Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Risk Factors of Antepartum Hemorrhage Among Mothers Who Gave Birth at Suhul General Hospital, 2016: A Case–Control Study
Authors Dibaba B , Edosa D , Hajure M , Gebre G
Received 28 June 2020
Accepted for publication 21 December 2020
Published 4 February 2021 Volume 2021:14 Pages 271—278
DOI https://doi.org/10.2147/JMDH.S269744
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Bekem Dibaba,1 Dejene Edosa,1 Mohammedamin Hajure,2 Gelawdiwos Gebre3
1Midwifery Department, Public Health and Medical Sciences, Mettu University, Mettu, Ethiopia; 2Psychiatry Department, Public Health and Medical Sciences, Mettu University, Mettu, Ethiopia; 3Midwifery Department, Public Health and Medical Sciences, Mekele University, Mekele, Ethiopia
Correspondence: Bekem Dibaba Email [email protected]
Background: Antepartum hemorrhage is a very serious problem and contributes significantly to maternal and neonatal morbidity and mortality in developing countries including Ethiopia. Identification of risk factors of antepartum hemorrhage will help for prevention and control programs.
Methods: An institutional-based case–control study was conducted from July 2013 to June 2016. A simple random sampling technique was employed, and 420 mothers’ medical cards were reviewed using a pretested checklist. The data were entered in to EPI-info version 7 and then exported to SPSS version 20 for analysis, and all variables with a P-value< 0.2 at bivariate logistic regression analysis were considered as a candidate for multivariate logistic regression analysis, and those variables with a P-value< 0.05 in multiple logistic regression analysis were considered as significantly associated at 95% confidence interval.
Results: Results of the multiple logistic regression showed that those mothers whose age was in the range of 35– 44 years were significantly 4-times more likely to present with antepartum hemorrhage as compared to mothers in the age range of 15– 24 years. Moreover, mothers who presented with a previous history of cesarean section were 4.7-times more likely to present with antepartum hemorrhage than those who had no previous history of cesarean section. Furthermore, women with a previous history of abortion were 2-times more likely to develop antepartum hemorrhage as compared to women who had no previous history of abortion.
Conclusion and Recommendation: In this study, the factors found to be risk factors of antepartum hemorrhage were maternal age, previous history of cesarean section, and previous history of abortion. Strategies towards reduction of unwanted pregnancy to prevent abortion, pregnancy at advanced age, and to reduce the cesarean section rate should be emphasized.
Keywords: antepartum hemorrhage, risk factors, Suhul, Tigrai, Ethiopia, 2016
Introduction
Antepartum hemorrhage (APH) is one of the leading causes of obstetrical hemorrhage and maternal death and also a major cause of perinatal morbidity and mortality worldwide. A study conducted at Medical College, Mysore, India showed that, in spite of a lot of improvement in the form of antenatal care and intrapartum surveillance, antepartum hemorrhage has not reduced. It still continues to constitute a major portion of obstetrical hemorrhage.1
Antepartum hemorrhage (APH) is very serious and one of the most frequent obstetrical emergencies, and is the most common preventable cause of maternal death, responsible for 25–60% of maternal mortality. Antepartum hemorrhage occurs without warning signs. Thus there is a need to identify the risk factors associated with antepartum hemorrhage to help obstetricians in the early diagnosis and treatment. These risk factors include previous APH, previous cesarean section, advanced maternal age (age greater than 35), urban/rural residence, previous termination of pregnancy (curettage), pregnancy-induced hypertension (PIH), multi-parity, and multiple pregnancy.2
In developing countries like India, women frequently experience adverse effects of obstetric hemorrhage due to widespread pre-existing anemia, difficulties with transport, and overwhelming inadequacies of maternity services.3
A case–control study conducted in Nigeria showed that the main causes of antepartum hemorrhage were placenta previa (55.6%), abruption placenta (33.3%), and unknown cause (8.4%). Antepartum hemorrhage contributes significantly to maternal and neonatal morbidity and mortality in sub-Saharan Africa.4
Antepartum hemorrhage could be prevented by early registration, regular antenatal care, early detection of high risk cases, and early referral to a higher center. Good facilities for cesarean section, availability of blood banks, and use of contraceptives can improve maternal and perinatal outcome of APH.5
A study conducted at Jimma university specialized hospital revealed that APH, primarily caused by abruption placenta and placenta previa, is a common complication of pregnancy and cause of maternal and perinatal mortality. The risk of adverse maternal and newborn outcomes including maternal mortality, perinatal mortality, and low birth weight is higher among APH cases in Jimma University Specialized Hospital compared to reports from other countries. Efforts to improve geographical access, referral services, and quality of comprehensive emergency obstetric care are needed to improve maternal and newborn outcomes in Ethiopia.6
Vaginal bleeding after mid-pregnancy is associated with maternal and fetal risks. Maternal morbidity may be caused by acute hemorrhage and operative delivery, and the fetus may be compromised by uteroplacental insufficiency and premature birth.7
More than 99% of all maternal deaths occur in the developing world and the great majority of these are avoidable. Women continue to die unnecessarily in pregnancy and childbirth in these countries due to obstetrics complications, specifically APH. If we are serious about stopping these unnecessary maternal deaths, with the proper resources and implementation we can build a future for these communities. APH, irrespective of cause, increases prenatal morbidity and mortality, hence the condition demands full investigation and careful management.8
Effective management of vaginal bleeding in late pregnancy requires recognition of potentially serious conditions, accurate and timely identification of the cause of bleeding, the team system or approach, which optimizes women’s safety, and well-timed intervention specific to diagnosis.9
Women with a history of APH are at increased risk for adverse perinatal outcomes including small for gestational age and growth restricted fetuses, therefore initiation of serial ultrasounds is recommended.10
This study, conducted at Jimma University specialized hospital, focused only on adverse maternal and newborn outcomes of abruption placenta and placenta previa and complications of APH rather than finding the risk factors contributing to APH, which is very important to identify the mothers at high risk to develop antepartum hemorrhage.
Objective
The objective of this study was to identify the risk factors of antepartum hemorrhage among women who gave birth at Suhul general hospital during the period of 2013–2016, north western Tigray: A case–control study.
Methods and Materials
Study Area and Period
The study was conducted at Suhul Hospital from June–July 2016 which is a general public hospital located in Shire Endasselassie town situated 301 kilometers from Mekelle and 1,087 kilometers from Addis Ababa in the North Western part of Tigray region in Ethiopia.
Study Design
An institutional-based case–control study was conducted.
Source Population
All cards of mothers who gave birth at Suhul general hospital. Cases: All cards of delivered mothers who developed APH during the period of 2013–2016. Controls: All cards of delivered mothers who did not developed APH during the period of 2013–2016.
Study Population
Cases: Randomly selected cards of delivered mothers who developed APH during the period of 2013–2016.
Controls: Randomly selected cards of delivered mothers who did not develop APH during the period of 2013–2016.
Eligibility Criteria
Inclusion and Exclusion Criteria
All mothers’ cards that contain full information needed for the study (the card which contains all variables used in the study) were included. Mothers who were registered on the log book but whose cards were missed and mother’s card with an unknown gestational age were excluded.
Sample Size Calculation, Techniques, and Procedures
Sample size was determined by two population proportions by EPI-info version 7 using 95% CI, 80% power, and sn odds ratio of 2.443 taken from a study conducted at Ladoke Akintola University of Technology (LAUTECH) Teaching Hospital, southwestern Nigeria, which shows that un-booked mothers were significantly more likely to present with antepartum hemorrhage, 66.7% (OR=2.443, 95% CI=1.030–5.794), and in the control exposed group those significantly at higher risk of having antepartum hemorrhage were 42.9% (OR=2.443, 95% CI=1.030–5.794), a 1:2 ratio of cases to controls. Accordingly the total of 420 cards, 140 cases, and 280 controls were included in the study.
The card numbers of both cases and controls were identified from a egistration book of those registered during the past 3 years, from July 2013 to June 2016. Accordingly 317 cases and 5,343 controls were identified. All cards were reviewed to check their completeness with information needed in the study. Mothers’ cards with APH (cases) which fulfilled the inclusion criteria used for their completeness were 283, 29 cards were incomplete, and five cards were missed and were excluded. Similarly the cards of the control group were checked for their completeness and 4,821 cards were complete and 522 cards excluded (503 cards for their incompleteness and 19 cards were missed). Then 283 cards of cases and 4,821 cards of controls were coded and entered into SPSS version 20 to select cards included in the study randomly (by computer generated simple random sampling).
Data Collection Procedure, Period, and Quality Control
The data was collected from August 1 to September 30, 2016 using mothers’ clinical records by a structured data collecting checklist which was developed from different literature. This structured checklist was prepared in English and tested before the actual data collection. The data was collected by two midwives who were oriented for 1 day before data collection on the proper application of the data collection tool. Data quality was ensured during data collection, coding, entry, and analysis. A pre-tested structured checklist was used. Orientation was given for the data collectors to prevent any confusion and have a common understanding about the study, provision of full information, and appropriate documentation. Supervision of data collectors included observation of how the data collectors collect data, and was done by the principal investigator.
Study Variables
Dependent variable: Antepartum hemorrhage.
Independent variables: Socio demographic characteristics (Maternal age, Residence).
Obstetrics characteristics during admission: Antenatal care, Pregnancy induced hypertension, Parity, Number of fetuses, Polyhydramnios, Amniocentesis, Macrosomia, Premature Rapture of Membrane, Chorioamnits, early pregnancy vaginal bleeding, Accident Trauma.
Previous obstetrics history: previous history of antepartum hemorrhage, prior cesarean section, previous termination of pregnancy curettage, previous pregnancy induced hypertension.
Data Analysis and Management
Data were coded and entered to EPI Info version 7, then exported to SPSS version 20 for analysis. Both descriptive and analytical statistical procedures were utilized. Descriptive statistics like percentage, mean and standard deviation were used for the presentation of demographic data and obstetrics factors. Tables and graphs were also used for data presentation.
Binary logistic regression was used to identify factors associated with antepartum hemorrhage. Associations between antepartum hemorrhage and socio-demographic and obstetrics factors were explored using bivariate and multivariate logistic regression. Multivariate logistic regression analysis was applied to investigate associated factors through stepwise adjustment. The variables were entered into the multivariate model using the forward Stepwise regression method.
All variables with a P-value<0.2 at bivariate logistic regression analysis were considered as a candidate for multiple logistic regression analysis and those variables with a P-value<0.05 in multiple logistic regression analysis were considered as significantly associated factors with antepartum hemorrhage. The degree of association between independent and dependent variables was assessed using an odds ratio with 95% confidence interval.
Operational Definition
Antepartum hemorrhage: Antepartum hemorrhage (APH) is defined as bleeding from or into the genital tract, occurring from 28 weeks of pregnancy and prior to the birth of the baby.
Card with incomplete information: Card which had no full information about mother’s pregnancy condition and past obstetric history (when one or more variables used in the study were missed).
Missed Card: Mother’s medical card which was not available on the shelf of the card room during the data collection period.
Unknown gestational age: No written gestational age on mother’s medical card because the mother did not remember her last menstrual period to calculate gestational age.
Results
Socio-Demographic Characteristics of Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH During the Period of 2013–2016
The mean (SD) age among the cases was 29.76 (±7.19) years (range=17–44), and among the controls was 27.55 (±6.28) years (range=17–44). Most of the women who presented with antepartum hemorrhage (cases) (78, 55.7%) were from out of Shire town and the remaining were from Shire town; and from the control group, 166 (59.3%) were living in Shire town and 114 (40.7%) were living out of Shire (Table 1).
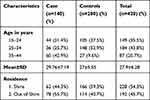 |
Table 1 Socio-Demographic Characteristics of Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH During the Period of 2013–2016 (n=420) |
Obstetrics Characteristics of Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH During the Period of 2013–2016
Among women who had antepartum hemorrhage (cases), 58 (41.43%), and among controls, 49 (17.5%) were grand multiparous. Among the study subjects, the majority of both cases and controls had ANC follow-up; 133 (95%) of cases and 266 (95%) of controls.
Among the study subjects, 67 (49.9%) of the cases and 60 (21.6%) of the controls were diagnosed by ultrasonography during their ANC follow-up. The number of women with antepartum hemorrhage (cases) and controls that developed vaginal bleeding during early pregnancy were 14 (10%) and 11 (3.9%), respectively.
Among mothers presented with antepartum hemorrhage (cases), six (4.3%) presented with blunt abdominal trauma, as did four (1.4%) of the controls.
Among the study subjects, 10 (7.1%) mothers with APH (cases) and 18 (6.4%) controls had premature rapture of membrane (PROM) during their admission, of which five (3.6%) f cases and nine (3.2%) controls had chorioamnionitis.
Regarding the number of fetuses, from the cases, 130 (92.9%) were singletons, 10 (7.1%), twins and from control group, 263 (93.9%) were singletons, 16 (5.7%) twins, and one (0.4%) was triplets.
REgarding pregnancy related disorders, 15 (10.7%) mothers with APH and 36 (12.9%) of the control group presented with pregnancy induced hypertension, and six (4.3%) cases and 12 (4.3%) of controls were diagnosed with polyhydramnios, from which only one (0.7%) of the cases and two (0.7%) of the controls were managed with amniocentesis.
Among the study subjects, 67 (49.9%) cases and 60 (21.6%) controls were diagnosed by ultrasonography during their ANC follow-up, and three (2.1%) women with APH and five(1.8%) controls were diagnosed with macrosomia. Among mothers with APH (cases), 76 (54.3%), and mothers without APH (controls), 26 (9.3%) were delivered at gestational age of <37 weeks (preterm birth) (Table 2).
 |
Table 2 Obstetric Characteristics of Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH at Admission During the Period of 2013–2016 |
Previous Obstetrics Characteristics of Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH During the Period of 2013–2016
Concerning other pre-existing maternal health problems, 11 (9.1%) mothers presented with APH (cases) and 27 (11.2%) mothers who were presented without APH (controls) complained of a previous history of pregnancy induced hypertension and 10 (8.3%) cases and 18 (7.5%) controls had a history of antepartum hemorrhage previously.
This study also demonstrated that 36 (25.7%) of the cases and 47 (16.8%) controls experienced previous history of abortion. Thirty-five (28.9%) mothers with APH and 20 (8.3%) of the controls had a history of previous cesarean section (see Table 3).
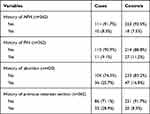 |
Table 3 Previous History of Obstetrics Characteristics of Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH During the Period of 2013–2016 |
Logistic Regression Analysis of Factors Associated with APH Among Mothers Who Gave Birth at Suhul General Hospital Who Had APH and Had No APH During the Period of 2013–2016
Variables considered for multiple logistic regression were those with a P-value<0.2 at bivariate logistic regression analysis and these included age, residence, previous history of abortion, parity, early pregnancy vaginal bleeding, and history of previous cesarean section.
During multiple logistic regression, advanced maternal age, previous history of abortion, and previous history of cesarean section delivery were significant risk factors for antepartum hemorrhage (Table 4).
Discussion
The finding of this study indicated that risk factors found to be associated with antepartum hemorrhage were advanced maternal age (≥35 years) (AOR=4.00, 95% CI=1.48–11.12), a history of previous cesarean section (AOR=4.70, 95% CI=2.29–9.69), and a history of previous abortion (AOR=2.00, 95% CI=1.08–3.46).
Results of the multiple logistic regression in this study showed that those mothers whose age was in the range of 35–44 years were significantly 4-times more likely to present with antepartum hemorrhage as compared to mothers in the age range of 15–24 years.
This is in agreement with studies done in India (Maharashtra & Medical College of Jodhpur), Nigeria, Iran, and Pakistan, which revealed that maternal age over 35 years was found to be a risk factor for antepartum hemorrhage.3,7,11,12 This is due to the fact that older maternal age may show an association with increased obstetric complications which may be secondary to reduced cardiovascular reserve, relatively high incidence of underlying medical disease, and also decreased ability to respond and adapt to the physical stress that accompanies aging. It also could be due to sclerotic changes on intra-myometrium arteries increases with increasing age, thereby reducing the blood supply to the placenta.2,3,7,11,12
Another risk factor of APH in this study was a previous history of cesarean section. Mothers who presented with previous history of cesarean section were 4.7-times more likely to present with antepartum hemorrhage than those who had no previous history of cesarean section.
This is comparable to the study in Grant Medical College and Sir JJ Group of Hospitals & Medical College, Jodhpur, India & Iran which has recently shown that the uterine scar of cesarean section prevented migration of the placenta during the course of pregnancy toward the more vascularized uterine fundus. Risk of placenta previa is highest in the pregnancy immediately following cesarean section. Failure of appropriate lower segment devolvement, because of scar tissue, could be a cause and raw area favorable for implantation. Incidence of placenta previa increases in a linear way with increasing number of previous cesarean sections.2,6,12
The findings of this study also confirmed another risk factor found to be associated with antepartum hemorrhage was previous history of abortion. This indicated that women with a previous history of abortion were 2-times more likely to develop APH as compared to women who had no previous history of abortion.
This is comparable to a studies conducted in Iran, Pakistan, and Sweden.11,12,13 The mechanism of how previous abortions predispose to APH development could be explained with possible endometrial damage during repeated abortions, which impedes successful fundal implantation of placenta.11,12,13
Limitations
The limitation of this study was the challenge to get adequate information concerning some variables. Using secondary data limits the study variables of socio-demographic characteristics such as religion, ethnicity, educational status, income, and occupation.
Conclusion
The finding of this study indicated that risk factors found to be associated with antepartum hemorrhage were advanced maternal age, previous history of abortion, and previous history of cesarean section.
Abbreviations
AOR, adjusted odds ratio; APH, antepartum hemorrhage; ANC, antenatal care; CI, confidence interval; CS, cesarean section; OR, odds ratio; PROM, premature rapture of membrane; SPSS, Statistical Package for Social Science.
Data Sharing Statement
Data sets used and examined in this study are obtainable from the corresponding author upon sound request.
Ethics Approval and Consent to Participate
The study was conducted following the 2013 revised Declaration of Helsinki and ethical clearance was gained from the ethical review committee of Mekele University, faculty of health and medical sciences. A letter of permission was obtained from the Midwifery department. Participants were communicated with about the purpose, risk, and benefits of the study and were invited to participate. Confidentiality was kept utmost and all related queries were responded to, and they provided written informed consent for participation.
Acknowledgments
The authors are grateful to Mekele University for providing ethical permission to undertake this study.
Funding
Ethiopian ministry of Education funded this study.
Disclosure
The authors state that they have no competing interests, financial or otherwise.
References
1. Nagapurkar S, Tale A, Ranjwan B. Risk factors for ante partum hemorrhage: a hospital based study. Int J Recent Trends Sci Technol. 2015;15(2):2277–2812.
2. Bhandiwad A, Abhishek A, Fadero B. Ante-partum hemorrhage and pregnancy outcome in LAUTECH Teaching Hospital, southwestern Nigeria. J Med Med Sci. 2011;2(12):1243–1247.
3. Naiknaware SV. Antepartum hemorrhage: causes & its effects on mother and child: an evaluation. Obstet Gynecol Int J. 2015;3(1).
4. Bhandiwad A, Bhandiwad AA. A study of maternal and fetal outcome in antepartum hemorrhage. J Evid Based Med Healthc. 2014;1(6):406–427. doi:10.18410/jebmh/2014/67
5. Maurya A. Dr. Sonal Arya study of antepartum hemorrhage & its maternal & perinatal outcome. Int J Sci Res. 2014;4(2):2250–3153.
6. Chufamo N, Segni H, Alemayehu YK. Incidence, contributing factors and outcomes of antepartum hemorrhage in Jimma University Specialized Hospital, Southwest Ethiopia. Univ J Public Health. 2015;3(4):153–159. doi:10.13189/ujph.2015.030403
7. Sakornbut E, Leeman L, Fontaine P. Management of late pregnancy bleeding. Am Fam Physicians. 2016;75(8):1199–1206.
8. Wolfson J. Obstetric haemorrhage in Gimbie, Ethiopia. Obstet Gynaecol. 2007;9:121–126. doi:10.1576/toag.9.2.121.27314
9. Sakornbut E, Leeman L, Fontaine P. Late pregnancy bleeding. Am Fam Physician. 2007;75(8):1199–1206.
10. Women KEMHf. Antepartum haemorrhage (APH) clinical guidelines: obstetrics & midwifery. Obstet Gynecol. 2015;2(3):1–2.
11. Naheed Rahim TR, Ara A. Risk factors associated with major placenta previa. J Med Sci. 2014;22(2):62.
12. Ghaheh HSFA, Mousavi M, Sohrabi D, Mesghari L, Mesghari L, Hosseini Z. Risk factors of placental abruption. J Res Med Sci. 2013;18:422–426.
13. Prochazka MLM, Slavik L, Hrachovec P. Selected pregnancy variables in women with placental abruption. Biomed Pap Med. 2006;150(2):271–273. doi:10.5507/bp.2006.040
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

