Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Satisfaction of Health Professionals Regarding the Short Binasal Prong Used as a Non-Invasive Ventilation Interface in Neonatology
Authors Ribeiro DDFC , Hembecker PK , Nakato AM , Fernandes BL , Nohama P
Received 30 April 2023
Accepted for publication 5 July 2023
Published 2 August 2023 Volume 2023:16 Pages 2217—2229
DOI https://doi.org/10.2147/JMDH.S415748
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Débora de Fátima Camillo Ribeiro,1,2 Paula Karina Hembecker,2 Adriane Muller Nakato,2 Beatriz Luci Fernandes,2 Percy Nohama2,3
1Neonatal Services, Waldemar Monastier Hospital, Campo Largo, Paraná, Brazil; 2Graduate Program on Health Technology, Pontifícia Universidade Católica Do Paraná, Curitiba, Paraná, Brazil; 3Graduate Program on Biomedical Engineering, Universidade Tecnológica Federal Do Paraná, Curitiba, Paraná, Brazil
Correspondence: Percy Nohama, Graduate Program on Health Technology, Pontifícia Universidade Católica do Paraná, Rua Imaculada Conceição 1155, Curitiba, Paraná, CEP 80215-901, Brazil, Tel +55 41 3271-1357, Email [email protected]
Purpose: To evaluate the health professionals’ satisfaction regarding the short binasal prong used in Neonatal Intensive Care Units (NICU), evaluate the difficulties related to its use, and present possible improvements in the design of this device.
Patients and Methods: Observational, cross-sectional study with prospective data collection carried out in the NICU of a public hospital in southern Brazil. This research was presented into two stages. In the first stage, the Quebec User Evaluation of Satisfaction with Assistive Technology was applied with 90 health professionals to evaluate the satisfaction regarding the short binasal prong. In the second stage, the health professional’s experiences and difficulties in using the binasal prongs in 14 newborns (NBs) that required non-invasive ventilation was collected. The short binasal prongs used was the Fanem® brand and the CPAP circuit was Gabisa Medical International (GMI®). Finally, improvements and recommendations were presented to optimize the device’s design.
Results: The mean score of the health professionals’ satisfaction with short binasal prongs was 3.8 ± 0.6. Ease of adjustment (3.27) and dimensions (3.62) variables had the worst scores. The main difficulties pointed out by health professionals were: circuit disconnection (57.1%), the size of the prong did not correspond to NBs’ anatomical characteristics (35.7%), air leakage (21.4%), and difficulty in fixing and positioning the prong in the NB (14.28%). The improvements suggested were: appropriate prong sizes based on the anatomical characteristics of the NBs; adjustable distance between insertion and base catheters; manufactured with malleable material, however not easily foldable; curved and adjustable insertion catheters and functional system of tracheas’ connection.
Conclusion: The dissatisfaction of health professionals with the dimensions and prongs adjustments and the difficulties faced in clinical practice indicate the need for improvements in these interfaces. The recommendations presented in this study may contribute to optimizing the design of the binasal prong in the future.
Keywords: assistive technology, neonatal intensive care, non-invasive ventilation, surveys and questionnaires
Introduction
Non-invasive ventilation (NIV) is an alternative to invasive mechanical ventilation in treating acute or chronic respiratory disorders in newborns (NB) associated with impaired respiratory function, inadequate pulmonary ventilation, and altered gas exchange, which result in respiratory failure.1 Avoiding intubation and using NIV modes in premature newborns reduces the risk of lung injury and optimizes neonatal outcomes.2
NIV systems generally have three main components: a gas source that supplies heated and humidified air and/or oxygen, a pressure generator that creates positive pressure, and an interface that connects the circuit to the newborns’ upper airways.3 The latter is essential for delivering ideal positive pressure to NB.4
The short binasal prong is the NIV interface most used in neonatology,5 once it offers less resistance to airflow and is more effective in preventing reintubation when compared to nasopharyngeal prongs.6 It was initially used by Wung et al7 and considered simple to use, effective and safe.3 It is also less invasive and facilitates mobilization and oral feeding.8 However, they present the risk of developing a nasal injury, allow leakage through the mouth, and are relatively challenging to fix.9
One of the risks of using nasal prongs is the injury. This damage can range from simple hyperemia to columella and nasal septum destruction.10 The incidence of this adverse effect ranges from 13.2% to 50%.11 It can reach rates of up to 100%,12 causing a negative impact, both for NBs and their families, due to pain, delayed functional recovery, and infections, as well as to health systems due to the increase in hospitalization time and the increase in costs with treatments for associated comorbidities.13
The other disadvantage of NIV using short binasal prongs is the air leakage through the mouth.14 Premature infants are more likely to open their mouths when pressure increase in the oropharynx with the application of NIV and also due to weakness of the orofacial muscles.15 To minimize air leakage through the mouth, using pacifiers or applying bandages under the NB’s chin is indicated as needed.3 However, the effects on the safety and efficacy of active mouth closure during nasal continuous positive airway pressure (CPAP) application are not yet known.16
Attaching the prong to the nostrils is an important factor in the success of NIV. Difficulties in fixation lead to increased mobility of the prongs in the nostrils, which may result in nasal injury, and enable fluctuations in oxygen supply and positive pressure, destabilizing the newborn.17
Faced with the problems related to the use of nasal prongs, the present study aimed to evaluate the degree of satisfaction of health professionals regarding the use of the short binasal prongs used in neonatology, to evaluate the difficulties related to its use in clinical practice and to present possible improvements in the design of these devices.
Materials and Methods
Study Design
The present study is observational and cross-sectional, with prospective data collection carried out at the Neonatal Intensive Care Unit (NICU) of the Hospital Infantil Waldemar Monastier (HIWM) located in the metropolitan region of Curitiba, Paraná, Brazil.
The study was carried out in two stages. First, the level of satisfaction of health professionals working in the NICU of the Hospital Infantil Waldemar Monastier was evaluated concerning the short binasal prong (Fanem®) used as a non-invasive ventilation interface for newborns in this NICU. In the second stage, possible difficulties related to using this interface in NBs who needed NIV between December 2018 and March 2020 were evaluated. Based on the results found in these two stages, the researchers of this study listed possible improvements in the short binasal prongs to optimize the design of these devices. However, it was not the scope of this study to develop such improvements or assess their feasibility.
First Stage
Participants
The study included nurses, physiotherapists, intensive care neonatologists, and nursing technicians of the HIWM NICU who agreed to participate in this research by signing the Informed Consent Form. Professionals with less than three months of experience in neonatology were excluded.
Data Collection Instruments and Procedures
The variables evaluated were the participants’ sociodemographic data and their level of satisfaction with the short binasal prong used in the NICU.
The sociodemographic data collected were age, gender, education, profession, marital status, laterality, and time of experience in neonatology.
The level of satisfaction was assessed using the translated and validated version of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) for Brazilian Portuguese, Quest-B.
Quest-B helps rehabilitation professionals, researchers, and managers of public and private services in their cost-benefit, cost-effectiveness, and cost-utility analyses, favoring technical improvement, cost reduction, and improvement in the quality of services provided.18
In addition, Quest-B consists of a questionnaire composed of twelve questions, divided into two stages: the first consists of eight items related to the use of assistive technology (dimensions, mass, adjustments, safety, durability, ease of use, comfort and effectiveness); and the second, on four items related to the provision of services (delivery process, repairs, and technical assistance, professional services and follow-up). For all items evaluated, the degree of satisfaction varies from 1 to 5, with 1 being dissatisfied and 5 being very satisfied. In the end, the interviewee was invited to mark the three that he considered most important among the twelve items evaluated.18
Considering that the second stage of the Quest-B did not apply to the reality of the NICU studied, only the first stage of the questionnaire mentioned above was applied in this study.
At the end of the questionnaire, professionals were invited to point out suggestions for improvements to the assessed interface.
Data Collection
The researcher initially approached health professionals individually during their work shift at the NICU, who explained the study and invited them to participate. After being instructed, the professionals who agreed to participate in the study read and signed the Free and Informed Consent Form and then answered the Quest-B questionnaire. All participants received prior instructions on how to complete the questionnaire mentioned above. In addition, all were informed that the responses would be anonymous and treated as confidential. Participation in the study was voluntary, and they had the right to withdraw their consent at any time. The approximate mean time to complete the questionnaire was 10 min.
Second Stage
Participants
Newborns who needed NIV as initial ventilatory support or as weaning, through the short binasal prong, for a minimum of 24 hours and whose parents or guardians authorized to participate in the research by signing the Term of Free and Informed Consent were selected. In addition, NBs with facial deformities, NBs who used NIV prior to the study, and NBs with skin lesions in the nasal region were excluded.
Evaluated Variables
The variables collected prior to the installation of NIV were: gender, gestational age, birth weight, the weight of the NB before NIV installation, Apgar score at 1 and 5 min, the reason for NIV installation, and cephalic perimeter. The variables evaluated every 24 h after installing NIV were: time of use of NIV, the need to change the size of the prong, the need to change the type of circuit fixation, and the general difficulties reported by the care team regarding the use of NIV with short binasal prongs in NBs.
Procedures
Initially, the NBs were analyzed according to the inclusion and exclusion. Then the parents were instructed about the study and signed the Informed Consent Form.
NIV was applied with the Interneo or Inter VII ventilator produced by Intermed® or CPAP in a hand-water seal. The physiotherapist on duty was responsible for choosing the equipment that he considered viable and available for use during NIV installation.
The NBs received NIV through a new (non-reused) short binasal prong refill. The interface size was chosen by the research physiotherapist using a specific short binasal prong scale, which makes it possible to choose the prong size based on the nostrils’ diameter and the columella’s width.
The researcher handcrafted the cap with Msó® brand orthopedic tubular mesh and put it on the NB’s head. Then a sheet of hydrocolloid Elect Hidro from the brand Syncera® or Comfeel Plus transparent from Coloplast® was cut into a rectangle and applied over the supralabial region. Next, the researcher separated three rectangular strips of Velcro. One was placed on the hydrocolloid plate, and the other two were wrapped in the prong. After these procedures, the prong was moistened with saline solution and introduced into the NB’s nostril, and the tracheas of the circuit were attached to the cap with a safety pin and an elastic band.
All NBs were reassessed every 24 hours after the installation of NIV until the medical suspension of ventilatory support. In the reassessment, the researcher, through visual inspection, evaluated the need to change the size of the interface and/or the type of fixation. In addition, the care team was asked about possible difficulties related to using NIV with the short binasal prong.
Statistical Analysis
Descriptive analysis was used to characterize the participants’ sociodemographic data for the first stage.
For both stages, central tendency and dispersion measures were expressed as means and standard deviation (mean + SD) for continuous variables with symmetric distribution and as medians, minimum and maximum values (median, minimum – maximum) for those with asymmetric distribution. Categorical variables were expressed in absolute and relative frequency.
Statistical analysis was also performed using the SPSS® v.22 software.
Results
First Stage
Ninety professionals participated in the study, 12 nurses, 13 physiotherapists, 15 neonatologists and 50 nursing technicians. Figure 1 presents the flowchart.
 |
Figure 1 Sample selection flowchart for first stage. |
Table 1 presents the sociodemographic characteristics of the sample. Most professionals were female (91.1%). The average age of professionals was 39.9 ± 6.7 years, with no difference between genders (p = 0.73), and the average time of experience in Neonatology was 9.71 ± 4.87 years.
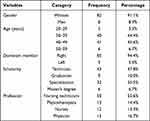 |
Table 1 Sociodemographic Characteristics of the Health Professionals (n=90) |
The average score referring to the professionals’ level of concerning the short binasal prong was 3.84 ± 0.62 points. The item that presented the best level of professional satisfaction was weight (mean of 4.33). On the other hand, the items with the worst ratings were ease of adjustment (mean 3.27) and dimensions (mean 3.62). Table 2 presents the satisfaction scores for each of the 8 items assessed by Quest-B.
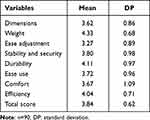 |
Table 2 Satisfaction Degree of Health Professionals for Items Related to the Characteristics of the Short Binasal Prong |
Table 3 shows the explanations of health professionals who justified each item evaluated by Quest-B when the satisfaction level was less than 5.
 |
Table 3 Additional Comments by Health Professionals Regarding Prong Usability Problems |
Second Stage
The sample was selected for convenience, subject to the availability of the researcher for data collection, as shown in Figure 2. The characteristics of the second stage sample are shown in Table 4.
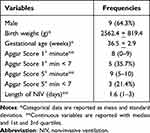 |
Table 4 Characteristics of Newborns (n=14) |
 |
Figure 2 Sample selection flowchart for second stage. |
The mean NBs weight in NIV installation (g) was 2758.6 + 1025.9, and the head circumference at NIV installation (cm) was 33.4 + 2.8. The NIV indication was elective post- extubation (71.4%) and Respiratory Distress (28.6%). The majority of them used Bubble CPAP handmade (78.6%). 50.0% used interface size number 4, 28.6% the number 3, and the others number 2. In 64.3%, the short binasal prong size was adequate without the need to change the size of the short binasal prongs. It was found that in 5 NBs (35.7%), the size indicated by the ruler did not correspond to the ideal size for the NB, and in three of them, the chosen prong did not enter the nostrils; therefore, the smaller prong size was selected. However, in all cases, the smaller prong pinched the septum. In two cases, the largest prong was too small for the NB.
The difficulties reported by the technical team during the use of NIV in the NBs studied are presented in Figure 3.
 |
Figure 3 Difficulties reported using the short binasal prong in the evaluated newborns. |
Circuit disconnection was the difficulty most reported by the team. To minimize disconnections, the team uses adhesive tape or elastic bandage to maintain the circuit connection (Figure 4a).
Figure 4b illustrates the difficulty with existing short binasal prong sizes. It is possible to observe that the prong used is small for the NB; however, the larger number of prongs did not enter the nostrils.
The presence of leakage from the circuit through the nostrils or the mouth was another difficulty reported by the technical team, requiring the introduction of hydrocolloids in the nasal region to minimize the loss of pressure through the nose. In addition, to minimize the loss of pressure through the mouth, it is common in the NICU to use restraint in the mandibular region to keep the mouth closed or to use a pacifier made with a silicone glove and seal the circuit (Figure 4c).
Another difficulty reported by the team was maintaining the proper positioning of the prongs due to difficulty fixing tracheas using pin and elastic in the tubular mesh for their flexibility. In these cases, it was decided to replace the fixation with a pin and elastic band with adhesive tape (Figure 4d).
Proposals for Improvements to Optimize the Design of the Short Binasal Prong
From the results of research stages I and II, the team of this study identified the need to improve short binasal prongs in five requirements: safety, efficacy, adaptation to the anatomical characteristics of NBs, ease of adjustments, and comfort for NBs.
The need for improvement safety was highlighted by a frequent disconnection between the prong and the tracheas and by the report that the prong used in the NICU was very malleable, being easily foldable, which obstructs airflow and loss of pressure supply, exposing the NB to risk.
Improvements in the efficacy is necessary because disconnection between the prong and the NIV circuit causes interruption of positive pressure to the NB and, in addition to jeopardizing the NB’s health, impairs this therapy’s effectiveness. In addition, another item that impairs the effectiveness of NIV is pressure leakage through the mouth and nose. Leakage through the nostrils is related to the inadequacy of the sizes of the existing prongs to the nasal dimensions of the NBs, as observed in the results of stage II of this study.
The need for adaptation to the anatomical characteristics of NBs was verified from the professionals’ report that the prongs have a single length for all sizes and that the insertion catheters are long, making it difficult to adapt to the NB. Moreover, the need for new sizes which adapt to the NBs’ anatomical characteristics was reported in both stages.
Another requirement to be improved is adjustment facilities because the few existing sizes cause frequent disconnections and difficulties in attaching the prong to the NB because force the team to adapt the prong and the NIV circuit to keep it working and positioned inside the nostrils.
Lastly, one more requirement to improve is NBs’ comfort. Difficulties in adapting the prong to the NBs’ anatomical specifications indicate that prongs are uncomfortable, requiring dimensions matching.
Based on the survey of requirements that need to be improved in short binasal prongs, possible improvements were defined to optimize the design of this interface.
We suggested that the short binasal prong has new sizes, which are based on the anatomical characteristics of NBs; that the distance between the insertion catheters and the base is adjustable; that it is malleable, however, that it does not bend easily; have curved and flexible insertion catheters and present a functional system for connecting to the tracheas.
Sizes Based on the Anatomical Characteristics of Newborns
Expanding and adjusting the prongs’ dimensions to the NB’s anthropometric dimensions will make them more functional, with less probability of leakage through the nostrils, improving their efficiency, safety, and comfort.
Distance Between Adjustable Insertion Catheters
It is recommended that the short binasal prong has an adjustable distance between the insertion catheters. Making it regulable implies reducing the compression of the nasal columella, facilitating the settlement of the prong to the NB’s nostrils, and promoting comfort during its use.
Prong Made with Malleable Material, but Not Foldable
It is suggested that the material used for making the prongs be malleable, however, not easily foldable, since the interruption of positive pressure compromises the safety and efficacy of NIV.
Adjustable Base Length
Aiming to respect the facial anatomy and facilitate adjustments of the prong to the NB, it is recommended that the nasal prongs have regulable sides to allow them to be shortened or lengthened according to the width of the NB’s face.
Curved and Adjustable Insertion Catheters
Based on the recommendations presented by health professionals and aiming to improve the adjustments of the prong to the NB’s nostrils, the short binasal prong must have curved insertion catheters and a system that allows adjustment in its length. Such adaptations would facilitate the prongs matching in NBs, promoting better comfort during the NIV application.
Functional Connection System to Tracheas
Disconnection of the prong from the NIV circuit compromises safety and effectiveness and makes it difficult to adjust this device to the NB. Based on the demand presented by health professionals, and the results of stage II, it is necessary to develop a functional system of connection to the tracheas. For this, improvements in the prongs and elbows must be implemented.
As for the prongs, the sides could be narrower and corrugated internally. Furthermore, as for the elbows, these could be longer. In addition, the part which connects with the prong must remain corrugated, as it increases the friction between surfaces, making it difficult to disconnect.
Discussion
This work aimed to evaluate the level of satisfaction of the multidisciplinary team regarding the short binasal prong and identify the possible difficulties faced with using this interface in clinical practice to verify the need for improvements in these devices.
Most of the professionals evaluated have an average of 10 years of experience in neonatology. The broad experience of those professionals lends credibility to the responses, as they had extensive practical experience with NBs submitted to NIV.
All health professionals who participated in this study are responsible for the babies in NICU, each with his attributions. Since the team works together to check that NB receives NIV properly and everyone has direct contact with the nasal prongs, all those professionals were invited to participate in the study.
We found that the professionals were unsatisfied with the dimensions and adjustments of the short binasal prongs but satisfied with the weight, stability and safety, durability, ease of use, comfort, and effectiveness of this interface.
This short binasal prongs are available in 5 sizes, namely: 00, 0, 1, 2, 3, and 4.19 Although there is a variety of sizes from this brand, lack larger sizes and intermediate sizes, existing sizes do not meet the anatomical characteristics of NBs and the prong base length is the same for all existing sizes. This dissatisfaction was proven by the difficulties encountered with using the prong in stage II, in which in 5 NBs (35.13%), the chosen size did not adapt to the anatomical characteristics of the NBs.
The prong with the correct diameter reduces air escape and prevents nasal damage.20 The small caliber prong can become mobile inside the nostrils and, due to friction, can cause injury.12 A prong with a caliber greater than the diameter of the nostril can cause enlargement and injury due to increased pressure on the nasal mucosa.21
In the HIWM NICU, the physiotherapists and neonatologists are responsible for evaluating the NB and the need for NIV. The physiotherapist is responsible for establishing NIV. He assembles and tests the ventilator to be used, defines the size of the prong, defines the cap to be used, connects and fixes the prong on the NB, and, together with the neonatologist, define the ventilatory parameters, and both are responsible for weaning this ventilatory support later. Physiotherapist, neonatologist, nurses and nursing technicians are all responsible for the care and monitoring of NBs on NIV, helping to maintain the proper positioning of the prongs and NIV circuits. Those professionals face the practical difficulties of keeping NIV working correctly, and develop several adaptations, such as using adhesive tape on the connections, to minimize air leaks and keep the prong and circuit connected and well-placed.
In addition to being less satisfied with the prongs’ sizes, according to Quest-B results, the professionals are also less satisfied with the adjustments of the short binasal prongs. This dissatisfaction may be related to the frequent disconnection between the prongs and the NIV circuit and the fixation of the circuit, which is performed with a tubular mesh, safety pin, and elastic band.
Disconnection of the NIV circuit was the main difficulty reported by the team. It may be associated with the design of the elbows that connect the prongs to the tracheas, which are short, facilitating frequent disconnection of the circuit, and may also be associated with the sterilization process of the prongs and NIV circuit, which causes enlargement of the tracheal tips and the sides of the prongs, compromising the connection between both.
The NICU studied, and in many Brazilian NICUs, nasal prongs and NIV circuits are reused in NBs after being submitted to ethylene oxide sterilization procedures for economic reasons. Due to the high costs of the NIV circuit, we sterilized the material in stage II because it was impossible to acquire new NIV circuits The circuits available at the HIWM NICU were made by Gabisa Medical International (GMI®). Although we used sterilized NIV circuits, it should be noted that the attempt to reduce costs by using reprocessed materials must be corrected and can occur both due to economic problems and a lack of awareness of health services. However, we reiterate that this only occurred in this research due to the difficulty of financial resources, which is a limitation of the study.
We observed that the tubular mesh used in stage II was very malleable, and this may have compromised the effectiveness of prong fixation in the NB, as the cap allowed mobility and traction of the tracheas, facilitating the disconnection of the circuit, as well as the difficulty of proper positioning of the prong inside the nostrils.
Frequent disconnections between the prong and the circuit and the difficulty in keeping the prong positioned adequately inside the nostrils increase the number of NBs to handle. Excessive handling and procedures, especially in premature infants, can alter blood pressure and cerebral blood flow, resulting in peri-interventricular hemorrhage and possible brain damage with sequelae for neuro psychomotor development.22 In addition, excessive handling negatively alters the sleep of premature infants, which is essential for brain maturation and the limbic, olfactory, tactile, and auditory neurosensory systems.23 Furthermore, disconnections from the circuit can compromise the effectiveness of NIV, causing damage to the health of NBs, as well as making them more vulnerable to possible infections due to excessive handling of the circuit and the presence of adhesive tapes placed in the system, in an attempt to keep the prong and tracheas connected.
Another difficulty reported by the team with the use of NIV was the presence of leakage, that is, loss of positive pressure through the oral or nasal route, which can compromise the effectiveness of ventilatory support. Air leakage through the mouth is a disadvantage of NIV with short binasal prongs.14 Due to the weakness of the orofacial muscles, premature infants are more likely to open their mouths when the pressure in the oropharynx increases due to NIV application.15
De Paoli et al16 compared the pharyngeal pressure of 11 premature infants who received CPAP with a Hudson®’s short binasal prong with the mouth open and actively closed. They observed an average pressure drop of 3.2 (2.6 to 3.7) cmH2O with the mouth open and 2.2 (1.6 to 2.8) cmH2O with the mouth closed, and they concluded that closing the mouth increases the transmission of CPAP. In our study, chin straps or pacifiers are used in NBs on NIV only when pressure loss compromises the NB’s clinical stability.
As for the loss of pressure through the nose, this is associated with the size of the prongs and nostrils,24 in which the insertion catheters are small concerning to the dimensions of the NB’s nostrils, not wholly sealing them. Therefore, in addition to being indicated to prevent nasal lesions, hydrocolloids can seal the nostrils, preventing leaks.25 We used hydrocolloids only in cases where the leak compromised the clinical stability of the NB.
In stage II, we observed that the prong used was too small for the NB’s nostril in 35.7%. This fact could be associated with the presence of leakage from the nose.
An interface of adequate size is essential to ensure that the NB receives the necessary pressures and enjoys the benefits of NIV. In addition, it reduces the risk of nasal injury, optimizes the professional’s work since he spends less time trying to adapt the prong to the nostrils, and reduces public spending on health, both by preventing waste with materials and by reducing the expenses allocated to the treatment of comorbidities associated with nasal injury.
The three items reported by professionals as the most important in an interface were: comfort, efficacy, and safety, and these are directly involved with adjustments and dimensions of the prong, which presented the lowest satisfaction scores. To achieve comfort, effectiveness, and safety, the prong used in the NB must have adequate size and fixation.
The results from steps I and II signaled the need for improvements in the design of short binasal prongs. In addition, new sizes are needed to make them more adaptable to the anatomical characteristics of NBs, promoting comfort and reducing leaks through the nostrils.
According to Chawla et al26 due to the unique anatomy of the NB, it is almost impossible for manufacturers of NIV interfaces to build different sizes and shapes that meet the fullness of NBs. However, one way to assist most of NBs would be to adjust the distance between insertion catheters. It is believed that this characteristic, combined with the proposal of new sizes based on the diameters of the nostrils, would make the binasal prong more adapted to the anatomical characteristics of NBs, thus improving the safety, efficacy, and comfort of this interface.
Another parameter to improve the prong’s design was using malleable material to make it not easily foldable, preventing the insertion of catheters from collapsing, ensuring the delivery of positive pressure to the NB, and providing safety and efficacy of this therapy. It should be noted that it was not part of the scope of this research the studies and indication of the most suitable material for manufacturing prongs.
The last parameter defined to improve the design of the prongs was to make the system connecting the prongs to the tracheas effective. Although the disconnection may be a consequence of sterilization of the circuit, which causes the widening of the connections, the site of the prong that connects to the elbows is internally smooth and, due to the humidification of the circuit, it ends up sliding over the elbows, thus favoring the disconnection. Furthermore, the circuit elbows are short, which can also favor disconnection; therefore, it is assumed that elbows of greater length would make disconnection more difficult.
Because of limitations, this study could not precisely evaluate the short binasal prong and the other components of the NIV circuit, since there needed more financial resources to acquire new NIV circuits. However, with the donation of short binasal prongs, stages I and II evaluations were directed exclusively to this device.
Regarding evaluating only Fanem® short binasal prong, we acknowledge that our study focused solely on this particular device. This choice was determined by the fact that our NICU exclusively used Fanem® prongs during the study period. As part of a public hospital with limited resources, our scope was to assess the technology implemented in a specific NICU rather than conducting a comparison of prongs from different brands. The intention was to assess the usability and satisfaction of healthcare professionals with the available technology and propose improvements based on the findings, hoping to benefit the newborns in NICU.
The prospective nature of our study aimed to gather insights and perspectives from healthcare professionals regarding the satisfaction and challenges associated with the specific short binasal prong used in studied NICU (Fanem®). It is important to note that those professionals play distinct roles in the newborns care under non-invasive ventilation, and their perspectives are valuable in understanding the challenges and potential improvements related to the short binasal prong. While the findings provide valuable information about the experiences of those professionals in our specific context, we recognize that it may not be directly applicable to other NIV nasal prongs or settings.
It is important to highlight that the study was conducted using rigorous methodologies and included a diverse group of experienced healthcare professionals in the NICU setting. The data collected were based on their real-world experiences and perceptions. However, it is important to note that the interpretation of qualitative data should consider its subjective nature and the potential for individual biases. Therefore, measures were took to ensure the reliability and validity of the data through appropriate data collection techniques and rigorous analysis.
Finally, it is essential to emphasize that this study was restricted to just pointing out suggestions for improvements based on feedback from health professionals and on the survey of difficulties related to the use of nasal prongs in NBs submitted to NIV. The specifications of the improvement processes and the study of their viability will be addressed in future studies.
Conclusion
Professionals working at the NICU are dissatisfied with the dimensions and adjustments of the short binasal prong, signaling the need for improvements in both aspects; in clinical practice, the difficulties associated with the use of prongs in NBs are related to the choice of the appropriate size, proper fixation, and positioning of the prongs in the NBs, the presence of leakage and frequent disconnection of the NIV circuit.
Short binasal prongs need improvements: safety, efficacy, adaptation to the anatomical characteristics of NBs, ease of adjustments, and comfort for NBs. For this, we suggested that the prongs have new sizes, which are based on the anatomical characteristics of the NBs; that the distance between the insertion catheters and the base is adjustable; that it is malleable, however, that it does not bend easily; have curved and flexible insertion catheters and present a functional system for connecting to the tracheas.
Abbreviations
CPAP, Continuous positive airway pressure; GMI, Gabisa Medical International; HIWM, Hospital Infantil Waldemar Monastier; NB, Newborn; NICU, Neonatal Intensive Care Unit; NIV, Non-invasive ventilation.
Ethics Approval and Informed Consent
This study was performed in accordance with national and international requirements that conduct ethics in research involving human beings, following the Declaration of Helsinki, and approved by the Ethics Committee on Research Involving Human Beings of the Pontifícia Universidade Católica do Paraná - PUCPR under Approval Letter numbers 03198318.5.0000.0020, and 89268418.0.0000.0020. The newborns’ parents were informed about the study and provided written informed consent.
Acknowledgments
We thank Fundação Araucária, Secretaria de Estado da Ciência, Tecnologia e Ensino Superior do Paraná (SETI), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for scholarships, and Waldemar Monastier Children’s Hospital directly for allowing the study to be performed on the NICU’s premises, Caobianco Materiais Médicos e Hospitalares for the donation of Fanem® prong.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fedor KL. Noninvasive respiratory support in infants and children. Respir Care. 2017;62(6):699–717. doi:10.4187/respcare.05244
2. Shi Y, Muniraman H, Biniwale M, Ramanathan R. A review on non-invasive respiratory support for management of respiratory distress in extremely preterm infants. Front Pediatr. 2020;8:270. doi:10.3389/fped.2020.00270
3. Sahni R, Schiaratura M, Polin RA. Strategies for the prevention of continuous positive airway pressure failure. Semin Fetal Neonatal Med. 2016;21(3):196–203. doi:10.1016/j.siny.2016.02.008
4. Chandrasekaran A, Thukral A, Jeeva Sankar M, Agarwal R, Paul VK, Deorari AK. Nasal masks or binasal prongs for delivering continuous positive airway pressure in preterm neonates-A randomised trial. Eur J Pediatr. 2017;176(3):379–386. doi:10.1007/s00431-017-2851-x
5. Greenough A, Lingam I. Invasive and non-invasive ventilation for prematurely born infants - current practice in neonatal ventilation. Expert Rev Respir Med. 2016;10(2):185–192. doi:10.1586/17476348.2016.1135741
6. De Paoli AG, Davis PG, Faber B, Morley CJ. Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database Syst Rev. 2008;2008(1):CD002977. doi:10.1002/14651858.CD002977.pub2
7. Wung JT, Driscoll JM Jr, Epstein RA, Hyman AI. A new device for CPAP by nasal route. Crit Care Med. 1975;3(2):76–78. doi:10.1097/00003246-197503000-00006
8. Boel L, Broad K, Chakraborty M. Non-invasive respiratory support in newborn infants. Paediatr Child Health. 2018;28(1):6–12. doi:10.1016/j.paed.2017.10.007
9. Sankar MJ, Sankar J, Agarwal R, Paul VK, Deorari AK. Protocol for administering continuous positive airway pressure in neonates. Indian J Pediatr. 2008;75(5):471–478. doi:10.1007/s12098-008-0074-x
10. Khan J, Sundaram V, Murki S, Bhatti A, Saini SS, Kumar P. Nasal injury and comfort with jet versus bubble continuous positive airway pressure delivery systems in preterm infants with respiratory distress. Eur J Pediatr. 2017;176(12):1629–1635. doi:10.1007/s00431-017-3016-7
11. Li Y, Sepulveda A, Buchanan EP. Late presenting nasal deformities after nasal continuous positive airway pressure injury: 33-year experience. J Plast Reconstr Aesthet Surg. 2015;68(3):339–343. doi:10.1016/j.bjps.2014.10.036
12. Nascimento RM, Ferreira ALC, Coutinho AC, Veríssimo RC. The frequency of nasal injury in newborns due to the use of continuous positive airway pressure with prongs. Rev Latino Am Enfermagem. 2009;17:489–494. doi:10.1590/S0104-11692009000400009
13. Galetto SG, Nascimento ER, Hermida PMV, Malfussi LB. Medical device-related pressure injuries: an integrative literature review. REBEn. 2019;72:505–512.
14. Johnston C. Ventilação não invasiva Rio de Janeiro Atheneu; 2018.
15. Fischer HS, Roehr CC, Proquitte H, Schmalisch G. Influence of nose and mouth leaks on peripheral oxygen saturation during continuous positive airway pressure in neonates. World J Pediatr. 2013;9(4):318–322. doi:10.1007/s12519-013-0435-z
16. De Paoli AG, Lau R, Davis PG, Morley CJ. Pharyngeal pressure in preterm infants receiving nasal continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 2005;90(1):F79–81. doi:10.1136/adc.2004.052274
17. Rego MA, Martinez FE. Repercussões clínicas e laboratoriais do CPAP nasal em recém-nascidos pré-termo. J Pediatr. 2000;76(5):339–348. Portuguese. doi:10.2223/JPED.125
18. Carvalho KEC, Gois Júnior MB, Sá KN. Translation and validation of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) into Portuguese. Rev Bras Reumatol. 2014;54(4):260–267. doi:10.1016/j.rbr.2014.04.003
19. Fanem. Kit CPAP; 2020. Available from: https://fanem.com.br/pt/produtos/kit-cpap/.
20. De Paoli AG, Morley C, Davis PG. Nasal CPAP for neonates: what do we know in 2003? Arch Dis Child Fetal Neonatal Ed. 2003;88(3):F168–172. doi:10.1136/fn.88.3.F168
21. Squires AJ, Hyndman M. Prevention of nasal injuries secondary to NCPAP application in the ELBW infant. Neonatal Netw. 2009;28(1):13–27. doi:10.1891/0730-0832.28.1.13
22. Ponte MD, Marba STM. Peri-intraventricular hemorrhage in newborns weighing less than 1500 grams: comparative analysis between 2 institutions. Rev Hosp Clín. 2003;58:299–304. doi:10.1590/S0041-87812003000600002
23. Orsi KCSC, Avena MJ, Lurdes de Cacia Pradella-Hallinan M, et al. Effects of handling and environment on preterm newborns sleeping in incubators. J Obstet Gynecol Neonatal Nurs. 2017;46(2):238–247. doi:10.1016/j.jogn.2016.09.005
24. Kahn DJ, Courtney SE, Steele AM, Habib RH. Unpredictability of delivered bubble nasal continuous positive airway pressure: role of bias flow magnitude and nares-prong air leaks. Pediatr Res. 2007;62(3):343–347. doi:10.1203/PDR.0b013e318123f702
25. Chen C-Y, Chou A-K, Chen Y-L, Chou H-C, Tsao P-N, Hsieh W-S. Quality improvement of nasal continuous positive airway pressure therapy in neonatal intensive care unit. Pediatr Neonatol. 2017;58(3):229–235. doi:10.1016/j.pedneo.2016.04.005
26. Chawla D. Optimizing nasal interface for continuous positive airway pressure in neonates. Indian Pediatr. 2015;52(12):1027–1028. doi:10.1007/s13312-015-0767-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

