Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Safety and Efficacy of Cryoballoon Pulmonary Vein Isolation and Left Atrial Appendage Closure Combined Procedure and Half-Dose Rivaroxaban After Operation in Elderly Patients with Atrial Fibrillation
Authors Zhang X, Xing Z, Fang C, Yang M, Luo J , Ning Z
Received 7 June 2023
Accepted for publication 8 August 2023
Published 5 September 2023 Volume 2023:16 Pages 2603—2611
DOI https://doi.org/10.2147/JMDH.S424843
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xiaogang Zhang,* Zhongying Xing,* Chao Fang, Meiling Yang, Jun Luo, Zhongping Ning
Department of Cardiology, Shanghai Pudong New Area Zhoupu Hospital (Shanghai Health Medical College Affiliated Zhoupu Hospital), Shanghai, 201318, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhongping Ning, Department of Cardiology, Shanghai Pudong New Area Zhoupu Hospital (Shanghai Health Medical College Affiliated Zhoupu Hospital), No. 1500 Zhouyuan Road, Pudong New District, Shanghai, 201318, People’s Republic of China, Tel +86-021-68135590, Email [email protected]
Background: To investigate the safety and effectiveness of cryo-balloon pulmonary vein isolation (PVI) and left atrial appendage closure (LAAC) combined procedure and half-dose rivaroxaban after operation in elderly patients with atrial fibrillation (AF).
Patients and Methods: A total of 203 AF patients presented for cryo-balloon PVI, and LAAC combined procedure was included from 2019 to 2021. Postoperative patients were anticoagulated with rivaroxaban with/without clopidogrel for 60 days, with oral rivaroxaban of 10 mg in the elderly group and 20 mg in the non-elderly group. Patients with AF ≥ 80 and < 80 years were considered elderly and non-elderly groups, respectively. Scheduled follow-ups and transesophageal echocardiography were used to assess peri- and post-procedural safety and effectiveness.
Results: A total of 203 patients underwent the combined procedure, 83 in the elderly and 120 in the non-elderly groups. All patients successfully obtained PVI and satisfactory LAAC. During the perioperative period, one patient had puncture complications in the elderly group and one with thrombosis in the non-elderly group. Oral rivaroxaban was administered to 83.2% and 75% of patients in the elderly and non-elderly groups, respectively, and rivaroxaban was combined with clopidogrel anticoagulation in the remaining patients. The annual rates of composite clinical events were 8.4% and 9.2% in the elderly and non-elderly groups, respectively, with no statistically significant difference. Patients in both groups had complete sealing, and there was no displacement of devices, death and peripheral arterial thrombosis. Recurrence of AF occurred in 25 and 32 patients in the elderly and non-elderly groups, respectively, with no statistically significant difference. Besides, the two groups had no statistically significant difference in cerebral infarction/transient ischemic attack and device-related thrombosis (p > 0.05).
Conclusion: This study suggests that cryo-balloon PVI and LAAC combined procedure and half-dose rivaroxaban after the operation is safe and effective in treating elderly patients with AF.
Keywords: pulmonary vein isolation, left atrial appendage closure, cryo-balloon, rivaroxaban, atrial fibrillation, elderly patients
Introduction
Atrial fibrillation (AF) is the most frequent arrhythmia in older people because its prevalence rises dramatically as people age.1 Non-valvular AF is one of the most common types of AF, accounting for approximately 65.2% of all AF.2 As the global population ages, the incidence and prevalence of AF continue to rise.3 The study found that older people (ie ≥80 years) with AF accounted for 51.2% of the total AF population in 2016, but this is expected to rise to 65.2% in 2060.4 AF can lead to various long-term complications that can seriously affect patients’ quality of life and therefore require timely intervention and treatment.5 Catheter ablation is now the mainstay of clinical treatment for AF, particularly in patients who have failed or are intolerant to antiarrhythmic drug therapy.6,7 In addition, compared to radio-frequency catheter ablation, cryo-balloon ablation has the advantages of shorter procedure duration, better patient tolerance, and lower complication and adverse event rates.8
The significant negative impact of AF is thrombosis and embolism. Non-valvular AF has an annual embolic event rate of 5% and accounts for 15–20% of all cerebral embolic events, increasing the risk of death and disability by more than 5 times.9,10 Approximately 90% of thrombi in patients with non-valvular AF originate in the left atrial appendage, so thromboembolism in patients with AF can be prevented by closing the left atrial appendage.11 Research has shown that left atrial appendage closure (LAAC) is efficient and safe for preventing strokes in people with non-valvular AF.12,13 To achieve comprehensive AF control and stroke prevention, cryo-balloon pulmonary vein isolation (PVI) combined with LAAC can treat patients with AF. Moreover, the efficacy and safety of this combined procedure have been proven in several studies.14–17
However, there has not been a consensus on anticoagulation protocols after LAAC. The US Food and Drug Administration approved Rivaroxaban in July 2011 for the anticoagulation treatment of non-valvular AF. The dose of rivaroxaban for preventing thromboembolic events in non-valvular AF in the elderly is controversial due to the reduced physiological function of several organs, multiple underlying diseases, and poor surgical tolerance. Therefore, this study evaluated the safety and efficacy of the PVI and LAAC combined procedure and postoperative half-dose rivaroxaban anticoagulation in elderly patients with AF.
Methods
Study Population
A retrospective analysis of 203 patients with non-valvular AF who received cryo-balloon PVI and LAAC combined procedures in our cardiology department from 2019 to 2021 was performed. Inclusion criteria: 1) patients with non-valvular AF; 2) age ≥18 years; 3) CHA2DS2-VASc score ≥2 for men and CHA2DS2-VASc score ≥3 for women, or HAS-BLED score ≥3; 4) patients with contraindications or adverse effects to anticoagulant therapy. Ineligible patients had one of the following conditions from this study: 1) thrombus in the left atrium; 2) valvular AF; 3) new stroke or transient ischemic attack within 1 month; 4) combined acute coronary syndrome; 5) history of left auricular ligation; 6) active bleeding disorders; 7) severe infection and sepsis; 8) severe hepatic and renal dysfunction. Eighty-three elderly patients ≥80 years old were used as the elderly group, and 120 patients <80 years old were used as the non-elderly group. All patients signed an informed consent form. Shanghai Pudong New Area Zhoupu Hospital (Zhoupu Hospital affiliated with Shanghai Medical College of Health) ethic committee approved (ZPYY LL-2018-02) this study.
Pre-Operative Preparation
Preoperative enhanced computerized tomography (CT) of the left atrium and 3D reconstruction of the left auricle was performed to analyze the left auricle’s morphology and adjacent structural relationships. Transesophageal echocardiography was performed within the preoperative day to rule out left atrial thrombus, and the left auricular orifice, landing zone diameter and depth were estimated at 0°, 45°, 90°, and 135°. If patients are anticoagulated with warfarin preoperatively, they will continue to be anticoagulated with warfarin perioperatively (maintaining an International Normalized Ratio (INR) of 2.0 to 3.0). If the patient is anticoagulated with a non-vitamin K antagonist, the drug was discontinued 24 h before the procedure. They were fasting for at least 8 h before surgery.
Cryoballoon PVI and LAAC Combined Procedure
For patients with cryo-balloon PVI combined with the Watchman LAAC device, the method of occlusion followed by ablation was adopted, and for patients with cryo-balloon PVI combined with Lacbes left atrial appendage occlusive device, the process of occlusion followed by ablation was adopted. Patients were operated on by general anaesthesia and transesophageal ultrasound assistance. Intraoperative heparin maintained the prothrombin activation time (ACT) of 250–300 s. The cryo-balloon PVI, Watchman and Lacbes left atrial appendage occlusive device standardized procedure is described previously.16,17 Patients were anticoagulated with rivaroxaban plus clopidogrel for 60 days postoperatively if they had undergone percutaneous coronary stenting. Otherwise, they were anticoagulated with rivaroxaban only for 60 days. Of these, 10 mg of oral rivaroxaban was administered to the elderly group and 20 mg to the non-elderly group. Dual antiplatelet treatment with aspirin and clopidogrel was administered 60 days after surgery until 6 months postoperatively, followed by a single antiplatelet agent with aspirin as a long-term therapy.
Study Endpoints
The perioperative period was defined as the day of surgery to 7 days postoperatively. The primary endpoint was the annual incidence of composite clinical events. Secondary endpoints included recurrence of AF, new thromboembolic events or death, major hemorrhage (BARC type 3 and above), pericardial tamponade, and device thrombosis (DRT) events. The risk of arterial embolism and bleeding reduction was calculated by comparing the normalized observed rate of events per year of follow-up with the predicted rate of events per year based on CHA2DS2-VASc and HAS-BLED scores from validation trials. AF arrhythmia recurrence was defined as AF, atrial flutter or atrial tachycardia of more than 30s duration recorded outside the blanking period (3 months after surgery).
All patients were required to undergo an ambulatory electrocardiogram (ECG) for review at 3, 6, and 12 months postoperatively. Patients were assessed by transesophageal echocardiography for device location, residual blood flow, and DRT at 2 and 12 months postoperatively. Postoperative telephone follow-up was performed every 12 months to document clinical outcomes.
Statistical Analysis
Data were analyzed using SPSS 23.0 and MEDCALC statistical software. If the continuous variables conform to the normal distribution test, they are expressed as mean ± standard deviation. If the data variance was equal, a t-test was used for both samples; otherwise, the Mann–Whitney test was used. The x2 test was used to evaluate percentage-based categorical factors. For the survival analysis, the incidence of adverse events was assessed using the Kaplan-Meier estimation method. The Log rank test was used to determine P-values. Two-sided P < 0.05 was considered a statistically significant difference.
Results
Patient Characteristics
A total of 203 patients with non-valvular AF treated with the cryo-balloon PVI and LAAC combined procedure were included. Among them, 83 patients were in the elderly group and 120 in the non-elderly group. The mean age of patients in the elderly and non-elderly groups was 82.6 ± 1.7 and 69.2 ± 7.4 years, respectively. Preoperative CHA2DS2-VASc and HAS-BLED scores were significantly higher in the elderly than in the non-elderly group patients (p< 0.001). In addition, the incidence of heart failure was also significantly higher in the elderly group than in the non-elderly group (P< 0.001). In contrast, persistent AF and left atrial diameter incidence was not significantly different from those in the non-elderly group (P > 0.05). The basic characteristics of the patients in both groups are shown in Table 1.
 |
Table 1 Baseline Demographic Characteristics |
Perioperative Information
Pulmonary artery dissection was successfully achieved in both groups. The cryoablation procedure time was 74.2±6.2 min and 72.9±4.9 min in the elderly and non-elderly groups, respectively, and the difference was not statistically significant (Table 2). In the elderly group, 29 (35%) patients used the Lacbes device, and 54 (65%) patients used the WATCHMAN device for LAAC. 55 (46%) patients in the non-elderly group used the Lacbes device, and 65 (54%) patients used the WATCHMAN device for LAAC. The device implantation success rate was 100% in both groups. The elderly and non-elderly groups had one perioperative complication, namely puncture complication and pericardial tamponade, respectively. No other complications, such as pericardial tamponade, hemorrhage or phrenic nerve injury, were observed in either group. After the operation, 83.2% of patients in the elderly group were on oral rivaroxaban, the rest were on rivaroxaban combined with clopidogrel, and 75% of patients in the non-elderly group were on oral rivaroxaban, and the rest were on rivaroxaban combined with clopidogrel for anticoagulation.
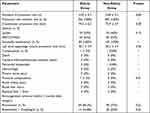 |
Table 2 Periprocedural Data |
Follow-Up
For the primary outcome, the annual rates of composite clinical events were 8.4% and 9.2% in the elderly and non-elderly groups, respectively, with no statistically significant difference (Table 3). Survival analysis, as shown in Figure 1, also showed that the annual rates of composite clinical events were not significantly different between elderly and non-elderly groups (P=0.85, hazard ratio (HR)=0.91, 95% confidence interval (CI) 0.36–2.33) (Figure 1).
 |
Table 3 Follow-Up Outcomes |
 |
Figure 1 Survival curves for the annual composite event rate. |
Regarding the secondary endpoints, no death and peripheral arterial thrombosis were found in the elderly or non-elderly age groups. Twenty-five patients in the elderly group and 32 non-elderly patients developed AF recurrence (P=0.59). Survival analysis also showed no significant difference in one-year AF-free incidence between the two groups (p=0.57, HR = 1.17, 95% CI: 0.68–2.03) (Figure 2). There was one hemorrhage and two cases of cerebral infarction/transient ischemic attack in each group, and the differences were not statistically significant (P > 0.05).
 |
Figure 2 Freedom from atrial fibrillation by survival analysis. |
Each patient was assessed with transesophageal echocardiography at 2 and 12 months. No residual flow was detected in patients in either group, and there was no displacement of devices. However, device-related thrombosis was seen in three patients in the elderly group and two in the non-elderly group, with no statistically significant difference (P > 0.05).
The CHA2DS2-VASc score predicted the incidence of arterial embolism in patients and found that the actual incidence of arterial embolism was 82.3% lower than expected in the elderly group and 83% lower than expected in the non-elderly group (Figure 3A). Prediction of the incidence of major postoperative bleeding in patients based on the HAS-BLED score revealed an 84.6% decrease in the actual incidence of significant bleeding in the elderly patients and a 23.6% decrease in the incidence of major bleeding in the non-elderly group compared with expectations (Figure 3B).
 |
Figure 3 Annualized arterial embolism (A) and bleeding (B) rate reduction from CHA2DS2-VASc and HAS-BLED score predicted rates in our population after the combined procedure. |
Discussion
The cryo-balloon PVI and LAAC combined procedure has gained widespread clinical acceptance and popularity as a new treatment for AF. The efficacy and safety of the cryo-balloon PVI and LAAC combined procedure in treating elderly patients with AF are the first time investigated in this research. This study found no statistical differences between elderly and non-elderly patients regarding procedure time, safety and efficacy. Although CHA2DS2 -VASc scores and HAS-BLED scores were higher in elderly patients than in non-elderly patients, there was no statistically significant change in the frequency of bleeding events between elderly patients on half-dose rivaroxaban and non-elderly individuals on a regular dose, suggesting that postoperative half-dose rivaroxaban anticoagulation may be more appropriate for elderly patients.
The management of patients with AF has two main purposes: to reduce peripheral arterial embolic events such as cerebral infarction while requiring attention to bleeding; the other is to reduce symptomatic AF. Radiofrequency and cryo-balloon ablation are currently the gold standard for catheter ablation and help control AF symptoms.18,19 Oral anticoagulants help prevent stroke and embolic events in AF patients with high thrombotic risk.6 However, the use of Oral anticoagulant therapy increases the risk of significant hemorrhage. Since 90% of the thrombus formation in nonvalvular AF patients is located in the left atrial appendage, LAAC has been proposed as an alternative to prevent stroke.20 In addition, the European consensus on left auricular closure is a viable approach to managing AF.12 Several studies have indicated the safety and efficacy of the combined cryo-balloon PVI and LAAC procedures in treating patients with AF. Swaans et al first reported using catheter ablation (CA) in combination with LAAC in 30 AF patients with a high risk of stroke or contraindications to oral anticoagulation therapy (OAC); this attempt was successful in all patients, with a 30% AF recurrence rate.14 Ren et al found cryo-balloon PVI and LAAC to have acceptable long-term safety and efficacy in treating patients with AF.17 Therefore, the cryo-balloon PVI and LAAC combined procedure may be a reasonable, effective and safe treatment option for patients with AF.
In this study, pulmonary vein potentiation isolation by cryo-balloon ablation was completed in 100% of 203 patients, and a left auricular occluder was successfully implanted. There were no significant differences in freezing duration and LAAC procedure time between the elderly and non-elderly groups. Perioperative complications were low and not statistically different between the two groups. There was no residual flow larger than 3 mm in either group. Only one patient in the non-elderly group had pericardial tamponade, and one in the elderly group had an arteriovenous fistula with no complications in the perioperative period. The low number of perioperative complications may be related to the simplicity of cryo-balloon ablation and the short operative time because the short operative time in elderly patients is important to reduce complications. The incidence of venous access complications due to cryo-balloon PVI was previously reported to be 1.79–2.3%,7,21 and the rate of puncture complications in the elderly group in this study was 1.2%. The success rate of the LAAC implantation in this study was 100%, and no perioperative major bleeding events were detected. The success rate of left auricular implantation in this study was higher than in the RECORD study (99.5%), and the perioperative major bleeding events were lower than in the RECORD study (1.06%).22 This result may be attributed to the fact that the surgeons in this study have rich surgical experience and have accumulated 1000 individual operations. The occlusions in our research centre can cover almost all the sizes of the left atrial appendage. In addition, the RECORD study also demonstrated a near doubling of the likelihood of successful left atrial appendage occlusion and a significant 58% reduction in the risk of life-threatening bleeding or hemorrhage in medical centres with ≥40 procedures per year compared to centres with <40 procedures per year.22
A one-year follow-up of all patients revealed no statistical difference in the one-year AF recurrence rates of 30.1% and 26.7% in the elderly and non-elderly groups, respectively. The AF recurrence rate in the elderly group in our study (30.1%) was consistent with the study by Tauseef et al (30%)23 but much higher than in the studies by Takashi (13.2%),24 which evaluated 1-year AF recurrence rates after cryo-balloon ablation in older patients’ ≥80 years of age with AF. This may be due to the different types of AF among the patients. The patients in Takashi’s study had paroxysmal AF, while only 45.8% of the elderly patients in this study had paroxysmal AF. Combining our and other studies,24 we found no difference in AF-free survival one year after surgery between elderly and non-elderly patients, regardless of the type of AF. The actual incidence of arterial embolism and bleeding was lower than expected in both groups at one-year follow-up, and the difference between the two groups was not statistically significant. Several studies have currently demonstrated the effectiveness of left atrial appendage occlusion in preventing peripheral artery embolization.25,26 The four-year follow-up of the PRAGUE-17 trial showed that in patients with non-valvular AF at high risk for stroke and bleeding, the LAAC treatment group had a non-inferior composite endpoint to the new oral anticoagulant group and a significantly lower rate of non-surgical clinically relevant bleeding with LAAC compared to the new oral anticoagulant group.25 Xavier et al also confirmed no difference in annual arterial embolism and adverse events between patients ≥80 and <80 years after left atrial appendage occlusion.26 Similar to previous studies, there was no statistical difference in the incidence of bleeding between the elderly and non-elderly groups in our study. Although the preoperative HAS-BLED score was higher in the elderly group than in the non-elderly group, the incidence of postoperative bleeding was lower than in the non-elderly group. This may be related to the different postoperative anticoagulant programs we gave to the two groups. Given the high rate of bleeding in elderly patients, we gave half dose of rivaroxaban anticoagulant to elderly patients, while the regular dose was given to non-elderly patients.
Previous studies reported that the incidence of DRT is 0.9% to 7.2%.27–29 This study found that the incidence of DRT in the elderly group and the non-elderly group was 3.6% and 1.7%, respectively, and there was no statistical difference between the two groups. The rate of DRT was slightly higher in the elderly group than the non-elderly group, which may be because most elderly patients had heart failure and were taking only half a dose of rivaroxaban. For the patients with DRT, we mostly used the regimen of extending anticoagulant time or increasing the dose of rivaroxaban, and the DRT disappeared after 2 months of reexamination. DRT can lead to arterial embolic events, but we did not find embolic events in the DRT patients in this study during follow-up. Jacqueline et al found that long-term administration of half-dose rivaroxaban amounts combined with aspirin in patients after LAAC reduced the risk of LAAC-related thrombosis, embolic events, and the composite endpoint of major bleeding.30 Long-term administration of half-dose rivaroxaban anticoagulation may be a good option. There was one pericardial tamponade event in each of the two groups at follow-up, occurring at 30 and 70 days postoperatively, respectively, with the pericardial tamponade occurring at 70 days postoperatively stemming from postcardiac injury syndrome, which develops from 3 to 140 days after cardiac-related surgery.31 Patients with a pericardial tamponade event were given pericardial drainage and an adjusted anticoagulation regimen. No recurrence of pericardial effusion was seen at the time of the subsequent follow-up.
Limitations
This study also has some limitations. First, this study was a single-centre study. Secondly, there were few elderly patients included in this study, and the follow-up time of patients was too short. Finally, no standard dose of rivaroxaban was set in the elderly group, which could not be compared with the half-dose rivaroxaban group for clinical events.
Conclusion
Cryo-balloon PVI and LAAC, a combined procedure and half-dose of rivaroxaban anticoagulation, are safe and effective in elderly patients with AF. However, multi-centre studies with larger sample sizes and more extended follow-up periods are still needed for validation.
Abbreviations
PVI, Pulmonary Vein Isolation; LAAC, Left Atrial Appendage Closure; AF, Atrial Fibrillation; CT, Computerized Tomography; ECG, Electrocardiogram; CA, Catheter Ablation; OAC, oral anticoagulation therapy.
Ethics
Shanghai Pudong New Area Zhoupu Hospital (Zhoupu Hospital affiliated with Shanghai Medical College of Health) ethic committee approved (ZPYY LL-2018-02) this study and conducted it in accordance with the 1964 Declaration of Helsinki and its later revisions.
Acknowledgment
We thank all participants for providing consent to publish their reports.
Funding
This study was supported by (1) Key Sub-Specialty of the Pudong New Area Health Committee (PWZy2020-08); (2) Construction of Peak Disciplines of Pudong New Area Health Commission (PWYgf2021-04).
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Orhan AL, Çınar T, Hayıroğlu Mİ, et al. Atrial fibrillation as a preoperative risk factor predicts long-term mortality in elderly patients without heart failure and undergoing Hip fracture surgery. Rev Assoc Med Bras. 2021;67(11):1633–1638. doi:10.1590/1806-9282.20210686
2. Kornej J, Börschel CS, Benjamin EJ, et al. Epidemiology of Atrial Fibrillation in the 21st Century: novel Methods and New Insights. Circ Res. 2020;127(1):e4–e20. doi:10.1161/CIRCRESAHA.120.316340
3. Xiang W, Zhang J, Liu M, et al. Antithrombotic therapy in elderly patients with non-valvular atrial fibrillation: a pilot study. Clin Interv Aging. 2015;10:e515–e519. doi:10.2147/CIA.S67974
4. Di Carlo A, Bellino L, Consoli D, et al. Prevalence of atrial fibrillation in the Italian elderly population and projections from 2020 to 2060 for Italy and the European Union: the FAI Project. Europace. 2019;21(10):e1468–e1475. doi:10.1093/europace/euz141
5. Alonso A, Norby FL. Predicting atrial fibrillation and its complications. Circ J. 2016;80(5):e1061–e1066. doi:10.1253/circj.CJ-16-0239
6. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):e2893–e2962. doi:10.1093/eurheartj/ehw210
7. Kuck KH, Brugada J, Furnkranz A, et al. Cryoballoon or Radiofrequency Ablation for Paroxysmal Atrial Fibrillation. N Engl J Med. 2016;374:e2235–e2245. doi:10.1056/NEJMoa1602014
8. Landolina M, Arena G, Iacopino S, et al. Center experience does not influence long-term outcome and peri-procedural complications after cryoballoon ablation of paroxysmal atrial fibrillation: data on 860 patients from the real-world multicenter observational project. Int J Cardiol. 2018;272:e130–e136. doi:10.1016/j.ijcard.2018.07.051
9. Lyaker MR, Tulman DB, Dimitrova GT, et al. Arterial embolism. Int J Crit Illn Inj Sci. 2013;3:e77. doi:10.4103/2229-5151.109429
10. Casu G, Gulizia MM, Molon G, et al. ANMCO/AIAC/SICI-GISE/SIC/SICCH consensus document: percutaneous occlusion of the left atrial appendage in non-valvular atrial fibrillation patients: indications, patient selection, staff skills, organisation, and training. Eur Heart J Suppl. 2017;19(suppl_D):e333–e353. doi:10.1093/eurheartj/sux008
11. Jain AK, Gallagher S. Percutaneous occlusion of the left atrial appendage in non-valvular atrial fibrillation for the prevention of thromboembolism: NICE guidance. Heart. 2011;97(9):e762–e765. doi:10.1136/hrt.2010.208223
12. Glikson M, Wolff R, Hindricks G, et al. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion - an update. Europace. 2020;22:e184. doi:10.1093/europace/euz258
13. Holmes DR, Kar S, Price MJ, et al. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014;64(1):e1–e12. doi:10.1016/j.jacc.2014.04.029
14. Swaans MJ, Post MC, Rensing BJ, et al. Ablation for atrial fibrillation in combination with left atrial appendage closure: first results of a feasibility study. J Am Heart Assoc. 2012;1:e002212. doi:10.1161/JAHA.112.002212
15. Phillips KP, Pokushalov E, Romanov A, et al. Combining Watchman left atrial appendage closure and catheter ablation for atrial fibrillation: multicentre registry results of feasibility and safety during implant and 30 days follow-up. Europace. 2018;20(6):e949–e955. doi:10.1093/europace/eux183
16. Ren Z, Zhang J, Zhu M, et al. Cryoablation Combined with Left Atrial Appendage Closure: a Safe and Effective Procedure for Paroxysmal Atrial Fibrillation Patients. Cardiol Res Pract. 2020;2020:6573296. doi:10.1155/2020/6573296
17. Ren Z, Zhang J, Wang S, et al. Two-Year Outcome From Combining Cryoballoon Ablation and Left Atrial Appendage Closure: CLACBAC Study. Front Cardiovasc Med. 2020;7:610537. doi:10.3389/fcvm.2020.610537
18. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018;20(1):e1–e160. doi:10.1093/europace/eux274
19. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74:e104–e132.
20. Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61:e755–e759. doi:10.1016/0003-4975(95)00887-X
21. Chen X, Xia Y, Lin Y, et al. Cryoballoon Ablation for Treatment of Atrial Fibrillation in a Chinese Population: five-Year Outcomes and Predictors of Recurrence After a Single Procedure. Front Cardiovasc Med. 2022;9:836392. doi:10.3389/fcvm.2022.836392
22. Su F, Gao C, Liu J, et al. Periprocedural Outcomes Associated With Use of a Left Atrial Appendage Occlusion Device in China. JAMA Netw Open. 2022;5(5):e2214594. doi:10.1001/jamanetworkopen.2022.14594
23. Akhtar T, Berger R, Marine JE, et al. Cryoballoon Ablation of Atrial Fibrillation in Octogenarians. Arrhythm Electrophysiol Rev. 2020;9:e104–e107. doi:10.15420/aer.2020.18
24. Kanda T, Masuda M, Kurata N, et al. Efficacy and safety of the cryoballoon-based atrial fibrillation ablation in patients aged ≥80 years. J Cardiovasc Electrophysiol. 2019;30(11):e2242–e2247. doi:10.1111/jce.14166
25. Osmancik P, Herman D, Neuzil P, et al. 4-Year Outcomes After Left Atrial Appendage Closure Versus Nonwarfarin Oral Anticoagulation for Atrial Fibrillation. J Am Coll Cardiol. 2022;79(1):e1–e14. doi:10.1016/j.jacc.2021.10.023
26. Freixa X, Schmidt B, Mazzone P, et al. Comparative data on left atrial appendage occlusion efficacy and clinical outcomes by age group in the Amplatzer™ Amulet™ Occluder Observational Study. Europace. 2021;23(2):e238–e246. doi:10.1093/europace/euaa262
27. Fauchier L, Cinaud A, Brigadeau F, et al. Device-Related Thrombosis After Percutaneous Left Atrial Appendage Occlusion for Atrial Fibrillation. J Am Coll Cardiol. 2018;71:e1528–e1536. doi:10.1016/j.jacc.2018.01.076
28. Bergmann MW, Betts TR, Sievert H, et al. Safety and efficacy of early anticoagulation drug regimens after WATCHMAN left atrial appendage closure: three-month data from the EWOLUTION prospective, multicentre, monitored international WATCHMAN LAA closure registry. Euro Intervention. 2017;13:e877–e884.
29. Saw J, Nielsen-Kudsk JE, Bergmann M, et al. Antithrombotic Therapy and Device-Related Thrombosis Following Endovascular Left Atrial Appendage Closure. JACC Cardiovasc Interv. 2019;12:e1067–e1076. doi:10.1016/j.jcin.2018.11.001
30. Garot P, Cormier B, Horvilleur J. Device-Related Thrombus After Left Atrial Appendage Closure. Interv Cardiol. 2019;14(1):e42–e44. doi:10.15420/icr.2018.21.3
31. Lehto J, Gunn J, Karjalainen P, et al. Incidence and risk factors of postpericardiotomy syndrome requiring medical attention: the Finland postpericardiotomy syndrome study. J Thorac Cardiovasc Surg. 2015;149(5):e1324–e1329. doi:10.1016/j.jtcvs.2015.01.031
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
