Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Secondary Traumatic Stress Disorder Among Physiotherapists Working in High Morbidity Departments: A Cross-Sectional Study
Authors Shalabi KM , Alshraif ZA, Ismail RI, Almubarak K, Mohmoud N , Shaik SA
Received 28 June 2023
Accepted for publication 13 October 2023
Published 6 November 2023 Volume 2023:16 Pages 3287—3297
DOI https://doi.org/10.2147/JMDH.S428034
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Kholood M Shalabi,1 Zahra A Alshraif,2 Rawaa Ismail Ismail,3 Kheloud Almubarak,2 Noha Mohmoud,1 Shaffi A Shaik4
1Rehabilitation Sciences Department, College of Health and Rehabilitation Sciences, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia; 2Rehabilitation Services Department, King Abdullah University Hospital, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia; 3College of Medicine, Almaarefa Colleges, Riyadh, Saudi Arabia; 4Family and Community Medicine Department, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Shaffi A Shaik, Department of Family & Community Medicine, College of Medicine, King Saud University, Riyadh, 11426, Saudi Arabia, Tel +966-11-4671544, Email [email protected]; [email protected]
Purpose: This study’s objective was to measure secondary traumatic stress disorder among Saudi Arabian physiotherapists employed in the critical care, neurology, cardiology, pulmonology, and mental health fields. Also, to identify the factors related to secondary traumatic stress.
Methods: Between July 2021 and June 2022, a cross-sectional study involving physiotherapists from the critical care, emergency, neurology, cardiology, pulmonology, and mental health departments was carried out. Data were collected from the participants by using the validated Secondary Traumatic Stress Scale (STSS). Appropriate Statistical analysis (bivariate and multivariate) was carried using SPSS 21.0 software to analyse the data.
Results: We quantified the prevalence of secondary traumatic stress, among 201 healthcare professionals (physiotherapists) in total were assessed; of them, 23.4% worked in the medical/surgical and neurosurgical departments and 5% in the critical care and emergency departments. Twenty-four percent of the participants slept less than five hours each day, and 26.4% worked more than 45 hours per week. Our study subjects had mild STS in 25.4% of cases, moderate stress in 15.9%, high STS in 15.9% and severe STS in 30.9% of cases. The intrusion score (mean = 11.65), avoidance score (mean = 5.5), arousal score (mean = 4.1) and total mean score of 42.50 of the STSS were significantly different across the age groups, marital status and years of experience of study participants. The regression analysis shows age groups and severe stress were independently related to the total STS scores.
Conclusion: The study has found out higher level of STS among physiotherapists which highlights the necessity for a variety of interventional programs to be implemented in hospital settings in order to enhance communication abilities, lessen emotional discomfort, and apply relaxing techniques.
Keywords: stress, secondary traumatic stress disorder, burnout, healthcare workers, physiotherapists, depression
Introduction
Secondary Traumatic Stress (STS) Disorder is the natural consequent behaviors resulting from knowledge about a traumatizing event experienced by the other person. It is the stress resulting from helping or wanting to help a traumatized or suffering person.1 In health sector, healthcare personnel will come across the instances which cause them STS. STS leads to the development of symptoms of post-traumatic stress disorder after direct or indirect exposure to trauma. The symptoms of STS can negatively impact professionals of health care.2 The mental and psychological health of healthcare personnel is negatively impacted by working in the field.1–3 In high-morbidity disciplines including emergency and critical care,4,5 neurology,6–9 cardiology,10 pulmonology,11 and mental health,12–16 healthcare professionals (HCPs) are particularly susceptible to psychological impairment. HCPs who are caring for those patients may experience comparable emotions after hearing about their suffering, discomfort, and concerns.17–19 Totally, 67.7% of doctors, 59.3% of emergency medical technicians, 53.8% of paramedics, 62.5% of health officers, 30% of nurses, and 80% of anaesthesia technicians were affected by a trauma that someone they treated or cared for had experienced, according to a study on the association between secondary traumatic stress (STS) and occupation.20
Among HCPs caring for patients in emergency departments (EDs), STS disorder entails the emergence of symptoms connected to indirect exposure to trauma or post-traumatic stress disorder (PTSD). It happens among doctors and HCPs caring for patients with a range of health issues who are part of traumatized populations.17 HCPs’ health may be negatively impacted by STS symptoms because they are more likely to make careless professional judgments on their patients’ treatment, such as incorrect diagnosis, shoddy treatment planning, or even mistreatment of patients.17,21–24
It is necessary for the doctor to receive therapy for STS disorder if STS manifests as the typical PTSD symptoms.25 Hypervigilance, intrusion, irritation, and avoidance/numbing are some of the symptoms of STS. Most critically, traumatic event-related symptoms can repeatedly recur in HCPs. It is connected with intrusion-associated clustering symptoms and can involve memories of past events as thoughts, perceptions, or visual representations.
Physical therapists (PTs) have also been found to have significant prevalence of Compassion Fatigue (CF) in several American, European, and Middle Eastern nations. Due to repeated exposure to second-hand trauma from the patients, physical therapists experience emotional and behavioural changes which leads to stress and compassion fatigue which include burnout and secondary traumatic stress.26–29 Acute care and rehabilitation, primary care, prevention, and public health are just a few of the specialties that physical therapists contribute to in today’s multidisciplinary healthcare teams.30 ED-PTs are in charge of treating patients with semi-urgent and non-urgent musculoskeletal problems. Patients are interviewed and examined, tests, including X-rays are ordered, diagnoses are made, relevant therapies are put into action, patients are referred for continuous management, and patient release is coordinated.31 As more PTs are employed in hospital EDs, they may also help with the care of patients with acute respiratory issues (by performing secretion clearing procedures, for example) or assist patients in their transition from ED discharge back into the community in an effort to reduce avoidable hospitalizations. Healthcare outcomes for patients treated by PTs in the ED have only been examined in a small number of research,32 but overall, the findings are favourable. Similar clinical outcomes (namely pain, function, and representation rate) among patients treated under the traditional ED model show that ED-PTs are capable of managing peripheral soft tissue injuries.33,34 PTs can help patients get started on the road to recovery early in the healing process after particular injury types.35 How far PTs advance along the compassion continuum may depend on their practice setting in addition to the degree of STS they have encountered. PTs may experience higher levels of STS if they live and operate in humanitarian emergencies such war zones,36 regions where there is civil instability,37 or catastrophe zones.38 However, there is a lack of information on the prevalence of STS among PTs who toil away treating debilitating conditions like Parkinson’s disease, muscular dystrophy, arthritis, and other bone diseases, as well as progressive conditions like heart failure and cancer, and who spend hours with patients and form strong bonds with them, particularly in the Middle Eastern nations like Saudi Arabia. It is important to accurately analyze STS dysfunction depending on occupation rather than from a general standpoint of all HCPs. It is necessary to establish suitable planning parameters, for which fundamental facts are needed from each setup.
This study focused on investigating the STS among PTs working in critical care, emergency, neurology, cardiology and pulmonology departments in Saudi Arabia. Managers and organizations who want to support clinician skill development and use STS management methods may find our study to be helpful. The study might improve knowledge of the difficulties and constraints faced by PTs in the ED.
Materials and Methods
Ethical Considerations
The Institutional Review Board of Princess Nourah bint Abdulrahman University’s Ethical Committee granted permission to conduct the study (IRB Approval # HAP-01-R-059). All PTs who accepted to take part in the study provided written informed consent, and their information was kept private. Also our study complies with the declaration of Helsinki.
Participants and Study Design
Between July 2021 and June 2022, PTs who worked in high mortality speciality departments, such as the emergency, critical care, neurology, pulmonology, and cardiology departments, participated in this cross-sectional study. PTs received invitations to participate in the study via email and WhatsApp. The email ids of PTs were obtained from the human resources department of their hospitals. A link to a Google Form-based online survey that collected demographic data and evaluated levels of STS dysfunction was sent to those who accepted to participate.
Survey Structure and Questions
There were two components to the survey. Questions about demographic information, such as age, gender, nationality, occupational state, marital status were included in the first portion. Additionally, it included questions on the PTs’ employment and experience, including their current department of practice, years of experience, number of hours worked each week, number of hours slept each day, and degree of felt job stress.
The STS scale was used in the second section to assess STS dysfunction. The reliability of this scale in this study was found to be high with Cronbach’s alpha coefficient of 0.923.
Sample Size
Based on the descriptive results of a pilot study of 10 subjects the sample size for the main study was calculated with a prevalence of STS as 20%, with a precision of ±6% at 0.05 level of significance and assuming 20% non-response a total of 205 subjects were targeted. But a total of 201 subjects were responded, of which 156 (77.6%) were female and 45 (22.4%) were male subjects.
Secondary Traumatic Stress Scale (STSS)
A 17-item self-administered questionnaire called the STSS is used to gauge how frequently STS symptoms occur.39 Participants are asked to rate how frequently they encountered each of the 17 symptoms over the course of the previous seven days on a five-point scale ranging from “never” to “very often” (0 = Never, 1 = Rarely, 2 = A Few Times, 3 = Somewhat Often, 4 = Often, and 5 = Very Often). The 17 items were created to evaluate the intrusion, avoidance, and arousal subscales.
Based on the scoring instructions for the scale, the STSS was manually scored.40 A higher score denotes a higher frequency of symptoms, and the total score was derived by adding the item scores. A score of less than 28 indicated little or no STS in the person. Participants who received a score between 28 and 37 had mild STS. Participants who had a score of 38 to 43 had moderate STS. A person had high STS if their score fell between 44 and 48, and severe STS if it reached 49 or above. Items 2, 3, 6, 10, and 13 were added together to determine the incursion score. The arousal score was obtained by adding items 4, 8, 11, 15, and 16 to the avoidance score, which was derived by adding items 1, 5, 7, 9, 12, 14, and 17.
Statistical Analysis
The statistical program SPSS 26.0 (IBM Inc., Chicago, USA) was used to analyze the data. The quantitative variables (scores of the three factors and total score of all items of the secondary traumatic stress scale) and categorical responses of sociodemographic and professional characteristics were described using descriptive statistics (mean, standard deviation, frequencies, and percentages). To compare the means of the three factors (Intrusion, Avoidance, and Arousal) and the overall mean score of all items of the secondary traumatic stress scale across the demographic professional characteristics of subjects that had two and more than two categories as well as across the four categories of stress level that were reported by the study subjects, we used the Student’s t-test for independent samples and one-way analysis of variance followed by Tukey’s post hoc test. Multiple linear regression was used to identify the independent variables related to the total STS scores (dependent variable). Dummy variables were created for the categorical independent variables. Coefficient of variability (R-square) and regression coefficients were used to report the significance of the model and the independent variables. To report the results’ statistical significance, a p-value of = 0.05 was employed.
Results
Table 1 displays the demographic characteristics and other information of the 201 participating subjects. According to the study participants’ subjective assessments of their job-related stress levels, 13.9% of them experienced severe stress, 5% had no stress, and the rest participants experienced mild to moderate stress. The mean values of the 17 items on the secondary traumatic stress scale are shown in Table 2, with the minimum mean value related to the item “I had disturbing dreams about my work with clients” and the maximum mean value related to the item “I felt discouraged about the future.” The mean values of these 17 items range from 1.95 to 2.95.
 |
Table 1 Socio-Demographic Characteristics of Study Subjects (n = 201) |
 |
Table 2 Descriptive Statistics of Study Subject’s Responses Towards 17 Items of Secondary Traumatic Stress Scale |
In Table 3, the mean values of the three factors (intrusion, avoidance and arousal) scores and the scale’s overall score are displayed. And the prevalence of STS level indicates that 30.3% of subjects had severe STS, 15.9% of them high and moderate STS, 25.4% had mild STS and only 12.4% of them had little or no STS.
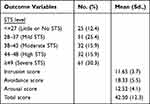 |
Table 3 Distribution of Prevalence of STS Level and Descriptive Statistics of Total Score and 3 Factors of STS Scale Among the Study Subjects (n = 201) |
The comparison of mean values of three factors (Intrusion, Avoidance & Arousal) and the total score of STS scale shows high statistical significant difference in the mean values of these three factors and total score in relation to the age groups, nationality, marital status and years of experience. For nationality, Non-Saudi subjects were having higher mean values of three factors and total score when compared with the mean values of Saudi subjects. And for marital status, divorced subjects were having higher mean values of three factors and total score of STS scale when compared with the mean values of subjects who were single and married. The corresponding p-values can be seen in Tables 4 and 5. The post-hoc test indicated that the mean values of three factors and total score were significantly higher in younger age groups (23–30 and 31–40) when compared with the two other age groups (41–50 and 51–60) and significantly higher in subjects who had lower years of experience (<5, 5–10 and 11–15) when compared with the subjects who had higher years of experience (16 −20 and >20). In relation to the gender, female subjects were having higher intrusion mean value when compared with male subjects (p = 0.037) and no significant difference between male and female subjects for mean values of Avoidance and Arousal and total mean score of STS scale. Also, there was no statistically significant difference in the mean values of three factors (intrusion, avoidance and arousal) and total score of STS scale in relation to the individuals’ departments, working hours per week and sleeping hours (Tables 4 and 5).
 |
Table 4 Comparison of Mean Values of 3 Factors Scores of Secondary Traumatic Stress Scale Across the Socio-Demographic Characteristics of Study Subjects |
 |
Table 5 Comparison of Mean Values of Total Score of Secondary Traumatic Stress Scale Across the Socio-Demographic Characteristics of Study Subjects |
When the study subject’s subjective response to the four categories of stress level of their job was compared to the mean values of the three factors (Intrusion, Avoidance, and Arousal) and the total scores of the secondary traumatic stress scale, there was a statistically significant difference between the three factors’ mean scores (p = 0.002, p = 0.002, p = 0.001, and p < 0.0001). In other words, compared to participants who reported being under moderate, mild, or no stress, subjects who reported being under severe stress had mean intrusion factor scores that were considerably higher. Intrusion factor mean values of subjects with moderate, mild, and no stress did not differ from one another according to the post-hoc test (p > 0.05). Additionally, when compared to mean scores of participants who replied with moderate, mild, or no stress, the mean value of avoidance factor scores among subjects who had responded as experiencing severe stress was statistically considerably greater. Additionally, the post-hoc test revealed no significant differences between the mean avoidance factor values of subjects with moderate, mild, and no stress (p > 0.05). And when compared to the mean score of respondents who replied with moderate, mild, or no stress, the mean value of arousal factor scores among subjects who had responded as having severe stress was statistically considerably greater. Furthermore, the post-hoc analysis revealed no significant differences in the mean arousal component values across subjects with moderate, mild, and no stress (p > 0.05). Additionally, when compared to the overall mean score of respondents who reported being under severe, moderate, or no stress, the mean value of the total score in the severe stress group was statistically considerably greater (p < 0.0001). Additionally, the post-hoc analysis revealed no significant difference between the mean total scores of subjects with moderate, mild, and no stress (p > 0.05) (Table 6).
 |
Table 6 Comparison of Mean Values of 3 Factors and Total Score of Secondary Traumatic Stress Scale in Relation to the Job-Related Stress Levels of Study Subjects |
Multivariate Analysis
The multiple linear regression analysis was carried out, with STS total scores as dependent variables and the bivariate significant variables: age groups (23–30, 31–40,41–50, 51–60); Nationality (Saudi & Non-Saudi), Marital status (Single, married and divorced); Years of experience (<5, 5–10, 11–15, 16–20 and >20) and study subject subjective response towards their job-related stress level (no stress, mild stress, moderate stress and severe stress) as independent variables in the model. The step-wise regression analysis at step3 shows Age groups (23 to 30 and 31 to 40) and stress level (severe) are statistically significantly related to the total STS scores. That is, the total STS scores on average increases by 14.755 and 9.282 units in subjects of age group 23 to 30 years and 31 to 40 when compared with subjects of 41 to 50 years which is highly statistically significant (p < 0.0001). And the total STS scores on average increase by 10.531 units in subjects who expressed as having severe stress when compared with the subjects who had expressed as having no stress, which is highly statistically significant (p < 0.0001). The model provides an R-square value of 0.244, which indicates 24.4% of change in total STS scores were explained by these three independent variables (Table 7).
 |
Table 7 Stepwise Multiple Linear Regression Analysis for Relationship Between the Total Score of Secondary Traumatic Stress Scale and Independent Variables |
Discussion
This study examined STS and the potential trauma or distress that physical therapists working in critical care, emergency, neurology, cardiology, and pulmonology departments may experience. PTs are exposed to a variety of stress and trauma-related phenomena that can harm and upset them emotionally. The study has found the prevalence of severe STS level, subjective opinion of their stress level, total STS score and the factors independently associated with STS. As per the study subject’s subjective opinion, only 5% of the participants in our study reported no stress, compared to 13.9% who reported severe stress and the remaining 81.1% who reported to have mild to moderate stress level of their job. But the prevalence of STS using the scale, it was found that 30.3% of them had severe STS, 12.4% had little or no STS and the remaining 57.2% of them had mild to high STS. This shows that PTs and other emergency healthcare workers (HCWs) still have high STS levels.
Their capacity to manage and carry out their responsibilities to the best of their abilities may be diminished by STS.17,21 A study by Li et al41 found that STS has a detrimental effect on both medical and non-medical workers, including PTs. Additionally, it has a more significant impact on non-frontline medical professionals than it does on front line medical personnel.41
In a study conducted by Orru et al during the COVID-19 outbreak with participants from 45 different nations, STS prevalence was observed to be 47.5% in frontline HCWs and 30.3% in other units.42 Research by Duffy et al43 and Dominguez-Gomez et al44 on emergency nurses revealed that STS prevalence rates were 64% and 33%, respectively, prior to the COVID-19 pandemic. We believe that spending more than a year on the front lines, while unsure of when things may change, is detrimental to the psychological health of emergency HCPs, given that only 5% of the participants in our study showed no symptoms of STS, and the remaining 95% had severe to moderate STS symptoms. To compensate and lessen their stress levels, emergency HCPs need quick financial and professional assistance. By doing so, they will be able to provide great healthcare, including PTs in the ED. Numerous studies, such as a systematic review and meta-analysis, have revealed that during a pandemic like COVID-19, HCPs, especially PTs, suffer from significant levels of stress-related disorders, like anxiety, depression, insomnia, and hopelessness because they must rehab infected patients, which is labour-intensive.17,19,22 The mean STS score of all items in this study was found to be 42.50 which is very close to STS mean of 41.19 as reported by Oginska and Michalska and they had concluded that STS is positively associated with job burnout.45 In other study by Kintzle et al had obtained a mean STS score of 30.76 among military primary and mental health care providers, which is much less than the present study mean score22 In that study the authors had listed out the various factors such as Education level and experience of study subjects which were contributed to the lower levels of STS. In our study also, the STS scores are lower in subjects whose working experience years increases.
The results of the current study showed that there were significant differences between the mean total STSS scores for the age groups of 23–30 and 40–50 years (p > 0.05). The fact that freshly employed, young HCPs or PTs with little psychological training are usually assigned to frontline services may be a contributing factor in their high incidence of STS. The results of the study demonstrate a connection between good physical health and good mental health in addition to the wisdom that comes with age and experience.44 The STS scores for the age groups of 40–50 and 50–60 in our study were not significant as a result. Robert et al’s study, which found that psychological resilience increases with age and becomes stronger to handle such circumstances, provided additional substantial evidence for this.46 The fact that mean scores are statistically significantly higher when comparing workers with 5, 5–10, and 11–15 years of experience when compared to their colleagues with 16–20 and >20 years of experience demonstrates that HCPs with more than 20 years of experience in the healthcare industry are more psychologically resilient.40 Additionally, there were statistically significant variations in the mean total STSS scores among the other research participants’ characteristics, like marital status. Married HCPs (including PTs) may be more emotionally strong due to their spouse’s support.
Participants in the four age groups gave responses that exhibited signs of intrusive thoughts, avoidance as a coping mechanism, and alertness in the presence of environmental signals. The results show that PTs aged 23–30 years and 30–40 years have higher levels of STS than PTs in other age groups (40–50 years and 50–60 years). Studies on STS among doctors and nurses during the COVID-19 pandemic done in India showed that younger HCPs also exhibited high STS as a result of their close contact and involvement with pandemic-related activities and patients.46,47 Despite the lack of comparable data for the pandemic and STS among HCWs in Saudi Arabia, other regional studies have found a relation between STS and the careers of HCPs such doctors, nurses, and other healthcare professionals.48,49 Research on STS also demonstrates that it can affect how HCPs interact with their partners and kids as it develops. Serving traumatized patient populations with difficult conditions or trauma might cause them to experience considerable amounts of relationship discomfort.25–50 It can also have a detrimental effect on their productivity and affect their psychological well-being. It can also result in crippling disorders like despair and anxiety. HCPs may experience burnout and lowered morale over time, which might hinder their capacity to accomplish their desired objectives. Studies have also demonstrated the emotional and psychological ties that carers and patients have.39
The first drawback of our study is that it only included HCWs, namely PTs working in EDs, and it used a cross-sectional study design. Second, the method of participant recruitment (a Google form disseminated on social media) may have biased the results by over representing tech-savvy people. Third, the limited sample size makes it difficult to extend the results to the total population of HCWs, particularly PTs. Fourth, the pandemic situation, which has increased the workload and sparked safety concerns, may have had an impact on the levels of STS and the overall STSS ratings.
Conclusions
There is strong evidence that HCWs, particularly PTs, who work in the emergency, critical care, neurology, cardiology, pulmonology, and mental health departments experience STS problem. STS levels were greater in the age categories of 23 to 30 and 30 to 40, besides who have less years of years of experience and reported to be under severe stress level of their job. By creating a happy environment in the hospital, HCWs might be alleviated of their mental and emotional stress. In order for HCWs to be motivated, resilient, and able to change their thinking toward beneficial parts of managing their patients with compassion and care, it is vital to relieve them of their emotional, cognitive, and physical pain.
Acknowledgments
We acknowledge all the research participants.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress in Those Who Treat the Traumatized. Brunner/Mazel Publishers; 1995.
2. Yehya A, Sankaranarayanan A, Alkhal A, et al. Job satisfaction and stress among healthcare workers in public hospitals in Qatar. Arch Environ Occup Health. 2020;75(1):10–17. doi:10.1080/19338244.2018.1531817
3. Raudenská J, Steinerová V, Javůrková A, et al. Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pract Res Clin Anaesthesiol. 2020;34(3):553–560. doi:10.1016/j.bpa.2020.07.008
4. Hofmann PB. Stress among healthcare professionals calls out for attention. J Healthc Manag. 2018;63(5):294–297. doi:10.1097/JHM-D-18-00137
5. Ibrahim MA, Isa KQ, Haji-Idris H-A, et al. Spiritual coping with stress among emergency and critical care nurses: a cross-sectional study. Commun Ment Health J. 2020;56(2):287–293. doi:10.1007/s10597-019-00486-6
6. Santana RDS, Fontes FLL, Morais MJA, et al. Occupational stress among emergency and urgent care nurses at a public hospital in Teresina, Piaui, Brazil. Rev Bras Med Trab. 2020;17(1):76–82. doi:10.5327/Z1679443520190295
7. Pu J, Zhou X, Zhu D, et al.; China Neurologist Association. Gender differences in psychological morbidity, burnout, job stress and job satisfaction among Chinese neurologists: a national cross-sectional study. Psychol Health Med. 2017;22(6):680–692. doi:10.1080/13548506.2016.1211717
8. Kristoffersen ES, Winsvold BS, Sandset EC, Storstein AM, Faiz KW. Experiences, distress and burden among neurologists in Norway during the COVID-19 pandemic. PLoS One. 2021;16(2):e0246567. doi:10.1371/journal.pone.0246567
9. Moore LR, Ziegler C, Hessler A, Singhal D, LaFaver K. Burnout and career satisfaction in women neurologists in the United States. J Womens Health. 2019;28(4):515–525. doi:10.1089/jwh.2017.6888
10. Al-Qahtani ZA, Alhazzani A. Prevalence of burnout among neurologists in Saudi Arabia. Egypt J Neurol Psychiatr Neurosurg. 2021;57(1). doi:10.1186/s41983-021-00309-0
11. Roz HKB, Mondal S, Podder P, Raval DT. A study on occupational stress and burnout among cardiologists: a cross-cultural perspective. Indian J Health Wellbeing. 2016;7(3):282–288.
12. Ruxandra-Mioara R, Armand-Gabriel R, Sabina AA, et al. Work-related stress factors and coping behaviour among pneumologists. Acta Medica Mediterr. 2020;36(5):2893–2899. doi:10.19193/0393-6384_2020_5_443.
13. Dhandapani A, Armugam SS, Chaturvedi SK. Professional stress among psychiatrists–a Delphi study. Eur Psychiatry. 2016;33(S1):S167–S167. doi:10.1016/j.eurpsy.2016.01.340
14. Coker A, Omoluabi P. Burnout and stress reaction among psychiatrists working in Lagos, Nigeria. IFE Psychol. 2010;18(1). doi:10.4314/ifep.v18i1.51647
15. Hardy P, Costemale-Lacoste JF, Trichard C, et al. Comparison of burnout, anxiety and depressive syndromes in hospital psychiatrists and other physicians: results from the ESTEM study. Psychiatry Res. 2020;284:112662. doi:10.1016/j.psychres.2019.112662
16. da Silva HC, da Rosa MM F, Berger W, et al. PTSD in mental health outpatient settings: highly prevalent and under-recognized. Rev Bras de Psiquiatr. 2019;41(3):213–217. doi:10.1590/1516-4446-2017-0025
17. Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):100. doi:10.1186/s12960-020-00544-1
18. Robins PM, Meltzer L, Zelikovsky N. The experience of secondary traumatic stress upon care providers working within a children’s hospital. J Pediatr Nurs. 2009;24(4):270–279. doi:10.1016/j.pedn.2008.03.007
19. Algamdi M. Prevalence of oncology nurses’ compassion satisfaction and compassion fatigue: systematic review and meta-analysis. Nursing Open. 2022;9(1):44–56. doi:10.1002/nop2.1070
20. Laor-Maayany R, Goldzweig G, Hasson-Ohayon I, Bar-Sela G, Engler-Gross A, Braun M. Compassion fatigue among oncologists: the role of grief, sense of failure, and exposure to suffering and death. Support Care Cancer. 2020;28(4):2025–2031. doi:10.1007/s00520-019-05009-3
21. Pak MD, Özcan E, Çoban AI. Secondary traumatic stress level and psychological resilience of emergency service staff. J Int Soc Res. 2017;10(52):629–644.
22. Kintzle S, Yarvis JS, Bride BE. Secondary traumatic stress in military primary and mental health care providers. Mil Med. 2013;178(12):1310–1315. doi:10.7205/MILMED-D-13-00087
23. Bercier ML, Maynard BR. Interventions for secondary traumatic stress with mental health A systematic review. Res Soc Work Pract. 2015;25(1):81–89. doi:10.1177/1049731513517142
24. Ogińska-Bulik N, Gurowiec PJ, Michalska P, Kędra E. Prevalence and predictors of secondary traumatic stress symptoms in health care professionals working with trauma victims: a cross-sectional study. PLoS One. 2021;16(2):e0247596. doi:10.1371/journal.pone.0247596
25. Devilly GJ, Wright R, Varker T. Vicarious trauma, secondary traumatic stress or simply burnout? Effect of trauma therapy on mental health professionals. Aust N Z J Psychiatry. 2009;43(4):373–385. doi:10.1080/00048670902721079
26. Newell JM, MacNeil GA. Professional burnout, vicarious trauma, secondary traumatic stress, and compassion fatigue. Best Pract Ment Health. 2010;6(2):57–68.
27. Klappa SG, Fulton LE, Cerier L, Peña A, Sibenaller A. Compassion fatigue among physiotherapist and physical therapists around the world. Glob J Med Physl Health Edu. 2015;3(5):124–137.
28. T PD, Khanwelkar C, Patil A, et al. Compassion fatigue among Indian physiotherapists: a descriptive cross sectional comparative study. Global Bioeth Enq J. 2019;7(1):17. doi:10.38020/gbe.7.1.2019.17-22
29. Palombaro KM, Erdman EA, McArdle KD, Black JD, Stewart AR, Jones SA. High civic-mindedness reduces compassion fatigue in the first 3 years of professional physical therapist practice: a pilot study. J Patient Exp. 2020;7(5):771–777. doi:10.1177/2374373519891346
30. Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–465. doi:10.1111/jnu.12229
31. Berry JW, Schurhammer NL, Haugen TJ, Piche SE, Buskness SL, Wentz JL. Job satisfaction and productivity requirements among physical therapists and physical therapist assistants. J Allied Health. 2022;51(1):e33–e38.
32. Anaf S, Sheppard L. Physiotherapy as a clinical service in emergency departments: a narrative review. Physiotherapy. 2007;93(4):243–252.
33. Kilner E. What evidence is there that a physiotherapy service in the emergency department improves health outcomes? A systematic review. J Health Serv Res Policy. 2011;16(1):51–58. doi:10.1258/jhsrp.2010.009129
34. McClellan CM, Greenwood R, Benger JR. Effect of an extended scope physiotherapy service on patient satisfaction and the outcome of soft tissue injuries in an adult emergency department. Emerg Med J. 2006;23(5):384–387. doi:10.1136/emj.2005.029231
35. Taylor NF, Norman E, Roddy L, Tang C, Pagram A, Hearn K. Primary contact physiotherapy in emergency departments can reduce length of stay for patients with peripheral musculoskeletal injuries compared with secondary contact physiotherapy: a prospective non-randomised controlled trial. Physiotherapy. 2011;97(2):107–114. doi:10.1016/j.physio.2010.08.011
36. McAnaw MB, Harris KW. The role of physical therapy in the rehabilitation of patients with mastectomy and breast reconstruction. Breast Dis. 2002;16(1):163–174. doi:10.3233/BD-2002-16122.
37. Bou-Karroum L, El-Harakeh A, Kassamany I, et al. Health care workers in conflict and post-conflict settings: systematic mapping of the evidence. PLoS One. 2020;15(5):e0233757. doi:10.1371/journal.pone.0233757
38. Musa SA, Hamid AA. Psychological problems among aid workers operating in Darfur. Soc Behav Pers. 2008;36(3):407–416. doi:10.2224/sbp.2008.36.3.407
39. Bride BE, Robinson MM, Yegidis B, Figley CR. Development and validation of the secondary traumatic stress scale. Res Soc Work Pract. 2004;14(1):27–35. doi:10.1177/1049731503254106
40. Guo YF, Cross W, Plummer V, Lam L, Luo YH, Zhang JP. Exploring resilience in Chinese nurses: a cross-sectional study. J Nurs Manag. 2017;25(3):223–230. doi:10.1111/jonm.12457
41. Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–919. doi:10.1016/j.bbi.2020.03.007
42. Orrù G, Marzetti F, Conversano C, et al. Secondary traumatic stress and burnout in healthcare workers during COVID-19 outbreak. Int J Environ Res Public Health. 2021;18(1):337. doi:10.3390/ijerph18010337
43. Duffy E, Avalos G, Dowling M. Secondary traumatic stress among emergency nurses: a cross-sectional study. Int Emerg Nurs. 2015;23(2):53–58. doi:10.1016/j.ienj.2014.05.001
44. Dominguez-Gomez E, Rutledge DN. Prevalence of secondary traumatic stress among emergency nurses. J Emerg Nursing. 2009;35(3):199–274. doi:10.1016/j.jen.2008.05.003
45. Ogińska-Bulik N, Michalska P. Psychological resilience and secondary traumatic stress in nurses working with terminally ill patients—The mediating role of job burnout. Psychol Serv. 2021;18:398. doi:10.1037/ser0000421
46. Roberts NJ, McAloney-Kocaman K, Lippiett K, Ray E, Welch L, Kelly C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respir Med. 2021;176:106219. doi:10.1016/j.rmed.2020.106219
47. Khasne RW, Dhakulkar BS, Mahajan HC, Kulkarni AP. Burnout among Healthcare Workers during COVID-19 pandemic in India: results of a questionnaire-based survey. Indian J Crit Care Med. 2020;24(8):664–671. doi:10.5005/jp-journals-10071-23518
48. Jose S, Dhandapani M, Cyriac MC. Burnout and resilience among frontline nurses during COVID-19 pandemic: a cross-sectional study in the emergency department of a Tertiary Care Center, North India. Indian J Crit Care Med. 2020;24(11):1081–1088. doi:10.5005/jp-journals-10071-23667
49. Grover S, Sahoo S, Bhalla A, Avasthi A. Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: a cross-sectional study. Indian J Psychiatry. 2018;60(2):175–188. doi:10.4103/psychiatry.IndianJPsychiatry_254_17
50. Klappa SG, Crocker R. Interprofessional collaborative practice during disaster relief work in Haiti: an ethnographic study. Health Policy Adm Phys Ther J Policy Adm Leadersh. 2013;13(4):J1–11.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
