Back to Journals » International Journal of General Medicine » Volume 15
Role of Procalcitonin in Predicting Mortality and Organ Dysfunction at Intensive Care Admission
Authors Suranadi IW , Sinardja CD, Suryadi IA
Received 1 March 2022
Accepted for publication 5 May 2022
Published 12 May 2022 Volume 2022:15 Pages 4917—4923
DOI https://doi.org/10.2147/IJGM.S362558
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
I Wayan Suranadi, Cynthia Dewi Sinardja, Iwan Antara Suryadi
Department of Anesthesiology and Intensive Care, Faculty of Medicine, Universitas Udayana/Sanglah General Hospital, Denpasar, Bali, 80113, Indonesia
Correspondence: I Wayan Suranadi, Department of Anesthesiology and Intensive Care, Faculty of Medicine, Universitas Udayana/Sanglah General Hospital, Diponegoro Street, Dauh Puri Klod, Denpasar, 80113, Indonesia, Tel/Fax +62361-227911, Email [email protected]
Objective: To assess the prognostic utility of procalcitonin (PCT) in high-risk sepsis patients.
Methods: A retrospective cohort study was conducted with the inclusion of all eligible intensive care unit patients with Sequential Organ Failure Assessment (SOFA) score of 2 or more.
Results: A total of 228 patients were acquired from January 2018 to December 2020, with male predominant (58.8%), mean age of 53.61 years old. The overall 28-day mortality was 57.5%. In the group with PCT ≥ 7 ng/mL, 28-day mortality was 68.5% (87 patients out of a total of 127). Cox regression showed that in this group, the risk of mortality occurring within 28 days from the day of ICU admission was 1.55 times higher (95% CI 1.074– 2252, p value 0.02). Independent sample t-test showed that in this group, the mean SOFA score was higher by 2.279 (95% CI 1.497– 3.060, p value < 0.001).
Conclusion: Procalcitonin levels are associated with mortality and SOFA scores in sepsis patients. Further studies need to be carried out to provide more evidence so that it can help reduce the mortality and morbidity of sepsis.
Keywords: procalcitonin, SOFA score, mortality, sepsis, ICU
Introduction
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. Sepsis is a global health crisis, with an estimated 31.5 million cases per year. The mortality rate for sepsis ranges from 20% to 80%. Hospital costs due to sepsis in the United States in 2011 were $20 billion.1 The increasing incidence of sepsis as well as its high mortality and morbidity have an impact on the burden of health services. The body’s response to sepsis is complex, and not all patients respond similarly. Therefore, one of the challenges of treating sepsis is the identification of patients at higher risk, who might benefit from close monitoring and intensive therapy. The use of biomarkers can be a solution to these challenges.2 Many biomarkers are available for sepsis but data regarding appropriate biomarkers for risk identification in patients with sepsis are lacking.
Measurement of sepsis biomarkers can help to make early intervention and can reduce the risk of death. Compared to various other biomarkers, procalcitonin (PCT) has a good diagnostic value for sepsis. Plasma PCT concentrations increase very rapidly (6–12 hours) after infection. Plasma PCT concentrations are also indirectly related to the severity of sepsis and systemic inflammatory reactions. In addition, the elimination of PCT indicates the course of the disease and successful treatment. Several studies emphasize the importance of the role of PCT as a biochemical marker for early detection of the infectious process in critically ill patients and also has several other functions such as a prognostic factor for sepsis.3 PCT research as an outcome predictor can help determine more optimal treatment and can improve the outcome of sepsis. In addition, existing data can also help in reducing the burden of sepsis. Therefore, the current study aims to assess the prognostic utility of procalcitonin (PCT) in high-risk sepsis patients.
Methodology
Study Design
This is a retrospective cohort analytic observational study in patients with sepsis in the intensive care unit (ICU) of a tertiary hospital. This study began with an assessment of PCT levels in patients with sepsis either when the patient arrived at the hospital or when the patient was admitted to the ICU. Data on PCT levels were identified based on medical records. The research subjects were divided into 2 groups according to previous study, namely the group with high PCT (≥7 ng/mL) and the group with low – moderate PCT (<7 ng/mL).4 Each group was followed-up through medical records for 28 days after being admitted to the ICU and assessed on life/death status and Sequential Organ Failure Assessment (SOFA) scores. The current study design was approved by the research committee of Universitas Udayana/Sanglah General Hospital (approval number 2651/UN14.2.2.VII.14/LT/2021), and individual consent was obtained from all study participants. This study complies with the Declaration of Helsinki and its amendments.
Study Population
All patients aged 18 years and over who were admitted to the ICU from January 1, 2018 – December 31, 2020 with clinical infection admitted to the ICU and signs of organ dysfunction, namely a SOFA score of 2 or more, were examined for PCT levels during the treatment period at the hospital. These patients were eligible for inclusion in this study. Patients were excluded if there was no medical record data at the expected time.
Data Collection and Laboratory Diagnostics
PCT measurements were taken from electronic medical records either when the patient arrived at the hospital or when the patient was admitted to the ICU. In this study, patients were divided into two groups based on PCT values, namely the group with high PCT (≥7 ng/mL) and the group with low – moderate PCT (<7 ng/mL).4 The Sequential Organ Failure Assessment (SOFA) score was measured the same day after the PCT examination or the day after. Where individual components of SOFA score were missing, no contribution was made to the total score (eg, equivalent to assigning 0 or imputing a normal value). The SOFA value used is the daily maximum SOFA score, which is the highest score for each parameter in the measurement period.5 Mortality was assessed from the patient’s life/death status, which was seen from the incidence of mortality within 28 days after being admitted to the ICU divided into survivors and non-survivors. Morbidity was assessed by the degree of organ dysfunction described by the SOFA score. Sepsis was defined according to the Sepsis-3 criteria.
Microbiological cultures were taken during the treatment period and viewed based on electronic medical records. Pathogens were grouped into Gram-positive bacteria, Gram-negative bacteria, and fungal. The focus of infection was identified retrospectively taking into account all available clinical and microbiological data. History of comorbid disease was assessed by the Charlson comorbidity index (CCI) which assessed 19 diseases with a value of 0–33.6 Other data recorded were the type of ICU admission (medical/surgical) as well as a history of antibiotic use before procalcitonin examination.
Statistical Analysis
Descriptive analysis aims to describe the characteristics of the subjects and research variables as well as describe PCT levels in sepsis patients in the ICU. The results of the descriptive statistical analysis are presented in a cross-distribution table so that the comparability of the characteristics of the subjects between the groups is seen. The comparative analysis of proportions aims to compare the proportion of mortality and SOFA scores between the high PCT group and the low–moderate PCT group. The statistical test used to compare mortality is the Chi square test, resulting in a relative risk (RR) value. The statistical test used to compare the SOFA scores is the independent sample t-test. Cox proportional hazard regression analysis aims to assess the effect of high PCT on the occurrence of mortality and take into account SOFA scores and control for confounding variables. The measure obtained from this analysis is the adjusted relative risk (ARR). Conclusions are drawn with 95% Confidence Interval (CI) and p value at <0.05. All stages of data analysis above using the statistical software SPSS 26.
Results
Characteristics of Research Subjects
This retrospective cohort study involved 228 patients at high risk of developing sepsis obtained from 1 January 2018 to 31 December 2020. The average age of the overall patients is 53.61 years (Table 1). The majority of the patients were male with 134 patients (58.8%) while female patients amounted to 94 patients (41.2%). Medical ICU admissions were 121 patients (53.1%), while surgical ICU admissions were 107 patients (46.9%). The most common primary diagnoses in the ICU were infection/sepsis in 69 patients (30.3%). The 28-day mortality rate obtained in the entire patient was 57.5%, calculated from the first day the patient was admitted to the ICU. The length of stay of patients in the hospital is 2–92 days (mean 23.77 days), and the length of stay in the ICU is 1–85 days (mean 16.33 days).
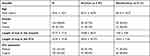 |
Table 1 Baseline Characteristics |
PCT levels of all patients with a minimum value of 0.03 and a maximum value of 567 (mean 44.62 ± 84.95) (Table 2). Patients who fall into the high PCT group category ≥7 ng/mL are 127 patients (55.7%) and patients who fall into the category of the low-moderate PCT group are 101 patients (44.3%). From the quick Sequential Organ Failure Assessment (qSOFA) score assessment, the minimum value is 0 and the maximum value is 3 (mean 2.45). SOFA score assessment obtained a minimum score of 2 and a maximum value of 17 (mean 7.1). From the CCI scores, the majority of patients had high comorbidity as many as 76 patients (33.3%). Before the PCT examination, the majority of the patients had received antibiotic therapy, 212 patients (93%) (Table 3). Based on data related to infection characteristics, the most common organ system as the focal infection was the lung in 198 patients (86.8%) and the majority of isolated organisms were Gram-negative bacteria in 211 patients (92.5%). Tables 1–3 show a comparison of data between the survivor and the non-survivor.
 |
Table 2 Procalcitonin and Score Distribution Among Survivor and Non-Survivor |
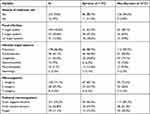 |
Table 3 Infection-Related Characteristics |
Relationship Between PCT Levels and Mortality
Bivariate analysis was performed to compare 28-day mortality by PCT category with the Chi-square test. In the group with high PCT (≥7 ng/mL), 87 patients died within 28 days after ICU admission (68.5%) and 40 patients were alive (31.5%). From the group with low to moderate PCT (<7 ng/mL), 44 patients died within 28 days after ICU treatment (43.6%) and 57 patients were alive (56.4%). These differences showed that PCT ≥ 7 ng/mL had a strong correlation with the incidence of death within 28 days after ICU admission with RR 1.572, p value <0.001 (Table 4).
 |
Table 4 Comparison of the Proportion of 28-Day Mortality by PCT Category |
Multivariate analysis was performed with 28-day mortality as the dependent variable. The independent variable used was PCT levels ≥7 ng/mL. By using Cox regression analysis, even after controlling for confounding variables namely age, gender, history of antibiotic use, number of microorganisms, ICU status, CCI score; PCT level ≥7 ng/mL is a variable that correlates with 28-day mortality with an ARR of 1.555, p value 0.02 (95% CI 1.074–2.252) (Table 5).
 |
Table 5 The Results of Cox Regression Analysis of the Relationship Between PCT Levels and 28-Day Mortality After Controlling for Confounding Variables |
The Relationship Between PCT Levels with SOFA Score
An assessment of the morbidity aspect of sepsis was carried out by comparing the SOFA scores based on the PCT category. Using the independent sample t-test, the mean ± SD in the PCT group ≥7 ng/mL was 8.11 ± 3.3, and the mean ± SD in the PCT group <7 ng/mL was 5.83 ± 2.7. There was a significant difference in the mean SOFA score in the two groups of 2.279 with CI 1.497–3.060 and p value <0.001.
Discussion
Mortality as one of the endpoints of the disease course is a good and clear research benchmark for researching a disease. The use of short-term mortality or 28 days is the period most often used, especially in sepsis which is an acute critical illness. Current study strengthened the evidence of PCT utility in high-risk sepsis patients. 28-day mortality in sepsis patients in the ICU was 57.5%. This figure is similar to a retrospective multi-center study in Indonesia where 58.3% of 14,076 sepsis patients died.1
Based on several studies, several risk factors have a role in increasing mortality in sepsis patients. PCT level is a strong indicator of mortality because it describes the degree of inflammation experienced by the patient. Previous studies showed that PCT levels of 7 ng/mL had 2.6 times higher risk of death (p = 0.02).4 The results of multivariate analysis controlling for these factors that may affect mortality in sepsis showed that PCT levels of 7 ng/mL had a strong correlation with 28-day mortality, which was statistically significant. Patients with a PCT of 7 ng/mL had a 1.55-fold risk of death within 28 days of ICU admission, p-value of 0.02.
PCT is released by parenchymal cells, including liver, kidney, adipocyte, and muscle cells in response to toxins from bacteria, causing levels to increase (up to 5000 times) within 2 to 4 hours.7 The biological effects of PCT on the host immune system have not been fully elucidated. However, there are several effects of PCT studied, including increasing the expression of surface markers of neutrophils and lymphocytes (CD16 and CD14) which indicate the movement of intracellular secretory vesicles towards the cell surface, increasing the concentration of intracellular calcium ions that facilitate the host response, decreasing the phagocytic activity of neutrophils in a dose-dependent manner, causes a dose-dependent increase in inflammatory cytokines, increases the malfunction of neutrophils, lymphocytes, and macrophages, acts as a potent trigger of the inflammatory cascade, increases body temperature and locomotor activity, affects energy homeostasis of the hypothalamus and pituitary gland, increases vasodilation and decreases renal function and cardiovascular stability. These effects can affect the course of the disease in sepsis patients and are also associated with morbidity and mortality.8
In a previous study, old age had a higher risk of mortality (adjusted OR 1.05) and surgical patients had a lower risk (adjusted OR 0.35).9 There are differences in the results found in this study, variables such as age, history of antibiotic use, number of microorganisms that cause infection, and ICU status were not proven to be significant risk factors for mortality in 28 days of ICU treatment, p value >0.05. Comorbidity described by the CCI score was also not proven to be a risk factor for mortality at 28 days in line with the study by Huddle et al, where the CCI score only had a role in predicting mortality at 1 year in sepsis patients with an area under the curve (AUC) 0.71 (95% CI 0.61–0.81).10
In this study, there was no difference in the risk of mortality between men and women. Nasir et al reported an increased risk of mortality in male patients with an RR of 1.73.11 Animal studies showed that female have a better immune and cardiovascular response than male. However, several epidemiological studies have shown inconsistent results where there is no difference between the two genders, a higher risk for men, and a higher risk for women. Inconsistent results may stem from differences in study design, small number of research subjects, and wide sample selection. Based on the theory from previous studies, women with higher estrogen levels should have a lower risk of sepsis mortality. However, sepsis itself was found to trigger an increase in estradiol concentrations through the adrenal stress response and peripheral aromatase activity so estrogen may also have harmful pathological effects in sepsis.12
Morbidity in sepsis described by SOFA scores was compared by PCT category. Using the independent sample t-test, the mean ± SD in the PCT group ≥7 ng/mL was 8.11 ± 3.3, and the mean ± SD in the PCT group <7 ng/mL was 5.83 ± 2.7. There was a significant difference in the mean SOFA score between the two groups of 2.279 with 95% CI 1.497–3.060 and a p value <0.001. This is in line with that reported by Novita et al, where there is a significant correlation based on the Spearman correlation test between SOFA scores and PCT levels (r = 0.752, p value <0.0001).13
There are several limitations in this study. Firstly, the study design was retrospective, so there were some limitations that it could not evaluate several variables, such as a specific history of previous antibiotic use, as well as one of the parameters of the SOFA score that was not examined when the patient was undergoing treatment. This study only assessed PCT levels at one point, and did not assess trends in PCT-level changes and their relationship to outcomes.
In conclusion, high PCT levels have a higher risk of mortality at 28 days in sepsis patients in the ICU and higher PCT levels were associated with higher SOFA scores in sepsis patients. Age, gender, history of antibiotic use, number of microorganisms causing infection, and ICU status were not proven as statistically significant correlated variables. Further research is needed to determine the relationship between the trend of PCT values in the course of the disease and its relationship to the outcome, as well as other factors that may affect PCT and outcome in patients with sepsis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Khairul A, Purba R, Mariana N, Aliska G, Hadi S. The burden and costs of sepsis and reimbursement of its treatment in a developing country: an observational study on focal infections in Indonesia. Int J Infect Dis. 2020;96:211–218. doi:10.1016/j.ijid.2020.04.075
2. Pregernig A, Müller M, Held U, Schimmer BB. Prediction of mortality in adult patients with sepsis using six biomarkers: a systematic review and meta ‑ analysis. Ann Intensive Care. 2019;9(1). doi:10.1186/s13613-019-0600-1
3. Mustafić S, Brkić S, Prnjavorac B, Sinanović A, Porobić-Jahić H, Salkić S. Diagnostic and prognostic value of procalcitonin in patients with sepsis. Med Glas. 2018;15(2):93–100. doi:10.17392/963-18
4. Jain S, Sinha S, Sharma SK, et al. Procalcitonin as a prognostic marker for sepsis: a prospective observational study. BMC Res Notes. 2014;7(1):1–7. doi:10.1186/1756-0500-7-458
5. Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score — development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23(1). doi:10.1186/10.1186/s13054-019-2663-7
6. Stavem K, Hoel H, Skjaker SA, Haagensen R. Charlson comorbidity index derived from chart review or administrative data: agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017;9:311–320. doi:10.2147/CLEP.S133624
7. Puspitasari AC, Mawari A. Presepsin: new biomarker to evaluate empirical antibiotic therapy outcome in septic condition. Fol Med Indones. 2020;56(2):148–153. doi:10.20473/fmi.v56i2.21236
8. Al-masoodi R, Abdullah U, Jassim H, Harun A. Immunomodulation effect of procalcitonin. J Bacteriol Mycol. 2019;6(4):1108.
9. Sanderson M, Chikhani M, Blyth E, et al. Predicting 30-day mortality in patients with sepsis: an exploratory analysis of process of care and patient characteristics. J Intensive Care Soc. 2018;19(4):299–304. doi:10.1177/1751143718758975
10. Huddle N, Arendts G, Macdonald SPJ, Fatovich DM, Brown SGA. Is comorbid status the best predictor of one-year mortality in patients with severe sepsis and sepsis with shock? Anaesth Intensive Care. 2013;41(4):482–489. doi:10.1177/0310057X1304100408
11. Nasir N, Jamil B, Siddiqui S, Talat N, Khan FA, Hussain R. Mortality in sepsis and its relationship with gender. Pak J Med Sci. 2015;31(5):1201–1206. doi:10.12669/pjms.315.6925
12. Pietropaoli AP, Glance LG, Oakes D, Fisher SG. Gender differences in mortality in patients with severe sepsis and septic shock. Gend Med. 2010;7(5):422–437. doi:10.1016/j.genm.2010.09.005
13. Novita C, Maat S, Tambunan BA. Correlation of procalcitonin level with sepsis degrees based on SOFA score. Indones J Clin Pathol Med Lab. 2019;25(3):312–317. doi:10.24293/ijcpml.v25i3.1497
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
