Back to Journals » Cancer Management and Research » Volume 15
Safety and Efficacy of Concurrent or Sequential Radiotherapy Plus (PD-1) Inhibitors in Oligometastatic Esophageal Cancer
Authors Duan Y, Qin W, Yang L, Zou B, Qie W, Song R, Xue L, Wang L
Received 8 October 2022
Accepted for publication 29 December 2022
Published 14 January 2023 Volume 2023:15 Pages 55—65
DOI https://doi.org/10.2147/CMAR.S391529
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Yanan Duan,1,2 Wenru Qin,1,3 Linlin Yang,1,4 Bing Zou,1 Wenting Qie,1,3 Ruiting Song,1,2 Lu Xue,1,2 Linlin Wang1
1Shandong Cancer Hospital and Institute, Shandong First Medical University and Shandong Academy of Medical Sciences, Jinan, Shandong, People’s Republic of China; 2Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, Shandong, People’s Republic of China; 3Weifang Medical University, Weifang, People’s Republic of China; 4Cheeloo College of Medicine, Shandong University, Jinan, People’s Republic of China
Correspondence: Linlin Wang, Shandong Cancer Hospital and Institute, Shandong First Medical University and Shandong Academy of Medical Science, Jinan, Shandong, People’s Republic of China, Email [email protected]
Purpose: We assess real-world outcomes, including safety and efficacy, of concurrent or sequential treatment with radiotherapy plus programmed cell death protein 1 (PD-1) inhibitors in patients with oligometastatic esophageal cancer (OMEC).
Methods: This cohort study retrospectively collected clinical data of patients with synchronous or metachronous OMEC. All patients underwent concurrent or sequential treatment with radiotherapy plus PD-1 inhibitors. Each patient had up to five measurable metastatic lesions and up to three organs involved. Study endpoints were progression-free survival (PFS), treatment-related toxicities, locoregional progression-free survival (LRPFS), objective response rate (ORR), and disease control rate (DCR). Description statistics and Kaplan–Meier models were used for statistical analysis.
Results: A total of 86 patients were included, most of whom were diagnosed with squamous cell carcinoma histology (98%) and presented with synchronous OMEC (64%). The median follow-up period was 17 months (range: 6– 32 months), the median PFS was 15.2 months (95% confidence interval: 12.1– 18.2 months); and the 1- and 2-year PFS rates were 61.4% and 26.7%, respectively. The 1- and 2-year LRPFS were 91.3% and 57.3%, respectively. The ORR and DCR were 46.5% and 91.8%, respectively. Forty-two patients (48.8%) experienced grade 3 or higher treatment-related adverse events (TRAEs); a grade 5 treatment-related adverse event was observed in one patient (1.2%) who died of immune-related pneumonitis.
Conclusion: Combining radiotherapy with PD-1 inhibitors is a safe and effective treatment option for patients with OMEC. No new safety concerns were identified in this study. However, due to the potential risk of cumulative toxicity, an individual risk-benefit assessment for each patient is required prior to treatment initiation.
Keywords: oligometastatic disease, esophageal cancer, PD-1 inhibitors, radiotherapy
Introduction
Esophageal cancer (EC) is the seventh most common type of cancer and the sixth-leading cause of cancer-related deaths worldwide.1 Overall, 33–50% of EC patients were diagnosed with distant metastases, and 20–50% of early or local advanced EC patients would inevitably develop distant metastasis after standard multimodal therapy.2 The outcome of metastatic EC patients was poor with the 5-year survival rate of less than 5%.3 Immune checkpoint inhibitors (ICI) have revolutionized treatment schemes across ESCC patients.4 In particular, PD-1 inhibitors in combination with chemotherapy have been recommended as the standard treatment for metastatic EC patients.4–8
Oligometastatic disease (OMD) is an intermediate state between locally advanced and widespread metastatic disease, which was first introduced in 1995 by Hellman and Weichselbaum.9 OMD was generally defined as “up to five measurable metastatic lesions and up to three organs involved”,10–13 and was associated with a better prognosis compared to patients suffering polymetastatic disease.
It should be noted that except for immunotherapy and chemotherapy, radiotherapy (RT) also plays an important role in the treatment of metastatic EC patients, especially oligometastatic esophageal cancer (OMEC).14–17 A recent Phase II randomized trial has shown that RT is associated with improved PFS and OS in OMEC patients compared to systemic chemotherapy alone.18 Our previous study also demonstrated the survival benefit from local RT of primary lesion for OMEC patients.19
Previous studies in the era of immunotherapy have demonstrated the synergistic effect of RT and immunotherapy by inducing the activation and recruitment of more antitumor effector immune cells, as well as the modulation of the tumor immune microenvironment.20–22 The combination of RT and ICIs has shown survival benefits in various cancers including locally advanced EC.23 Thus, we aimed to determine the efficacy and safety of concurrent or sequential RT combined with PD-1 inhibitors in OMEC.
Material and Methods
Patients
This study was approved by the Medical Ethics Committee of Shandong Cancer Hospital. Data were collected from patients who were treated at Shandong Cancer Hospital from October 2019 to December 2021. Due to the retrospective nature of this study, the requirement for patient informed consent was waived by the aforementioned committee (SDTHEC 2022012032). We retrospectively analyzed patients with OMEC who received radiotherapy and PD-1 inhibitors. The inclusion criteria for this study were as follows: (1) pathologically confirmed EC; (2) tumor staging performed according to the American Joint Committee on Cancer 8th edition; (3) presence of de novo synchronous OMEC (ITIM ≤6 months) or de novo metachronous OMEC (ITIM >6 months); (4) involvement of up to five measurable metastatic lesions and up to three organs;24 (5) each patient receives at least 2 cycles of PD-1 inhibitors; (6) oligometastatic lesions or primary tumor treated with radiotherapy. The exclusion criteria were as follows: (1) presence of other active synchronous carcinomas; (2) occurrence of bleeding, perforation, autoimmune diseases, or diseases affecting radiotherapy prior to treatment; (3) therapy involving fewer than two treatment cycles with PD-1 inhibitors; and (4) patients lost to follow-up. RT concurrent with PD-1 was defined as receiving at least one treatment PD-1 inhibitor during the course of radiotherapy or within 7 days from the last session. RT sequential with PD-1 was defined as follows: 1) the interval between the last dose of PD-1 inhibitors and initiation of radiotherapy more than 7 days; 2) when the patients completed radiotherapy, the beginning of the administration of PD-1 inhibitors was also more than 7 days.
Identification of metastatic lesions was performed through diagnostic computed tomography (CT) or 18F-fluorodeoxyglucose positron-emission tomography/computed tomography (PET/CT). Magnetic resonance imaging was required for some lesions, such as liver, bone, and brain metastases. Whole-body bone scan was performed for patients without PET/CT scan data. In case of unclear diagnosis of metastatic lesions, a pathological biopsy was performed for confirmation.
Treatments
Prior to treatment initiation, each patient was evaluated by a multidisciplinary team, including a thoracic surgeon, a radiation oncologist, and a medical oncologist. All patients received radiotherapy and systemic therapy (chemotherapy plus PD-1 inhibitors). The delineation of target volumes, such as gross tumor volume (GTV), clinical target volume (CTV), planned target volume (PTV), and organs at risk volume (OAR), was based on the Radiation Therapy and Oncology Group guidelines. Radiotherapy was planned on the Eclipse Treatment Planning System (version 13.5.35; Varian Medical Systems, Palo Alto, CA, USA) by a radiation oncologist and a physiotherapist. The team attempted to increase the irradiation dose to the target volumes without further exposure of normal tissue to radiation. The dose-fractionation prescription was determined by the treating physicians and modulated according to the maximum diameter and site of the tumor. Eventually, the prescribed doses of radiotherapy were 30–60 Gy in 1.8–3 Gy fractions once daily, for a total of five fractions per week.
The treating physicians determined the treatment strategies for each patient based on their age, performance status, and previous treatment. Chemotherapy doses and adjustments were determined according to guidelines established by the National Comprehensive Cancer Network (NCCN) and the Chinese Society of Clinical Oncology (CSCO). The selection of PD-1 monoclonal antibody (eg, pembrolizumab, camrelizumab, sintilimab, and tislelizumab) was based on the financial situation of the patient, the protocol of the clinical trial, and recommendation by the physician. All treatments were administered intravenously in 3-week cycles. All patients were followed up through clinical visits or telephone interviews.
Statistical Analysis
The primary endpoints were PFS and treatment-related adverse events (TRAEs). PFS was defined as the time from the diagnosis of OMEC to the date of progression, death, or last follow-up. TRAEs were assessed according to the Common Terminology Criteria for Adverse Events, version 4.03. Secondary outcomes were locoregional progression-free survival (LRPFS), objective response rate (ORR), disease control rate (DCR), and duration of response (DOR). The LRPFS was based on the time from diagnosis of OMEC to the detection of locoregional failure (LRF), death, or last follow-up. LRF was defined as progression in the radiation field on CT or other imaging examinations, including PET/CT. Distant metastasis (DM) was defined as progression beyond the radiation field. Tumor response was based on the Response Evaluation Criteria in Solid Tumors, version 1.1 (RECIST v1.1). Treatment response was defined as complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD). ORR included CR and PR, while DCR included CR, PR, and SD. The DOR was measured from the time of response until progression or last follow-up. The SPSS statistical software (version 25.0) was used for statistical analyses. Progression-free survival curves were plotted using the Kaplan–Meier method and compared through the Log rank test. The median follow-up time was calculated using the reverse Kaplan–Meier method. All statistical tests were conducted at a 5% level of significance, and 95% confidence intervals (CIs) were calculated. Two-tailed P-values <0.05 indicated statistically significant differences.
Results
Patient Selection
From October 2019 to December 2021, a total of 800 patients with EC who received PD-1 inhibitors were screened for OMEC. Synchronous or metachronous OMEC was identified in 224 patients (28%). Patients with other active synchronous carcinomas (n=11) and those who only received systemic therapy (n=127) were excluded. Eventually, 86 patients with OMEC who received radiotherapy plus PD-1 inhibitors were included in this study. Figure 1 shows the flowchart of patient selection.
Baseline Characteristics
Of the 86 patients (median age: 61.2 years; interquartile range: 57.8–66.7 years), the vast majority were diagnosed with squamous cell carcinoma (n=84, 98%); the remaining two patients were diagnosed with neuroendocrine carcinoma and adenocarcinoma, respectively. The most predominant pathological stage was T3 (n=66, 77%), and the actual percentage of patients who had PET/CT staging was 25.6% (22/86). Patient and tumor characteristics are listed in Table 1.
 |
Table 1 Baseline Characteristics (n=86) |
OMEC Characteristics
Of the patients, 54 and 32 had synchronous OMEC (SO) and metachronous OMEC (MO), respectively. The number of metastatic lesions was 1–2 and 3–5 in 42 (49%) and 44 (51%) patients, respectively. The distribution of distant metastases was as follows: only extraregional lymph node (n=61, 71%); only distant organ (n=17, 20%); and both extraregional lymph node and distant organ (n=8, 9%). Table 2 shows details of the sites of distant metastases.
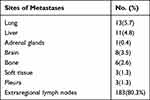 |
Table 2 Details of Distant Metastatic Sites (n=228) |
Management for OMEC
The management course was either “RT concurrent with PD-1” (51%) or “RT sequential with PD-1” (49%). Radiotherapy was administered at the primary site and/or metastatic sites. All patients in this study received intensity-modulated radiotherapy (IMRT); three patients received simultaneous integrated boost intensity-modulated radiotherapy (SIB-IMRT). The median dose of radiotherapy was 50.4Gy (range: 30–61.2Gy). A total of 82 patients completed the course of radiotherapy, three patients interrupted because of severe pulmonary infection, and one patient discontinued radiotherapy due to poor tolerance. In addition, one patient discontinued treatment due to active tuberculosis after four cycles of immunotherapy plus radiotherapy and experienced disease progression. Chemotherapy regimens included the TP (docetaxel plus platinum) regimen (n=67), PF (platinum plus fluorouracil) regimen (n=4), or other regimens (n=15). Single-agent chemotherapy was selected for nine frail patients; another nine patients received anti-vascular targeted therapy with apatinib. The median number of chemotherapy cycles was four (range: 2–6 cycles).
Outcome
The median follow-up period was 17 months (range: 6–32 months) that ended on July 1, 2022. The median PFS was 15.2 months (95% CI: 12.1–18.2 months) across all included patients (Figure 2A), 15.1 months for SO patients (95% CI: 11.7–18.5 months), and 16.3 months (95% CI: 12.0–20.6 months) for those with MO (P=0.63) (Figure 2B). No significant differences in median PFS were observed between patients with SO and those with MO. The 1- and 2-year PFS rate was 61.4% and 26.7%, respectively. At least one follow-up imaging scan was available for each of the 86 patients. Overall, the ORR and the DCR were 46.5% and 91.8%, respectively. The median DOR was 13.5 months (95% CI, 11.2–16.0 months) (Table 3).
 |
Table 3 Response to Treatment |
At the cutoff date, 46 patients (53.5%) had experienced disease recurrence or progression. Patterns of failure were as follows: only locoregional (16.3%); only distant metastasis (23.3%); both locoregional and distant metastasis (7.0%); and unable to confirm due to death (7.0%). In addition, the 1- and 2-year LRPFS rates were 91.3% and 57.3%, respectively. Failure patterns in the full-analysis population are listed in Table 4.
 |
Table 4 Failure Patterns in Full-Analysis Population |
Table 5 shows the details of TRAEs. The most common TRAEs were hematological toxicity and gastrointestinal issues. Grade 3 or higher TRAEs occurred in 42 patients (48.8%), seven patients (8.1%) experienced grade 3 or higher immune-related adverse effects (irAEs). Of note, a grade 5 serious event was observed in one patient (1.2%) with SO; the patient developed refractory pneumonia after completion of concurrent treatment with radiotherapy and PD-1 inhibitors and died 4 months later. Moreover, one patient with MO discontinued radiotherapy due to poor tolerance and died because of a tracheoesophageal fistula that developed following tumor progression 3 months later.
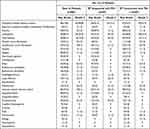 |
Table 5 Treatment-Related Adverse Events |
Notably, five patients had PFS > 2 years (mean: 27.6 months; range: 25–32 months). Four patients had lower thoracic esophagus with supraclavicular lymph node metastasis, while one patient had middle thoracic esophagus with retroperitoneal lymph node metastasis. Three patients with SO received radiotherapy for primary tumors and metastases, while two patients with MO received radiotherapy for metastases. All five patients received radiotherapy doses >50 Gy, and two of those reached a dose of 60 Gy.
Discussion
Oligometastatic disease refers to an intermediate state between localized disease and widespread dissemination. This type of disease is linked to a better prognosis compared to multiple-site metastasis. Clinically, oligometastatic disease offers the opportunity to improve prognosis through local treatment, such as surgery, radiotherapy, or other ablative approaches. The existence of the oligometastatic status in EC has been demonstrated in previous studies.19,25 In the present study, the incidence of OMEC was 28%. Several studies have shown that the addition of local treatment may improve the prognosis of patients with OMEC.16–18 Similar findings were observed in our study.
The median PFS of patients with OMEC who received radiotherapy plus PD-1 inhibitors reached 15 months, regardless of SO or MO. This median PFS is significantly better than that of poly-metastatic EC.4–6,8
Recently, several randomized trials demonstrated that the combination of PD-1 inhibitors with chemotherapy is becoming the standard of care for metastatic EC, significantly prolonging the survival of patients.5–8,26 Furthermore, radiotherapy plays an important role in the treatment of EC by improving the local control rate (LCR) and delaying disease progression. Due to the lack of evidence from large, randomized, and controlled trials, there is controversy regarding the optimal treatment strategy for OMEC. Nevertheless, the efficacy and safety of radiotherapy in patients with OMEC have been demonstrated in several studies.16–18 Liu et al18 conducted a prospective Phase 2 study, which included 34 OMEC patients with up to two metastatic lesions. These patients received stereotactic body radiation therapy with or without chemotherapy. The final results revealed a median PFS of 13.3 months for patients with oligometastatic esophageal squamous cell carcinoma; the 1- and 2-year PFS rates were 55.9% and 33.8%, respectively; the 1-year LCR was 92.1%. These results were largely consistent with our study. In the previous study, the 2-year LCR remained at 92.1%, whereas it was only 57.3% in the present study. This discrepancy may be attributed to differences in the study design; for example, the previous study only included patients with one or two metastatic lesions, whereas our study included patients with three to five metastatic lesions (n=44, 51%). Large tumor burden is associated with a poor LCR. Nevertheless, our findings remain comparable to those obtained from other studies investigating locally advanced EC. Xu et al14 compared the efficacy of different radiation doses (60 vs 50 Gy) for the treatment of locally advanced squamous EC. The results revealed that there were no statistically significant differences in LRPFS (P=0.94) between the two treatment groups. The 2-year LRPFS rates were 56.9% and 57.2%, respectively. These findings were similar to the results of our study; however, it should be noted that the previous study included a population without distant metastases, whereas our study involved patients with up to five distant metastases. This similarity may be attributed to the addition of PD-1 inhibitors.
PD-1 inhibitors plus chemotherapy may improve DCR compared to chemotherapy only. The present study demonstrated that radiotherapy plus PD-1 inhibitors is a more effective approach compared with chemoradiotherapy in patients with OMEC. Our findings also indicate that, following the addition of PD-1 inhibitors, the LCR of OMEC is non-inferior to that of locally advanced EC. Radical local treatment plus systemic therapy is a promising option for patients with OMEC.
In addition, we noticed that the PFS of five patients with OMEC was >2 years. These patients shared some characteristics; for instance, four patients had metastases confined to one extra-regional lymph node station and up to two extra-regional lymph node stations. All five patients were treated with radical radiotherapy (dose: >50 Gy). This indicates that OMEC patients with metastases present in up to two extra-regional lymph node stations can be treated with more aggressive radical radiotherapy to potentially extend survival. Considering the above results, patients with OMEC and a physical condition that permits the completion of radical local treatment combined with systemic treatment may benefit from a relatively more aggressive therapeutic approach.
The study conducted by Liu et al18 investigated high-dose radiotherapy (48 Gy in 8-Gy fractions). In contrast, the present study focused on low-dose radiotherapy (30–60 Gy in 1.8–3 Gy fractions). This could potentially introduce bias in the interpretation of the results. Nevertheless, previous studies have confirmed lower rates of side effects and higher LCR associated with low-dose radiotherapy in patients with OMEC.16,17 Li et al16,17 and Shi et al17 demonstrated the superior efficacy and manageable toxicity of low-dose radiotherapy combined with chemotherapy versus chemotherapy alone in patients with SO and MO (with up to five measurable metastatic lesions and up to three organs involved). The median overall survival rate in these studies was 14 and 18.5 months, respectively. Compared with these findings, the treatment in the present study achieved a good prognosis (median PFS: 15 months), which may be attributed to the addition of PD-1 inhibitors. The above findings demonstrated that the combination of radiotherapy plus immunotherapy may extend survival.
Despite the satisfactory efficacy of radiotherapy plus PD-1 inhibitors, treatment-related toxicity cannot be ignored. In our study, the incidence of grade ≥3 TRAEs was 48.8%, which is generally similar to that observed in patients receiving systemic therapy alone. Patients who received “RT concurrent with PD-1” had a slightly higher incidence of TRAEs versus those who received “RT sequential with PD-1”; nonetheless, the overall safety was manageable. Of note, one patient experienced a grade 5 TRAE in our study (1.2%). This patient developed refractory pneumonia after completing radiotherapy to the abdominal and retroperitoneal lymph nodes (total dose: 48.6Gy) and eventually died of respiratory failure 4 months later. It should be noted that the incidence of pneumonia in our study was higher than that reported in patients receiving chemotherapy plus immunotherapy.
The incidence of grade 1–2 pneumonia in our study was 12.8% (11/86); in other studies, this incidence ranged 1–5%. Rate of grade ≥3 pneumonia in this study was 4.7%; in other studies, this rate ranged 1–2%. This difference may be related to injury to the alveolar epithelium caused by the combination of radiotherapy plus PD-1 inhibitors. Several prospective studies examined the potential toxicity of immunotherapy combined with radiotherapy.27–30 Similar to our findings, in these studies, the incidence of grade ≥3 TRAEs in patients receiving radiotherapy plus PD-1 inhibitors ranged 10–57%.
This study had several limitations. Firstly, due to the retrospective nature of the study, selection bias may have occurred. Secondly, histologically, the majority of cases were squamous cell carcinoma; consequently, the generalization of our results in other histological types is limited. Finally, the follow-up period in this study was relatively short. Thus, studies with longer follow-up periods are necessary to evaluate PFS and improve treatment.
Conclusions
This is the first study showing that radiotherapy combined with systemic therapy (PD-1 inhibitors and chemotherapy) improves efficacy and overall safety. No new safety concerns were identified in this study. However, due to the potential risk of cumulative toxicity, an individual risk-benefit assessment for each patient is required prior to treatment initiation. Moreover, large prospective studies are warranted to validate the present findings.
Data Sharing Statement
Data are available upon reasonable request to the corresponding author ([email protected]).
Ethics and Consent Statements
All procedures performed in studies involving human participants were in accordance with ethical standards, and this research was approved by the Ethics Committee of Shandong Cancer Hospital (SDTHEC 2022012032). This study was performed in accordance with the principle of the 1975 Declaration of Helsinki and its later amendments or comparable ethical standards, and data confidentiality was ensured. The date was anonymized for this study. Due to the retrospective nature of the study, informed consent was waived by the Ethics Committee of Shandong Cancer Hospital and Institute.
Author Contributions
The authors contribute to the conception, design, and execution of the study, as well as the acquisition, analysis, and interpretation of data. The authors participated in drafting, revising, or critically reviewing the article. They approved the final version of the manuscript, agreed with the submission of the article to the journal, and assume responsibility for all aspects of the work.
Funding
This research was supported by the Natural Science Foundation of Shandong Province, (Grant number ZR2019LZL012), Jinan Clinical Medical Science and Technology Innovation Plan (Grant number 202019043), National Natural Science Foundation of China (Grant number 8217102892), The Key Research and Development Program of Shandong (Major Science & Technology Innovation Project) (2021SFGC0501), and Start-up fund of Shandong Cancer Hospital (2022-B14).
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Ghaly G, Kamel M, Nasar A, et al. Locally advanced esophageal cancer: what becomes of 5-year survivors? J Thorac Cardiovasc Surg. 2016;151(3):726–732. doi:10.1016/j.jtcvs.2015.10.096
3. National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer stat facts: esophageal and stomach cancer. Avialable from: https://seer.cancer.gov/statfacts/html/esoph.html.
4. Kojima T, Shah MA, Muro K, et al. Randomized Phase III KEYNOTE-181 study of pembrolizumab versus chemotherapy in advanced esophageal cancer. J Clin Oncol. 2020;38(35):4138–4148.
5. Luo H, Lu J, Bai Y, et al. Effect of camrelizumab vs placebo added to chemotherapy on survival and progression-free survival in patients with advanced or metastatic esophageal squamous cell carcinoma: the ESCORT-1st randomized clinical trial. JAMA. 2021;326(10):916–925. doi:10.1001/jama.2021.12836
6. Lu Z, Wang J, Shu Y, et al. Sintilimab versus placebo in combination with chemotherapy as first line treatment for locally advanced or metastatic oesophageal squamous cell carcinoma (ORIENT-15): multicentre, randomised, double blind, Phase 3 trial. BMJ. 2022;377:e068714. doi:10.1136/bmj-2021-068714
7. Doki Y, Ajani JA, Kato K, et al. Nivolumab Combination Therapy in Advanced Esophageal Squamous-Cell Carcinoma. N Engl J Med. 2022;386(5):449–462. doi:10.1056/NEJMoa2111380
8. Sun JM, Shen L, Shah MA, et al. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–771. doi:10.1016/S0140-6736(21)01234-4
9. Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13(1):8–10. doi:10.1200/JCO.1995.13.1.8
10. Stone E, Vinod SK. Oligometastatic disease in NSCLC - not just wishful thinking? J Thorac Oncol. 2019;14(12):2042–2045. doi:10.1016/j.jtho.2019.10.008
11. Ettinger DS, Wood DE, Aisner DL, et al. NCCN guidelines insights: non-small cell lung cancer, version 2.2021. J Natl Compr Canc Netw. 2021;19(3):254–266. doi:10.6004/jnccn.2021.0013
12. Levy A, Hendriks LEL, Berghmans T, et al. EORTC Lung Cancer Group survey on the definition of NSCLC synchronous oligometastatic disease. Eur J Cancer. 2019;122:109–114. doi:10.1016/j.ejca.2019.09.012
13. Dingemans AC, Hendriks LEL, Berghmans T, et al. Definition of synchronous oligometastatic non-small cell lung cancer-a consensus report. J Thorac Oncol. 2019;14(12):2109–2119. doi:10.1016/j.jtho.2019.07.025
14. Xu Y, Dong B, Zhu W, et al. A phase iii multicenter randomized clinical trial of 60 Gy versus 50 Gy radiation dose in concurrent chemoradiotherapy for inoperable esophageal squamous cell carcinoma. Clin Cancer Res. 2022;28(9):1792–1799. doi:10.1158/1078-0432.CCR-21-3843
15. Borg D, Sundberg J, Brun E, et al. Palliative short-course hypofractionated radiotherapy followed by chemotherapy in esophageal adenocarcinoma: the Phase II PALAESTRA trial. Acta Oncol. 2020;59(2):212–218. doi:10.1080/0284186X.2019.1670861
16. Li J, Wen Y, Xiang Z, et al. Radical radiotherapy for metachronous oligometastasis after initial treatment of esophageal cancer. Radiother Oncol. 2021;154:201–206. doi:10.1016/j.radonc.2020.09.042
17. Shi Z, Zhu X, Ke S, et al. Survival impact of concurrent chemoradiotherapy for elderly patients with synchronous oligometastatic esophageal squamous cell carcinoma: a propensity score matching and landmark analyses. Radiother Oncol. 2021;164:236–244. doi:10.1016/j.radonc.2021.09.033
18. Liu Q, Zhu Z, Chen Y, et al. Phase 2 study of stereotactic body radiation therapy for patients with oligometastatic esophageal squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2020;108(3):707–715. doi:10.1016/j.ijrobp.2020.05.003
19. Li B, Wang R, Zhang T, et al. Development and validation of a nomogram prognostic model for esophageal cancer patients with oligometastases. Sci Rep. 2020;10(1):11259. doi:10.1038/s41598-020-68160-6
20. Dovedi SJ, Cheadle EJ, Popple AL, et al. Fractionated radiation therapy stimulates antitumor immunity mediated by both resident and infiltrating polyclonal T-cell populations when combined with PD-1 blockade. Clin Cancer Res. 2017;23(18):5514–5526. doi:10.1158/1078-0432.CCR-16-1673
21. Gong X, Li X, Jiang T, et al. Combined radiotherapy and Anti-PD-L1 Antibody synergistically enhances antitumor effect in non-small cell lung cancer. J Thorac Oncol. 2017;12(7):1085–1097. doi:10.1016/j.jtho.2017.04.014
22. Deng L, Liang H, Burnette B, et al. Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest. 2014;124(2):687–695. doi:10.1172/JCI67313
23. Zhang W, Yan C, Zhang T, et al. Addition of camrelizumab to docetaxel, cisplatin, and radiation therapy in patients with locally advanced esophageal squamous cell carcinoma: a phase 1b study. Oncoimmunology. 2021;10(1):1971418. doi:10.1080/2162402X.2021.1971418
24. Lievens Y, Guckenberger M, Gomez D, et al. Defining oligometastatic disease from a radiation oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020;148:157–166. doi:10.1016/j.radonc.2020.04.003
25. Kroese TE, Christ SM, van Rossum PSN, et al. Incidence and survival of patients with oligometastatic esophagogastric cancer: a multicenter cohort study. Radiother Oncol. 2022;173:269–276. doi:10.1016/j.radonc.2022.06.012
26. Kato K, Cho BC, Takahashi M, et al. Nivolumab versus chemotherapy in patients with advanced oesophageal squamous cell carcinoma refractory or intolerant to previous chemotherapy (ATTRACTION-3): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(11):1506–1517. doi:10.1016/S1470-2045(19)30626-6
27. Welsh J, Menon H, Chen D, et al. Pembrolizumab with or without radiation therapy for metastatic non-small cell lung cancer: a randomized phase I/II trial. J Immunother Cancer. 2020;8(2):e001001. doi:10.1136/jitc-2020-001001
28. Verma V, Cushman TR, Selek U, Tang C, Welsh JW. Safety of combined immunotherapy and thoracic radiation therapy: analysis of 3 single-institutional Phase I/II trials. Int J Radiat Oncol Biol Phys. 2018;101(5):1141–1148. doi:10.1016/j.ijrobp.2018.04.054
29. Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet. 2019;393(10185):2051–2058. doi:10.1016/S0140-6736(18)32487-5
30. Zhang W, Yan C, Gao X, et al. Safety and feasibility of radiotherapy plus camrelizumab for locally advanced esophageal squamous cell carcinoma. Oncologist. 2021;26(7):e1110–e1124. doi:10.1002/onco.13797
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


