest. Moreover, being head of a polygamous household increases the chance of poor HSB by six times (AOR= 5.741 at 95% CI 1.337 to 24.661, p-value= 0.019) relative to being a male-headed household (Table 4).
Non-smokers were four times more likely to have poor HSB (AOR= 4. 306 at 95% CI 1.379 to 13.473, P-value = 0.012) as compared to smoker. Not having CBHI coverage increase the probability of poor HSB by four times (AOR= 3.480 at 95% CI 1.846, 6.561, p-value< 0.001) relative to having health insurance coverage. The study participants with good health status (per self-rating scale) were less likely to have poor HSB by 72% (AOR=0.273 at 95% CI 0.127 to 0.586, p-value= 0.001) relative to those with poor health status. Having ≤ 3 times the number of illnesses was less likely to incur poor HSB by 91% (AOR= 0.089 at 95 CI 0.045 to 0.174, p-value <0.001) relative to those who had ≥4-time illness per a year before the interview. Self-perceiving mild severity of illness increases the likelihood of poor HSB by eight times (AOR=7.911 at 95 CI 3.598 to 17.396, p-value= <0.001) relative to very severe. Self-medication increase chance of poor HSB by three times (AOR= 2.965 at 95% CI 1.732 to 5.076, p-value < 0.001) compared to their counterpart (Table 4).
Not having hypertension contributes for poor HSB by two times (AOR= 2.310 at 95% CI 1.169 to 4.567, p-value=0.016) as compared to a hypertensive participant. Not being diagnosed with DM contributes for poor HSB by six times (AOR= 6.370 at 95% CI 1.513 to 26.26.815, p-value=0.012) relative to DM participant. Not having oro-dental problem increases the likelihood of poor HSB by twelve times (AOR= 12.307 at 95% CI 1.078 to 140.555, p-value= 0.043) relative to their counterpart. Participants with musculoskeletal problem were less likely to have poor HSB (AOR= 0.323 at 95% CI 0.205 to 0.507, p-value< 0.001) compared to their counterpart (Table 4).
Discussion
This was a community-based cross-sectional study with the primary aim of assessing the level of self-reported morbidity, HSB and its determinant among the geriatric (≥60 years) population in West Shoa zone, Ethiopia. Accordingly, this study identified a high prevalence of morbidity among the geriatric population. Similar to this study, other studies conducted in the rest of the world have shown,the majority of the geriatric populations face illness with different prevalence. For instance, a community-based study conducted in Nepal identified that 86.5% of participants included in the study experience illness.19 Another community-based study conducted in India identified the prevalence of morbidity among the geriatrics population from 84% to 93.3%.20,21 Moreover,studies conducted in different parts of Ethiopia also reported moderate to the high prevalence of morbidity.7,16 The highest prevalence of morbidity might be a result of physiologic change contributed by the aging process.
As compared to the study conducted in Bedele town, Ethiopia,17 this study identified the low level of HSB; because only less than half had good HSB (46.1%). Similarly, the finding of this study was lower than the study conducted in the urban slum of Assam where HSB was 56.1%.22 However, the proportion of elderly who had good HSB in this study was higher than the study conducted in Nigeria; only one-third of the elderly visit a health service even for an ordinary checkup.13 The variation may be due to the difference in socioeconomic status because a study has shown that socio-economic factor affects the HSB of people.23
Nevertheless, the finding of this study was lower than the finding of other studies conducted in other parts of Ethiopia.14,15 This discrepancy maybe because of the fact that the current study assed HSB in relation to any infirmity happened to elderly (the ratio of visiting health care facilities to the number of illness) in the year before data collection, unlike other studies that identified HSB at least once in a year visiting health care, irrespective of the number of illnesses.17 This may overestimate the HSB, because people may seek medical care for one of their illnesses even though they may have more than one episode of illness. Another study conducted in southern Ethiopia assessed HSB over one month.14
The most prevalent health problem among the elderly in West Shoa zone was a musculoskeletal problem. A similar finding was reported by other studies conducted in different developing countries including Ethiopia, which reported the prevalence of musculoskeletal problems (33% to 86.4%).13,17,21,24 This may be because of the physiologic effect of aging on the component of the musculoskeletal system. Walter R Frontera reported that aging is associated with significant losses of structural and functional properties of tendons, ligaments, bone, and cartilage.25
In this study, we assessed the predictors of HSB among the geriatric population. Similar to the national sample survey conducted in India,26 this study identified residence as an independent predictor of HSB among the elderly. Living in a village increased the likelihood of having poor HSB by two times relative to urban areas. This may be because of access to health facilities, quality and availability of health service in Urban than in Village. Thus, physical access to health service, quality and availability of health service negatively affects the HSB.13,14,17,21,27
Occupation (being a housewife) of the elderly was an independent predictor of poor HSB relative employed elderly. This may be because of the financial dependency of the housewife as compared to employed elderly. There was a report that financial dependency has a positive association with poor HSB.11 On the other hand, women’s autonomy on their own HSB may contribute for not seeking medical care during their illness. This study identified health service utilization was decided by another (caregiver/husband) for 34% of women, unlike males that were 15%. Babar T. Shaikh and Juanita Hatcher reported that women have less autonomy in seeking medical care as compared to males in developing countries.28 Similar to the previous studies conducted in developing countries.12,13,26,29 Lower economic status was found to be a factor that was positively associated with poor HSB. Being in lower economic status increases the odds of poor HSB among the elderly in West Shoa. This could be because of un-affordability of modern medical care services for economically disadvantaged populations. Thus, they may rely on alternative care. A study conducted in Bangladesh also reported that poverty was an important predictor of HSB among elderly.30
The behavior of the elderly (smoking status) was also identified as an important determinant of HSB. This might be because of the severity of illness among smokers as compared to a non-smoker. The study done in the Turkish Republic of Northern Cyprus also identified that smoking increases the odds of HSB.31
Having CBHI coverage plays an important role in the HSB of the elderly. Hence, not having CBHI coverage increases the probability of poor HSB by four times. Previous studies conducted in Ethiopia also reported that being a member of CBHI increases the utilization of health service.32,33 This might be because of the fact that those who have CBHI coverage can utilize health services free of charge once they pay an annual insurance. Thus, having health insurance increases their affordability of medical care. This calls that the government should increase the coverage of CBHI for those vulnerable populations.
Self-perceived severity of illness is a morbidity condition that was found to be an independent predictor of HSB. The same finding was reported by a similar study done in Nigeria that reports the nature of the illness is the major factor that was associated with HSB.13 Self-medication is also an independent predictor of HSB among the geriatric population. This could be because people may get relief for their illness if they take medication especially anti-pain; as the majority of the study participant included in this study reported that they were suffering from musculoskeletal problems like arthralgia and myalgia. On the other hand, people may choose self-medication than seeking medical care from a physician because of poor economic status, lack of health insurance, for mild illness and prior use of medication.34–36
The presences of chronic disease (hypertension, DM, and Oro-dental problems) were the morbidity pattern identified as positive independent predictors of good HSB. A similar finding was reported by the study conducted in Bedele town, Ethiopia.17 However, the current study identified that those who had musculoskeletal problems more likely to have poor HSB. This may be because this problem is not acute and it is not a life-threatening problem. Again, it may manifests with the same symptom of previous illness, thus they might learn how to manage it through self-medication. Thus, people may practice self-medication, as this study also identified self-medication was positively associated with poor HSB. On the other hand, the elderly may associate the musculoskeletal problems with aging.
This study was interpreted with the limitation of being self-reported morbidity or provisional diagnosis and HSB assessment; however, the authors believe that under or over-reporting may balance each other. Even though the authors tried to reduce recall bias using memorable local calendar, still there might be a recall bias. Moreover, some of the diseases may not have any symptom or signs (undiagnosed at time of data collection) which contributes for under reporting of the morbidity level.
Conclusion and Recommendations
There was a high prevalence of morbidity and poor HSB among the geriatric population in the West Shoa Zone of Ethiopia. Residence, wealth status/index,occupation (being housewife), and being the head of a polygamous household were the socio-demographic factors that were significantly associated with HSB. There should be an effort to improve the social structure of the geriatric population to improve their HSB.
This could be improved through offering free health care services or reduction of health care costs for geriatric populations. Besides, improving their income may also improve their HSB. Thus, health policymakers should consider making geriatric health care free of charge or cost reduction to avoid health care disparity owing to low income. Other stakeholders working on the economy of the community should also consider improving the economic status of the geriatric population or any possible alternative. For instance, the availability of CBHI is one of the health system factors that were found to be the independent predictor of HSB in the study area. Thus, the West Shoa health sector administration should strengthen CBHI for the geriatric population as one alternative to improve their HSB.
Data Sharing Information
The data sets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to thank Ambo University for funding this study. Indeed, we appreciate the data collectors and study participants for their endless cooperation.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; agreed on the journal to which the article will be submitted and agree to be accountable for all aspects of the work.
Funding
The source of funding was Ambo University.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Tao P, Lin MH, Peng LN, et al. Reducing the burden of morbidity and medical utilization of older patients by outpatient geriatric services: implications to primary health‐care settings. Geriatr Gerontol Int. 2012;12(4):612–621. doi:10.1111/j.1447-0594.2011.00823.x
2. Economic Do, Nations SAU. World Population Ageing: 1950-2050. UN; 2002.
3. CentralStatisticalAgency. Population Projection of Ethiopia; 2007-2037. Federal Democratic Republic of Ethiopia, Population Census Commission; 2013.
4. Nations U. Current Status of the Social Situation, Well-Being, Participation in Development and Rights of Older Persons Worldwide. New York; 2011.
5. de Bruijn J. Global age watch index 2015, London, 2015, ch 8 Western Europe, North America and Australasia. Global Age Watch Index. 2015.
6. FederalDemocraticRepublicofEthiopia. National social protection policy of Ethiopia. Final Draft’, Ministry of Labour and Social Affairs, Addis Ababa, Ethiopia. 2012.
7. The State of Health and Ageing in Ethiopia: A Survey of Health Needs and Challenges of Service Provisions. Addis Ababa, Ethiopia: HelpAge International in Ethiopia; 2013.
8. Eneyew A, Bekele W. Analysis of wealth and livelihood capitals in Southern Ethiopia: a lesson for policy makers. Curr Res J Soc Sci. 2013;5(1):1–10. doi:10.19026/crjss.5.5533
9. Vulnerability of Older People in Ethiopia: The Case of Oromia, Amhara and SNNP Regional States. Addis Ababa: HelpAge Intenational; 2013.
10. Conner M, Sparks P. The theory of planned behaviour and health behaviours. In: Conner M, Norman P, editors. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Maidenhead, BRK England: Open University Press; 1996.
11. Shukla M, Ahmad S, Brajesh Anand P, Ranjan R. A study on health care seeking behaviour among elderly in a rural area of eastern Uttar Pradesh. Natl J Multidisciplinary Res Develop. 2017;2(2):15–18.
12. Patle RA, Khakse GM. Health-seeking behaviour of elderly individuals: a community-based cross-sectional study. Natl Med J India. 2015;28(4):181–184.
13. Abdulraheem I. Health needs assessment and determinants of health-seeking behaviour among elderly Nigerians: a house-hold survey. Ann Afr Med. 2007;6(2):58. doi:10.4103/1596-3519.55715
14. Falaha T, Worku A, Meskele M, Facha W. Health care seeking behaviour of elderly people in rural part of Wolaita Zone, Southern Ethiopia. Health Sci J. 2016;10(4):1.
15. Terfa Y, Germossa G, Hailu F, Feyisa G, Jeleta F. Determinants of health care utilization among the elderly population in Jimma Town, Oromia Region, Southwest Ethiopia. Int Arch Nurs Health Care. 2019;5:131.
16. Neme A. Assessment of factors influencing health seeking behaviors of elderly in Bilida Kebele, Manna Woreda, Jimma Zone, South West Ethiopia. J Public Health Dis Preventive. 2018;1:103.
17. Amente T, Kebede B. Determinants of health service utilization among older adults in Bedele Town, illubabor zone, Ethiopia. J Diabetes Metab. 2016;7(11):1–7. doi:10.4172/2155-6156.1000713
18. CentralStatisticalAgency, ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
19. Baral R, Sapkota P. Health seeking behaviour among elderly people of bharatpur municipality of Chitwan, Nepal. J Coll Med Sci. 2018;14(3):150–153. doi:10.3126/jcmsn.v14i3.21178
20. Gupta E, Thakur A, Dixit S. Morbidity pattern and health seeking behavior of the geriatric population in a rural area of district Faridabad, Haryana: a cross-sectional study. Int J Commun Med Public Health. 2019;16:3.
21. Sharma D, Mazta SR, Parashar A. Morbidity pattern and health-seeking behavior of aged population residing in Shimla hills of north India: a cross-sectional study. J Fam Med Prim Care. 2013;2(2):188. doi:10.4103/2249-4863.117421
22. Barua K, Borah M, Deka C, Kakati R. Morbidity pattern and health-seeking behavior of elderly in urban slums: a cross-sectional study in Assam, India. J Fam Med Prim Care. 2017;6(2):345. doi:10.4103/2249-4863.220030
23. Ahmed SM, Tomson G, Petzold M, Kabir ZN. Socioeconomic status overrides age and gender in determining health-seeking behaviour in rural Bangladesh. Bull World Health Organ. 2005;83:109–117.
24. Waweru L, Kabiru E, Mbithi J, Some E. Health status and health seeking behaviour of the elderly persons in Dagoretti division, Nairobi. East Afr Med J. 2003;80(2):63–67.
25. Frontera WR. Physiologic changes of the musculoskeletal system with aging: a brief review. Phys Med Rehabilitation Clin. 2017;28(4):705–711.
26. Srivastava S, Gill A. Untreated morbidity and treatment-seeking behaviour among the elderly in India: analysis based on National Sample Survey 2004 and 2014. SSM-Population Health. 2020;10:100557. doi:10.1016/j.ssmph.2020.100557
27. Anselmi L, Lagarde M, Hanson K. Health service availability and health seeking behaviour in resource poor settings: evidence from Mozambique. Health Econ Rev. 2015;5(1):26. doi:10.1186/s13561-015-0062-6
28. Shaikh BT, Hatcher J. Health seeking behaviour and health service utilization in Pakistan: challenging the policy makers. J Public Health (Bangkok). 2005;27(1):49–54. doi:10.1093/pubmed/fdh207
29. Adhikari D, Rijal DP. Factors affecting health seeking behavior of senior citizens of Dharan. J Nobel Med Coll. 2014;3(1):50–57. doi:10.3126/jonmc.v3i1.10055
30. Cain MT. The activities of the elderly in rural Bangladesh. Popul Stud. 1991;45(2):189–202. doi:10.1080/0032472031000145386
31. Abuduxike G, Aşut Ö, Vaizoğlu SA, Cali S. Health-seeking behaviors and its determinants: a facility-based cross-sectional study in the Turkish Republic of Northern Cyprus. Int J Health Policy Manage. 2020;9(6):240–249.
32. Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8(8):e019613. doi:10.1136/bmjopen-2017-019613
33. Demissie B, Negeri KG. Effect of community-based health insurance on utilization of outpatient health care services in Southern Ethiopia: a comparative cross-sectional study. Risk Manag Healthc Policy. 2020;13:141. doi:10.2147/RMHP.S215836
34. Shafie M, Eyasu M, Muzeyin K, Worku Y, Martin-Aragon S. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One. 2018;13(3):e0194122. doi:10.1371/journal.pone.0194122
35. Sisay M, Mengistu G, Edessa D. Epidemiology of self-medication in Ethiopia: a systematic review and meta-analysis of observational studies. BMC Pharmacol Toxicol. 2018;19(1):56. doi:10.1186/s40360-018-0248-8
36. Nakhaee M, Vatankhah S. Prevalence and cause of self-medication in Iran: a systematic review and meta-analysis on health center based studies. J Biochem Tech. 2019;2:90–105.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.