Back to Journals » Clinical Epidemiology » Volume 10
Risk of pneumonia in patients with burn injury: a population-based cohort study
Authors Chan CH , Yang SF , Yeh HW, Yeh YT, Wang YH, Teng YH, Yeh CB
Received 3 May 2018
Accepted for publication 21 June 2018
Published 29 August 2018 Volume 2018:10 Pages 1083—1091
DOI https://doi.org/10.2147/CLEP.S172980
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Irene Petersen
Chi-Ho Chan,1 Shun-Fa Yang,2,3 Han-Wei Yeh,4 Ying-Tung Yeh,5–7 Yu-Hsun Wang,2 Ying-Hock Teng,8,9 Chao-Bin Yeh8,9
1Department of Microbiology and Immunology, Chung Shan Medical University, Taichung, Taiwan, Republic of China; 2Department of Medical Research, Chung Shan Medical University Hospital, Taichung, Taiwan, Republic of China; 3Institute of Medicine, Chung Shan Medical University, Taichung, Taiwan, Republic of China; 4School of Medicine, Chang Gung University, Taoyuan City, Taiwan, Republic of China; 5Graduate School of Dentistry, Chung Shan Medical University, Taichung, Taiwan, Republic of China; 6School of Dentistry, Chung Shan Medical University, Taichung, Taiwan, Republic of China; 7Department of Dentistry, Chung Shan Medical University Hospital, Taichung, Taiwan, Republic of China; 8Department of Emergency Medicine, School of Medicine, Chung Shan Medical University, Taichung, Taiwan, Republic of China; 9Department of Emergency Medicine, Chung Shan Medical University Hospital, Taichung, Taiwan, Republic of China
Background: Burns are the main cause of accidental injury, and pneumonia is a common respiratory disease in humans.
Aim: The purpose of this study was to investigate the relationship between burn injury and pneumonia.
Patients and methods: A nationwide population-based cohort study was conducted using data from the National Health Insurance Research Database in Taiwan. We identified and enrolled 2,893 subjects with burn injury, who were individually matched to 2,893 subjects in the comparison group by using the propensity score. Furthermore, we used a self-controlled case-series design to estimate the temporal association between burn injury and pneumonia.
Results: Exposure to burn injury revealed a higher risk of pneumonia than that to non-burn injury within 1 year. The Cox proportional hazards model revealed that, compared with the non-burn injury, burn injury yielded a 2.39-fold (95% CI=1.44–3.96) increase in risk of pneumonia. The exposure period of burn injury within 30 days showed 2.76-fold increase in risk of pneumonia (95% CI=1.44–3.96) compared with that in the baseline period.
Conclusion: Burn injury was associated with a significant increased risk of pneumonia, especially occurring within 30 days.
Keywords: burn injury, pneumonia, odds ratio
Background
Burns are one of the major causes of traumatic injury in humans.1 The etiology of burn injury is diverse, including injury from fire, boiling water, and electricity. Skin burns can be classified into three categories according to severity.2 A first-degree burn involves injury to the epidermis, which may extend to the partial separation of epidermal and dermal layers. A second-degree burn extends injury to the entire epidermis and also to various parts of the dermis. A third-degree burn involves destruction of the entire epidermis and dermis and even damage to adipose tissue.2,3 Not only do burns affect skin tissue on the body’s surface, they can also induce pulmonary changes.4 In an animal study, a burn injury covering 40% of the body surface area induced pulmonary microvascular dysfunction.4 In another study, a serious burn increased pulmonary vascular permeability and decreased the PaO2:FiO2 ratio.5
Pneumonia is a common respiratory infectious disease that involves the inflammation of the pulmonary parenchyma. Individuals can acquire pneumonia on the basis of various epidemiologies, pathogeneses, and risk factors. For example, community-acquired pneumonia can occur anywhere outside hospitals, such as households, schools, and work places.6 By contrast, hospital-acquired pneumonia (HAP) can occur in hospitalized patients and outpatients.7 Moreover, HAP occurs 48 hours or more after hospitalization and does not present on admission. For hospitalized patients, HAP can be divided into ventilator hospital-acquired pneumonia (V-HAP), in which pneumonia develops after endotracheal intubation over 48–72 hours, and nonventilator hospital-acquired pneumonia (NV-HAP).7,8 A similar pathogenesis may exist in patients with burn injury. Repeat hospitalization might be another risk for burn injury patients, especially the older patients, to acquire pneumonia. These patients were admitted to hospitals for many reasons such as wound coverage, sepsis, and rehabilitation. Respiratory infection was one of most diagnosis in the 30-days re-hospitalization.9 Therefore, it is reasonable to expect that patients with burns have a higher risk of developing pneumonia, especially HAP. The etiologies of pneumonia include bacteria, viruses, fungi, and protozoa. For immunocompromised patients, pneumonia can be easily acquired when patients are exposed to pathogens from the air or opportunistic microbes that colonize in the buccal cavity or upper respiratory tract.10 A similar pathogenesis may exist in patients with burn injury.
Pneumonia is a general clinical presentation of the respiratory system, whereas burns are always related to extensive cutaneous injury. Indeed, lung function was unable to be restored completely in burn patients, while burn injury led to impaired immune system and increased susceptibility to infectious complication.11–13 It is rational to expect that burn injury patients may have a higher risk to develop pneumonia. However, systemic study of the relationship between pneumonia and burn injury and the interaction between symptoms remains limited. It would be valuable to know whether burn injury increases the risk of pneumonia. We hypothesized that patients with burn injury have a higher risk of developing pneumonia than the non-burn injury patients.
Patients and methods
Study population
The Longitudinal Health Insurance Database (LHID) is managed by the Taiwan National Health Research Institutes and contains data from one million randomly sampled beneficiaries, featuring all outpatient and inpatient medical claims, including drug medications, medical operations, procedures, and fees. Moreover, the LHID does not hold any identifying patient data. The study was approved by the ethical review board of the Chung Shan Medical University Hospital (CSMU No.: 15061).
Study design
This study used a retrospective cohort design. Patients aged ≥18 years with burn injury (ICD Ninth Revision Clinical Modification [ICD-9-CM] codes 940–949) which required emergency skin wound treatment or hospitalization were recruited between January 1, 2010, and December 31, 2012. The index date was defined as the first date of the burn injury. To avoid the confounding of disease history, we excluded patients who received a diagnosis of pneumonia within half a year before the index date.
A comparison group of patients who had not suffered from burn injury between 2009 and 2013 was selected. First, we performed a 1:18 age and sex matching to provide an index date corresponding to the comparison group. During matching, we excluded patients who received a diagnosis of pneumonia before the index date. Second, a propensity score matching (1:1) was performed for the comparison group according to age, sex, hypertension (ICD-9-CM codes 401–405), hyperlipidemia (ICD-9-CM codes 272.0–272.4), diabetes mellitus (ICD-9-CM codes 250), cerebrovascular disease (ICD-9-CM codes 430–438), renal disease (ICD-9-CM codes 582–582.9, 583–583.7, 585, 586, 588–588.9), liver disease (ICD-9-CM codes 571.2, 571.5, 571.6, 571.4–571.49, 572.2–572.8, 456.0–456.21), chronic pulmonary disease (ICD-9-CM codes 490–496, 500–505, 506.4), and ischemic heart disease (ICD-9-CM codes 410–414). All diseases were defined as having been diagnosed 1 year before the index date.
Outcome measurement
The outcome was the occurrence of pneumonia (ICD-9-CM codes 481, 482, 483, 485, 486) diagnosed during an emergency visit or hospitalization. All patients were traced until the occurrence of pneumonia within 1 year after the index date, withdrawal from the social insurance system, or the end of 2013, whichever came first. Furthermore, we used the proportion of BSA to distinguish the effects of different types of burn injury on pneumonia.
In order to estimate the temporal association between burn injury and pneumonia, we used a self-controlled case-series design to verify it.14 Patients with new diagnosis of pneumonia between January 1, 2010, and December 31, 2013 were recruited. We defined the exposure period as the interval of 30 days after burn injuries. The unexposed periods in the 4-year study were defined as the baseline period. Finally, we identified 151 patients with pneumonia that occurred before and after burn injury (Figure S1).
Statistical analyses
The comparison between burn injury and non-burn injury was performed using a chi-squared test or independent t-test, as appropriate. The cumulative incidence of pneumonia was performed using Kaplan–Meier analysis. The Cox proportional hazards model was used to estimate the hazard ratios of burn injury. The incidence rate ratio (IRR) of pneumonia in the exposure period compared with the baseline period was performed using a conditional Poisson regression. Statistical analyses were performed using SPSS V.18.0 (SPSS Inc., Chicago, IL, USA) and Stata V.12.0 (StataCorp LP, College Station, TX, USA).
Results
Characteristics of study patients
A total of 2,893 individuals with burn and the same number of individuals with non-burn between 2009 and 2013 were selected based on our inclusion and exclusion criteria (Figure 1). After matching, the mean values of age, sex, and comorbidities were similar between the groups. Before the unmatched comparison of burn injury and non-burn injury, the patients with burn injury exhibited higher risks of the following comorbidities: hypertension, hyperlipidemia, diabetes, myocardial infarction, and chronic pulmonary diseases (Table 1). The median and interquartile range (IQR) of time to pneumonia in the burn injury group were 164 and 84–295 days, respectively. The types of pneumonia are analyzed in Table S1.
  | Figure 1 Flow chart for burn injury patient’s selection. Abbreviations: LHID, Longitudinal Health Insurance Database; ICD-9-CM, ICD Ninth Revision Clinical Modification. |
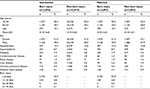  | Table 1 Demographic characteristics of burn injury and non-burn injury Abbreviation: BSA, burn surface area. |
Risk of pneumonia and exposure to burn injury
We estimated the cumulative incidence of pneumonia cases that were exposed to burn injury. The curve of exposure for burn injury revealed a higher risk of pneumonia than that for non-burn injury (Figure 2). The Cox proportional hazards model revealed a 2.39-fold increased risk of pneumonia for burn injury compared with that for non-burn injury (Table 2). For the different subgroups of age, the risk of pneumonia also increased 1.72-fold for patients aged 40–65 years and 9.97-fold for those aged ≥65 years, when compared with patients aged 18–40 years. In addition, male patients had a 1.83-fold higher risk of pneumonia compared with female patients. An increased risk of pneumonia with the following comorbidities was also noted: diabetes (adjusted hazard ratio [aHR]=2.58, 95% CI 1.44–4.64), cerebrovascular disease (aHR=2.75, 95% CI 1.42–5.31), and liver disease (aHR=2.55, 95% CI 1.15–5.65; Table 2). In addition, when the patients were categorized into two groups according to burn surface area (BSA; ≤10% and >10%), the group with BSA ≤10% displayed a high risk of acquiring pneumonia (aHR=2.36, 95% CI 1.41–3.93). When BSA was >10%, the risk of acquiring pneumonia became higher in trend (aHR=3.01, 95% CI 0.89–10.17).
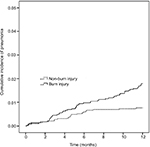  | Figure 2 Kaplan–Meier curves of the occurrence of pneumonia in burn injury patients. |
  | Table 2 Cox proportional hazards model of pneumonia and exposure to burn injury Abbreviations: HR, hazard ratio; BSA, burn surface area. |
Risk of pneumonia among patients with and without burn injury and subgroup-specific characteristics
We performed subgroup analysis between the burn injury group and the non-burn injury group. An increased risk of pneumonia was statistically observed in the burn injury group for patients aged ≥65 years (2.06-fold). An increased risk of pneumonia was also observed in male patients in the burn injury group (2.96-fold). Furthermore, an increased risk of pneumonia was observed with the comorbidities of ischemic heart disease in the burn injury group (Table 3).
Temporal association between burn injury and pneumonia
For the self-controlled case-series population, the IRR of pneumonia of exposure period ≤30 days was 2.76-fold (95% CI=1.44–3.96) compared with that of the baseline period. The IRR within the exposure period between 31 and 60 days was 1.51-fold (95% CI=0.74–3.07), and the IRR within the exposure period between 61 and 90 days was 1.79-fold (95% CI=0.92–3.50; Table S2).
Discussion
Patients with varying degrees of burn injury were recruited for observation of the risk of pneumonia within 1 year (2010). We observed that patients with burn injury were more likely to acquire pneumonia after recovery from burns. Although pneumonia was reported as a major complication in burn injury,15 the present study is the first to indicate an increased risk and frequency of acquiring pneumonia after a burn injury. Burn injury exacerbates the destruction of the respiratory system and increases mortality rate.15 The BSA percentage of burn injury also caused pneumonia in hospitalized patients. In one study, 27 out of 56 patients who had severe burn injury developed pneumonia.16 Face and neck burns were also risk factors of respiratory infection, which developed into pneumonia. Inhalation injury and endotracheal intubation were associated with respiratory infection during hospitalization.17
Burn injury can cause several sequelae, which can be affected by psychiatric or physiologic factors such as age and sex. In our study, the risk of pneumonia increased for male patients and those aged ≥65 years. Moreover, regarding the functional sequelae of burn injury, certain organs could not recover to their original function. For example, orofacial contractures after severe head and neck burns affect the ability to swallow.18 Therefore, rehabilitation is required to reduce the swallowing impairment. Another burn sequela is heterotopic ossification (HO), which appears in the joints of limbs.19 HO affects the flexible movement of limbs and requires surgery to excise pathologic bone tissue. The formation of HO was associated with the activation of both T- and B-lymphocytes in an animal study.20 Osteomyelitis was reported in children with burn injury who were infected with fungi in their bone tissue.21 A key study that agreed with ours indicated that patients who survived severe burn injury found it difficult to regain healthy lung function.11 These findings might explain our result of burn injury patients having a higher risk of pneumonia.
The total burn surface area (TBSA) was correlated with symptoms of acute respiratory distress syndrome (ARDS), inhalation injury, and sepsis.22 Similarly, patients with inhalation injury exhibited high TBSA, pneumonia, ARDS, and mortality rates.23 Conversely, a reduction in burn-induced inflammation could improve pulmonary function and survival.24 In our study, we categorized patients with burn injury into two groups (BSA ≤10% and BSA >10%). Obviously, the group with a BSA of ≤10% displayed a high risk of acquiring pneumonia. aHR even increased furtherly in the group with BSA >10%. This result implied that BSA has a positive relationship with getting pneumonia.
In burn injury, pathogens including bacteria, viruses, and fungi can infect respiratory tissue through two major routes. One is from mechanical therapy, such as ventilation and endotracheal intubation. The second is the bloodstream.25 Early pathogenic colonization in acute burn wounds may also influence infection rate.26 In addition, deep burns promote the risk of developing an infection.27 In a study, a high level of blood glucose elevation was discovered in patients with severe burn injury, which suggested that airway secretion also contained a high concentration of glucose. The secretion acted as a culture medium for bacteria growth and promoted respiratory infection.28 This might explain why infection of the respiratory tract was established more easily in patients with burn injury. Risk factors for the development of pneumonia in elderly patients with burn injury were sex, high TBSA, and existing comorbidities.29 In our study, patients aged 40 years or older had a higher risk of acquiring pneumonia. This finding was consistent with the aforementioned report that stated that aging was a crucial risk factor for patients with burn injury.30
Our study had some limitations. First, although smoke inhalation injury is also a complication of burn injury – especially in fire burns – it was excluded in our study because the insufficient number of cases might have led to underestimation of the odds ratio of pneumonia for burn injury exposure. Second, the database used did not contain information regarding patients’ clinical presentations of the severity of their pneumonia, laboratory data, or microbiological culture data that might affect pneumonia occurrence. Third, Taiwan’s National Health Insurance system is based on the Taiwanese population and our data accurately reflect the situation in Taiwan. Therefore, our results may not be applicable to Western populations. Fourth, we did not have access to potentially relevant personal behavioral information, such as smoking, alcohol consumption, and body mass index. These confounding factors might have influenced the results.
Conclusion
Burn injury patients were highly associated with an increased risk of pneumonia. Aging and BSA were another vital risk factor of pneumonia. Especially, the potential risk of pneumonia could be observed in burn injury, which refers to pneumonia which occurred within 30 days.
Acknowledgments
This study was partly based on data from the National Health Insurance Research Database (NHIRD) provided by the NHI Administration, Ministry of Health and Welfare, and managed by the National Health Research Institutes (registration number: NHIRD-104–148). The interpretation and conclusions contained herein do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare, or National Health Research Institutes. Also, this study was supported by research grants from “Association For Dental Sciences of the Republic of China”. The funders had no role in the study design data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14(5):R188. | ||
Lee KC, Joory K, Moiemen NS. History of burns: the past, present and the future. Burns Trauma. 2014;2(4):169–180. | ||
Iyoho A, Ng L, Chan P. The development of a probabilistic dose-response for a burn injury model. Mil Med. 2017;182(S1):202–209. | ||
Rothenbach PA, Dahl B, Schwartz JJ, et al. Recombinant plasma gelsolin infusion attenuates burn-induced pulmonary microvascular dysfunction. J Appl Physiol. 2004;96(1):25–31. | ||
Johansson J, Steinvall I, Herwald H, Lindbom L, Sjöberg F. Alteration of leukocyte count correlates with increased pulmonary vascular permeability and decreased PaO2:FiO2 ratio early after major burns. J Burn Care Res. 2015;36(4):484–492. | ||
Kolditz M, Ewig S. Community-acquired pneumonia in adults. Dtsch Arztebl Int. 2017;114(49):838–848. | ||
Giuliano KK, Baker D, Quinn B. The epidemiology of nonventilator hospital-acquired pneumonia in the United States. Am J Infect Control. 2018;46(3):322–327. | ||
Phu VD, Nadjm B, Duy NHA, et al. Ventilator-associated respiratory infection in a resource-restricted setting: impact and etiology. J Intensive Care. 2017;5:69. | ||
Mandell SP, Pham T, Klein MB. Repeat hospitalization and mortality in older adult burn patients. J Burn Care Res. 2013;34(1):e36–e41. | ||
Wong JL, Evans SE. Bacterial pneumonia in patients with cancer: novel risk factors and management. Clin Chest Med. 2017;38(2):263–277. | ||
Mlcak R, Desai MH, Robinson E, Nichols R, Herndon DN. Lung function following thermal injury in children – an 8-year follow up. Burns. 1998;24(3):213–216. | ||
Kobayashi M, Takahashi H, Sanford AP, Herndon DN, Pollard RB, Suzuki F. An increase in the susceptibility of burned patients to infectious complications due to impaired production of macrophage inflammatory protein 1 alpha. J Immunol. 2002;169(8):4460–4466. | ||
Stanojcic M, Chen P, Xiu F, Jeschke MG. Impaired immune response in elderly burn patients: new insights into the immune-senescence phenotype. Ann Surg. 2016;264(1):195–202. | ||
Petersen I, Douglas I, Whitaker H. Self controlled case series methods: an alternative to standard epidemiological study designs. BMJ. 2016;354:i4515. | ||
Chen MC, Chen MH, Wen BS, Lee MH, Ma H. The impact of inhalation injury in patients with small and moderate burns. Burns. 2014;40(8):1481–1486. | ||
de La Cal MA, Cerdaé E, Garciéa-Hierro P, et al. Pneumonia in patients with severe burns. Chest. 2001;119(4):1160–1165. | ||
Costa Santos D, Barros F, Gomes N, Guedes T, Maia M. Face and/or neck burns: a risk factor for respiratory infection? Ann Burns Fire Disasters. 2016;29(2):97–102. | ||
Clayton NA, Ward EC, Maitz PK. Intensive swallowing and orofacial contracture rehabilitation after severe burn: a pilot study and literature review. Burns. 2017;43(1):e7–e17. | ||
Manske MC, Hanel DP. Postburn contractures of the elbow and heterotopic ossification. Hand Clin. 2017;33(2):375–388. | ||
Ranganathan K, Agarwal S, Cholok D, et al. The role of the adaptive immune system in burn-induced heterotopic ossification and mesenchymal cell osteogenic differentiation. J Surg Res. 2016;206(1):53–61. | ||
Rosanova MT, Voto C, Carnovale S, et al. Osteomyelitis in burn children: ten years of experience. Arch Argent Pediatr. 2018;116(1):59–61. | ||
Steinvall I, Bak Z, Sjoberg F. Acute respiratory distress syndrome is as important as inhalation injury for the development of respiratory dysfunction in major burns. Burns. 2008;34(4):441–451. | ||
Monteiro D, Silva I, Egipto P, et al. Inhalation injury in a burn unit: a retrospective review of prognostic factors. Ann Burns Fire Disasters. 2017;30(2):121–125. | ||
Ipaktchi K, Mattar A, Niederbichler AD, et al. Attenuating burn wound inflammation improves pulmonary function and survival in a burn-pneumonia model. Crit Care Med. 2007;35(9):2139–2144. | ||
Devrim İ, Kara A, Düzgöl M, et al. Burn-associated bloodstream infections in pediatric burn patients: time distribution of etiologic agents. Burns. 2017;43(1):144–148. | ||
Park HS, Pham C, Paul E, Padiglione A, Lo C, Cleland H. Early pathogenic colonisers of acute burn wounds: a retrospective review. Burns. 2017;43(8):1757–1765. | ||
Ramirez-Blanco CE, Ramirez-Rivero CE, Diaz-Martinez LA, Sosa-Avila LM. Infection in burn patients in a referral center in Colombia. Burns. 2017;43(3):642–653. | ||
Kraft R, Herndon DN, Mlcak RP, et al. Bacterial respiratory tract infections are promoted by systemic hyperglycemia after severe burn injury in pediatric patients. Burns. 2014;40(3):428–435. | ||
Pham TN, Kramer CB, Klein MB. Risk factors for the development of pneumonia in older adults with burn injury. J Burn Care Res. 2010;31(1):105–110. | ||
Rani M, Schwacha MG. Aging and the pathogenic response to burn. Aging Dis. 2012;3(2):171–180. |
Supplementary materials
  | Table S1 Type of pneumonia event |
  | Table S2 IRR for pneumonia after burn injury occurred Note: *P<0.001. Abbreviation: IRR, incidence rate ratio. |
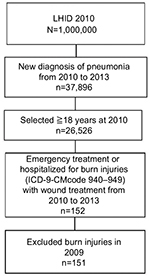  | Figure S1 Flow chart for study selection of Self Controlled Case Series. Abbreviations: LHID, Longitudinal Health Insurance Database; ICD-9-CM, ICD Ninth Revision Clinical Modification. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

