Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 15
Saliva-Based Protein Analysis in Pediatric Dentofacial Inflammation
Authors Orzechowska-Wylęgała B , Wylęgała A, Zalejska Fiolka J, Czuba Z , Toborek M
Received 14 September 2023
Accepted for publication 9 January 2024
Published 27 February 2024 Volume 2024:15 Pages 95—102
DOI https://doi.org/10.2147/PHMT.S440223
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Bogusława Orzechowska-Wylęgała,1 Adam Wylęgała,2 Jolanta Zalejska Fiolka,3 Zenon Czuba,4 Michal Toborek5
1Department of Pediatric Otolaryngology, Head and Neck Surgery, Chair of Pediatric Surgery, Medical University of Silesia (SUM), Katowice, Poland; 2Health Promotion and Obesity Management, Department of Pathophysiology in Katowice, SUM, Katowice, Poland; 3Department of Biochemistry Faculty of Medical Science in Zabrze, SUM, Katowice, Poland; 4Department and Division of Microbiology and Immunology in Zabrze, SUM, Katowice, Poland; 5Department of Biochemistry and Molecular Biology, University of Miami, School of Medicine, Miami, FL, USA
Correspondence: Bogusława Orzechowska-Wylęgała, Email [email protected]
Aim: Saliva contains various proteins that are important in developing inflammatory processes and their prevention. One key aspect of saliva research is the relationship between oral infections and inflammation, and the role of some salivary proteins.
The Work Aims: To demonstrate which salivary cytokines can be biomarkers of acute odontogenic oral and facial infections in children.
Material and Methods: The study included two groups of patients: a study group of 28 children: 7 girls and 21 boys aged 3 − 17 years with acute dentofacial inflammation (DI) and a control group of 52 children: 16 girls and 36 boys aged 4– 17 years with uncomplicated dental caries (CE). The levels of Interleukin-5 (IL-5), Interleukin − 10 (IL-10), Interleukin-17A (IL-17A), Interleukin-12p70 (IL-12p70), Eotaxin, Rantes, Vascular Endothelial Growth Factor (VEGF), and Interferon gamma-induced protein 10 (IP10) in the saliva of children in DI and CE groups were compared. Statistical analysis was performed with Statistica 13. The Student’s t-test and the Wilcoxon signed-rank test were used.
Results: The results show that IL-10, IL-17A, and Eotaxin showed a statistically significant increase in the DI group compared to the CE group. The significance level for IL-10 was p=0.02, for IL-17A was equal to Eotaxin and p=0.04. The other measured parameters did not differ statistically significant between the two groups.
Conclusion: IL-10, IL-17A, and Eotaxin can be used as potential biomarkers for tooth-related inflammatory states of the oral cavity and face in children. These biomarkers can be useful in identifying and monitoring the presence of inflammation in the oral cavity and face.
Keywords: salivary cytokines and chemokines, odontogenic oral and facial inflammation, children
Dentofacial Inflammation of the head and neck in children refers to inflammation or infection originating from the teeth, potentially causing swelling, pain, and complications such as difficulty swallowing or breathing. This condition often results from untreated dental caries, abscesses, or periodontal disease.1,2 Immediate dental and medical attention is crucial to prevent the infection from spreading and causing more serious health complications.3 Anatomical differences that significantly impact the course of inflammatory processes in the facial tissues of the skull in children are associated with a lower degree of jaw bone calcification, the presence of wide marrow spaces with a well-developed vascular system, the presence of tooth buds, as well as the existence of a slit-like, undeveloped maxillary sinus and a greater amount of cancellous bone. Additionally, a distinct immunologic response contributes to the dynamic development of the inflammatory process within the head and neck tissues, leading to the spread of inflammation to the eye socket, sinus cells, and cranial cavity. The higher water content and lower fat tissue content in pediatric patients, along with qualitative and quantitative differences in blood-borne drug transport proteins, determine variations in the pharmacokinetics of drugs, including antibiotics.4–6
Saliva is a readily available, low-cost, and non-invasive biofluid. This is important, especially for children who may find it very difficult to draw blood. Analysis of the saliva can provide insights into various health conditions. Salivary proteins play crucial roles in various biological processes, and changes in protein profiles can be indicative of specific conditions, including inflammation. This study focuses on the analysis of specific saliva proteins, including Interleukin-5 (IL-5), Interleukin-10 (IL-10), Interleukin-17A (IL-17A), Interleukin-12p70 (IL-12p70), Eotaxin, Rantes, Vascular Endothelial Growth Factor (VEGF), and Interferon gamma-induced protein 10 (IP10). These proteins are key players in the immune response and inflammation regulation within the body, participating in processes such as chemotaxis, immune cell recruitment, and angiogenesis.7,8 Several reviews have described the evidence of salivary cytokines as biomarkers for oral conditions.5,7–11 Understanding these biomarkers can contribute to a comprehensive comprehension of pediatric dentofacial inflammation and guide effective preventive and therapeutic strategies.7
No publications were found in the available literature on cytokines and chemokines in the saliva of children with dentofacial inflammation.
Interleukin-5 (IL-5) - a type of cytokine that is involved in the stimulation and regulation of the growth, differentiation, and activation of certain immune cells, particularly eosinophils, in response to infections, allergens, and parasites.12,13
Interleukin-10 (IL-10) is involved in regulating the immune system. IL-10 is primarily produced by immune cells such as macrophages, monocytes, and T-cells, and plays an important role in controlling inflammation and the body’s response to infection.14
IL-10 is often considered an “anti-inflammatory” cytokine because it can reduce the production of other pro-inflammatory cytokines and limit the activity of immune cells involved in the inflammatory response. This can help to prevent excessive or chronic inflammation, which can contribute to various diseases and conditions such as autoimmune disorders and allergies. IL-10 is also involved in other functions within the immune system, such as promoting the development and activity of regulatory T-cells, which help prevent the immune system from attacking the body’s tissues. Additionally, IL-10 may have roles in tissue repair and wound healing.8
Interleukin 17A (IL-17A) - a cytokine produced by a type of immune cell called Th17 cells, and is involved in the regulation of inflammation and immune responses. It plays a role in the defense against certain bacterial and fungal infections, as well as in autoimmune diseases and allergic reactions.15
Interleukin 12p70 (IL-12p70) plays a key role in regulating the immune system. Specifically, it is a heterodimeric cytokine composed of two subunits, IL-12p35 and IL-12p40. IL-12p70 is primarily produced by antigen-presenting cells such as dendritic cells, macrophages, and B-cells, and it helps to activate T-cells and natural killer (NK) cells. IL-12p70 is involved in promoting the production of other cytokines that stimulate the immune response, particularly the production of interferon-gamma. It also helps to direct T-cells towards a “Th1” response, which is important for fighting intracellular pathogens such as viruses and certain bacteria.
The production of IL-12p70 is tightly regulated, as excessive amounts of this cytokine can contribute to inflammatory diseases and autoimmune disorders. Conversely, deficiencies in IL-12p70 or its receptor have been associated with increased susceptibility to infections, particularly those caused by intracellular pathogens. Therefore, maintaining an appropriate balance of IL-12p70 production is crucial for a healthy immune response.
Eotaxin - a chemokine involved in the recruitment of immune cells, specifically eosinophils, to sites of inflammation.13
Rantes - another chemokine involved in the recruitment of immune cells, including T cells and monocytes, to sites of inflammation.
Vascular Endothelial Growth Factor (VEGF) stimulates the growth of new blood vessels.13,16
Interferon gamma-induced protein 10 (IP10) is involved in the recruitment of immune cells, specifically T cells, to sites of inflammation.
The study aimed to compare the levels of IL-5, IL-10, IL-17A, IL-12p70, Eotaxin, Rantes, VEGF, and IP10 in a group of children with uncomplicated dental caries (CE) with a group of children with dentofacial inflammation (DI).
Material and Methods
This prospective observational study, conducted in 2020–2022 at the Department of Pediatric Otolaryngology, Head and Neck Surgery, Chair of Pediatric Surgery of the SUM in Katowice, Poland, aimed to investigate the prevalence and potential biomarkers of acute dentofacial inflammation in children.
Qualification of Patients
The study included 80 systemically healthy children diagnosed with uncomplicated dental caries (CE group) and dentofacial inflammation (DI group).
The diagnosis of dental-related inflammatory conditions is determined according to the criteria established by the World Health Organization (WHO) in 1986. These criteria include clinical, radiographic, and laboratory criteria used to diagnose and classify different types of oral and dental diseases. The WHO criteria provide a standardized approach for diagnosis, which can aid in developing treatment plans and tracking the disease over time.6
The Bioethical Committee of the Medical University of Silesia (SUM) approved the planned study with the reference number PCN/0022/KB1/1/20 and the study complied with the Declaration of Helsinki.
The inclusion criteria for the study were children who were free of any systemic diseases and had not taken any medications in the past month. Children with submucosal abscesses, cellulitis, and osteomyelitis have been classified into the DI group. Exclusion criteria included the occurrence of mucositis, gingivitis, periodontitis, systemic conditions that prevented the continuation of the study, lack of cooperation from the child, and refusal of the parent to conduct the study. All legal guardians and children over the age of 16 signed informed consent for the study.
Clinical Examination and Treatment
The examinations were conducted by a single doctor, visually and by touch, and then intra-orally using a probe and mirror. In the study group, the number of teeth with caries and teeth causing inflammation was determined. In the control group, teeth with uncomplicated caries were determined.1 Parents and older children have explained the purpose of saliva collection.
Saliva Collection
Saliva was collected in the morning between 8:00 and 11:00 am on an empty stomach, after rinsing the mouth with water and waiting 10 minutes. Patients were asked to self-collect 1.5 mL of their unstimulated saliva in a sterile tube, avoiding mucous secretions from the oropharynx and sputum. The saliva was centrifuged for 10 min at 3000 rpm at 4°C in a Centurion centrifuge, and frozen at −80°C for future studies. Rack with 96 coded test tubes, 1.2 mL, PP material, BRAND no cat. 781566 was used to collect the saliva. Their analysis was performed within a period not exceeding 6 months from the moment of freezing.14
Cytokine Analysis
The Luminex platform is a combination of Luminex xMAP instruments and multiplex assays for RNA and protein detection and measurement. Luminex multiplex assays use xMAP bead-based technology to simultaneously detect and quantitate multiple secreted proteins including cytokines, chemokines, and growth factors using ProcartaPlex assays. All the biomarkers were determined from a single kit. The analysis was performed using the Bio-Plex 200 System from Bio-Rad and the Bio-Plex Pro Human Cytokine Grp I Panel 27-Plex kit. The research was carried on in the Department and Division of Microbiology and Immunology, Silesian Medical University in Zabrze.13,17,18 All procedures followed good laboratory practice (GLP). Saliva samples were collected in the Department of Biochemistry Faculty of Medical Science in Zabrze Medical University of Silesia, Katowice, Poland. To avoid bias, all samples have been anonymized and numbered. For biochemical assays, saliva was collected and stored frozen (−80°C) for subsequent analyses. All analytical methods were under continuous interlaboratory quality control and met the criteria of the external (interlaboratory) controls organized by the Central Center for Quality Testing in Laboratory Diagnostics in Łódź (Poland) and Labquality (Finland).
Statistical Analysis
Statistical analysis was performed with Statistica13 (Tibco, Palo Alto, Ca, USA). Normality was assessed using the Shapiro–Wilk test. The Student’s t-test and the Wilcoxon signed-rank test were used for statistical analysis for parametric and nonparametric samples respectively. The normality of the data was assessed using the Shapiro–Wilk test. For Quantitative data either the Wilcoxon test and Student’s t-test were used to compare the levels of the cytokines collected from two independent groups depending on the normality of the data for parametric Student’s t-test was used while for non-parametric data the former. They were used as this is independent of group samples to see if the variability is significant. The study sample size was calculated based on the mean and standard deviation exhibited in the paper by Menon et al 5 The accepted level of significance was set as P ≤ 0.05, with a wanted power of 90%. Using a sample size of 24 patients per group, the study would have had a power of 90.9% to yield statistically significant results under the conditions expressed above.
Results
The study involved two groups of patients: a study group of 28 children (7 girls and 21 boys, aged 3–17 years, mean 8.67 years, SD±4.64 years) with acute dentofacial inflammation (DI) and a control group of 52 children (16 girls and 36 boys, aged 4–17 years, mean 8.38 years, SD±3.67 years) with uncomplicated dental caries (CE).
Therefore, we attempted to compare the levels of cytokines such as IL-5, IL-10, IL-17A, IL-12p70, Eotaxin, Rantes, VEGF, and IP10 in the saliva of children with acute dental-related facial and neck inflammation (DI) with their levels in children with uncomplicated dental caries (CE).
In analyzing the biomarkers related to CE and DI, distinct tendencies and significant observations emerged. The largest differences were observed for IP-10 (1421.91 pg/mL vs 926.03 pg/mL), Rantes (24.73 pg/mL vs 35.15 pg/mL), and VEGF (409.64 pg/mL vs 314.91 pg/mL) for DI and CE respectively. Notably, IL-5 tended towards higher levels (mean: 58.04, median: 39.65), suggesting potential significance in the DI. The variability in IL-5 levels, reflected in the wide range (0.37 to 212.27) and high standard deviation (62.89), underscores the complexity of immune responses.
IL-10, with a central tendency towards moderate values (mean: 8.08, median: 4.33), hinted at its potential involvement in DI. The broad range (0.02 to 85.19) and notable standard deviation (15.66) indicate variability in IL-10 levels, emphasizing its nuanced role.
For IL-12p70, the higher mean and median values (19.06 and 5.91) suggest a tendency towards elevated levels in DI. The wide range (0.47 to 85.54) and substantial standard deviation (27.20) underscore the variability in IL-12p70 levels.
In the case of IL-17A, moderate mean and median values (11.29 and 6.71) indicate a central tendency related to DI. The range (0.94 to 61.53) and standard deviation (12.55) highlight the variability in IL-17A levels, reflecting its potential role.
The range (0.09 to 70.76) and standard deviation (14.88) conveyed variability in Eotaxin levels, offering insights into its potential significance (Table 1).
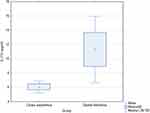
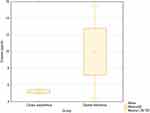
While only IL-10, IL-17A, and Eotaxin showed statistically significant increases in the DI group compared to the CE group, the overall tendency was for all interleukins except for Rantes to be elevated in patients with DI. The significance level for IL-10 was p=0.02 (Figure 1), and for IL-17A (Figure 2) and Eotaxin (Figure 3), it was p=0.04.
Discussion and Conclusion
This is the first study to present a comprehensive cytokine profile of children with dentofacial inflammation. Only Rinderknecht et al showed the associations between salivary cytokines and oral health in the pediatric population.4 They demonstrated that some salivary cytokines positively correlate with gingivitis. Similar observations were made by Santos et al. Belstrøm et al showed negative correlations between salivary cytokine concentration and early gingivitis.9,11 Diesch et al7 in their systematic review compared studies of Sharma et al, Cogulu et al, Menon et al, and Gornowicz et al due to caries in children. The results of Sharma and Gornowicz et al were consistent in levels of IL-6, IL-8, and TNF-α which were significantly higher in patients with caries. A similar result had Menon et al who examined only IL-6 in children with caries.5,8,10,19
To further integrate the information provided, acute dental-origin inflammation of the head and neck in children can lead to the release of various cytokines and chemokines that play important roles in immune response and inflammation. The cytokines IL-5, IL-10, IL-17A, and IL-12p70, along with chemokines such as Eotaxin, Rantes, VEGF, and IP10, are involved in regulating and modulating the immune system’s response to the inflammation caused by dental problems.
This research objective makes sense because comparing cytokine and chemokine levels in children with uncomplicated dental caries to children with acute dental inflammatory conditions can provide important information about the immune system response in these two disease states.
IL-10 is an anti-inflammatory cytokine that helps to regulate and suppress the immune response, limiting the potential for tissue damage and reducing the risk of autoimmunity.
IL-17A is a pro-inflammatory cytokine that plays a role in defending against extracellular bacteria and fungi but may also contribute to the development of chronic inflammation and autoimmune diseases. Recruits monocytes and neutrophils to the site of infection. Activation of IL-17, in turn, activate downstream of many cytokines and chemokine, such as IL‐1, IL‐6, IL‐8, IL‐21, TNF‐β, and MCP‐1.20
Eotaxin is a chemokine that recruits eosinophils, a type of white blood cell, to sites of inflammation. Eosinophils are important in defending against parasites and are also involved in allergic reactions.21
So, while these three molecules play different roles in the immune response, they are all involved in modulating the inflammatory response in some way.14
The results of our investigations show that IL-10, IL-17A, and Eotaxin showed a statistically significant increase in the DI group compared to the CE group. The significance level for IL-10 was p= 0.02, for IL-17A was equal to Eotaxin and it was also p=0.04. This is consistent with the results of other authors.8,15,22
Comparing cytokine levels such as IL-5, IL-10, IL-17A, and IL-12p70, which play important roles in regulating the immune response, can help to understand the differences between the inflammatory and tissue regeneration processes.22
Additionally, Eotaxin, Rantes, VEGF, and IP-10 are chemokines that play a significant role in the chemotaxis and recruitment of different types of cells to sites of infection or inflammation, which can influence the course of the disease.
IL-10, IL-17A, and Eotaxin can be used as potential biomarkers for tooth-related inflammatory states of the oral cavity and face in children. These biomarkers can be useful in identifying and monitoring the presence of inflammation in the oral cavity and face.
Developing a panel of pro-inflammatory cytokines and chemokines in the saliva of children with dental infections could help with loss of control and prevent exacerbations of these diseases.21
If this correlation was indeed found in a well-designed and conducted study, it could potentially improve the diagnosis, treatment, and prevention of oral cavity diseases by providing insights into the underlying mechanisms of immune response and inflammation. However, it is important to note that further research would be needed to confirm and build upon these findings before they could be applied in clinical practice.
In conclusion, understanding the role of these cytokines and chemokines in dental inflammation can help identify markers for early childhood caries (ECC) and contribute to preventive measures and maintaining oral health. Additionally, prompt dental and medical attention is crucial to address the underlying dental problems, prevent complications, and manage the immune response and inflammation associated with acute dental origin inflammation in children.
Acknowledgments
The authors would like to thank all patients and their parents for their participation in the research. This study was supported by scientific grants from the Medical University of Silesia number PCN-1-120/N/O/K.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Słotwińska-Pawlaczyk A, Orzechowska-Wylęgała B, Latusek K, Roszkowska AM. Analysis of clinical symptoms and biochemical parameters in odontogenic cellulitis of the head and neck region in children. Children. 2023;10(1):172. doi:10.3390/children10010172
2. Słotwińska-Pawlaczyk A, Orzechowska-Wylęgała B, Latusek K, Roszkowska AM. Analysis of the clinical status and treatment of facial cellulitis of odontogenic origin in pediatric patients. Int J Environ Res Public Health. 2023;20(6):4874. doi:10.3390/IJERPH20064874
3. Frimpong A, Owusu EDA, Amponsah JA, et al. Cytokines as potential biomarkers for differential diagnosis of sepsis and other non-septic disease conditions. Front Cell Infect Microbiol. 2022;12:1. doi:10.3389/FCIMB.2022.901433/FULL
4. Rinderknecht C, Filippi C, Ritz N, et al. Associations between salivary cytokines and oral health, age, and sex in healthy children. Sci Rep. 2022;12(1):15991. doi:10.1038/s41598-022-20475-2
5. Madhavan Menon M, Varma Balagopal R, Sajitha K, et al. Evaluation of salivary interleukin-6 in children with early childhood caries after treatment. Contemp Clin Dent. 2016;7(2):198. doi:10.4103/0976-237X.183059
6. Tandon S, Satyamoorthy K, Bhalla S. Salivary proteins and early childhood caries: a gel electrophoretic analysis. Contemp Clin Dent. 2010;1(1):17. doi:10.4103/0976-237X.62515
7. Diesch T, Filippi C, Fritschi N, Filippi A, Ritz N. Cytokines in saliva as biomarkers of oral and systemic oncological or infectious diseases: a systematic review. Cytokine. 2021;143. doi:10.1016/J.CYTO.2021.155506
8. Cogulu D, Onay H, Ozdemir Y, et al. Associations of interleukin (IL)-1β, IL-1 receptor antagonist, and IL-10 with dental caries. J Oral Sci. 2015;57(1):31–36. doi:10.2334/josnusd.57.31
9. Belstrøm D, Damgaard C, Könönen E, Gürsoy M, Holmstrup P, Gürsoy UK. Salivary cytokine levels in early gingival inflammation. J Oral Microbiol. 2017;9(1):1364101. doi:10.1080/20002297.2017.1364101
10. Gornowicz A, Bielawska A, Bielawski K, et al. Pro-inflammatory cytokines in saliva of adolescents with dental caries disease; 2012. Available from: www.aaem.pl.
11. Santos MTBR, Diniz MB, Guaré RO, Ferreira MCD, Gutierrez GM, Gorjão R. Inflammatory markers in saliva as indicators of gingival inflammation in cerebral palsy children with and without cervical motor control. Int J Paediatr Dent. 2017;27(5):364–371. doi:10.1111/ipd.12270
12. Zheng L, Yang C, Zhang W, et al. Is there association between severe multispace infections of the oral maxillofacial region and diabetes mellitus? J Oral Maxillofacial Surg. 2012;70(7):1565–1572. doi:10.1016/j.joms.2011.07.010
13. Idzik M, Poloczek J, Skrzep-Poloczek B, et al. The effects of 21-day general rehabilitation after hip or knee surgical implantation on plasma levels of selected interleukins, VEGF, TNF-α, PDGF-BB, and Eotaxin-1. Biomolecules. 2022;12(5):605. doi:10.3390/BIOM12050605
14. Novak T, Hamedi M, Bergmeier LA, Fortune F, Hagi-Pavli E. Saliva and serum cytokine profiles during oral ulceration in behçet’s disease. Front Immunol. 2021;2021:12. doi:10.3389/FIMMU.2021.724900/FULL
15. Zielińska K, Karczmarek-Borowska B, Kwaśniak K, et al. Salivary IL-17A, IL-17F, and TNF- α are associated with disease advancement in patients with oral and oropharyngeal cancer. J Immunol Res. 2020;2020. doi:10.1155/2020/3928504
16. Pammer J, Weninger W, Mildner M, Burian M, Wojta J, Tschachler E. Vascular endothelial growth factor is constitutively expressed in normal human salivary glands and is secreted in the saliva of healthy individuals. J Pathol. 1998;182(2). doi:10.1002/(SICI)1096-9896
17. Lejawa M, Osadnik K, Czuba Z, Osadnik T, Pawlas N. Association of metabolically healthy and unhealthy obesity phenotype with markers related to obesity, diabetes among young, healthy adult men. Analysis of MAGNETIC study. Life. 2021;11(12). doi:10.3390/LIFE11121350
18. Grudzińska E, Grzegorczyn S, Czuba ZP. Chemokines and growth factors produced by lymphocytes in the incompetent great saphenous vein. Mediators Inflamm. 2019;2019. doi:10.1155/2019/7057303
19. Sharma V, Gupta N, Srivastava N, et al. Diagnostic potential of inflammatory biomarkers in early childhood caries - A case control study. Clin Chim Acta. 2017;471:158–163. doi:10.1016/J.CCA.2017.05.037
20. Yui S, Sasayama D, Yamaguchi M, Washizuka S. Altered levels of salivary cytokines in patients with major depressive disorder. Clin Neurol Neurosurg. 2022;221:107390. doi:10.1016/J.CLINEURO.2022.107390
21. Little FF, Delgado DM, Wexler PJ, et al. Salivary inflammatory mediator profiling and correlation to clinical disease markers in asthma. PLoS One. 2014;9(1). doi:10.1371/JOURNAL.PONE.0084449
22. Szulimowska J, Zalewska A, Taranta-Janusz K, Marczuk-Kolada G, Żendzian-Piotrowska M, Maciejczyk M. Association between salivary cytokines, chemokines and growth factors and salivary gland function in children with chronic kidney disease. J Inflamm Res. 2023;16:1103–1120. doi:10.2147/JIR.S399786
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.