Back to Journals » Infection and Drug Resistance » Volume 16
Screening and Drug Resistance Analysis of Non-Tuberculous Mycobacteria in Patients with Suspected Pulmonary Tuberculosis on the Hainan Island, China
Authors Wang J, Chen Z, Xu Y, Qiu W, Chen S, Pei H, Zhong Y
Received 11 November 2022
Accepted for publication 16 January 2023
Published 25 January 2023 Volume 2023:16 Pages 463—476
DOI https://doi.org/10.2147/IDR.S396050
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Jieying Wang,* Zhuolin Chen,* Yuni Xu, Wenhua Qiu, Shaowen Chen, Hua Pei, Yeteng Zhong
Department of Clinical Laboratory, The Second Affiliated Hospital of Hainan Medical University, Haikou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yeteng Zhong; Hua Pei, Department of Clinical Laboratory, The Second Affiliated Hospital of Hainan Medical University, Haikou, People’s Republic of China, Email [email protected]; [email protected]
Background: China has seen a drastic increase in the incidence of non-tuberculous mycobacteria (NTM) infection, which is a notable public health issue. Due to a lack of reliable epidemiological surveillance information, there is a need to gather accurate epidemiological and surveillance data, which can help clinicians effectively treat NTM patients. Moreover, drug susceptibility testing for NTM is not frequently performed in China. This retrospective study, therefore, determined the prevalence and resistance characteristics of NTM to provide a reference to control the NTM epidemic.
Methods: Sputum, alveolar lavage fluid, and other respiratory specimens were collected from 3025 patients with suspected pulmonary tuberculosis attending The Second Affiliated Hospital of Hainan Medical University from January 2014 to December 2021. Strain identification and species distribution of NTM were performed by DNA chip technology and gene sequencing, and the drug resistance of NTM isolates was evaluated by calculating the minimum inhibitory concentration through antimicrobial susceptibility testing for NTM.
Results: From 2014 to 2021, 373 strains of NTM were isolated and identified from respiratory specimens of 3025 suspected tuberculosis patients. Except in 2014, NTM-infected patients accounted for more than 10% of suspected tuberculosis patients in other years. The median age of patients with NTM infection was 62.0 years (53.0, 71.0), and the male-to-female ratio among these patients was 0.79:1. Among culture-positive strains, 12.3% (373/3040; 95% CI 11.1– 13.4%) were identified as NTM comprising forty species of NTM. The forty species of NTM included 23 slow-growing mycobacteria (SGM) and 17 rapidly-growing mycobacteria (RGM). Among the NTM isolates, 58.7% (219/373; 95% CI 53.7– 63.7%) were SGM and 41.3% (154/373; 95% CI 36.3– 46.3%) were RGM. M.avium complex(MAC)(41.3%; 95% CI 36.3– 46.3%) and M.abscessus complex (MABC)(33.2%; 95% CI 28.4– 38.0%) were the most frequently detected species, followed by M.simiae Complex (11.8%; 95% CI 8.5– 15.1%), M.fortuitum group (5.1%; 95% CI 2.9– 7.3%), and others. Drug sensitivity test results showed that most of the NTM isolates were susceptible to amikacin and clarithromycin with a drug resistance rate of less than 10%. However, clarithromycin could induce drug resistance, followed by linezolid and moxifloxacin, and their drug resistance rate was less than 50%.
Conclusion: During 2014– 2021, the number of NTM isolates detected in the respiratory specimens of the study patients in The Second Affiliated Hospital of Hainan Medical University increased year by year. M. intracellulare is the most common pathogenic NTM species, and there is a high incidence of NTM infection on Hainan Island. Our findings might be of great importance for diagnosing and treating this patient population in Hainan.
Keywords: Mycobacterium, non-tuberculous mycobacteria, pulmonary disease, drug resistance
Background
Non-tuberculous mycobacteria (NTM) is an acid-resistant bacillus widely found in water, soil, and air. NTM colonization may also occur in the human body, causing infectious diseases when the body’s immune function is low.1 Although NTM is not an obligate pathogen, its cold resistance, hydrophobicity, and intracellular pathogenicity are similar to those of M.tuberculosis (MTB).2 NTM can cause diseases in the lungs and other organs, mainly lymph nodes, skin/soft tissue, and disseminated diseases.3–5 Thus far, more than 270 NTM species/subspecies have been identified, of which more than 60 are pathogenic.6 The incidence of NTM infection has increased globally, with China alone seeing an increase from 4.9% in 1990 to 22.9% in 2010.7 However, because most nations and territories do not have mandatory reporting of NTM infections, currently available epidemiological surveillance data are scarce and unreliable.8,9 Therefore, there is an urgent need to study and accumulate accurate epidemiological and surveillance data to effectively treat NTM patients.
Treatment choices range substantially because of the high specificity of the drug resistance spectrum across NTM, even though clinical symptoms of several NTM infections may be comparable.5,10,11 Hence, the proper identification of NTM strains is crucial. The recommended treatment course for NTM infection is a combination regimen that includes macrolides.10 However, drug susceptibility testing of NTM is not performed very frequently in the clinical laboratory in China. Clinicians must have accurate information on the antimicrobial susceptibility of NTM to make the best treatment decisions. Therefore, we aimed to retrospectively analyze the prevalence and resistance characteristics of NTM to provide a reference to control the local NTM epidemic.
In recent years, NTM has gained continuous attention globally, and the pathogenicity of many NTM species has been relatively known. The reasons for this may be as follows: (1) NTM species are becoming more well-known; (2) the number of immunosuppressed patients, including patients with human immunodeficiency virus infection, is increasing; (3) more patients have pre-existing lung conditions; and (4) the application of NTM detection methods has increased.12
In China, tuberculosis (TB) has long been a notable public health issue. In China, NTM detection is performed only in a few clinical laboratories; hence, there is a high possibility of misdiagnosis and wrong treatment provided to NTM patients.5,13 In other words, in countries with a high TB burden, NTM-positive sputum smears are likely to undergo misdiagnosis as TB. NTM species are also inherently resistant to widely used anti-TB medications. Treatment for NTM infections may be postponed for several months or longer once anti-TB therapy fails. Therefore, spreading knowledge about NTM recognition as early as possible is critical. It is important to differentiate the disorders caused by various microorganisms to provide appropriate treatment. According to an article published by The American Thoracic Society, NTM identification is typically best made at the species level.10
Hainan Island is China’s southernmost province, with 15 counties in 4 states and an estimated population of 10.2 million. Hainan Island is located in the tropics and subtropics, a tropical monsoon climate region is the only tropical island in China, the latitude is low, there are unique regional differences in China, and Hainan is also a high incidence area of multi-drug resistant tuberculosis.14 According to the epidemiological survey data, the NTM infection rate in the south was higher than that in the north, and it was higher in the climate-suitable area than that in the cold area, especially in the southern coastal area with high humidity.12
However, there was no special epidemiological study on NTM infection on the Hainan Island. In our work, the strain identification and species distribution were analyzed in 373 clinical NTM isolates from 3025 patients with suspected pulmonary tuberculosis in the Hainan province to classify the species or subspecies in Hainan, China. These data might provide a preliminary understanding of the different species of NTM and the distribution of NTM-associated lung infections on the Hainan Island, China, and highlight the importance of distinguishing mycobacterial species to prevent treatment failure.
Materials and Methods
Study Subjects
According to the criteria of the national health construction commission for judging patients with suspected TB,15 sputum, alveolar lavage fluid, and other respiratory tract specimens were collected from patients with suspected TB attending the Second Affiliated Hospital of Hainan Medical University from January 2014 to December 2021.
The samples were subjected to NTM isolation and culture in addition to analyses for bacterial distribution characteristics and drug resistance characteristics. The experimental process is shown in Figure 1. This hospital, designated the Provincial Clinical Center on Tuberculosis of Hainan, is a 2300-bed general hospital, of which 92-bed open wards were designed for use in delivering specialized treatment for tuberculosis. Inclusion criteria: cough, sputum for ≥ 2 weeks, or blood in sputum or hemoptysis with suspicious symptoms of pulmonary tuberculosis in the respiratory system, and at least one NTM isolated and cultured from a respiratory specimen under the premise of ensuring no exogenous contamination of the specimen. During the study period, when a sample from the same patient was cultured no less than two times and identified to have the same NTM strain. When one type of NTM strain was isolated from the first culture of that patient, it was recorded and other duplicate strains were not considered. When the same patient was co-infected with MTB and NTM, the demographic data for both groups were included in the analysis. When a patient was co-infected with two different NTM strains, the demographic data of only one strain were included.
 |
Figure 1 Flowchart of the experimental process of the study. |
The exclusion criteria were as follows: Exogenous contaminating bacteria contamination.
The Institutional Review Committee approved this study of The Second Affiliated Hospital of Hainan Medical University, and the ethics committee waived the need for written informed consent from the enrolled patients because the patient information used in this study was routinely collected and anonymously analyzed.
The MTB H37Rv standard sensitive strain and the foreign Mycobacterium ATCC700686 standard strain, and S. aureus ATCC29213 were made available by the clinical center for TB control and prevention, the Chinese Center for Disease Control and Prevention. The Clinical Laboratory Centre of the Ministry of Health offers Staphylococcus aureus ATCC29213 for research use.
Instruments and Reagents
SLideWasherTM 8 chip washing and drying instrument, ExtractorTM 36 nucleic acid rapid extraction instrument, BiOMixerTM II hybridization instrument, and LuxScan™ 10K-B Microarray Scanner (all from CapitalBio Technology Inc., China) were used. Life Express gene amplifier was obtained from Hangzhou Bori Technology Co., Ltd, China. BSC-1600II B2 biosafety cabinet was purchased from Sujing Antai Company. A constant temperature incubator was obtained from Shanghai Boxun Company. Lowenstein–Jensen (L-J) medium, the culture medium for bacterial identification, acid-fast staining dye, and NTM drug sensitivity kit was procured from Zhuhai Baso Company, China. Mycobacterium species identification kit and supporting reagent were obtained from Beijing Boao Company, China, and the gene sequencing amplification primer was synthesized by Beijing Ruiboxingke Biotechnology Co., Ltd., China.
Test Method
Mycobacterium Culture and Identification
Respiratory tract specimens (2–3 mL), such as sputum and alveolar lavage fluid, were strictly collected from patients with suspected TB and mixed with 4%NaOH solution to prepare pretreated specimens. These specimens were allowed to stand at room temperature for 15 min. Subsequently, disposable sterile straws were used to absorb 150 µL of pretreated specimens, and the specimens were inoculated evenly on the slopes of acidic L-J medium in two tubes. The tubes were incubated at 36±1 °C for culturing, and colony growth was observed once on culture days 3 and 7, mainly to observe whether the specimen was contaminated or had the growth of RGM. From then on, colony growth was observed once a week, and culture and contamination were recorded until week 8.
Identification of NTM Species
A visible colony was scraped using a disposable sterile inoculating loop and put into a nucleic acid extraction tube containing 80 µL of nucleic acid extract and magnetic beads. After shaking for 10 min using a nucleic acid rapid extraction instrument, the nucleic acid extraction tube was subjected to the denaturation process at 95 °C for 5 min. The nucleic acid extraction tube was then removed, and the contents were centrifuged at 12,000 rpm. Next, 2 µL of the obtained nucleic acid extract was added into a polymerase chain reaction (PCR)assay tube containing 18 µL of PCR reaction mixture. The PCR assay tube was placed into a thermocycler for PCR amplification; the PCR product was then placed in the thermocycler for denaturation at 95 °C for 5 min. Immediately, the PCR product was placed in a cold-water mixture for 3 min, following which it was taken out. The hybrid mixture was configured, and 13.5 µL of this mixture was added to the microarray for hybridization for 2 h at 5rpm and 50 °C in the hybridization apparatus. After this step, the hybridized product was dried by spin-off using a chip scrubber. In the final step, the chip was placed into the scanner for chip scanning, and the results were interpreted.
Gene Sequencing for Identifying Strains
Strains initially screened as NTM and non-mycobacteria were further identified by sequencing hsp65 (hsp65-TB11: 5’-ACCAACGATGGTGTGTCCAT −3’; hsp65-TB12: 5’-CTTGTCGAACCGCATACCCT-3’, 440 bp) and rpoB (Myco-F 5’-GGCAAGGTCACCCCGAAGGG-3’; Myco-R 5’-AGCGGCTGCTGGGTGATCATC-3’, 764 bp).
Using fragment amplification primers, the DNA of the MTN strain was amplified by PCR, and electrophoresis was performed to determine whether the amplified products included the target fragments. The isolated PCR products were sent to Beijing Ruiboxingke Biotechnology Co., Ltd. for synthesizing gene sequencing amplification primers for bidirectional gene sequencing.
The nucleotide sequences were aligned with the homologous sequences of the reference mycobacterial strain based on multiple sequence alignments on the BLAST website (http://www.ncbi.nlm.nih.gov/BLAST). A similarity of 97% was used for species identification.6,16,17
Drug Susceptibility Testing
Following the Clinical and Laboratory Standards Institute (CLSI) guidelines18, in vitro antimicrobial susceptibility testing for NTM was performed using the micro broth dilution method. Fourteen antibiotics were used: clarithromycin (CLR), amikacin (AK), moxifloxacin (MFX), linezolid(LZD), cefoxitin (FOX), tobramycin (TOB), rifampicin (RFP), minocycline (MNO), amoxicillin/clavulanic acid(AMC), doxycycline (DOX), ciprofloxacin (CIP), imipenem (IPM), tigecycline (TGC), and trimethoprim/sulfamethoxazole (TMP-SMX). Minimum inhibitory concentration (MIC) was defined as the lowest concentration of the drug that inhibited the visible growth of the tested strain. MIC breakpoints (susceptible, intermediate, and resistant) were interpreted according to the CLSI guidelines.18
Quality Control
According to the quality control requirements of Tuberculosis Laboratory Testing Procedures, positive sputum smear tests but negative Mycobacterium culture should be less than 10%, with a contamination rate of less than 5%. When the DNA microarray chip detected each sample, internal quality control was carried out simultaneously. When the quality control results were wrong, the sample results were considered invalid, and the samples had to be retested. The TB laboratory of The Second Affiliated Hospital of Hainan Medical University participates in and passes the TB smear test, TB culture, TB drug sensitivity (first-line and second-line drugs), and TB molecular diagnosis conducted by the Tuberculosis Clinical Center of the Chinese Center for Disease Control and Prevention every year.
Statistical Analysis
SPSS 25.0 software was used for the descriptive analysis of the information of patients with suspected pulmonary infection due to NTM. Data of patient age had a non-normal distribution and were presented as median; they were analyzed using the non-parametric independent-samples Mann–Whitney U-test. Differences were considered statistically significant at P<0.05.
Results
Demographic Data of Patients
Overall, 3025 patients with suspected TB were enrolled between January 1, 2014, and December 31, 2021.2659 MTB and 373 NTM strains were isolated from the respiratory specimens of 3025 patients with suspected tuberculosis, including 351 patients with singly infected NTM, 2651 patients with singly infected MTB, and 8 patients with mixed MTB and NTM infections. Two different NTMs were isolated from 7 patients, as shown in Table 1.
 |
Table 1 From 2014 to 2021, 7 Patients with NTM Co-Infection and 8 Patients with NTM-MTB Co-Infection Were Found on the Hainan Island |
NTM infection accounted for 12.1% (366/3025; 95% CI 10.9–13.3%) of all suspected TB cases. Besides, we also detected Gordonia bronchialis (n = 1), Gordonia otitidis (n = 1), Gordonia paraffinivorans (n = 1), Gordonia aichiensis (n = 2), Nocardia farcinica (n = 1), and Tsukamurella paurometabola (n = 2).Overall, 366 patients with a median age of 62.0 years (53.0, 71.0) had NTM infection. Of the 366 patients, 161 males had NTM infection and were aged 65.0 years (54.0, 76.0), while 205 females had NTM infection and were aged 61.0 (53.0, 67.0) years, with a male-to-female ratio of 0.79:1 (Figure 2).
 |
Figure 2 Sex and age distribution of patients with and NTM. Abbreviations: TB, tuberculosis; NTM, non-tuberculous mycobacteria. |
2659 patients, with a median age of 50.0 years (35.0, 61.0), had MTB infection. Of the 2659 patients, 2181 males had MTB infection and were aged 51.0 years (38.0, 62.0), while 478 females had MTB infection and were aged 41.0 years (27.0, 56.0), with a male-to-female ratio of 4.57:1 (Figure 2).
In parallel, we compared the proportion of infection with NTM in suspected TB during the 8-year study period. From 2015 to 2021, the number of non-tuberculous mycobacteria detected in respiratory specimens of suspected pulmonary tuberculosis patients was more than 10% (Figure 3).
 |
Figure 3 Distribution of positive specimens in culture and identification of Mycobacterium during 2014–2021. Abbreviations: MTB, Mycobacterium tuberculosis; NTM, non-tuberculous mycobacteria. |
NTM Species Distribution
Gene chip and further gene sequencing analysis showed that 40 species of NTM were detected, including 23 species of SGM (58.7%, 219/373; 95% CI 53.7–63.7%) and 17 species of RGM (41.3%, 154/373; 95% CI 36.3–46.3%) (Figure 4). The four most commonly isolated NTM flora, accounting for 91.4% of all NTM species, included M.avium complex(MAC)(41.3%; 95% CI 36.3–46.3%), M.abscessus complex (MABC)(33.2%; 95% CI 28.4–38.0%), M.simiae complex (11.8%; 95% CI 8.5–15.1%), and M.fortuitum group (5.1%; 95% CI 2.9–7.3%). MAC was further subgrouped into nine subspecies: M.intracellulare(109 isolates), and M.intracellulare subsp.chimaera (17 isolates), M.columbine(8 isolates), M.avium(5 isolates), M.timonense(5 isolates), M.intracellulare subsp. yongonense (6 isolates), M.marseillense(2 isolates), M.paraintracellulare(1 isolate), and M.bouchedurhonense(1 isolate). MABC included three subspecies: M.abscessus subsp. abscessus (74 isolates), M.abscessus subsp. massiliense (38 isolates), and M.abscessus subsp. bolletii (12 isolates).
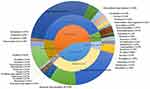 |
Figure 4 Distribution of non-tuberculous Mycobacterium species isolated from patients with suspected pulmonary NTM on the Hainan Island, China. Abbreviation: NTM, non-tuberculous mycobacteria. |
Drug Sensitivity Test
The appropriate sensitivity distribution data, including the MIC50/MIC90 (50%/90% minimum inhibitory concentration) values for RGM, are shown in Table 2. TGC was the most effective drug against all RGM strains, followed by AK, with the lowest resistance rate of 0.65% (1/154). RGM strains had resistance rates of 7.14% (11/154) and 27.92% (43/154) to FOX and LZD, respectively. Furthermore, 44.80% (69/154) of RGM strains showed no resistance to CLR on day 3 but the resistance was detected on day 14. 11.04% (17/154) of RGM strains showed resistance to CLR on days 3 and 14. After culture 14 days, 47.58% MABC had a resistance rate to CLR. Table 3 compares the drug susceptibility status among the major species of MABC, namely, M.abscessus subsp. abscessus, M.abscessus subsp.massiliense, and M.abscessus subsp. bolletii. Among the three MABC species, M.abscessus subsp. abscessus had the highest rate of antibiotic induced resistance against CLR. The CLR induced resistance rates for the three MABC species (M.abscessus subsp. abscessus, M.abscessus subsp.massiliense, and M.abscessus subsp. bolletii) were 71.63%, 2.63%, and 41.67%, respectively. For the three subspecies of MABC, the resistance rates to CLR (14D) were 85.14% (M.abscessus subsp. abscessus), 5.26% (M.abscessus subsp. massiliense), and 41.67% (M.abscessus subsp. bolletii), with significant differences. RGM exhibited high levels of resistance to several drugs including IPM, TOB, DOX, MFX, AMC, CIP, and TMP-SMX). More than 90% MABC infection pathogens showed resistance to DOX, MFX, AMC, CIP, and TMP-SMX. Comparison between MABC and the rest RGM strains we found that there were significantly difference in the drug resistance rates for AK, IPM, LZD, TOB, DOX, MFX, AMC, CIP, and TMP-SMX. Additionally, a significant difference was noted between the drug resistance rates of M.abscessus subsp. abscessus and M.abscessus subsp.massiliense to TOB (77.03% vs 94.74%).
 |
Table 2 The Sensitivity of RGM to Antibiotics Was Determined by MIC Method |
 |
Table 3 The Sensitivity of MABC to Antimicrobial Agents Was Determined by MIC Method |
MIC information was obtained for 219 SGM isolates. Antimicrobial susceptibility testing was performed to assess the susceptibility of 154 MAC isolates to four antimicrobial drugs. CLR and AK resistance tests demonstrated outstanding bacteriostatic activity (Table 4), suggesting that they can be used as first-line antibacterial agents for MAC isolates. Amikacin was the most effective drug against MAC, with a 3.90% (6/154) resistance rate, while CLR had a resistance rate of 5.19% (8/154). MAC isolates had drug resistance rates of 42.86% and 25.32% to LZD and MFX, respectively, suggesting that these drugs can be used as second-line antibacterial agents.
 |
Table 4 The Sensitivity of MAC to Antimicrobial Agents Was Determined by MIC Method |
Table 5 presents the data on the susceptibility of 44 M. simiae complex to 10 antibiotics. M. simiae complex showed resistance to DOX, MNO, and AMC. The resistance rates of M. simiae complex to RFP and CIP were higher than 95%, followed by resistance to LZD (79.55%, 35/44), TMP-SMX (54.55%, 24/44), AK (27.27%, 12/44), MFX (18.18%, 8/44), and CLR (13.64%, 6/44).
 |
Table 5 The Susceptibility of M.simiae Complex to Antibiotics Was Determined by MIC Method |
The drug susceptibility results of the other 21 SGM isolates were shown in Table 6. All SGM isolates were sensitive to AK. The resistance rates of the 21 SGM isolates to CLR, MFX, and LZD were lower than 10%, followed by resistance to CIP (23.8%, 5/21), TMP-SMX (33.33%, 7/21), MNO (38.10%, 8/21), RFP (42.86%, 9/21), DOX (47.62%, 10/21), and AMC (71.43%, 15/21).
 |
Table 6 The Sensitivity of Other SGM to Antimicrobial Agents Was Determined by MIC Method |
Table 7 shows a comparison of the medication susceptibility patterns of several SGM species. M. simiae complex exhibited considerably stronger resistance to AK than did MAC(χ2=26.871, P<0.001). M. simiae complex considerably outperformed MAC and other SGM isolates in terms of drug resistance to LZD (χ2=31.608, P<0.001). Additionally, no discernible variation was noted in the rates of resistance to CLR and MFX among various SGM species.
 |
Table 7 Drug Resistance Rate of Different Species of SGM |
Discussion
Clinically, it might be challenging to distinguish pulmonary TB from pulmonary infection caused by NTM. Most NTM strains are not responsive to anti-TB medications and therefore were erroneously identified as drug-resistant TB strains. However, some cases of NTM are misdiagnosed and caused inappropriate treatment.19,20 Therefore, determine the pathogen spectrum of the isolated strains at the species level is crucial for managing these diseases. In comparison to regions and degrees of economic development, the infection rate and distribution of NTM were very different. In our study, the results of isolation and identification of 40 different NTM species from the respiratory samples of 3025 patients with pulmonary TB indicated diversity in NTM species among Hainan Island patients. M. intracellulare was the most prevalent NTM pathogen, followed by M.abscessus subsp. abscessus subspecies, which was consistent with earlier discoveries in the coastal regions of southern China, India, Japan, and other countries.6,21–23 To the best of our knowledge, this is the first study on strain identification, drug sensitivity testing, and screening among patients with suspected TB due to NTM lung illness in the Hainan Province.
Our data suggest that the proportion of NTM lung prevalence among patients with suspected TB in recent years cannot be underestimated. Most patients were elderly and middle-aged females. The age of onset of NTM distribution in female patients was earlier than that in male patients, which may be related to female physiological factors. After menopause, the hormone level secreted by the body varies, which weakens metabolic ability and immunity. The higher prevalence of NTM among middle-aged and elderly patients may be related to the decrease in immunity with aging.24,25
AK is the most effective antimicrobial agent against NTM infection, followed by CLR, but CLR can induce resistance to MABC isolates. The 14-day resistance rate of MABC to CLR was 56.45%, consistent with the results of multi-center studies conducted in China.12 Further subspecies analysis showed that the resistance rates of the three subspecies of MABC to CLR (14D) were 85.14% (M. abscessus subsp. abscessus), 41.67% (M. abscessus subsp.bolletii), and 5.26% (M. abscessus subsp. massiliense). This may be due to the presence of an erm(41) T28 gene mutation in M. abscessus subsp. M.abscessus subsp. abscessus and M. abscessus subsp. bolletii and erm(41) gene deletion at the 274 bp site in M. abscessus subsp. massiliense, resulting in the inactivation of the erm(41) gene. However, the erm(41) T28 genotype can produce the active erm protein, which may be related to CLR induced resistance.It has been proposed that the high rate of induced resistance of MABC to CLR in this region may be because the majority of MABC subspecies in this region are M.abscessus subsp. bolletii and M.abscessus subsp. abscesses of the erm(41) T28 genotype.26,27 Therefore, it is crucial to correctly identify the MABC subspecies to utilize the effectiveness of CLR as a medication.
RGM isolates exhibited high levels of resistance to IPM, TOB, DOX, MFX, AMC, CIP, and TMP-SMX. More than 90% of patients with MABC infection in this study had resistance to DOX, MFX, AMC, CIP, and TMP-SMX. Moreover, different isolates of RGM had different resistance patterns, but all RGM isolates showed very good sensitivity to TGC. Past studies have shown that TGC has a good curative effect on MDR RGM infection in vitro and in vivo.28 The MIC breakpoint for TGC for RGM has not yet been established, though, by the CLSI or the European Committee for Antimicrobial Susceptibility Testing. Further clinical investigation is required to identify new therapeutic options because TGC has not been authorized for the management of mycobacterial infections.29 The sensitivity rates of SGM to AK and CLR were greater than 50%. The sensitivity of SGM to commonly used anti-TB drugs was higher than that of RGM. MAC is the predominant isolate of SGM, which is highly sensitive to the commonly used first-line drugs (CLR and AK) and slightly less sensitive to the second-line drugs (MFX and LZD). The resistance rate of Mycobacterium simiae complex to AK and LZD was significantly higher than those of MAC and Other SGM. The Other SGM was highly sensitive to the first-line drugs AK and CLR and the second-line drugs LZD and MFX, with susceptibility rates of more than 85%. Therefore, CLR and AK are suggested as the first choice of anti-SGM drugs.
Although the clinical importance of isolating various NTM species from a patient is not reported, the co-existence of NTM species might indicate signs of NTM lung infection. In contrast to a previous study conducted in Chongqing, Southwest China, where the proportion of co-infected patients was substantially greater (7.5%),9 two NTM species were isolated from seven patients in our study (1.91%). In a Singapore study, the rate was even higher, at 30.1%.30 There were no species-matching patterns or sequence order. NTM strains may change during or after treatment for NTM lung disease, which may be due to clinical conditions or drug-induced changes31. However, because we did not collect data related to clinical treatment, the relationship between multispecies infection and clinical treatment could not be examined. Therefore, more research is required to clarify the clinical importance of isolating numerous species from the same patient.
MTB and NTM were isolated from 8 patients (2.19%). Consistently, approximately 3% of patients with suspected MDR-TB in China had co-infection with MTB and NTM.32 Zoe et al also demonstrated that nearly a quarter of patients with pulmonary infection due to NTM had a history of pulmonary TB.9,30 In the United States, a population-based study showed that 14% of TB patients had co-infection with NTM and MTB and that NTM was often isolated soon after TB diagnosis.33 Structural lung diseases make people more susceptible to pulmonary NTM, and tuberculosis is an important pathophysiological process associated with severe structural lung damage.34 Asian patients with pulmonary NTM infection are highly likely to have a history of pulmonary TB.30,35 TB is a chronic disease occurring owing to poor socioeconomic conditions, malnutrition, and poor immunity, which increase the rates of co-infection with NTM and MTB.19,36,37 In settings of high TB burden, cases of NTM-MTB co-infection may be misdiagnosed as cases of MDR-TB owing to the widespread resistance of NTM to anti-TB drugs.38 Because of the differences in growth rate and culture conditions requirements after culturing a mixture of MTB and NTM in vitro, it becomes difficult to identify NTM-MTB co-infection accurately and timely using conventional methods. Although NTM-MTB co-infection may affect only a small subset of the overall TB patient population, accurate identification of NTM-MTB co-infection is important before initiating treatment regimens for MDR-TB. The strains should be distinguished, and drug susceptibility tests should be performed as accurately as possible to reduce misdiagnosis and missed diagnosis, especially to not misdiagnose sensitive MTB as MDR-TB.
Additionally, regularly used commercial kits can identify only less than 20 NTM species, which has made molecular diagnostics and other approaches for species identification more popular. Targeted DNA sequencing techniques such as 16S rRNA, rpoB, hsp65, and ITS can distinguish NTM, MTB, and non-Mycobacterium taxa and identify NTM strains at the species level.1,39–42 The sequencing analysis in the present study identified not only 40 NTM and MTB species but also 8 non-mycobacterial strains (including Gordonia bronchialis [n = 1], Gordonia otitidis [n = 1], Gordonia paraffinivorans [n = 1], Gordonia aichiensis [n = 2], Nocardia farcinica[n = 1], and Tsukamurella paurometabola [n = 2]). The genera Nocardia, Gordonia, and Tsukamura belong to the order Actinomycetes. Acid-fast staining showed a positive result for Gordonia and Tsukamura and a weakly positive result for Nocardia. The morphology of the three strains was similar to that of Mycobacterium, and they could also cause pulmonary infection, which was easily misdiagnosed as pulmonary TB or NTM pulmonary infection. Therefore, the accurate distinction between Mycobacterium and non-mycobacteria is extremely important in the clinical workup.
Notably, most NTM species are widely present in common water sources and air, especially in warm and moist air. Therefore, we must exercise caution when interpreting positive results in clinical workups because positive results do not always indicate that the patient has been exposed to pathogens. The diagnosis of NTM pulmonary infection needs to be combined with the clinical diagnosis because a positive result could also be attributed to bacterial colonization, a temporary infection that is quickly cleared by the body’s immune system, or environmental NTM contamination during sample collection and transport.1
Our study findings have a few limitations that deserve addressing. First, only a small number of patients were included in the study analysis, although every patient received care at a facility that regularly recognizes and manages a sizable number of patients with NTM lung infections. To support our findings, a comprehensive investigation involving patients from several hospitals on Hainan Island is needed in the future. Second, because NTM can infect the lymph nodes and soft tissues of the skin in addition to causing pulmonary infection, there is a need to broaden the sample types in research to understand the dispersion of strains better. This study assessed only the NTM drug resistance phenotype; the drug resistance mechanism was not thoroughly investigated. Moreover, we did not conduct an in-depth analysis of the genotypes underlying the various subtypes of MABC’s resistance to macrocyclic lipids, for instance; however, this aspect will be assessed in future studies.
Conclusion
According to our research, M. intracellulare is the most common pathogenic NTM species, and there is a high incidence of NTM infection on Hainan Island. Therefore, for patients with symptoms similar to those of TB, clinicians should consider NTM infection during diagnosis and treatment. Because different NTM species have varying susceptibilities to antimicrobial drugs, identification of NTM species and drug sensitivity testing are crucial for determining the effectiveness of treatment.
Acknowledgment
The work is funded by the Hainan Provincial Natural Science Foundation of China (No. 820MS144, No. 822RC844), Hainan Medical Scientific research projects (No.19A200162), and Hainan Province Clinical Medical Center.
Disclosure
All authors declare no conflicts of interest in this work.
References
1. Stout JE, Koh WJ, Yew WW. Update on pulmonary disease due to non-tuberculous mycobacteria. Int J Infect Dis. 2016;45:123–134. doi:10.1016/j.ijid.2016.03.006
2. Good RC, Snider DE. Isolation of nontuberculous mycobacteria in the United States, 1980. J Infect Dis. 1982;146(6):829–833. doi:10.1093/infdis/146.6.829
3. Medical Section of the American Lung Association. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Am J Respir Crit Care Med. 1997;156(2 Pt 2):S1–25. doi:10.1164/ajrccm.156.2.atsstatement
4. Latshang TD, Lo Cascio CM, Russi EW. Atypische Mykobakteriose der Lunge [Nontuberculous mycobacterial infections of the lung]. Ther Umsch. 2011;68(7):402–406. German. doi:10.1024/0040-5930/a000184
5. Li G, Pang H, Guo Q, et al. Antimicrobial susceptibility and MIC distribution of 41 drugs against clinical isolates from China and reference strains of nontuberculous mycobacteria. Int J Antimicrob Agents. 2017;49(3):364–374. doi:10.1016/j.ijantimicag.2016.10.024
6. Sun Q, Yan J, Liao X, et al. Trends and species diversity of non-tuberculous mycobacteria isolated from respiratory samples in Northern China, 2014–2021. Front Public Health. 2022;10:923968. doi:10.3389/fpubh.2022.923968
7. Wang L, Zhang H, Ruan Y, et al. Tuberculosis prevalence in China, 1990–2010; a longitudinal analysis of national survey data. Lancet. 2014;383(9934):2057–2064. doi:10.1016/S0140-6736(13)62639-2
8. Lopez-Roa P, Aznar E, Cacho J, et al. Epidemiology of Non-Tuberculous Mycobacteria isolated from clinical specimens in Madrid, Spain, from 2013 to 2017. Eur J Clin Microbiol Infect Dis. 2020;39(6):1089–1094. doi:10.1007/s10096-020-03826-7
9. Zhang H, Luo M, Zhang K, et al. Species identification and antimicrobial susceptibility testing of non-tuberculous mycobacteria isolated in Chongqing, Southwest China. Epidemiol Infect. 2020;149:e7. doi:10.1017/S0950268820003088
10. Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416. doi:10.1164/rccm.200604-571ST
11. Mougari F, Loiseau J, Veziris N, et al. Evaluation of the new GenoType NTM-DR kit for the molecular detection of antimicrobial resistance in non-tuberculous mycobacteria. J Antimicrob Chemother. 2017;72(6):1669–1677. doi:10.1093/jac/dkx021
12. Liu CF, Song YM, He WC, et al. Nontuberculous mycobacteria in China: incidence and antimicrobial resistance spectrum from a nationwide survey. Infect Dis Poverty. 2021;10(1):59. doi:10.1186/s40249-021-00844-1
13. Shao Y, Chen C, Song H, et al. The epidemiology and geographic distribution of nontuberculous mycobacteria clinical isolates from sputum samples in the eastern region of China. PLoS Negl Trop Dis. 2015;9(3):e0003623. doi:10.1371/journal.pntd.0003623
14. Lin M, Zhong Y, Chen Z, et al. High incidence of drug-resistant Mycobacterium tuberculosis in Hainan Island, China. Trop Med Int Health. 2019;24(9):1098–1103. doi:10.1111/tmi.13285
15. People’s Republic of China and Family Planning Commission. Diagnosis of Tuberculosis. Beijing: People’s Republic of China and Family Planning Commission; 2017.
16. Liu H, Lian L, Jiang Y, et al. Identification of species of nontuberculous mycobacteria clinical isolates from 8 provinces of China. Biomed Res Int. 2016;2016:2153910. doi:10.1155/2016/2153910
17. McNabb A, Eisler D, Adie K, et al. Assessment of partial sequencing of the 65-kilodalton heat shock protein gene (hsp65) for routine identification of Mycobacterium species isolated from clinical sources. J Clin Microbiol. 2004;42(7):3000–3011. doi:10.1128/JCM.42.7.3000-3011.2004
18. Clinical and Laboratory Standards Institute. Susceptibility testing of mycobacteria, Nocardia spp., and other aerobic actinomycetes.
19. Karamat A, Ambreen A, Ishtiaq A, Tahseen S, Rahman MA, Mustafa T. Isolation of non-tuberculous mycobacteria among tuberculosis patients, a study from a tertiary care hospital in Lahore, Pakistan. BMC Infect Dis. 2021;21(1):381. doi:10.1186/s12879-021-06086-8
20. Wani SR, Wattal C, Raveendran R. Epidemiology and risk factors associated with NTM pulmonary and extrapulmonary infections in a high tuberculosis endemic Region. Indian J Med Microbiol. 2020;38(2):169–175. doi:10.4103/ijmm.IJMM_20_274
21. Thangavelu K, Krishnakumariamma K, Pallam G, et al. Prevalence and speciation of non-tuberculous mycobacteria among pulmonary and extrapulmonary tuberculosis suspects in South India. J Infect Public Health. 2021;14(3):320–323. doi:10.1016/j.jiph.2020.12.027
22. Huang JJ, Li YX, Zhao Y, et al. Prevalence of nontuberculous mycobacteria in a tertiary hospital in Beijing, China, January 2013 to December 2018. BMC Microbiol. 2020;20(1):158. doi:10.1186/s12866-020-01840-5
23. Furuuchi K, Morimoto K, Yoshiyama T, et al. Interrelational changes in the epidemiology and clinical features of nontuberculous mycobacterial pulmonary disease and tuberculosis in a referral hospital in Japan. Respir Med. 2019;152:74–80. doi:10.1016/j.rmed.2019.05.001
24. Chalermskulrat W, Gilbey JG, Donohue JF. Nontuberculous mycobacteria in women, young and old. Clin Chest Med. 2002;23(3):675–686. doi:10.1016/S0272-5231(02)00010-2
25. Moon P, Guillaumin E, Chan ED. Non-tuberculous mycobacterial lung disease due to multiple “minor” risk factors: an illustrative case and a review of these “lesser elements”. J Thorac Dis. 2020;12(9):4960–4972. doi:10.21037/jtd-20-986
26. Bastian S, Veziris N, Roux AL, et al. Assessment of clarithromycin susceptibility in strains belonging to the Mycobacterium abscessus group by erm(41) and rrl sequencing. Antimicrob Agents Chemother. 2011;55(2):775–781. doi:10.1128/AAC.00861-10
27. Richard M, Gutierrez AV, Kremer L. Dissecting erm (41)-mediated macrolide-inducible resistance in mycobacterium abscessus. Antimicrob Agents Chemother. 2020;64(2). doi:10.1128/AAC.01879-19
28. Wallace RJ, Dukart G, Brown-Elliott BA, Griffith DE, Scerpella EG, Marshall B. Clinical experience in 52 patients with tigecycline-containing regimens for salvage treatment of Mycobacterium abscessus and Mycobacterium chelonae infections. J Antimicrob Chemother. 2014;69(7):1945–1953. doi:10.1093/jac/dku062
29. Hatakeyama S, Ohama Y, Okazaki M, Nukui Y, Moriya K. Antimicrobial susceptibility testing of rapidly growing mycobacteria isolated in Japan. BMC Infect Dis. 2017;17(1):197. doi:10.1186/s12879-017-2298-8
30. Zhang ZX, Cherng BPZ, Sng LH, Tan YE. Clinical and microbiological characteristics of non-tuberculous mycobacteria diseases in Singapore with a focus on pulmonary disease, 2012–2016. BMC Infect Dis. 2019;19(1):436. doi:10.1186/s12879-019-3909-3
31. Lee JS, Lee JH, Yoon SH, et al. Implication of species change of nontuberculous mycobacteria during or after treatment. BMC Pulm Med. 2017;17(1):213. doi:10.1186/s12890-017-0539-7
32. Huang M, Tan Y, Zhang X, et al. Effect of mixed infections with mycobacterium tuberculosis and nontuberculous mycobacteria on diagnosis of multidrug-resistant tuberculosis: a retrospective multicentre study in China. Infect Drug Resist. 2022;15:157–166. doi:10.2147/IDR.S341817
33. Kendall BA, Varley CD, Hedberg K, Cassidy PM, Winthrop KL. Isolation of non-tuberculous mycobacteria from the sputum of patients with active tuberculosis. Int J Tuberculosis Lung Dis. 2010;14(5):654–656.
34. Andrejak C, Nielsen R, Thomsen VO, Duhaut P, Sorensen HT, Thomsen RW. Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax. 2013;68(3):256–262. doi:10.1136/thoraxjnl-2012-201772
35. Simons S, van Ingen J, Hsueh PR, et al. Nontuberculous mycobacteria in respiratory tract infections, Eastern Asia. Emerg Infect Dis. 2011;17(3):343–349. doi:10.3201/eid170310060
36. Hu C, Huang L, Cai M, Wang W, Shi X, Chen W. Characterization of non-tuberculous mycobacterial pulmonary disease in Nanjing district of China. BMC Infect Dis. 2019;19(1):764. doi:10.1186/s12879-019-4412-6
37. Meghji J, Lesosky M, Joekes E, et al. Patient outcomes associated with post-tuberculosis lung damage in Malawi: a prospective cohort study. Thorax. 2020;75(3):269–278. doi:10.1136/thoraxjnl-2019-213808
38. Johansen MD, Herrmann JL, Kremer L. Non-tuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat Rev Microbiol. 2020;18(7):392–407. doi:10.1038/s41579-020-0331-1
39. Nour-Neamatollahie A, Ebrahimzadeh N, Siadat SD, et al. Distribution of non-tuberculosis mycobacteria strains from suspected tuberculosis patients by heat shock protein 65 PCR-RFLP. Saudi J Biol Sci. 2017;24(6):1380–1386. doi:10.1016/j.sjbs.2016.02.001
40. Liang Q, Shang Y, Huo F, et al. Assessment of current diagnostic algorithm for detection of mixed infection with Mycobacterium tuberculosis and nontuberculous mycobacteria. J Infect Public Health. 2020;13(12):1967–1971. doi:10.1016/j.jiph.2020.03.017
41. Kim SH, Shin JH. Identification of nontuberculous mycobacteria using multilocous sequence analysis of 16S rRNA, hsp65, and rpoB. J Clin Lab Anal. 2018;32(1). doi:10.1002/jcla.22184
42. Xu Y, Liang B, Du C, et al. Rapid identification of clinically relevant mycobacterium species by multicolor melting curve analysis. J Clin Microbiol. 2019;57(1). doi:10.1128/JCM.01096-18
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
