Back to Journals » Journal of Pain Research » Volume 16
Risk Factors for Short-Term and Long-Term Low Back Pain After Transforaminal Endoscopic Lumbar Discectomy
Authors Wang H, Zhou X, Li X, Xu Z, Meng Q, Wang J, Shen X, Chen H, Yuan W, Wu X
Received 13 June 2023
Accepted for publication 27 September 2023
Published 20 October 2023 Volume 2023:16 Pages 3505—3517
DOI https://doi.org/10.2147/JPR.S422595
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Krishnan Chakravarthy
Hui Wang,1,* Xiaonan Zhou,2,* Xingyu Li,1,* Zeng Xu,1,* Qingbing Meng,3 Jianxi Wang,1 Xiaolong Shen,1 Huajiang Chen,1 Wen Yuan,1 Xiaodong Wu1
1Department of Orthopedics, Shanghai Changzheng Hospital, Naval Medical University, Shanghai, People’s Republic of China; 2Department of Anesthesiology, Shanghai Changzheng Hospital, Naval Medical University, Shanghai, People’s Republic of China; 3Department of Orthopedics, Shanghai Zhongshan Hospital, Fudan University Shanghai School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Huajiang Chen; Xiaodong Wu, Email [email protected]; [email protected]
Introduction: Low back pain following transforaminal endoscopic lumbar discectomy (TELD) is prevalent (15– 25% incidence). Modifying TELD techniques to avoid excessive disc removal has been suggested to reduce such pain. Facet injury, re-herniation, and disc space collapse might contribute. This retrospective study aimed to explore factors linked to post-TELD low back pain.
Methods: A total of 351 patients with L3/4, L4/5, and L5/S1 intervertebral lumbar disc herniations, who underwent TELD at two spine centers, were included. Patients were followed for one year. Low back and leg pain visual analogue scale (VAS) scores, Oswestry Disability Index (ODI), Pfirrmann grade, and disc height were measured at 3 months and 1 year. Correlation analyses examined links between postoperative low back pain VAS scores, age, sex, disc/vertebrae height ratio (D/V H ratio), Pfirrmann grade, cannula position grade, re-herniation grade, high-intensity zone (HIZ), disc calcification, surgical grade, and other factors. Significant variables were identified using partial least square tests, with variable importance in projection (VIP) values quantifying their impact on low back pain.
Results: Univariate analysis indicated that surgical grade correlated with long-term postoperative low back pain (P = 0.023), while re-herniation (P = 0.008, P = 0.000), disc height (P = 0.001, P = 0.034), and sex (P = 0.025, P = 0.003) correlated with both short- and long-term postoperative low back pain. Trephine/cannula position is correlated with short-term low back pain (P = 0.036). Worsening low back pain was associated with female sex, improper trephine/cannula position, re-herniation, and post-surgical disc space collapse. Intradiscal irrigation was linked to decreased low back pain.
Discussion: This study highlights factors influencing low back pain after TELD. Loss of disc height, extent of re-herniation, quality of trephine/cannula position, and sex were associated with low back pain at both 3 months and 1-year post-TELD. Proper techniques, like minimizing disc height loss and re-herniation, may help mitigate postoperative low back pain.
Keywords: spine, endoscopy, radiology, minimally invasive surgical procedure, postoperative low back pain
Introduction
Low back pain is anatomically defined as pain from the 12th rib to the iliac crest, sometimes overlapping with discomfort extending from the iliac crest to the gluteal folds.1 Worldwide, low back pain stands as the second most prevalent contributor to adult disability.2 The occurrence of low back pain during one’s lifetime ranges from 54% to 80%,3 and the annual economic burden associated with this condition is estimated at approximately $100 billion on a national scale.4 The origins of low back pain encompass factors such as facet joint issues, osteoarthritis, strains in soft tissues, disc degeneration, Modic changes, instability, nerve compression, infections, and neoplasms.5
Transforaminal endoscopic lumbar discectomy is an effective procedure for intervertebral disc herniation and has been performed with good results for a long time. However, postoperative low back pain is a common complication after surgery. Postoperative low back pain can be linked to various factors, including paraspinal muscle injuries, recurrent disc herniation, epidural scarring, intervertebral disc collapse, facet joint arthritis, and injury to the posterior branch of the nerve root. Numerous anatomical structures are implicated in low back pain, with the posterior longitudinal ligament, nerve root, endplate, annulus fibrosus, and posterior nerve root branch being particularly sensitive pain sources during transforaminal endoscopic lumbar discectomy (TELD).6 Lantao Liu reported that compared with microscope-assisted tubular discectomy, TELD is expected to lead to less postoperative back pain.7 However, patients still had persistent low back pain (VAS ranged from 1.6 to 3) at follow-up,5 including pain at the central spinous process and pain radiating to the lateral gluteal side.
Recurrent disc herniation is a common cause of recurrent leg pain and reoperation after primary discectomy (incidence range, 7–24%).8 However, it is not clear whether recurrent disc herniation is associated with low back pain after TELD. Intradiscal normal disc removal has been reported to decrease re-herniation; however, it increases low back pain after discectomy. Pan reported that increased load bearing by the facets and misarrangement of the facet joint were associated with lateral buttock pain after discectomy.9 The precise amount of intradiscal nucleus pulposus removal cannot be controlled by forcep decompression. Wu initially reported that the use of intra-disc high-pressure irrigation instead of normal disc removal during decompression can control the amount of discectomy.10 Increasing the intradiscal pressure before decompression can ease loose disc removal and keep the firmly attached nucleus pulposus in place.
This study aimed to investigate whether this technique influences postoperative low back pain. The findings of this study shed light on the potential impact of intradiscal pressure manipulation on postoperative pain outcomes.
Methods and Materials
Study Design and Participants
This retrospective study was approved by Shanghai Changzheng hospital institutional review board (Registration number: 2022SL060). The study included 351 patients who were diagnosed with symptomatic lumbar disc herniation at one level with no prior surgery at any other spinal level and underwent TELD at two spine centers with a one-year postoperative follow-up (Table 1). All the patients had radiating pain to the lower limbs for a duration of one month to four months. Preoperative MRI showed one-level disc herniation compressed on the corresponding nerve root. The symptoms and physical signs were consistent with the involved segment and nerve root shown on MRI. The high-intensity zone at the herniation on T2 MRI and the type of herniation (contained, protruded, extruded or sequestered) were recorded. The exclusion criteria included more than two levels of discectomy; concomitant surgery in addition to TELD performed at the same or different levels; and evidence of stenosis, infection, fractures, or tumors.
 |
Table 1 Demographic of This Series of Patients |
Surgical Procedure
All surgeries were performed by two senior surgeons in the two hospitals. The two surgeries, nurses and other healthcare staff were trained in before this study. Local anesthesia was administered to the patients while they were positioned prone on a radiolucent table prior to the procedure, the surgical segment was verified using fluoroscopy, and a marker line was drawn to ensure accuracy. Throughout the entire surgical process, patient feedback was closely monitored to prevent any potential harm to neural structures. An anesthesiologist was responsible for managing the depth of sedation and analgesia (using dexmedetomidine and dezocine) based on the patient’s responses. All standard operating procedures (SOPs) were referring to Anthony Tung Yeung.11 Then, the drainage was placed alongside the incision and were removed in 1 days. Following the surgery, patients were advised to undergo a rest period ranging from 7 to 14 days, depending on their individual recovery progress.
Surgical Types (with or without Intradiscal Irrigation)
Conventional TELD
A marker was placed on the skin over the target disc with the guidance of C-arm fluoroscopy. After sterilization and draping, TELD was performed according to the standard procedure.10 A 15 cm 16 G needle was placed cephalad-caudally to the facet, and infiltration local anesthesia was performed. A guide wire was placed through the 16 G needle, and the needle was withdrawn. The guide rod entered through the guide wire, and a subsequent expanding pipe was placed. Foraminoplasty was performed, and the working cannula was inserted into the spinal canal through the enlarged foramen. Endoscopy was performed, and the herniated fragment was removed. Intradiscal normal disc removal was performed directly using forceps. Finally, the endoscope and working cannula were withdrawn.
TELD with Intradiscal Irrigation
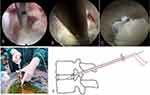
A marker was placed on the skin over the target disc with the guidance of C-arm fluoroscopy. After sterilization and draping, TELD was performed according to the standard procedure.10 After the working cannula was placed, the endoscope was inserted. Intradiscal irrigation with diluted methylene blue or pure saline was injected by pressure through a 25 cm-long needle into the annulus via the working channel of the endoscope to increase the pressure of the disc (Figure 1A–E). The bulk of the fragment tethered within the annulus fibrosus was removed by the flow. After irrigation, discectomy of the herniated disc within the spinal canal was performed, and further intradiscal irrigation was administered until no sequestered or loose fragments were washed out (Figures 1C and 2). The endoscope was withdrawn.
Usage of Methylene Blue
To determine the torn annulus, methylene blue was injected into the disc for patients with protruded, extruded or contained disc herniation in both groups. For the conventional group, an 18 cm 21 G needle was placed through the 16 G needle and inserted into the annulus fibrosus to perform nucleus pulposus staining by methylene blue. Nuclear pulposus staining was used to differentiate the nucleus pulposus from the surrounding annulus fibrosus.
For the disc irrigation group, a 25 cm-long 18 G needle was inserted through the working channel of the endoscope into the annulus fibrosus. Intradiscal irrigation was performed using methylene blue or saline to increase the pressure of the disc and wash the herniation out of the disc before discectomy.
Follow-Up
All patients were followed up at the 3rd, 6th and 12th months post-operatively. A visual analog scale (VAS) of 0–10.0 was used to evaluate low back pain, including central back pain and radiating pain to the lateral buttock. Neutral standing lateral radiographs were taken for disc height measurement, and MRI was performed for Pfirrmann grade classification preoperatively and 12 months post-operatively (Figure 2).
Measurement and Evaluation
Disc-Vertebra Height Ratio (D-V H Ratio) on Radiograph
A modified Mochida method was used to measure the D-V H ratio at three points on the endplate of the involved segment (anterior point, middle point and posterior point) on the neural lateral radiograph.12 The D-V H ratios of the three points were averaged to calculate the D-V H ratio for the operative level (Figure 3A). D-V H ratio=(a+b+c)/(A+B+C) (Figure 3A). Disc height ratio loss was calculated by subtracting the postoperative disc height ratio from the preoperative disc height ratio (Figure 3B, E and G).
Pfirrmann Grades and HIZ on MRI
The Pfirrmann grading system was used to classify degeneration of the disc into five grades. The preoperative and postoperative Pfirrmann grades were recorded (Figure 3C, D, F and H). Preoperative HIZ was also recorded.
Trephine and Cannula Position Grades During TELD
The position of the trephine and working cannula during the surgery was classified into three grades, termed the cannula position grade. Grade 1 indicated a good position with no violation of the annulus, endplate or facet. Grade 2 indicated that the tip of the working cannula penetrated less than 50% of the annulus fibrosus with no violation to the endplate or that the working cannula was placed too dorsally or caudally to the tip of the superior articular process. Grade 3 indicated that the tip of the working cannula penetrated more than 50% of the annulus fibrous and/or violated the endplate or that the working cannula violated the facet joints or was placed more caudally to the superior rim of the pedicle (Figure 4). In this study, we have creatively established a Trephine and Cannula Position Grading System. To ensure the consistency of individual testers, we invited two different testers to independently grade the position of the trephine and cannula twice for each patient. The average score was recorded for univariate linear regression analysis and PLS analysis. The consistency of these results was analyzed by Weighted Kappa.
Re-Herniation Grade
Re-herniation of the surgical disc on MRI at the 12-month follow-up was also classified into 3 grades, termed the re-herniation grade. Grade 1 indicated that herniation was less than 10% of the central sagittal distance of the spinal canal, Grade 2 indicated that herniation was more than 10% and less than 20%, and Grade 3 indicated that herniation was more than 20%.
Statistical Analysis
To determine the relationship between postoperative low back pain and the selected factors, univariate linear regression analysis was performed between the low back pain VAS score and age, sex, D-V H ratio, Pfirrmann grade, cannula position grade, re-herniation grade, HIZ, disc calcification and surgical grade using SPSS 16.0. Pearson’s correlation coefficient r was calculated. P<0.05 was defined as significant. The factors with P<0.05 were chosen for further PLS analysis to quantify the impact of these factors on postoperative low back pain using Simca (Umetrics, Sweden). The R2 values of these factors were calculated. The variable importance in projection (VIP) value was calculated to quantify each factor’s impact on postoperative low back pain. The 3-month VAS and 1-year VAS scores were analyzed separately with the above factors.
Results
Demographic Information
Sex, age, operative segment, herniation type, reoperation, 3-month/1-year low back pain, leg pain and ODI are listed in Table 1. Postoperative complication incidence rate was collected in Table 2. Dysesthesia was the most common complications after operation, and the incidence rate is 1.71%.
 |
Table 2 Postoperative Complications |
Univariate Linear Regression Analysis
The Pearson correlation coefficients and P values of postoperative back pain VAS, age, sex, preoperative D/V H ratio, postoperative D/V H ratio, D/V H ratio loss, preoperative Pfirrmann grade, postoperative Pfirrmann grade, methylene blue usage, surgical type, re-herniation grade, cannula position grade, HIZ, operative segment, and disc calcification are listed in Table 3. Both the short-term VAS and long-term VAS scores for low back pain and Correlation analysis of postoperative VAS of short term and long term are presented in Table 1 and Table 3.
 |
Table 3 Correlation Analysis of Postoperative Pain (VAS) with Various Factors |
Surgical Type
The univariate linear regression analysis showed that the surgical type was significantly correlated with the long-term postoperative low back pain VAS score but was not significantly correlated with the short-term postoperative low back pain VAS score. The r values were −0.128 (P = 0.218) and 0.211 (P = 0.023), respectively.
Re-Herniation Grade
The univariate linear regression analysis showed that the grade of recurrent disc herniation was significantly correlated with both short-term and long-term postoperative low back pain. The r values were 0.273 (P = 0.008) and 0.368 (P = 0.000), respectively.
Disc Height Ratio Loss
The univariate linear regression analysis showed that D-V H ratio loss was significantly correlated with both short-term and long-term postoperative low back pain. The r values were 0.335 (P = 0.001) and 0.2 (P = 0.034), respectively.
Sex and Age
The univariate linear regression analysis showed that both short-term and long-term postoperative low back pain were significantly correlated with sex but not age. The r values were 0.231 (P = 0.025) and 0.271 (P = 0.003), respectively, for sex.
Trephine and Cannula Position Grades
The consistency test of Cannula position-grade system showed a kappa value of 0.667. The univariate linear regression analysis showed that the position of the trephine/working cannula was significantly correlated with short-term postoperative low back pain but not long-term postoperative low back pain. The r values were 0.216 (P = 0.036) and 0.053 (P = 0.57), respectively.
D-V H Ratio, Pfirrmann Grade, and Methylene Blue Usage
The univariate linear regression analysis showed that postoperative low back pain was not significantly correlated with the preoperative or postoperative D-V H ratio, Pfirrmann grade or use of methylene blue/saline. The r values are listed in Table 3.
PLS for Postoperative Back Pain
The re-herniation grade, D-V height ratio loss, trephine/cannula position and sex were significant variables affecting short-term postoperative low back pain according to the univariate linear regression analysis. The re-herniation grade, surgical type, D-V height ratio loss and sex were significant variables affecting long-term postoperative low back pain according to the univariate linear regression analysis. The impact of these variables on low back pain was analyzed by using PLS. The R2 values were 0.246 and 0.304, respectively. The VIPs of these variables are presented in Table 4. For short-term pain, the PLS coefficient showed that sex, trephine/cannula position, re-herniation and disc height loss were positive factors for increasing low back pain. For long-term pain, the PLS coefficient showed that intradiscal irrigation was a negative factor, while sex, re-herniation and disc height loss were positive factors for increasing low back pain (Table 5).
 |
Table 4 PLS Analysis of Low Back Pain VAS at 3 Months and 1 Year with Significant Variables |
 |
Table 5 Significant Coefficients of Variables in PLS Analysis of Low Back Pain VAS |
Discussion
Recurrent low back pain is a frequently observed complication following both transforaminal endoscopic lumbar discectomy (TELD) and microdiscectomy procedures. A comprehensive review of the literature and a prospective study assessing outcomes revealed that noticeable recurrent low back pain can manifest in approximately 15% to 25% of patients at the 2-year mark post-discectomy.13 A study published in BMJ indicated that patients who underwent TELD experienced more favorable outcomes compared to those who underwent fenestration discectomy. In terms of back pain, the reported pain score after TELD (VAS 1.6) was lower than that following fenestration discectomy (VAS 2.1).14 Nevertheless, the occurrence of pain radiating to the low back, particularly in the lateral buttock area, remains a common complaint among patients who have undergone TELD. Chen’s findings demonstrated that 8.1% of patients continued to experience persistent low back pain at the 2-year follow-up.15
In the past five years, several articles have identified risk factors for low back pain following percutaneous endoscopic lumbar discectomy (TELD). Modic changes have been highlighted as a significant risk factor after TELD.5,16,17 Other important sources of pain after the operation include the posterior longitudinal ligament, endplate abnormalities, and muscle fatty infiltration6,16,18(Table 6).
 |
Table 6 Part of Articles Related to Risks of TELD |
In this study, we reported for the first time that short-term postoperative low back pain was correlated with sex, quality of trephine/cannula position, extent of re-herniation, and disc height loss, and long-term postoperative low back pain was correlated with sex, intradiscal irrigation, extent of re-herniation and disc height loss. Facet joint injury, posterior branch of nerve root irritation, annulus fibrous damage, and cartilage endplate violation were correlated with low back pain at the short-term follow-up, which indicated that malposition of the trephine or cannula would result in worse low back pain (Figure 4). In the long term, the low back pain VAS score and ODI decreased, and pain was not correlated with cannula position grade, indicating that physical repair of these injuries might occur over time. Loss of disc height was reported to increase the aberrant stress on facets;19 consequently, both short-term and long-term low back pain were significantly correlated with disc height loss. Intradiscal irrigation was effective in decompressing the intradiscal loose fragment, preventing excessive normal disc removal and reducing loss of disc height following TELD (Figures 2 and 3).20,21 In this study, intradiscal irrigation was shown to reduce long-term low back pain (r = −0.221). Sex has been reported to be significantly associated with the severity of pain and analgesic usage.22 In this study, sex was found to be significantly correlated with low back pain after TELD. Female patients tend to have a higher extent of LBP than male patients following TELD. The re-herniation grade was found to be a significant factor associated with low back pain, indicating that a higher re-herniation ratio on MRI could indicate greater low back pain. By PLS analysis, sex, disc re-herniation, intradiscal irrigation, and disc height loss were found to be factors with a significant impact on the prediction of postoperative low back pain, and the linear combination of the four factors contributed to almost 30% of the long-term low back pain VAS score after TELD. Re-herniation extent and disc height loss were proven to be associated with intradiscal irrigation.20,21 These generalized results indicated that intradiscal irrigation was more effective in decreasing low back pain at the long-term follow-up, while careful foraminoplasty and cannula placement were effective in preventing short-term low back pain.
The intradiscal irrigation procedure, which was initially reported by our group,20,21 was found to be correlated with a lower rate of low back pain after TELD. Discogenic back pain constitutes 30–40% of low back pain in the lumbar spine. Annulus fibrosis tears induce local nonbacterial inflammation at the herniation site, and inflammatory constituents within the intervertebral discs stimulate sensitized nociceptors and nucleus pulposus cells within the tears.23 Inflammation can also create a detrimental environment; if inflammation within the nucleus pulposus is not addressed, it will influence NP cells and induce a feedback loop to escalate inflammation.24,25 Our group has reported the use of an intradiscal irrigation needle to remove the degenerative and loose fragments within the disc, which will also wash away the inflammatory constituents within the disc and recentralize the signal of the nucleus pulposus after TELD (Figures 2 and 3).20,21 We hypothesized that intradiscal irrigation would eliminate inflammation in the nucleus pulposus and recentralize the nucleus pulposus, which results in a lower grade of low back pain after TELD.
The judicious removal of normal disc tissue through intradiscal irrigation has been demonstrated to effectively decrease the level of low back pain following transforaminal endoscopic lumbar discectomy (TELD). Research by McGirt has indicated that overly aggressive normal disc removal is linked to higher rates of recurrent back and leg pain. On the other hand, limited discectomy tends to result in a greater incidence of re-herniation in the long term.26 Although an extensive removal of normal disc tissue does reduce the likelihood of re-herniation, it concurrently diminishes disc height, compromises disc structural integrity, and disrupts the bio-mechanical functionality of the disc. In the context of this study, the application of intradiscal irrigation successfully reduced postoperative low back pain without causing an increase in the need for re-operation. In existing literature, reported low back pain Visual Analog Scale (VAS) scores have ranged from 1.6 to 3.0.14,27 However, when employing intradiscal irrigation, the average long-term VAS score for low back pain decreased to 1.08. One plausible explanation for this observation is that disc irrigation helps prevent excessive normal disc removal, leading to the restoration of disc height. Both of these factors—normal disc preservation and disc height restoration—have shown significant associations with postoperative back pain in this study.
Conclusion
The study shows that one year after surgery, low back pain correlates with disc height loss, re-herniation extent, intradiscal irrigation, and sex. At three months, it relates to disc height loss, re-herniation extent, trephine/cannula positioning, and sex.
Date Availability
The data are available from the corresponding author on reasonable request.
Ethic Declaration
The Ethics Committee of Shanghai Changzheng Hospital does not require us to obtain explicit written consent from patients. Because all operative procedure had undergo rigorous ethical review for keeping the safety of medical care and individual privacy. All patients’ data were reserved confidentially under the inspection of the ethical committee even if without written consent. And all surgical procedures have no adverse effect on the patient’s prognosis. We will always comply with relevant laws, regulations, and international ethical guidelines, particularly the “Helsinki Declaration”.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work is sponsored by Science Foundation of Shanghai “The application of PIS aspiration system in the early treatment of intervertebral disc herniation and foraminoscopy” (21Y11911300) and also sponsored by NSFC “the modulation of integrin alpha6 in hypoxia effect on degeneration of nucleus pulposus cells” (82072485).
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP. Low back pain. Lancet. 2021;398(10294):78–92. doi:10.1016/S0140-6736(21)00733-9
2. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163–2196. doi:10.1016/S0140-6736(12)61729-2
3. Boswell MV, Trescot AM, Datta S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10:1.
4. Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(2):21–24. doi:10.2106/JBJS.E.01273
5. Xu J, Li Y, Wang B, et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation with Modic changes via a transforaminal approach: a retrospective study. Pain Physician. 2019;22(6):E601–E608.
6. Ru N, Su C, Li J, et al. Varied low back pain induced by different spinal tissues in percutaneous endoscopic lumbar discectomy: a retrospective study. Pain Physician. 2022;25(2):E331–E339.
7. Liu L, Xue H, Jiang L, et al. Comparison of percutaneous transforaminal endoscopic discectomy and microscope-assisted tubular discectomy for lumbar disc herniation. Orthop Surg. 2021;13(5):1587–1595. doi:10.1111/os.12909
8. Kirnaz S, Capadona C, Wong T, et al. Fundamentals of intervertebral disc degeneration. World Neurosurg. 2022;157:264–273. doi:10.1016/j.wneu.2021.09.066
9. Pan -C-C, Simon P, Espinoza Orías AA, et al. Lumbar facet joint subchondral bone density in low back pain and asymptomatic subjects. Skeletal Radiol. 2020;49(4):571–576. doi:10.1007/s00256-019-03314-w
10. Wu X, Wang J, Xu Z, et al. Bi-needle PELD with intra-discal irrigation technique for the management of lumbar disc herniation. Pain Physician. 2022;25(2):E309–E317.
11. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27(7):722–731. doi:10.1097/00007632-200204010-00009
12. Eun SS, Lee S-H, Sabal LA. Long-term follow-up results of percutaneous endoscopic lumbar discectomy. Pain Physician. 2016;19(8):E1161–E1166.
13. Parker SL, Mendenhall SK, Godil SS, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 2015;473(6):1988–1999. doi:10.1007/s11999-015-4193-1
14. Gadjradj PS, Rubinstein SM, Peul WC, et al. Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial. BMJ. 2022;376:e065846. doi:10.1136/bmj-2021-065846
15. Chen Z, He L, Di J, et al. Lumbar facet joint osteoarthritis as the underlying reason for persistent low back pain after minimally invasive discectomy. Arch Orthop Trauma Surg. 2023;143(7):3811–3821. doi:10.1007/s00402-022-04595-y
16. Chen F, Xin J, Su C, Liu X, Cui X. Pain variability of tissues under endoscope in percutaneous endoscopic lumbar discectomy and its significance: a retrospective study. Pain Physician. 2021;24(6):E877–E882.
17. Zhong D, Ke Z-Y, Chen Q, Liu Y, Lin L, Wang Y. A clinical nomogram for predicting the residual low back pain after percutaneous endoscopic surgery for lumbar disc herniation. Int Orthop. 2023;47(3):819–830. doi:10.1007/s00264-022-05658-w
18. Fu Y, Yan Y-C, Ru X-L, Qu H-B. Analysis of chronic low back pain caused by lumbar microinstability after percutaneous endoscopic transforaminal discectomy: a retrospective study. J Pain Res. 2022;15:2821–2831. doi:10.2147/JPR.S380060
19. Yeung A, Lewandrowski K-U. Early and staged endoscopic management of common pain generators in the spine. J Spine Surg. 2020;6(Suppl 1):S1–S5. doi:10.21037/jss.2019.09.03
20. X-D W, Chen Y, W-C Y, et al. Effectiveness of bi-needle technique (hybrid Yeung endoscopic spine system/transforaminal endoscopic spine system) for percutaneous endoscopic lumbar discectomy. World Neurosurg. 2018;119:e53–e59. doi:10.1016/j.wneu.2018.06.220
21. Xu Z, Zheng J-C, Sun B, et al. Bi-needle technique versus transforaminal endoscopic spine system technique for percutaneous endoscopic lumbar discectomy in treating intervertebral disc calcification: a propensity score matched cohort analysis. Br J Neurosurg. 2021;35(3):245–250. doi:10.1080/02688697.2020.1784393
22. Pieretti S, Di Giannuario A, Di Giovannandrea R, et al. Gender differences in pain and its relief. Ann Ist Super Sanita. 2016;52(2):184–189. doi:10.4415/ANN_16_02_09
23. Khan AN, Jacobsen HE, Khan J, et al. Inflammatory biomarkers of low back pain and disc degeneration: a review. Ann N Y Acad Sci. 2017;1410(1):68–84. doi:10.1111/nyas.13551
24. Xia C, Zeng Z, Fang B, et al. Mesenchymal stem cell-derived exosomes ameliorate intervertebral disc degeneration via anti-oxidant and anti-inflammatory effects. Free Radic Biol Med. 2019;137:143. doi:10.1016/j.freeradbiomed.2019.04.030
25. Zhang Y, He F, Chen Z, et al. Melatonin modulates IL-1β-induced extracellular matrix remodeling in human nucleus pulposus cells and attenuates rat intervertebral disc degeneration and inflammation. Aging. 2019;11(22):10499–10512. doi:10.18632/aging.102472
26. McGirt MJ, Ambrossi GLG, Datoo G, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery. 2009;64(2). doi:10.1227/01.NEU.0000337574.58662.E2
27. Choi KC, Kim J-S, Park C-K. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Physician. 2016;19(2):E291–E300. doi:10.36076/ppj/2016.19.E291
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.