Back to Journals » Infection and Drug Resistance » Volume 16
Risk Factors for Pulmonary Infection and Nursing Interventions Post-Tracheostomy in Patients with Spinal Cord Injury
Authors Lv Q, Zhang X, Guo K, Hu D, Deng Z
Received 26 April 2023
Accepted for publication 21 September 2023
Published 13 October 2023 Volume 2023:16 Pages 6691—6701
DOI https://doi.org/10.2147/IDR.S418894
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Qin Lv,1,* Xinliang Zhang,1,* Kucun Guo,1 Dezheng Hu,1 Zhuojun Deng2
1Department of Emergency, The Third Hospital of Hebei Medical University, Shijiazhuang City, Hebei Province, 050051, People’s Republic of China; 2Department of General Medicine, The Third Hospital of Hebei Medical University, Shijiazhuang City, Hebei Province, 050000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xinliang Zhang, Department of Emergency, The Third Hospital of Hebei Medical University, No. 139 Ziqiang Road, Qiaoxi District, Shijiazhuang City, Hebei Province, People’s Republic of China, 050051, Tel +86 18533112509 ; +86 311-88602030, Email [email protected]
Objective: We analyzed the characteristics and risk factors for pulmonary infection in patients with spinal cord injury who underwent tracheostomy and propose measures to help in early detection and intervention to reduce mortality and improve prognosis.
Methods: We collected data retrospectively from January 1, 2018, to December 31, 2022. The inclusion criteria were: Patients aged 18 years or more with a spinal cord injury who underwent tracheostomy, were treated with mechanical ventilation for over 48 hours, and were diagnosed as having a pulmonary infection. Sputum samples were cultured and analyzed.
Results: 101 cases of pulmonary infection were analyzed, and the incidence was 32.17%. Diabetes (OR 2.302, 95% CI 1.285– 3.972), hypoproteinemia (OR 1.992, 95% CI 1.125– 3.101), administration of glucocorticoids (OR 2.934, 95% CI 1.412– 4.661), ASIA grade A (OR 3.672, 95% CI 1.988– 5.046), mechanical ventilation for ≥ 6 days (OR 2.108, 95% CI 1.385– 4.751), and length of hospital stay for ≥ 20 days (OR 2.137, 95% CI 1.092– 3.842) were risk factors for pulmonary infection in patients with spinal cord injury post-tracheostomy. Among 213 pathogenic bacteria, 52 (51.48%) were Gram-negative and 24 (23.76%) were Gram-positive. Klebsiella pneumoniae (15.84%) and Staphylococcus aureus (8.91%) were the most common pathogenic bacteria. The mortality rate of patients with gram-positive infection was higher than that of patients with gram-negative infection. K. pneumoniae and S. aureus were sensitive to cefoperazone, meropenem, and levofloxacin.
Conclusion: Pulmonary infection is a complication post-tracheostomy in patients with spinal cord injury. Diabetes, hypoproteinemia, administration of glucocorticoids, mechanical ventilation for ≥ 6 days, length of hospital stay for ≥ 20 days were risk factors for pulmonary infection. Pulmonary infection was mainly caused by gram-negative bacteria. Timely and effective measures for managing risk factors are essential for improving the prognosis of pulmonary infection post-tracheostomy in patients with spinal cord injuries.
Keywords: risk factors of pulmonary infection, spinal cord injury, tracheostomy
Introduction
The main causes of acute traumatic spinal cord injury (ATSCI) include falls from heights, traffic accidents, industrial and construction accidents, and sports injuries.1 It is estimated that most deaths usually occur within three days of a spinal cord injury.2 The greater the extent of the injury, the higher is the mortality rate.3 Spinal cord injury not only severely impairs sensory, motor, and sympathetic activity, but also causes respiratory muscle weakness or paralysis and respiratory impairment.4 Pulmonary complications include atelectasis, pulmonary infection, respiratory failure, aspiration of gastric contents, pulmonary embolism, and bronchospasm,5 which are the most common causes of morbidity in spinal cord injury and death.5–8 Jackson et al9,10 estimated that approximately 67% patients with spinal cord injury had pulmonary complications, and longer duration of mechanical ventilation were required once pulmonary complications set in.
Tracheostomy is often performed on critically ill patients in the emergency department, accounting for 6% of this population, and is one of the most commonly performed procedures for mechanically ventilated patients in the intensive care unit (ICU).11–13 It is estimated that approximately 21% to 77% patients with complete cervical spinal cord injury require tracheostomy for respiratory support.14,15 Tracheostomy is conducive for patients with prolonged and complicated mechanical ventilation to wean them off the ventilator, and reduces the complications of long-term endotracheal intubation,16 shortens the length of stay in the ICU, increases comfort, improves vocalization and swallowing functions, reduces the dose of sedative drugs, shortens the duration of sedation,17 improves lung drainage, and reduces pulmonary complications.
However, tracheostomy is an invasive procedure in which the tracheostomy acts as a bypass, eliminating the protective impact of the nasal passage that provides air filtration, humidification, and warming, thereby disrupting the body’s barrier and inhibiting the airway’s own defenses. Tracheostomy tubes also create a direct entry point for viruses and bacteria into the lower respiratory tract, and the presence of the cannula can also cause local inflammatory reactions, thereby increasing the risk of respiratory tract infections, delaying patient recovery and causing worsening of the disease.18 In addition, pathogenic bacteria that cause infection in the hospital are more complex and may be multi-drug resistant.
Pulmonary infection is a common and serious complication after tracheostomy in patients with a spinal cord injury. The objective of our study was to investigate the prognostic factors for pulmonary infection in such patients and propose measures for clinical nursing practices. Therefore, we aimed to analyze the characteristics of pulmonary infection in patients with spinal cord injury post-tracheostomy, identify the risk factors for pulmonary infection, and carry out early detection and intervention for secondary pulmonary infection in patients with spinal cord injury, which could help reduce mortality, improve prognosis, and provide a reliable basis for the treatment of clinical spinal cord injury. Additionally, we aimed to explore nursing interventions to prevent pulmonary infection in patients with spinal cord injury.
Data and Methods
Ethical Considerations
We carried out all research procedures in this study in accordance with relevant guidelines and regulations, and with the approval of the Ethics Committee of the Third Hospital of Hebei Medical University (approval number: Section 2022-005-1). This study was conducted in accordance with the declaration of Helsinki. The Ethics Committee of the Third Hospital of Hebei Medical University exempted the requirement of written informed consent: This clinical study is a retrospective study. It only collects the patient’s clinical data, does not interfere with the patient’s treatment plan, and will not bring risks to the patient’s physiology. The researchers confirm that patients’ information will not be disclosed unless it is de-identified, in order to maintain confidentiality and personal privacy.
Research Participants
In this study, we selected patients who underwent tracheostomy for acute traumatic cervical spinal cord injury and were admitted to our hospital from January 1, 2018 to December 31, 2022, as participants.
Inclusion Criteria
- Based on imaging and the clinical data, patients who received a definite diagnosis of traumatic cervical spinal cord injury (including patients with cervical fracture dislocation and cervical spinal cord injury without fracture).
- Patients with spinal cord injury who underwent tracheostomy during hospitalization.
- Patients on mechanical ventilation for over 48 h.
- Age ≥ 18 years.
- The clinical data of patients were complete.
Exclusion Criteria
- Patients with chronic cervical spinal cord injury due to other diseases.
- Patients with chronic diseases of the respiratory system or obvious chest trauma.
- Patients with locally open wounds who underwent debridement and suturing in the emergency department.
- Patients who received other surgical treatment in the emergency department due to other organ injuries before surgery.
- Patients with poor physical condition due to diagnosed tumors or other well-defined consumptive diseases.
- Patients who received anti-infective therapy before admission.
- Patients with a definite diagnosis or complications associated with other types of infections (such as urinary tract infections, incision infections, and so on) post-surgery.
Research Methods
Data Collection
We collected the following clinical data retrospectively: gender, age, body mass index, alcohol consumption, smoking, hypertension, diabetes, hyperlipidemia, hypoproteinemia (total plasma protein < 60 g/L), administration of glucocorticoids, indwelling gastric tube, type of spinal cord injury (grading based on the American Spinal Injury Association (ASIA) impairment scale),19 duration of mechanical ventilation, length of hospital stay, and mortality. We divided patients into the pulmonary infection group and the non-pulmonary infection group based on whether there was pulmonary infection or not, respectively, and analyzed the characteristics of the two groups.
Diagnostic Criteria for Pulmonary Infection
In our study, we focused on pulmonary infections in patients with spinal cord injury post-tracheostomy, which is part of hospital-acquired pneumonia. The diagnosis of pneumonia was based on the following diagnostic criteria for hospital-acquired pneumonia formulated by the Respiratory Disease Branch of the Chinese Medical Association:20 (1) Newly developed cough, expectoration, or worsening of the symptoms of the original respiratory disease, with purulent sputum. With or without chest pain; (2) Fever; (3) Signs of pulmonary consolidation and/or crackles; (4) Blood leukocytes > 10×109/L or <4×109/L, with or without left shift; (5) Chest X-ray showed patchy infiltrates or interstitial changes, with or without pleural effusion; (6) The time and place of disease onset were consistent with nosocomial infection. Definite diagnosis could be made with any of the above items from 1–4 plus items 5 and 6, excluding atelectasis, heart failure and pulmonary edema, pulmonary embolism, respiratory distress syndrome and other diseases. Reinfection was defined as redevelopment of pulmonary infection one week after discontinuation of antibiotics in patients with pulmonary infection who were stable after treatment.
Specimen Collection and Sputum Culture
Sputum was collected from patients diagnosed with pulmonary infection, and procedures were stringently followed to avoid contamination.21
All specimens were sent to the laboratory immediately for routine isolation and culture. We used the automatic bacterial culture detector Bact/ALERT@3D (bioMérieux, Marcy l’Étoile, France) to identify pathogenic bacteria, and the pathogenic bacteria were confirmed if more than two consecutive cultures gave the same results.
Gram-positive infection was defined as only gram-positive bacterium detected in the sputum culture, while gram-negative infection was defined as only gram-negative bacterium detected in the sputum culture. A diagnosis of mixed infection was made when two or more pathogenic bacteria were detected. We described each type of infection using the number and percentage of patients and analyzed the relationship between injury type and pathogenic bacteria distribution.
We used a sputum culture device to suck the deep secretions of the lower respiratory tract through the tracheal cannula, and the samples were immediately sent to our laboratory for bacteria culture and a drug sensitivity test. Sterile procedures were strictly adhered to during the process of sputum specimen collection.
Spinal Cord Injury Assessment
We referred to the Acute Cervical Spine and Spinal Cord Injury Management Guidelines formulated by the American Association of Neurological Surgeons (AANS)22 for the diagnostic criteria for spinal cord injury In this study, we assessed the type of spinal cord injury as per the 5th edition of the American Spinal Injury Association’s (ASIA) injury grading scale (Table 1),19 and the categories were complete spinal cord injury (ASIA grade A) and incomplete spinal cord injury (ASIA grade B, C, and D). The assessment of the degree of nerve damage is usually based on neuroimaging findings. In this case, we used magnetic resonance imaging (MRI) to assess the degree of nerve injury and classified it as a high cervical cord injury (C1–C3) or a low cervical cord injury (C4–T1) based on the anatomical structure of the cervical spine and the location of the injury on the spinal cord.
 |
Table 1 Classification of the ASIA Impairment Grade |
The cervical spine consists of vertebrae C1 through C7, where C1 is the first bone of the cervical spine and C7 is the seventh bone of the cervical spine. The high cervical spinal cord refers to the part of the cervical spine from C1 to C3. This area is the connection between the neck and the head and mainly controls the movement and sensation of the head and neck. The lower cervical cord refers to the part of the cervical spine from C4 to T1, which is the connection between the neck and the upper body and mainly controls the movement and sensation of the upper body.
Therefore, we used MRI to assess and classify the nerve injury, to accurately understand the location and extent of the injury and facilitate more effective treatment and rehabilitation programs.
Statistical Analysis
We used the SPSS 24.0 software for statistical analysis. We used mean ± standard deviation analysis for normally distributed continuous variables and t-test for between-group comparisons. For continuous variables that did not fall into normal distribution, we expressed the results as the median and inter-quartile range (IQR) and used the Mann–Whitney U-test for between-group comparisons. We expressed counting data as number or percentage (%), and the chi-squared test was used for between-group comparisons. In univariate regression analysis, we used the chi-squared test or Fisher’s exact probability method for categorical variables. In multivariate analysis, we used logistic regression to analyze risk factors associated with the development of pulmonary infection. In this study, we considered P < 0.05 as statistically significant. Diabetes mellitus, hypoproteinemia, coma ≥ 22 h, mechanical ventilation ≥ 6 d, hospital stay ≥20 d were risk factors for pulmonary infection. Sample size was calculated to be around 100.
Results
There were 531 patients with traumatic cervical spinal cord injury in our hospital from January 1, 2018 to December 31, 2022, and as per the inclusion and exclusion criteria, we included a total of 314 patients with spinal cord injury who underwent tracheostomy. The main causes of injuries included motor vehicle accidents, bruise injuries on the neck caused by heavy objects, injuries by falls from height, and falling over. All patients underwent tracheostomy to improve artificial respiration and correct respiratory impairment. Among them, there were 101 cases of pulmonary infection, with an incidence rate of 32.17%.
Population Characteristics of Patients with Spinal Cord Injury Who Underwent Tracheostomy and Univariate Analysis of Pulmonary Infection
There were significant differences between the pulmonary infection group and the non-pulmonary infection group in terms of diabetes, hypoproteinemia, administration of glucocorticoids, ASIA grade, duration of mechanical ventilation, length of hospital stay, and fatality rate (all P < 0.05) (Table 2). There were no significant differences in gender, age, body mass index, alcohol consumption, smoking, hypertension, hyperlipidemia, indwelling gastric tube, and nerve injury level (P > 0.05).
 |
Table 2 Summary of Influencing Factors in the Pulmonary Infection Group and Non-Pulmonary Infection Group in Patients with Spinal Cord Injury Post-Tracheostomy |
Multivariate Analysis of Pulmonary Infection in Patients with Spinal Cord Injury Who Underwent Tracheostomy
We included the significant indicators in univariate analysis (diabetes, hypoproteinemia, administration of glucocorticoids, ASIA grade, duration of mechanical ventilation, length of hospital stay) in the logistic regression analysis. We found that diabetes (OR 2.302, 95% CI 1.285–3.972), hypoproteinemia (OR 1.992, 95% CI 1.125–3.101), administration of glucocorticoids (OR 2.934, 95% CI 1.412–4.661), ASIA grade A (OR 3.672, 95% CI 1.988–5.046), mechanical ventilation for ≥ 6 days (OR 2.108, 95% CI 1.385–4.751), and length of hospital stay for ≥ 20 days (OR 2.137, 95% CI 1.092–3.842) were risk factors for pulmonary infection in patients with spinal cord injury post-tracheostomy (P < 0.05) (Table 3 and Table 4).
 |
Table 3 Risk Factors and Assignment of Pulmonary Infection |
 |
Table 4 Logistic Regression Analysis of Multifactorial Risk Factors for Pulmonary Infection in Patients with Spinal Cord Injury Post-Tracheostomy |
Bacteriological Analysis of Pulmonary Infection in Patients with Spinal Cord Injury Who Underwent Tracheostomy
Bacteriological Distribution of Pulmonary Infection
We isolated a total of 213 pathogenic bacteria from the lower respiratory tract secretions of 101 patients with pulmonary infection—these included 52 cases (51.48%) of gram-negative bacteria infection and 24 cases (23.76%) of gram-positive bacterial infection. Among the pathogenic bacteria of pulmonary infection, Klebsiella pneumoniae (15.84%) and Staphylococcus aureus (8.91%) were the most common pathogens. The mortality rate of patients with gram-positive bacterial infection was significantly higher than that of patients with gram-negative bacteria infection (P < 0.05).
Among the 101 patients with pulmonary infection, a total of 21 (20.79%) had mixed bacterial infections, mainly Candida tropicalis, S. aureus, Pseudomonas aeruginosa, and Acinetobacter baumannii (Table 5).
 |
Table 5 Bacterial Distribution of Pulmonary Infection in Patients with Spinal Cord Injury Post-Tracheostomy (n = 101) |
Drug Resistance Rate and Susceptibility Test of K. pneumoniae and S. aureus in Patients with Pulmonary Infection
The antibiotic resistance rates and drug susceptibility tests of K. pneumoniae and S. aureus are shown in Table 6. K. pneumoniae and S. aureus were highly sensitive to cefoperazone, meropenem, and levofloxacin.
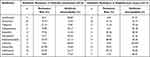 |
Table 6 Antibiotic Resistance Rates and Susceptibility Test Results of Klebsiella pneumoniae and Staphylococcus aureus |
Discussion
The treatment of ATSCI remains a challenge in the field of spinal trauma. The concurrent incomplete or complete paralysis often leads to respiratory dysfunction due to phrenic nerve paralysis and respiratory muscle weakness, weakened ability to actively remove secretions, and poor coughing up of sputum caused by body position. This easily facilitates pathogenic bacteria to enter the lower respiratory tract and cause pulmonary complications. Among them, the most important focus of treatment is pulmonary infection, which is also one of the main causes of early death in patients with ATSCI. Therefore, in such patients, the prevention and control of pulmonary infection is the core challenge in the comprehensive treatment of spinal cord injury. To achieve favorable and effective recovery, it is essential to comprehensively understand the relevant factors toward preventing and treating pulmonary infection.
In this study, we found that the incidence of pulmonary infection in patients with spinal cord injury who underwent tracheostomy was 32.17%. The results of logistic regression analysis revealed that the most important factor affecting lung infection was ASIA grade A cervical spinal cord injury, and other risk factors were administration of glucocorticoids, diabetes, length of hospital stay for ≥ 20 days, mechanical ventilation for ≥ 6 days, and hypoproteinemia, in that order. It is essential to carry out early prevention and intervention for these risk factors in clinical nursing.
Post-tracheostomy, the air is not humidified and filtered by the upper respiratory tract, but directly enters the lungs, and this can damage the ciliated epithelium of the respiratory mucosa, making it difficult to remove secretions and foreign bodies.23 Inhalation of dry air, blockage of sputum, pathogenic bacteria and particles containing pathogenic bacteria are likely to cause pulmonary infection.24 Neurological function is impaired in patients with ASIA grade A spinal cord injury, and they have dysphagia, which can easily cause reflux and inhalation of gastric contents into the lungs. The bronchial mucosa and cilia can be damaged by digestive juices, resulting in pneumonia.25,26
Patients with diabetes have poorer immunity and an increased risk of infection when compared to non-diabetic patients.27,28 It was found in one study29 that the high-glucose environment of patients with diabetes provides a good breeding environment for pathogenic microorganisms, which can increase the risk of infection. Therefore, it is important to intensify interventions for improving the immune status and stabilizing blood glucose in patients with diabetes.
In addition, decreased pulmonary function caused by dysfunction of the spinal cord nerve is also an important cause of infection. Therefore, respiratory interventions should be improved. The general physical condition, resistance against pathogenic bacteria, and repairing ability are relatively poor in individuals with chronic underlying diseases, so they are more likely to develop pulmonary infections.30 Thus, in addition to making necessary improvements in the immune status of these patients, close monitoring of blood glucose fluctuations and enhanced respiratory management are necessary treatments.31
In this study, we found that hypoproteinemia and administration of glucocorticoids were independent risk factors for pulmonary infection in patients post-tracheostomy. Albumin is an important protein synthesized by the liver, and changes in albumin level can reflect the nutritional status of patients to a certain extent,32 suggesting that pulmonary infection in patients with tracheostomy is related to their nutritional status, resistance, and pulmonary function.
Glucocorticoids are important hormones that regulate the body’s stress response and are frequently used in the emergency care of patients in intensive care units (ICU).33 However, several studies34,35 have shown that glucocorticoids can reduce immune function and lead to decreased anti-infection ability, which is an independent risk factor of infection, and hence suggest that administration of glucocorticoids for patients in the ICU should be restricted before and after tracheostomy. Additionally, patients need to be provided nutritional support based on their specific health conditions to improve their resistance and continuously prevent the occurrence of infection.
The ventilator is often used for patients with ASIA grade A/B spinal cord injury to assist breathing due to respiratory paralysis or shock, and the accompanying ventilator-related pneumonia is always the focus in the prevention and treatment of nosocomial infections. The main causes are contamination of colonizing bacteria in the oropharynx and upper respiratory tract and exogenous bacterial invasion, among others.36 Studies have shown that in patients with spinal cord injury, the incidence of ventilator-associated pneumonia is higher due to respiratory muscle weakness, prolonged supine position, and ineffective cough.37 In this study, we found that mechanical ventilation for ≥ 6 days and length of hospital stay for ≥ 20 days were independent risk factors for pulmonary infection. Therefore, optimizing ventilator parameters and weaning patients early from the ventilator can reduce the incidence of pneumonia in patients.
In this study, we cultured sputum samples from patients for identification and analyzed the pathogenic bacteria species and distribution. We found that the pathogenic bacteria of pulmonary infection were still mainly gram-negative bacteria, followed by gram-positive bacteria and fungi. K. pneumoniae (15.84%) and S. aureus (8.91%) were the most common pathogenic bacteria in the distribution of pathogenic bacteria. The mortality rate of patients with gram-positive infection was significantly higher than that of patients with gram-negative infection.
We also found that the proportion of mixed infection in pulmonary infection was as high as 20.79%. Patients with ASIA grade A spinal cord injury have severely deteriorated respiratory muscle strength, significantly reduced cough and expectoration ability, sputum retention in alveoli and bronchi, and mass-production of different pathogens in the sputum, and these can easily cause mixed infections. Hence, we suggest that monitoring of pathogenic organisms should be enhanced and targeted therapy should be administered during treatment.
We found that K. pneumoniae and S. aureus were highly sensitive to cefoperazone, meropenem, and levofloxacin. Therefore, in clinical practice, the use of antibiotics must be based on resistance and susceptibility tests in order to improve their efficacy and safety.38,39
Clinical management and nursing procedures, including tracheostomy, dressing changes, and endotracheal intubation care, should strictly adhere to aseptic procedures. Additionally, bacterial culture of sputum and drug susceptibility test should be carried out in time, and antibiotics should be adjusted in time as per the test results. Contamination must be avoided during collection of the sputum specimen as this may affect the test results and delay treatment. It is important to perform timely suction of sputum to avoid infection of the tissue surrounding the tracheostomy incision and damage to the respiratory mucosa, thus reducing bacterial migration.40,41 In addition, the patient must be placed in a reasonable position and periodic turning over and back-patting must be done to avoid sputum accumulation, which is conducive to prevent pneumonia.42–44 In addition, early nutritional support is necessary and, if necessary, plasma or albumin should be administered to improve the body’s resistance so as to prevent and reduce the chances of nosocomial infections.
There are several limitations of this study. First, this study is a retrospectively designed study, with all clinical data obtained from patient statements at the time of their clinical consultations and records of the attending physician. The data collected are limited. Second, there are many factors influencing the laboratory data collected. Despite our strict requirements for patient inclusion, there were still unavoidable confounding factors, and there may have been other factors affecting pulmonary infections that we could not include in the analysis. Third, follow-up research requires more large-sample, multi-center epidemiological investigations to clarify the distribution of pathogenic bacteria in patients who develop pulmonary infection with spinal cord injury post-tracheostomy, to more scientifically guide the early administration of antibiotics.
Conclusion
Pulmonary infection is a common and serious complication in patients with spinal cord injury post-tracheostomy. We found that diabetes, hypoproteinemia, administration of glucocorticoids, mechanical ventilation for ≥ 6 days, length of hospital stay for ≥ 20 days were risk factors for pulmonary infection. As per our study results, pulmonary infections were mainly caused by gram-negative bacteria. Timely and effective measures for risk factors are essential to improve the prognosis of pulmonary infection in patients with spinal cord injury following tracheostomy.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethical Statement
This study was conducted with approval from the Ethics Committee of the Third Hospital of Hebei Medical University (approval number: Section 2022-005-1). This study was conducted in accordance with the declaration of Helsinki. The Ethics Committee of the Third Hospital of Hebei Medical University exempted the requirement of written informed consent: This clinical study is a retrospective study. It only collects the patient’s clinical data, does not interfere with the patient’s treatment plan, and will not bring risks to the patient’s physiology. The researchers confirm that patients’ information will not be disclosed unless it is de-identified, in order to maintain confidentiality and personal privacy.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
This study was funded by Health Commission of Hebei Province 2019 Medical Science Research Project of Hebei Province, project number: 20190624. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Disclosure
The authors declare that they have no competing interests.
References
1. Li J, Liu G, Zheng Y, et al. The epidemiological survey of acute traumatic spinal cord injury (ATSCI) of 2002 in Beijing municipality. Spinal Cord. 2011;49(7):777–782. doi:10.1038/sc.2011.8
2. Algahtany MA. Association between orthopedic fractures and traumatic spinal injury due to road traffic accidents. Eur Rev Med Pharmacol Sci. 2021;25(24):7878–7886. doi:10.26355/eurrev_202112_27636
3. Perot PL, Lee WA, Hsu CY, Hogan EL, Cox RD, Gross AJ. Therapeutic model for experimental spinal cord injury in the rat: i. Mortality and motor deficit. Cent Nerv Syst Trauma. 1987;4(3):149–159. doi:10.1089/cns.1987.4.149
4. Winslow C, Bode RK, Felton D, Chen D, Meyer PR. Impact of respiratory complications on length of stay and hospital costs in acute cervical spine injury. Chest. 2002;121(5):1548–1554. doi:10.1378/chest.121.5.1548
5. Urdaneta F, Layon AJ, Guiot B, Mendel E, Kirby RR. Respiratory complications in patients with traumatic cervical spine injuries: case report and review of the literature. J Clin Anesth. 2003;15(5):398–405. doi:10.1016/s0952-8180(03)00105-3
6. Vidal J, Javierre C, Segura R, Lizarraga A, Barbany JR, Pérez A. Physiological adaptations to exercise in people with spinal cord injury. J Physiol Biochem. 2003;59(1):11–18. doi:10.1007/BF03179863
7. Winslow C, Rozovsky J. Effect of spinal cord injury on the respiratory system. Am J Phys Med Rehabil. 2003;82(10):803–814. doi:10.1097/01.PHM.0000078184.08835.01
8. Berlly M, Shem K. Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med. 2007;30(4):309–318. doi:10.1080/10790268.2007.11753946
9. Jackson AB, Groomes TE. Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil. 1994;75(3):270–275. doi:10.1016/0003-9993(94)90027-2
10. Determann RM, Royakkers A, Wolthuis EK, et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care. 2010;14(1):R1. doi:10.1186/cc8230
11. Frutos-Vivar F, Esteban A, Apezteguía C, et al. Outcome of mechanically ventilated patients who require a tracheostomy. Crit Care Med. 2005;33(2):290–298. doi:10.1097/01.ccm.0000150026.85210.13
12. Freeman BD, Morris PE. Tracheostomy practice in adults with acute respiratory failure. Crit Care Med. 2012;40(10):2890–2896. doi:10.1097/CCM.0b013e31825bc948
13. Cheung NH, Napolitano LM. Tracheostomy: epidemiology, indications, timing, technique, and outcomes. Respir Care. 2014;59(6):895–919. doi:10.4187/respcare.02971
14. Harrop JS, Sharan AD, Scheid EH, Vaccaro AR, Przybylski GJ. Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg. 2004;100(1 Suppl Spine):20–23. doi:10.3171/spi.2004.100.1.0020
15. Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheostomy to prolonged translaryngeal intubation (delayed tracheostomy) in critically ill medical patients [published correction appears in Crit Care Med. 2004 Dec;32(12):2566]. Crit Care Med. 2004;32(8):1689–1694. doi:10.1097/01.ccm.0000134835.05161.b6
16. Galeiras Vázquez R, Rascado Sedes P, Mourelo Fariña M, Montoto Marqués A, Ferreiro Velasco ME. Respiratory management in the patient with spinal cord injury. Biomed Res Int. 2013;2013:168757. doi:10.1155/2013/168757
17. Randelman M, Zholudeva LV, Vinit S, Lane MA. Respiratory Training and Plasticity After Cervical Spinal Cord Injury. Front Cell Neurosci. 2021;15:700821. doi:10.3389/fncel.2021.700821
18. Friedberg SA, Griffith TE, Hass GM. Histologic changes in the trachea following tracheostomy. Ann Otol Rhinol Laryngol. 1965;74(3):785–798. doi:10.1177/000348946507400317
19. Ditunno JF, Young W, Donovan WH, Creasey G. The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia. 1994;32(2):70–80. doi:10.1038/sc.1994.13
20. Shi Y, Huang Y, Zhang TT, et al. Chinese guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in adults (2018 edition). J Thorac Dis. 2019;11(6):2581–2616. doi:10.21037/jtd.2019.06.09
21. Leone M, Bouadma L, Bouhemad B, et al. Brief summary of French guidelines for the prevention, diagnosis and treatment of hospital-acquired pneumonia in ICU. Ann Intensive Care. 2018;8(1):104. doi:10.1186/s13613-018-0444-0
22. Walters BC, Hadley MN, Hurlbert RJ, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60(CN_suppl_1):82–91. doi:10.1227/01.neu.0000430319.32247.7f
23. Gosling AF, Bose S, Gomez E, et al. Perioperative Considerations for Tracheostomies in the Era of COVID-19. Anesth Analg. 2020;131(2):378–386. doi:10.1213/ANE.0000000000005009
24. Angel L, Kon ZN, Chang SH, et al. Novel percutaneous tracheostomy for critically ill patients with COVID-19. Ann Thorac Surg. 2020;110(3):1006–1011. doi:10.1016/j.athoracsur.2020.04.010
25. Raimondi N, Vial MR, Calleja J, et al. Evidence-based guidelines for the use of tracheostomy in critically ill patients. J Crit Care. 2017;38:304–318. doi:10.1016/j.jcrc.2016.10.009
26. Siempos II, Ntaidou TK, Filippidis FT, Choi AMK. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(2):150–158. doi:10.1016/S2213-2600(15)00007-7
27. Witcher KG, Bray CE, Chunchai T, et al. Traumatic brain injury causes chronic cortical inflammation and neuronal dysfunction mediated by microglia. J Neurosci. 2021;41(7):1597–1616. doi:10.1523/JNEUROSCI.2469-20.2020
28. Abou-El-Hassan H, Dia B, Choucair K, et al. Traumatic brain injury, diabetic neuropathy and altered-psychiatric health: the fateful triangle. Med Hypotheses. 2017;108:69–80. doi:10.1016/j.mehy.2017.08.008
29. Fu C, Zhou B, Li Z, et al. Risk factors and nursing intervention of pulmonary infection in patients with tracheotomy in ICU.Chinese. J Disinfect. 2017;34(8):760–763. doi:10.11726/j.issn.1001-7658.2017.08.018
30. DiSilvio B, Young M, Gordon A, Malik K, Singh A, Cheema T. Complications and Outcomes of Acute Respiratory Distress Syndrome. Crit Care Nurs Q. 2019;42(4):349–361. doi:10.1097/CNQ.0000000000000275
31. Raimondi N, Vial MR, Calleja J, et al. Evidence-based guides in tracheostomy use in critical patients. Guías basadas en la evidencia para el uso de traqueostomía en el paciente crítico. Med Intensiva. 2017;41(2):94–115. doi:10.1016/j.medin.2016.12.001
32. Shi H, Na Q, Zhang X, Jiang X. Correlations between the levels of acute infection markers and serum albumin in elderly patients with Hip fracture. Aging Clin Exp Res. 2017;29(3):435–441. doi:10.1007/s40520-016-0585-7
33. Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: infectious complications and vaccination recommendations. J Am Acad Dermatol. 2017;76(2):191–198. doi:10.1016/j.jaad.2016.02.1240
34. Quatrini L, Wieduwild E, Escaliere B, et al. Endogenous glucocorticoids control host resistance to viral infection through the tissue-specific regulation of PD-1 expression on NK cells. Nat Immunol. 2018;19(9):954–962. doi:10.1038/s41590-018-0185-0
35. Ince LM, Zhang Z, Beesley S, et al. Circadian variation in pulmonary inflammatory responses is independent of rhythmic glucocorticoid signaling in airway epithelial cells. FASEB J. 2019;33(1):126–139. doi:10.1096/fj.201800026RR
36. Rouzé A, Martin-Loeches I, Nseir S. Airway devices in ventilator-associated pneumonia pathogenesis and prevention. Clin Chest Med. 2018;39(4):775–783. doi:10.1016/j.ccm.2018.08.001
37. Younan D, Lin E, Griffin R, et al. Early trauma-induced coagulopathy is associated with increased ventilator-associated pneumonia in spinal cord injury patients. Shock. 2016;45(5):502–505. doi:10.1097/SHK.0000000000000531
38. Alastruey-Izquierdo A, Cadranel J, Flick H, et al. Treatment of chronic pulmonary aspergillosis: current standards and future perspectives. Respiration. 2018;96(2):159–170. doi:10.1159/000489474
39. Feng C, Zhang M, Zhang S, Zhang J, Li C, Zhou J. Therapeutic effects of pentoxifylline on invasive pulmonary aspergillosis in immunosuppressed mice. BMC Pulm Med. 2021;21(1):31. doi:10.1186/s12890-021-01396-8
40. Asemahagn MA. Sputum smear conversion and associated factors among smear-positive pulmonary tuberculosis patients in East Gojjam Zone, Northwest Ethiopia: a longitudinal study. BMC Pulm Med. 2021;21(1):118. doi:10.1186/s12890-021-01483-w
41. Long SM, Chern A, Feit NZ, et al. Percutaneous and open tracheostomy in patients with COVID-19: comparison and outcomes of an institutional series in New York City. Ann Surg. 2021;273(3):403–409. doi:10.1097/SLA.0000000000004428
42. Mubashir T, Arif AA, Ernest P, et al. Early versus late tracheostomy in patients with acute traumatic spinal cord injury: a systematic review and meta-analysis. Anesth Analg. 2021;132(2):384–394. doi:10.1213/ANE.0000000000005212
43. Wästfelt M, Cao Y, Ström JO. Predictors of post-stroke fever and infections: a systematic review and meta-analysis. BMC Neurol. 2018;18(1):49. doi:10.1186/s12883-018-1046-z
44. Rejeski K, Kunz WG, Rudelius M, et al. Severe Candida glabrata pancolitis and fatal Aspergillus fumigatus pulmonary infection in the setting of bone marrow aplasia after CD19-directed CAR T-cell therapy - a case report. BMC Infect Dis. 2021;21(1):121. doi:10.1186/s12879-020-05755-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
