Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Safety and efficacy of paliperidone palmitate 1-month formulation in Chinese patients with schizophrenia: a 25-week, open-label, multicenter, Phase IV study
Authors Zhao JP, Li LH, Shi JG, Li Y, Xu XF, Li KQ, Zhang LL , Cai SL, Feng Y, Zhuo JM, Liu WH, Lu HF
Received 29 December 2016
Accepted for publication 11 May 2017
Published 2 August 2017 Volume 2017:13 Pages 2045—2056
DOI https://doi.org/10.2147/NDT.S131224
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wai Kwong Tang
Jingping Zhao,1,* Lehua Li,1,* Jianguo Shi,2 Yi Li,3 Xiufeng Xu,4 Keqing Li,5 Lili Zhang,6 Shangli Cai,6 Yu Feng,6 Jianmin Zhuo,6 Weihong Liu,6 Huafei Lu6
1Department of Psychiatry, The Mental Health Institute, The Second Xiangya Hospital of Central South University, 2Department of Psychiatry, Mental Health Center of Xi’an City, 3Department of Psychiatry, Mental Health Center of Wuhan City, 4Department of Psychiatry, First Affiliated Hospital of Kunming Medical University, 5Department of Psychiatry, The Sixth People’s Hospital of Hebei Province, 6Department of Medical Affairs, Xi’an Janssen Pharmaceutical Ltd., Beijing, People’s Republic of China
*These authors contributed equally to this work
Rationale: Long-acting injectable (LAI) paliperidone palmitate 1-month formulation (PP1M) has demonstrated acceptable tolerability and favorable clinical outcomes in Western and Asian patients with schizophrenia. Hence, analysis of the outcomes of long-term PP1M treatment specifically in Chinese patients is of interest.
Objective: The aim of this study is to evaluate the long-term safety and efficacy of PP1M treatment in Chinese patients with schizophrenia.
Methods: In this 25-week, open-label, Phase IV study, patients (18–65 years) diagnosed with schizophrenia and having a baseline Positive and Negative Syndrome Scale (PANSS) total score of 60–120 (inclusive) were enrolled. All patients received injections of PP1M 150 mg eq. (day 1) and 100 mg eq. (day 8), followed by a flexible once-monthly maintenance dosing (75, 100, or 150 mg eq.).
Results: Of the 353 patients, 234 (66.3%) completed the study treatment (mean age, 31.1 years; 52.7% men). The PANSS total score (primary end point) improved significantly over the 6-month treatment period (mean [standard deviation] change from baseline to end of treatment, -27.2 [18.30]; P<0.0001). The Clinical Global Impressions-Severity and Personal and Social Performance scores (secondary end points) also improved significantly (P<0.0001). At 6 months, PP1M had a positive impact on medication satisfaction, adherence, and increased preference for LAIs. Treatment-emergent adverse events (TEAEs) were reported by 181 (51.3%) patients (TEAEs ≥5%: extrapyramidal disorder [15.3%], akathisia [10.5%], blood prolactin increase [8.8%], insomnia [5.4%]). A total of 8 deaths were reported, including 4 completed suicides.
Conclusion: Long-term treatment with PP1M was efficacious, and no new safety concerns were identified in Chinese patients with schizophrenia. Overall, the results were comparable with observations from previous studies.
Keywords: Chinese, long-acting injectables, open-label, paliperidone palmitate, PANSS, schizophrenia
Introduction
Sustained symptomatic remission and prevention of relapses are key components of the pharmacotherapy of schizophrenia that positively impact treatment outcomes.1–3 Medication nonadherence is regarded as the strongest determinant of psychotic relapses that in turn impose enormous occupational and social impediment and considerably increase the risk of suicidal behavior.4–7 In Chinese patients with schizophrenia, the medication nonadherence rate is estimated to range from 20% to 38%.8,9 Among several other factors, poor medication compliance was reported to be the most important predictor of psychotic relapses in these patients.9
Long-acting injectable (LAI) antipsychotics have the advantage of simplified treatment regimen, steady drug delivery, and freedom from daily dosing compared to their oral counterparts.10,11 LAIs also increase the feasibility of monitoring appointments for scheduled injections, enabling tracking of nonadherence.11 Several clinical studies and meta-analyses have attributed LAIs with optimum control of symptoms, prevention of relapses, and reductions in rehospitalizations, likely through achieving improved medication adherence.10,12–14 The atypical LAI, paliperidone palmitate 1-month formulation (PP1M), is approved for acute symptom control and maintenance treatment of schizophrenia in adults in most countries worldwide.15,16 Although LAIs are most likely used in cases of failure of oral antipsychotic treatment, exacerbations of symptoms, and frequent relapses, the unique pharmacokinetic profile of PP1M supports initiation of PP1M even in acute cases of early psychosis.11,15–17
A large body of clinical data from global studies has substantiated the efficacy and acceptable tolerability of PP1M for short-term treatment of schizophrenia.10,18–24 The efficacy of PP1M for acute treatment of schizophrenia in Chinese patients was demonstrated by 4 short-term (13-week) studies that reported PP1M to be well tolerated with similar safety findings as other populations.17,25–27
The benefits of long-term maintenance28–31 and recurrence prevention32 in global patient populations with schizophrenia have also been shown across a flexible dose range of 50–150 mg eq. Two recently published long-term studies demonstrated the favorable efficacy and safety of PP1M in patients from the Asia-Pacific region (Chinese patients: n=100 in each study).33,34 The 18-month study of PP1M in patients with recent-onset schizophrenia also showed significant reduction in the number and duration of hospitalizations.33 The second study was a global noninferiority study including patients from the People’s Republic of China that compared efficacy of PP1M to the newer paliperidone palmitate 3-month formulation.34 Both studies established the acceptable tolerability of PP1M for maintenance therapy of schizophrenia and did not raise any safety concern specific to the Asian population.
The present study was conducted in response to a request from the China Food and Drug Administration to collect clinical data for PP1M in 500 Chinese patients. Previous clinical studies from the Asia-Pacific region provided data for 200 Chinese patients.33,34 Therefore, the aim of the present study is to evaluate the safety and efficacy of PP1M in routine clinical use over a 6-month treatment period in an additional 300 Chinese patients with recent-onset or chronic schizophrenia. The study also intends to explore outcomes that are close to real world such as treatment adherence and caregiver burden following treatment with PP1M in these patients.
Methods
Study design
This 25-week, multicenter, non-randomized, open-label, prospective Phase IV study was conducted between October 2013 and March 2015, across 13 centers in the People’s Republic of China (ClinicalTrials.gov identifier: NCT01947803). The study was divided into a screening phase (up to 1 week), a treatment phase (25 weeks), and a follow-up phase (30 days). The study protocol and amendments were reviewed by an Independent Ethics Committee at each study site: The Second Xiangya Hospital of Central South University, Nanjing Brain Hospital, First Hospital of Shanxi Medical University, First Affiliated Hospital of Kunming Medical University, Tianjin Anding Hospital, Guangzhou Brain Hospital, Mental Health Center of Wuhan City, First Affiliated Hospital of Medical College of Xi’an Jiaotong University, The Sixth People’s Hospital of Hebei Province, The First Hospital of Hebei Medical University, Mental Health Center of Xi’an City, Beijing Huilongguan Hospital, West China Hospital, and The First Affiliated Hospital of College of Medicine – Zhejiang University. All studies were conducted in compliance with the Declaration of Helsinki consistent with Good Clinical Practices and applicable regulatory requirements. Written informed consent was obtained from all patients before enrollment.
Patients
Men and women aged 18–65 years (inclusive), diagnosed with schizophrenia (according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision [DSM-IV-TR]), having a Positive and Negative Syndrome Scale (PANSS) total score between 60 and 120 (inclusive), and currently receiving treatment with or without any antipsychotic were eligible. Enrolled patients included those who experienced recurrent episodes and those experiencing first psychotic episode.
Key exclusion criteria included active DSM-IV-TR diagnosis other than schizophrenia, history of substance dependence within 6 months before screening, suicide attempt within 12 months before screening or being at an imminent risk of suicidal or violent behavior, history of nonresponsiveness to risperidone or paliperidone, and prior treatment with clozapine for refractory schizophrenia.
Study treatments
Doses of PP1M given to the patients are expressed herein as mg eq. of paliperidone, the active fraction of PP1M.19 During the treatment phase, eligible patients received deltoid injections of paliperidone palmitate 150 mg eq. on day 1 and 100 mg eq. on day 8 followed by a monthly flexible dosing (75, 100, or 150 mg eq.), based on patient’s tolerability and/or efficacy, administered as either deltoid or gluteal injection. Patients without documented exposure to oral risperidone, paliperidone extended-release (ER), risperidone LAI, or PP1M were recommended for oral tolerability testing and received paliperidone ER (3–6 mg/day) or oral risperidone (1–3 mg/day) for 2–3 days during the screening phase.
Concomitant medications
Mood stabilizers or antidepressants (except nonselective or irreversible monoamine oxidase inhibitors, β-blockers, sedative hypnotics, and anticholinergic antiparkinsonian medications) were allowed. Benzodiazepines (≤10 consecutive days within 1 month) were permitted in cases of emergencies during the study. Use of lorazepam (≤6 mg/day orally) or any other equivalent short-acting benzodiazepine to control agitation, irritability, restlessness, and hostility was allowed. All antipsychotics other than PP1M were discontinued before initiation of study treatment on day 1. Any other psychoactive prescription medications, herbal agents, and over-the-counter drugs were not allowed during the treatment phase. Electroconvulsive therapy and transcranial magnetic stimulation were also prohibited during the course of this study.
Efficacy measures
The primary efficacy end point was changes in PANSS total score35 from baseline to days 8, 36, 92, and 176. The secondary efficacy analysis included changes in Clinical Global Impressions-Severity (CGI-S) scores36 and Personal and Social Performance (PSP) scores37 from baseline to days 8, 36, 92, and 176. Medication satisfaction was evaluated based on changes from baseline to days 64 and 176 in Medication Satisfaction Questionnaire (MSQ) score. The MSQ was a single-item questionnaire that was offered to patients or caregivers who rated the treatment between 1 (extremely dissatisfied) and 7 (extremely satisfied).38,39 Medication adherence was assessed using changes from baseline to days 64 and 176 in the 10-item questionnaire, Medication Adherence Rating Scale (MARS; total score <4 indicates nonadherence).40,41 The Attitude of Patient’s Preference for LAI (APL) measure was used to evaluate patient’s preference for LAI over oral antipsychotics and was calculated as the number and percentage of patients showing preference for either treatment and also investigated the reasons for preference. The Involvement Evaluation Questionnaire-31 (IEQ-31) was used to evaluate caregiver burden and was offered to all caregivers. Scoring was based on a 5-point Likert scale for 31 items on 4 dimensions (tension, supervision, worrying, and urging) and recorded during the previous 4 weeks as a recall period to assess caregiver consequences.42
Safety measures
Evaluations of safety and tolerability included incidence of treatment-emergent adverse events (TEAEs) and changes from baseline in extrapyramidal symptom (EPS) rating scales (Abnormal Involuntary Movement Scale [AIMS],43 Barnes Akathisia Rating Scale [BARS],44 and Simpson Angus Scale [SAS]),45 Columbia-Suicide Severity Rating Scale (C-SSRS; included after protocol amendment), clinical laboratory tests (including prolactin measurements), vital signs measurements, 12-lead electrocardiograms (ECGs), and physical examinations.
Statistical analysis
No formal sample size calculation was performed. Assuming a dropout rate of 15% based on experiences from 2 previous clinical studies of PP1M, 353 patients were expected to be enrolled in this study.33,34 This sample size provided ~95% chance of observing no less than 1% of incidence of TEAEs.
All efficacy analyses were performed on the full analysis set that included patients who received at least 1 injection of PP1M during the treatment phase and had at least 1 postbaseline efficacy assessment. The safety set that included patients who received at least 1 injection of PP1M during study duration was used for safety evaluations. IEQ-31 evaluation was performed on the pharmacoeconomic analysis set comprising caregivers for patients who received at least 1 injection of PP1M during the treatment phase and had at least 1 postbaseline evaluation. All efficacy end points were compared using paired t-test or Wilcoxon signed-rank test, at a 2-sided significance level of 5%, and no adjustments were made for multiplicity. Subgroup analyses based on disease duration (recent-onset schizophrenia: ≤5 years and chronic schizophrenia: >5 years of psychiatric history) were performed using analysis of covariance, and the values at baseline were used as covariates. The cut-off year for the subgroups was fixed at 5 years based on evidence suggestive of functional deterioration and decline in antipsychotic treatment responses within the 5 years of first psychiatric diagnosis.46–48 For all efficacy end points, the values and changes from baseline were summarized descriptively, and last observation carried forward data were used for missing data imputation. All safety measurements were summarized descriptively.
Results
Patient disposition and characteristics
A total of 403 patients were screened for eligibility of which 353 with mean (standard deviation, SD) age of 31.1 (10.52) years entered the treatment phase. The majority (68.6%, n=242) of patients had recent-onset schizophrenia (Table 1). The demographic characteristics were consistent across the 2 subgroups except mean (SD) body weight (64.0 [12.28] vs 66.3 [12.29] kg), body mass index (23.1 [3.80] vs 24.4 [3.95] kg/m2), and age (28.3 [9.40] vs 37.2 [10.32] years) that were numerically lower in patients with psychiatric history of ≤5 years than those with history of >5 years. The baseline clinical characteristics were similar between the 2 subgroups. The commonly prescribed prior antipsychotic and concomitant medications included trihexyphenidyl hydrochloride (24.4%), risperidone (11.3%), paliperidone (8.2%), lorazepam (7.4%), and alprazolam (5.9%).
Of the 353 enrolled patients, 234 (66.3%) completed the treatment at day 176. The most common reasons for study discontinuation were withdrawal of consent (36 [10.2%]), TEAEs (30 [8.5%]), and lack of efficacy (15 [4.2%]) (Figure 1). All patients were included in the safety set (100%), whereas the full analysis set had 345 (97.7%) patients and the pharmacoeconomic analysis set had 301 (85.3%) patients. Of the 234 patients who completed the 25-week study, 230 completed the follow-up period at day 206. The mean (SD) dose of PP1M (excluding the dose on day 1 and day 8) in the entire patient population was 118.7 (24.60) mg eq. (recent-onset subgroup, 117.3 [24.43]; chronic schizophrenia subgroup, 121.8 [24.82]) during the study.
  | Figure 1 Patient disposition. |
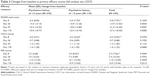
Primary efficacy
A significant (P<0.0001) improvement in mean (SD) PANSS total score was observed from baseline to day 8 (−5.8 [7.97]), day 36 (−13.9 [13.02]), day 92 (−21.5 [16.46]), and day 176 (end of the 6-month treatment period; −27.2 [18.30]) (Table 2). The subgroup analyses revealed that the magnitude of reductions in PANSS total scores was greater in patients with psychiatric history of ≤5 years as compared with those with a history of >5 years at all time points measured (Table 2).
Secondary efficacy
Significant (P<0.0001) changes in mean (SD) CGI-S scores from baseline on day 8 (−0.2 [0.55]), day 36 (−0.7 [0.88]), day 92 (−1.2 [1.06]), and day 176 (−1.6 [1.22]) were observed (Table 2). Mean (SD) changes in PSP scores also showed significant improvement on day 8 (3.3 [7.26]), day 36 (7.4 [10.24]), day 92 (11.0 [13.09]), and day 176 (14.9 [15.04]) (P<0.0001). Clinically meaningful and significant changes in mean (SD) MSQ scores on day 64 (0.6 [1.51], P<0.0001) and day 176 (0.8 [1.62], P<0.0001) represented treatment satisfaction among patients. Subgroup analysis did not indicate any significant differences in the extent of improvement for CGI-S, PSP, and MSQ scores between patients with a psychiatric history of ≤5 and >5 years.
Improved medication adherence was observed as indicated by significant mean (SD) changes from baseline in MARS scores on day 64 (1.7 [3.06], P<0.0001) and day 176 (2.2 [3.28], P<0.0001). Overall, the treatment adherence rate for all medications increased from 46.9% at baseline to 75.0% on day 64 and 82.3% on day 176 (Table 3). Based on the APL, the percentage of patients preferring LAI over oral antipsychotics was greater consistently throughout the study: 70.4% (baseline), 79.2% (day 64), and 76.9% (day 176) (Table 3). Among patients preferring LAIs, >70% favored deltoid injections over gluteal injections at all investigated study points. The reasons for this preference were simpler procedure and less embarrassment than receiving gluteal injections. A smaller proportion of patients preferred gluteal injections and claimed that these were less painful and simpler than deltoid injections. Simplified regimen, freedom from taking oral antipsychotics, and better symptom remission were among the top reasons for the higher preference toward LAIs. Significant (P<0.0001) mean (SD) reduction from baseline (31.8 [15.52]) in IEQ-31 scores was observed on day 64 (−6.7 [14.30]) and day 176 (−8.2 [15.84]), indicating meaningful relief in caregiver burden. Lowering of caregiver burden was significant (P<0.0001) for both subgroups on day 176 (psychiatric history of ≤5 years, −8.6 [16.98]; psychiatric history of >5 years, −7.2 [13.01]).
Safety
Overall, 181 (51.3%) patients experienced TEAEs during the study. The most frequently reported TEAEs (in ≥5% patients) were extrapyramidal disorder (54 [15.3%]), akathisia (37 [10.5%]), blood prolactin increase (31 [8.8%]), and insomnia (19 [5.4%]) (Table 4). The majority of TEAEs were rated as mild or moderate. There were 24 (6.8%) serious TEAEs; exacerbation of psychotic symptoms (11 [3.1%]) was the most common serious TEAE. In total, 31 (8.8%) patients prematurely discontinued the study due to TEAEs; worsening of schizophrenia (10 [2.8%]) was the most frequent TEAE responsible for discontinuation. In all, 96 (27.2%) patients experienced EPS-related TEAEs. Extrapyramidal disorder (54 [15.3%]), akathisia (37 [10.5%]), restlessness (3 [0.8%]), musculoskeletal stiffness (3 [0.8%]), Parkinsonism (2 [0.6%]), and tremor (2 [0.6%]) were the common (n≥2) EPS events. Changes in EPS-rating scales (AIMS/BARS/SAS) indicated that >90% of patients had normal movements (severity of abnormal movement = none) throughout the study (based on AIMS assessment of severity of dyskinesia) and that the majority (≥75%) of patients had no akathisia, and none reported severe akathisia throughout the study (BARS scores). No trend suggestive of Parkinsonism was identified throughout the study as indicated by the median SAS total score (0.00) at the end of treatment phase. Prolactin-related TEAEs were experienced by 41 (11.6%) patients, and the more common (n≥3) events included increased blood prolactin levels (31 [8.8%]), amenorrhea, menstrual disorder, and galactorrhea (3 [0.8%] each). Glucose-related TEAEs (blood glucose increase) were reported in 2 (0.6%) patients. Clinically relevant weight gain (>7% increase in body weight) was reported in 28.6% of patients at the end of the follow-up period (day 206). Post-baseline changes in hematological parameters, vital signs, or ECGs were not clinically meaningful.
Deaths were reported in 8 (2.3%) patients (completed suicide, n=4; deaths, n=2; unexplained deaths, n=2). One of the 2 deaths was reported as a “sudden cardiac death” since the autopsy results did not find any other cause for the death, such as trauma or poisoning. However, the consideration of the death as a “sudden cardiac death” was speculative as the death was not witnessed and no ECG monitoring was performed. The reason for the second death (found dead in river) was not reported; however, the possibility of a suicide could not be ruled out. Patients who died were in the age group of 22–45 years (completed suicides, 22–45 years; other deaths, 30–43 years); mostly women (completed suicides: men =2, women =2; other deaths: men =1, women =3) and 6 of the 8 patients had a psychiatric history of >5 years (completed suicides and other deaths, n=3 each). As compared with patients who survived (n=345), the patients who died had a longer duration of schizophrenia (mean [SD] duration, 4.6 [5.79] vs 7.5 [4.92] years). The mean (SD) MARS total score at baseline was 4.6 (2.26) in patients who died (n=8) and 4.3 (2.89) in patients who survived (n=341). Among the suicidal events, 2 of 3 suicide attempters and 2 of 4 suicide completers were women, and all 7 events occurred in younger patients (19–45 years). Two of the 4 suicide completers had documented prior nonfatal suicide attempt, and recent hospital admissions were reported in 3 of the 4 fatal suicide cases.
A protocol amendment was initiated to collect additional safety data, to include suicide risk evaluation (C-SSRS) and additional 12-lead ECG examination at all weekly visits (in addition to baseline and day 176 assessments, up to day 206 of the follow-up). After the amendment, evaluation of suicide risk based on C-SSRS scores was conducted in 28 of 353 patients. There were no reported suicidal attempts or completed suicides after amendment. No clinically notable cardiovascular abnormalities were observed based on additional ECG assessments.
Discussion
The present study evaluated the long-term safety and efficacy of PP1M in a large population of Chinese patients (n=353) with schizophrenia. In contrast to randomized controlled trials, the patient sample included in this study was representative of patients treated in everyday clinical practice, thus improving the external validity of these results. In addition, this study was designed to simulate real-world clinical situations in which patients are treated with flexible dosing of PP1M and evaluate pragmatic outcomes that potentially predict treatment responses. To our knowledge, such findings have not been reported earlier in a Chinese population with schizophrenia.
The efficacy findings from this study demonstrated that monthly flexible dosing (75, 100, or 150 mg eq.) of PP1M over a period of 25 weeks achieved favorable and significant (P=0.0001) reductions from baseline in the PANSS total scores (primary efficacy measure) for both total population and subgroups (patients with psychiatric history of ≤5 years and >5 years). Significant improvements in secondary efficacy end points, CGI-S and PSP scores, indicated progressive treatment response and improvements in psychosocial functioning in these patients.
Overall, PP1M showed greater symptom improvement in patients with recent-onset schizophrenia (psychiatric history of ≤5 years). This finding adds to available evidence that values the use of PP1M treatment in early schizophrenia, challenging the practice of reserving LAIs for chronic cases and treatment failures.17,48,49 The efficacy findings from this study are consistent with the outcomes from earlier global studies of PP1M and studies in Asian patients with schizophrenia.21,22,25,27,31,33
The safety findings from this study also corroborated the outcomes reported in other studies of PP1M in patients from the Asia-Pacific region.17,25–27 The rates of TEAEs (51.3%) reported herein were consistent with the results of 2 long-term studies of PP1M in patients from the Asia-Pacific region (66.0% and 82.3%)33,34 and global studies of PP1M,30,31,50,51 and were comparable with the TEAE rates generally observed with oral atypical antipsychotic treatment (64%–70%).52 Worsening of schizophrenia (2.8%) was the most common TEAE that led to treatment discontinuation.
The clinical benefits of PP1M with regard to treatment satisfaction (MSQ scores), adherence to antipsychotic medications (MARS), and preference for LAI treatments over oral equivalents (APL) were also demonstrated by this study. These efficacy measures are indicators of antipsychotic treatment success in the real world that impact long-term management of schizophrenia, ultimately achieving prevention of relapses and reductions in hospitalizations.4,11,53 Several studies have regarded positive patient attitude as a key outcome driver and a reliable predictor of treatment acceptance that favorably impacts long-term medication adherence and clinical responses.54–59 Improved patient satisfaction and positive attitude toward LAIs have been considered as important attributes that influence treatment choice among physicians.54,56 In the present study, a higher number of patients preferred LAIs throughout the course of the 6-month treatment with PP1M. These results, along with data from a systematic review that observed a greater preference for LAIs among patients previously treated with LAIs versus LAI-naïve patients, represent a progressive trend and changing attitude towards LAIs among patients, as well as prescribing physicians.55,59 The higher patient preference for deltoid over gluteal injections noted in this study is consistent with results from other reports, although gluteal injections have been associated with better tolerability.50,54 Thus, the flexibility of PP1M administration as both deltoid and gluteal injections offers an additional advantage. These results add to the current knowledge about patient and physician experiences that favor the use of LAI antipsychotics in routine clinical practice at different stages of schizophrenia.54,60,61
A significant reduction in the magnitude of caregiver burden following the 6-month treatment with PP1M was also observed. Alleviations in caregiver burden reflect meaningful changes in various aspects of life such as social functioning, personal relationships, daily routine activities, leisure, and physical and mental health, all suggestive of improving the quality of life. In most cases, family members are the caregivers, and reducing the burden positively influences their role in offering intensive patient support and care and ensuring treatment adherence.62,63
A total of 8 deaths were reported in the present study, and half of those deaths were reportedly due to suicide. A greater risk of suicidality has been observed in patients with psychiatric illness as compared with the general population, with the estimates for lifetime risk of suicide attempt ranging from 1% to 4.7% in the non-afflicted population, escalating to 5%–22% in patients with schizophrenia.64–67 The prevalence of schizophrenia in the People’s Republic of China is generally similar to that of Western and other Asian populations; however, there are some different demographic and sociocultural risk factors for suicide in China. For example, in rural China, women are considered to be at greater risk than men for suicide.68–71
Some common predictors of suicides associated with schizophrenia include prior suicide attempt, comorbid depression or higher depressive symptoms, early onset of illness, frequent psychiatric hospitalizations, and unemployment.65,72–76 In the present study, most patients who completed suicide were documented as having multiple known risk factors for suicide, including younger age at onset of illness and a history of prior suicide attempts, which is a strong clinical correlate of an eventual successful suicide attempt.75,77
Overall, the crude incidence rate for completed suicide noted in this study (28.42 per 1,000 patient-years; 95% confidence interval [CI]: 7.74–72.76) was substantially higher than the pooled incidence data for PP1M from the 4 studies (NCT01685931, NCT01051531, NCT01515423, and current study) conducted in the People’s Republic of China (7.06 per 1,000 patient-years; 95% CI: 2.29–16.47; Table 5) (unpublished data on file). Treatment with atypical antipsychotics has been favorably associated with reduction in suicidal intentions and a potential for protection against suicide via attenuation of symptom severity.73,78 Further, based on cumulative experience from controlled Phase III studies of PP1M in Chinese patients with schizophrenia, the rates for completed suicide in the PP1M active treatment arms have been observed to be lower in comparison with placebo and risperidone LAI treatment arms. From case-level analysis, patients who completed suicides during the present study had a range of documented suicide-related risk factors. Thus, it is likely that the suicide rate in this study was related to patient selection.
The remaining 4 of the 8 deaths that occurred in the study were of unclear etiology. Two were classified as “unexplained”, and 1 was classified as being “of cardiac origin” but this result was speculative since the autopsy failed to yield any other clear cause. Unfortunately, none of the 4 deaths were witnessed; all 4 patients were found dead (1 each in a “rental room”, “by a river”, “in bed”, and “at home”). According to a previous study, mortality rates in schizophrenia were significantly greater than in the general population.79 Cardiovascular disorders were the most common causes of sudden death in schizophrenia patients admitted to a psychiatric hospital, and sudden cardiac death occurred at a 0.8% rate in a psychiatric hospital, which is well above general population rates.80 In the present study, 2 of 4 deaths of unclear etiology reported abnormal ECG at baseline suggestive of a possible cardiovascular involvement. Recent population-based studies from the People’s Republic of China have presented age-stratified mortality rates among patients with schizophrenia81 and noted higher mortality rates in younger patients that diminished greatly with increased age (standard mortality ratio, 18–29 years: 120.89; 70+ years: 4.95).81,82 Similar to observations among patients who had fatal suicides in this study, the patients who died (all-cause) were young and had prolonged history of schizophrenia (≥5 years) as compared with patients who survived.
The crude incidence rates for deaths (all-cause) observed in this study were also considerably higher than the pooled data from 4 Chinese studies (including the current study) of PP1M (16.94 per 1,000 patient-years; 95% CI: 8.75–29.59; Table 5) and global studies (7.1 per 1,000 patient-years);83 the pooled death rates from 3 studies excluding the present study range from 5.86 to 8.24 per 1,000 person-years (unpublished data on file). The all-cause mortality rates in the present study were also higher than that reported in a large observational (ZODIAC) study (13 per 1,000 patient-years) for other antipsychotics (ziprasidone and olanzapine).84
Based on the limited data from the 8 deaths reported during this study, the high crude incidence rate of completed suicides and deaths does not appear to indicate a definite association with PP1M treatment. The high suicide and all-cause mortality rates may be attributable to an interplay of preexisting pertinent risk factors,72,81,82 limitations in analysis, and other study-related variables such as small sample size, low number of observed cases (completed suicides and suicide attempts), and wide CIs that limit the assessment of the validity of these findings. Furthermore, there is insufficient information to ascertain if there was a systematic bias involved in selection of high-risk patients. Thus, the findings from the current study do not represent a new identified risk for PP1M, and the benefit–risk assessment of PP1M remains positive and unchanged for the approved indications.
The higher occurrence of EPS-related events (27.2%) during this study was similar to that reported in earlier studies of PP1M in Chinese patients with schizophrenia.25,26 Extrapyramidal disorder (15.3%) showed the highest incidence among the EPS-related events, although the EPS-rating scale (SAS; median score: 0.0) did not indicate any trend of Parkinsonism. Further, the higher incidences of EPS events did not appear to deter medication adherence or the patient’s preferences for LAI in this study. The rates of other clinically significant TEAEs, including prolactin-related TEAEs and glucose-related TEAEs, were also generally comparable with previous studies of PP1M.25,27,31,33,48
The open-label design and absence of a comparator in the current study may have introduced an observational bias on the physicians, and the knowledge of treatment allocation may have resulted in reporting bias for subjective outcomes such as patient-reported end points.
To summarize, treatment with PP1M showed symptom improvement, and no new safety concerns were identified over a 6-month treatment period in a real-world setting. These results were comparable with available evidence, validating the long-term benefits of PP1M in Chinese patients with schizophrenia.
Acknowledgments
The authors thank Priya Ganpathy, ISMPP CMPP™ (SIRO Clinpharm Pvt. Ltd., India), for writing assistance and Dr Ellen Baum (Janssen Research & Development, LLC) for additional editorial assistance in the preparation of this manuscript. The authors also thank the study participants, without whom this study would not have been accomplished, and the following investigators for their contributions to this study: Drs Xueyi Wang, Fude Yang, Kerang Zhang, Jie Li, Wei Deng, Yi Xu, Chengge Gao, and Jianxiong Fan. This study was funded by Xi’an Janssen Pharmaceutical Ltd., People’s Republic of China. The sponsor also provided a formal review of the manuscript.
Author contributions
Drs Lili Zhang, Shangli Cai, Yu Feng, Weihong Liu, and Huafei Lu were responsible for the design, conduct, and data analysis of the study. Drs Jingping Zhao, Lehua Li, Jianguo Shi, Yi Li, Xiufeng Xu, and Keqing Li were the principal investigators of the study, contributed data, and participated in the development of the manuscript. Jianmin Zhuo was responsible for the statistical analyses and design/interpretation of study results. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors meet ICMJE criteria, and all those who fulfilled those criteria are listed as authors.
Disclosure
Drs Jingping Zhao, Lehua Li, Jianguo Shi, Yi Li, Xiufeng Xu, and Keqing Li were the principal investigators of this study and have received research support or fees as consultants from Xi’an Janssen Pharmaceutical Ltd., People’s Republic of China. Drs Lili Zhang, Yu Feng, Jianmin Zhuo, Weihong Liu, and Huafei Lu are employees of Xi’an Janssen Pharmaceutical Ltd., People’s Republic of China, which is a Johnson & Johnson company. Dr Shangli Cai was an employee of Xi’an Janssen Pharmaceutical Ltd., People’s Republic of China, at the time of study. The authors report no other conflicts of interest in this work.
References
Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. 2013;13:50. | ||
Karson C, Duffy RA, Eramo A, Nylander AG, Offord SJ. Long-term outcomes of antipsychotic treatment in patients with first-episode schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:57–67. | ||
De Hert M, Sermon J, Geerts P, Vansteelandt K, Peuskens J, Detraux J. The use of continuous treatment versus placebo or intermittent treatment strategies in stabilized patients with schizophrenia: a systematic review and meta-analysis of randomized controlled trials with first- and second-generation antipsychotics. CNS Drugs. 2015;29(8): 637–658. | ||
Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. | ||
Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67(3):453–460. | ||
Sendt KV, Tracy DK, Bhattacharyya S. A systematic review of factors influencing adherence to antipsychotic medication in schizophrenia-spectrum disorders. Psychiatry Res. 2015;225(1–2):14–30. | ||
Schennach R, Obermeier M, Meyer S, et al. Predictors of relapse in the year after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2012;63(1):87–90. | ||
Wang X, Zhang W, Ma N, et al. Adherence to antipsychotic medication by community-based patients with schizophrenia in China: a cross-sectional study. Psychiatr Serv. 2016;67(4):431–437. | ||
Xiao J, Mi W, Li L, Shi Y, Zhang H. High relapse rate and poor medication adherence in the Chinese population with schizophrenia: results from an observational survey in the People’s Republic of China. Neuropsychiatr Dis Treat. 2015;11:1161–1167. | ||
Alphs L, Bossie CA, Sliwa JK, Fu DJ, Ma YW, Hulihan J. Paliperidone palmitate and risperidone long-acting injectable in subjects with schizophrenia recently treated with oral risperidone or other oral antipsychotics. Neuropsychiatr Dis Treat. 2013;9:341–350. | ||
Agid O, Foussias G, Remington G. Long-acting injectable antipsychotics in the treatment of schizophrenia: their role in relapse prevention. Expert Opin Pharmacother. 2010;11(14):2301–2317. | ||
Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168(6):603–609. | ||
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S. Oral versus depot antipsychotic drugs for schizophrenia – a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res. 2011;127(1–3):83–92. | ||
Schreiner A, Aadamsoo K, Altamura C, et al. A randomized, active-controlled rater-blinded 2-year study of paliperidone palmitate versus investigators’ choice of oral antipsychotic monotherapy in patients with schizophrenia (prosipal). Eur Psychiatry. 2014;29 Suppl 1:1. | ||
Citrome L. Paliperidone palmitate – review of the efficacy, safety and cost of a new second-generation depot antipsychotic medication. Int J Clin Pract. 2010;64(2):216–239. | ||
Newton R, Hustig H, Lakshmana R, et al. Practical guidelines on the use of paliperidone palmitate in schizophrenia. Curr Med Res Opin. 2012;28(4):559–567. | ||
Li H, Turkoz I, Zhang F. Efficacy and safety of once-monthly injection of paliperidone palmitate in hospitalized Asian patients with acute exacerbated schizophrenia: an open-label, prospective, noncomparative study. Neuropsychiatr Dis Treat. 2015;12:15–24. | ||
Alphs L, Bossie CA, Sliwa JK, Ma YW, Turner N. Onset of efficacy with acute long-acting injectable paliperidone palmitate treatment in markedly to severely ill patients with schizophrenia: post hoc analysis of a randomized, double-blind clinical trial. Ann Gen Psychiatry. 2011;10(1):12. | ||
Bossie CA, Fu DJ, Sliwa JK, Ma YW, Alphs L. Tolerability of initiation doses of once-monthly paliperidone palmitate in patients with recently diagnosed schizophrenia in an acute treatment trial. Ther Adv Psychopharmacol. 2011;1(4):111–124. | ||
Fu DJ, Bossie CA, Sliwa JK, Ma YW, Alphs L. Paliperidone palmitate versus oral risperidone and risperidone long-acting injection in patients with recently diagnosed schizophrenia: a tolerability and efficacy comparison. Int Clin Psychopharmacol. 2014;29(1):45–55. | ||
Kramer M, Litman R, Hough D, et al. Paliperidone palmitate, a potential long-acting treatment for patients with schizophrenia. Results of a randomized, double-blind, placebo-controlled efficacy and safety study. Int J Neuropsychopharmacol. 2010;13(5):635–647. | ||
Pandina G, Lane R, Gopal S, et al. A double-blind study of paliperidone palmitate and risperidone long-acting injectable in adults with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(1):218–226. | ||
Pandina GJ, Lindenmayer JP, Lull J, et al. A randomized, placebo-controlled study to assess the efficacy and safety of 3 doses of paliperidone palmitate in adults with acutely exacerbated schizophrenia. J Clin Psychopharmacol. 2010;30(3):235–244. | ||
Gopal S, Hough DW, Xu H, et al. Efficacy and safety of paliperidone palmitate in adult patients with acutely symptomatic schizophrenia: a randomized, double-blind, placebo-controlled, dose-response study. Int Clin Psychopharmacol. 2010;25(5):247–256. | ||
Li H, Rui Q, Ning X, Xu H, Gu N. A comparative study of paliperidone palmitate and risperidone long-acting injectable therapy in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(4):1002–1008. | ||
Si T, Zhang K, Tang J, et al. Efficacy and safety of flexibly dosed paliperidone palmitate in Chinese patients with acute schizophrenia: an open-label, single-arm, prospective, interventional study. Neuropsychiatr Dis Treat. 2015;11:1483–1492. | ||
Takahashi N, Takahashi M, Saito T, et al. Randomized, placebo-controlled, double-blind study assessing the efficacy and safety of paliperidone palmitate in Asian patients with schizophrenia. Neuropsychiatr Dis Treat. 2013;8:1889–1898. | ||
Sliwa JK, Bossie CA, Fu DJ, Turkoz I, Alphs L. Long-term tolerability of once-monthly injectable paliperidone palmitate in subjects with recently diagnosed schizophrenia. Neuropsychiatr Dis Treat. 2012;8:375–385. | ||
Attard A, Olofinjana O, Cornelius V, Curtis V, Taylor D. Paliperidone palmitate long-acting injection – prospective year-long follow-up of use in clinical practice. Acta Psychiatr Scand. 2014;130(1):46–51. | ||
Coppola D, Liu Y, Gopal S, et al. A one-year prospective study of the safety, tolerability and pharmacokinetics of the highest available dose of paliperidone palmitate in patients with schizophrenia. BMC Psychiatry. 2012;12:26. | ||
Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M, Hough D. A 52-week open-label study of the safety and tolerability of paliperidone palmitate in patients with schizophrenia. J Psychopharmacol. 2011;25(5):685–697. | ||
Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116(2–3):107–117. | ||
Zhang F, Si T, Chiou CF, et al. Efficacy, safety, and impact on hospitalizations of paliperidone palmitate in recent-onset schizophrenia. Neuropsychiatr Dis Treat. 2015;11:657–668. | ||
Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, noninferiority study. Int J Neuropsychopharmacol. 2016;19(7). | ||
Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997;58(12):538–546. | ||
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4(7):28–37. | ||
Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101(4):323–329. | ||
Gharabawi GM, Greenspan A, Rupnow MF, et al. Reduction in psychotic symptoms as a predictor of patient satisfaction with antipsychotic medication in schizophrenia: data from a randomized double-blind trial. BMC Psychiatry. 2006;6:45. | ||
Vernon MK, Revicki DA, Awad AG, et al. Psychometric evaluation of the Medication Satisfaction Questionnaire (MSQ) to assess satisfaction with antipsychotic medication among schizophrenia patients. Schizophr Res. 2010;118(1–3):271–278. | ||
Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–247. | ||
Fialko L, Garety PA, Kuipers E, et al. A large-scale validation study of the Medication Adherence Rating Scale (MARS). Schizophr Res. 2008;100(1–3):53–59. | ||
van Wijngaarden B, Schene A, Koeter M, et al. People with schizophrenia in five countries: conceptual similarities and intercultural differences in family caregiving. Schizophr Bull. 2003;29(3):573–586. | ||
Guy W; Early Clinical Drug Evaluation Unit (ECDEU). Assessment Manual for Psychopharmacology. Rockville, MD: National Institute of Mental Health; 1976. | ||
Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–676. | ||
Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19. | ||
Lieberman J, Jody D, Geisler S, et al. Time course and biologic correlates of treatment response in first-episode schizophrenia. Arch Gen Psychiatry. 1993;50(5):369–376. | ||
McGlashan TH, Johannessen JO. Early detection and intervention with schizophrenia: rationale. Schizophr Bull. 1996;22(2):201–222. | ||
Alphs L, Bossie C, Mao L, Lee E, Starr HL. Treatment effect with paliperidone palmitate compared with oral antipsychotics in patients with recent-onset versus more chronic schizophrenia and a history of criminal justice system involvement. Early Interv Psychiatry. Epub 2015 Sep 25. | ||
Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. A randomized clinical trial. JAMA Psychiatry. 2015;72(8):822–829. | ||
Hough D, Lindenmayer JP, Gopal S, et al. Safety and tolerability of deltoid and gluteal injections of paliperidone palmitate in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(6):1022–1031. | ||
Hargarter L, Cherubin P, Bergmans P, et al. Intramuscular long-acting paliperidone palmitate in acute patients with schizophrenia unsuccessfully treated with oral antipsychotics. Prog Neuropsychopharmacol Biol Psychiatry. 2015;58:1–7. | ||
Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. | ||
Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754–768. | ||
Geerts P, Martinez G, Schreiner A. Attitudes towards the administration of long-acting antipsychotics: a survey of physicians and nurses. BMC Psychiatry. 2013;13:58. | ||
Waddell L, Taylor M. Attitudes of patients and mental health staff to antipsychotic long-acting injections: systematic review. Br J Psychiatry Suppl. 2009;52:S43–S50. | ||
Heres S, Reichhart T, Hamann J, Mendel R, Leucht S, Kissling W. Psychiatrists’ attitude to antipsychotic depot treatment in patients with first-episode schizophrenia. Eur Psychiatry. 2011;26(5):297–301. | ||
Patel MX, Haddad PM, Chaudhry IB, McLoughlin S, Husain N, David AS. Psychiatrists’ use, knowledge and attitudes to first- and second-generation antipsychotic long-acting injections: comparisons over 5 years. J Psychopharmacol. 2010;24(10):1473–1482. | ||
Kwon JS, Kim SN, Han J, et al. Satisfaction of immediate or delayed switch to paliperidone palmitate in patients unsatisfied with current oral atypical antipsychotics. Int Clin Psychopharmacol. 2015;30(6):320–328. | ||
Kaplan G, Casoy J, Zummo J. Impact of long-acting injectable antipsychotics on medication adherence and clinical, functional, and economic outcomes of schizophrenia. Patient Prefer Adherence. 2013;7:1171–1180. | ||
Stevens GL, Dawson G, Zummo J. Clinical benefits and impact of early use of long-acting injectable antipsychotics for schizophrenia. Early Interv Psychiatry. 2016;10(5):365–377. | ||
González-Rodríguez A, Catálan R, Penadés R, et al. Profile of paliperidone palmitate once-monthly long-acting injectable in the management of schizophrenia: long-term safety, efficacy, and patient acceptability – a review. Patient Prefer Adherence. 2015;9:695–706. | ||
Caqueo-Urízar A, Rus-Calafell M, Urzúa A, Escudero J, Gutiérrez-Maldonado J. The role of family therapy in the management of schizophrenia: challenges and solutions. Neuropsychiatr Dis Treat. 2015;11:145–151. | ||
Shuler KM. Approaches to improve adherence to pharmacotherapy in patients with schizophrenia. Patient Prefer Adherence. 2014;8:701–714. | ||
Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005;62(3):247–253. | ||
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(4 Suppl):81–90. | ||
Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. | ||
Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. | ||
Vijayakumar L. Suicide and mental disorders in Asia. Int Rev Psychiatry. 2005;17(2):109–114. | ||
Phillips MR, Yang G, Li S, Li Y. Suicide and the unique prevalence pattern of schizophrenia in mainland China: a retrospective observational study. Lancet. 2004;364(9439):1062–1068. | ||
Xiang YT, Weng YZ, Leung CM, Tang WK, Ungvari GS. Socio-demographic and clinical correlates of lifetime suicide attempts and their impact on quality of life in Chinese schizophrenia patients. J Psychiatr Res. 2008;42(6):495–502. | ||
Lyu J, Zhang J. Characteristics of schizophrenia suicides compared with suicides by other diagnosed psychiatric disorders and those without a psychiatric disorder. Schizophr Res. 2014;155(1–3):59–65. | ||
Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet. 2002;360(9347):1728–1736. | ||
Lui SY. Risk factors for deliberate self-harm and completed suicide in young Chinese people with schizophrenia. Aust N Z J Psychiatry. 2009;43(3):252–259. | ||
Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15(2):127–135. | ||
Zhang XY, Al Jurdi RK, Zoghbi AW, et al. Prevalence, demographic and clinical correlates of suicide attempts in Chinese medicated chronic inpatients with schizophrenia. J Psychiatr Res. 2013;47(10):1370–1375. | ||
Montross LP, Kasckow J, Golshan S, Solorzano E, Lehman D, Zisook S. Suicidal ideation and suicide attempts among middle-aged and older patients with schizophrenia spectrum disorders and concurrent subsyndromal depression. J Nerv Ment Dis. 2008;196(12):884–890. | ||
Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, Lönnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161(3):562–563. | ||
Meltzer HY, Alphs L, Green AI, et al; International Suicide Prevention Trial Study Group. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry. 2003;60(1):82–91. | ||
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–1131. | ||
Ifteni P, Correll CU, Burtea V, Kane JM, Manu P. Sudden unexpected death in schizophrenia: autopsy findings in psychiatric inpatients. Schizophr Res. 2014;155(1–3):72–76. | ||
Liu T, Song X, Chen G, Paradis AD, Zheng X. Prevalence of schizophrenia disability and associated mortality among Chinese men and women. Psychiatry Res. 2014;220(1–2):181–187. | ||
Ran MS, Mao WJ, Chan CL, Chen EY, Conwell Y. Gender differences in outcomes in people with schizophrenia in rural China: 14-year follow-up study. Br J Psychiatry. 2015;206(4):283–288. | ||
Pierce P, Gopal S, Savitz A, et al. Paliperidone palmitate: Japanese postmarketing mortality results in patients with schizophrenia. Curr Med Res Opin. 2016:1–9. | ||
Strom BL, Eng SM, Faich G, et al. Comparative mortality associated with ziprasidone and olanzapine in real-world use among 18,154 patients with schizophrenia: the Ziprasidone Observational Study of Cardiac Outcomes (ZODIAC). Am J Psychiatry. 2011;168(2):193–201. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.