Back to Journals » International Journal of General Medicine » Volume 16
Risk Factors for Negative Emotions in Patients Undergoing Radical Resection of Hilar Cholangiocarcinoma and Their Influence on Prognosis
Authors Yin R, Xu S, Zhu J, Zhu H, He C
Received 15 September 2023
Accepted for publication 21 November 2023
Published 11 December 2023 Volume 2023:16 Pages 5841—5853
DOI https://doi.org/10.2147/IJGM.S440469
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Hyam Leffert
Rong Yin, Shasha Xu, Jing Zhu, Haiou Zhu, Chao He
Department of Hepatobiliary Center Ward II, The First Affiliated Hospital of Nanjing Medical University, Nanjing, People’s Republic of China
Correspondence: Rong Yin, Department of Hepatobiliary Center Ward II, The First Affiliated Hospital of Nanjing Medical University, No. 300, Guangzhou Road, Nanjing, 210029, People’s Republic of China, Email [email protected]
Background: Hilar cholangiocarcinoma (HCCA) is a common malignant tumor of the biliary system. Factors such as limited physical function, intractability, and high mortality caused by the tumor lead to negative emotions, such as anxiety and depression in patients. In this study, we investigated the risk factors for negative emotions in patients undergoing radical resection of HCCA during the perioperative period and its effect on prognosis to provide strategies for alleviating the negative emotional disorders of patients and improving prognosis.
Methods: From September 2016 to August 2021, we retrospectively examined 205 patients with HCCA who underwent radical resection in our hospital. The incidence of negative emotions and the clinical parameters of patients were compared using Chi-square tests and t-tests. The independent risk factors for unfavorable feelings in patients during the perioperative period were determined using binary logistic regression. The key variables influencing the postoperative survival status of HCCA patients were identified using the log-rank univariate analysis and Cox proportional risk regression analysis.
Results: The results of the binary logistic regression analysis showed that perioperative negative emotions were independently influenced by family monthly income (OR = 0.069), medical insurance (OR = 0.089), family care (OR = 0.013), sleep quality (OR = 0.071), TNF-α (OR = 5.851), and bile leakage (OR = 29.412) (P < 0.05). The age of the patient (OR = 2.003), preoperative CA19– 9 (OR = 2.038), lymph node metastases (OR = 2.327), and negative mood (OR = 3.054) were independent risk variables that affected the survival status of patients, as determined by the results of Cox regression analysis (P < 0.05).
Conclusion: In this study, we found that anxiety and depression in patients undergoing radical operation of HCCA are related to family monthly income, medical insurance, sleep quality, family care, TNF-α, and bile leakage; also, negative emotions have adverse effects on prognosis.
Keywords: hilar cholangiocarcinoma, radical resection, depression, anxiety, risk factors, prognosis
Introduction
Hilar cholangiocarcinoma (HCCA), also known as Klatskin tumor, is a malignant tumor that occurs in the common hepatic duct, left and right hepatic duct, and hepatic duct confluence. HCCA accounts for 60–70% of the incidence of cholangiocarcinoma; it is the most common type of cholangiocarcinoma and has the worst prognosis among them.1,2 Although HCCA was an inoperable cancer earlier, in the past 20 years, with the advancement of imaging and surgical techniques, the diagnosis and treatment of HCCA have progressed considerably, the surgical resection rate has increased, and the survival rate has improved significantly.3,4 Radical resection is currently the only effective treatment for patients with HCCA to achieve long-term survival.5 However, due to the location and invasive growth of HCCA, it can invade blood vessels, nerves, lymph node tissues, and adjacent liver tissues very easily. The operation is difficult and risky, the long-term efficacy is unsatisfactory, and the postoperative complication rate is high.6,7
Due to physiological changes caused by cancer, surgical trauma, and toxic side effects of treatment, patients with HCCA have different degrees of psychological pressure and emotional disorders. This stress response can affect the level of cytokines secreted in the body, which in turn can affect the normal function of the body. These changes can result in a decrease in immunity and resistance, as well as, tissue and organ function disorders, which can threaten the health of patients and adversely affect their recovery.8,9 Some studies have shown that anxiety and depression are common mental health problems in patients with malignant tumors,10 but mental health problems are often at the edge of tumor treatment and are often underestimated and ignored. Among patients with malignant tumors in China, the incidence of anxiety is 32–40.0%, and the incidence of depression is 25.8–58.0%.11 Effectively solving the emotional problems of patients can reduce postoperative adverse consequences. At present, the pathogenesis of perioperative anxiety and depression in patients with HCCA is not clear. Few studies have investigated the influencing factors of anxiety and depression in patients with HCCA. Although the incidence of emotional disorders among patients with malignant tumors in clinics is high, the detection rate is low. The influence of psychological factors and the emotional status of patients with HCCA on their immunity and disease outcomes need to be investigated.
In recent years, the traditional medical model has shifted to the bio-psycho-social model.12 With an increase in the incidence of malignant tumors, researchers have focused on developing ways to perform psychological construction for cancer patients. The treatment of patients with HCCA should not only be limited to disease control but should also focus on improving their mental health, life span, and quality of life. Therefore, in this study, we investigated and analyzed the risk factors that might affect the perioperative negative emotions of patients undergoing HCCA radical surgery and the relationship with poor prognosis. Our findings provided novel information that can used in further clinical research and practice.
Materials and Methods
Research Participants
In this study, we included 205 patients who underwent radical resection of HCCA at The First Affiliated Hospital of Nanjing Medical University between September 2016 and August 2021.
The inclusion criteria were as follows: (I) patients who underwent pathological biopsy and were diagnosed according to the HCCA clinical diagnostic criteria; (II) patients with symptoms that were indications for HCCA radical resection; (III) those who were not provided any other anti-tumor treatment before and during the operation; (IV) patients with no major systemic illness; (V) patients who had full awareness and could communicate normally; (VI) patients with complete clinical data and who underwent complete follow-up after the operation; (VII) patients who signed the informed consent form.
The exclusion criteria were as follows: (I) patients who refused surgical treatment or changed surgical methods; (II) patients with other biliary system diseases; (III) patients with liver, kidney function, or other important organ insufficiency; (IV) patients with cardiovascular and cerebrovascular diseases or other malignant tumors; (V) patients with mental disorders, language disorders, or without complete awareness; (VI) patients with missing or lost clinical data (see Figure 1). The study was conducted according to the Declaration of Helsinki, and it was approved by the review committee of The First Affiliated Hospital of Nanjing Medical University.
 |
Figure 1 Study flowchart. |
Based on the guidelines to perform binary logistic regression and multiple linear regression, the ratio of item number to sample size must be between 1:5 and 1:10. Thus, 240 patients represented the sample size required for addressing the objective in this study. Due to 35 cases of patient loss and lack of follow-up, we included 205 cases in this study.
General Situation Questionnaire
The general information questionnaire included socio-demographic characteristics (gender, age, income, medical payment method, sleep quality, the degree of family care, etc.) and clinical characteristics (Bismuth-Corlette classification, tumor diameter, tumor differentiation, liver function and inflammatory indicators, complications, etc.).
Assessment of Negative Emotions
Using a questionnaire, we conducted an in-person survey focusing on the negative emotions of patients one week after surgery.
The self-rating anxiety scale (SAS) was used to evaluate whether the patients had anxiety and determine the degree of anxiety. The scale included 20 items, and each item could be given a score of 1–4. Anxiety had a standard score of 50; a score of 50–59 indicated mild anxiety, a score of 60–69 indicated moderate anxiety, and a score of 70 or higher indicated severe anxiety.13
The self-rating depression scale (SDS) was used to evaluate whether the patients had depression and the severity of depression. The scale contained 20 items, and each item could be given a score of 1–4. Depression had a standard score of ≥ 53; a score of 53–62 indicated mild depression, a score of 63–72 indicated moderate depression, and a score above 72 indicated severe depression.14
Karnofsky Performance Score
The Karnofsky Performance Score (KPS)15 is an index used to evaluate the functional activity of patients. A higher score indicates that the cancer patient can bear greater side effects of treatment. The evaluation standard is as follows: 100 points: normal, no signs and symptoms; 90 points: patients can perform normal activities, have mild signs and symptoms; 80 points: almost normal activities, there are some signs and symptoms; 70 points: patients can take care of themselves but cannot maintain normal life and work; 60 points: patients can perform basic self-care, occasionally need help; 50 points: patients often need care; 40 points: patients cannot take care of themselves, need special care and help; 30 points: patients are seriously unable to take care of themselves; 20 points: patients are seriously ill, need hospitalization and active support treatment; 10 points: critically ill, on the verge of death; 0 points: death.
Prognostic Score
The Eastern Cooperative Oncology Group (ECOG) Prognostic Score (PS) is used to evaluate the daily living abilities of cancer patients. According to the ability of daily life, from good to bad, it is divided into five grades. The scoring criteria are as follows: 0 points: patients can move normally; 1 point: patients with relatively mild symptoms can take care of themselves and engage in light physical activity; 2 points: patients have prominent symptoms, but they can take care of themselves, the time spent in bed during the day is no more than 50%; 3 points: patients have prominent symptoms; the time spent in bed is more than 50%, but patients can get up and stand; patients can take care of themselves; 4 points: patients with severe symptoms, bedridden; 5 points: patient dead.
Quality of Life Score
The Quality of Life (QOL) score is a common score for cancer patients. It is the comprehensive assessment of 12 aspects, which include appetite, sleep, spirit, fatigue, pain, family understanding and cooperation, understanding and cooperation of colleagues, the awareness of the patients regarding cancer, attitude toward treatment, daily life, side effects of treatment, and facial expressions. Quality of life classification: total score: 60; 51–60 indicates good; 41–50 indicates better; 31–40 indicates general; 21–30 indicates poor; < 20 indicates very poor.
Follow-Up Method
Patients were mainly followed up over the telephone and by outpatient or inpatient review; the follow-up deadline was September 2022. The survival time from the date of operation to the date of death of the patient or the last follow-up time was calculated in months. The patient was regarded as “lost to follow-up” if they died due to another illness. The postoperative survival status, tumor recurrence, and metastasis were the key points evaluated during the follow-up.
Statistical Analysis
All data in this study were analyzed by the SPSS 26.0 software. The difference in count data was compared by conducting an independent samples t-test, and the difference in measurement data was compared by a Chi-square test. Binary logistic regression was used to analyze the independent risk factors for the negative emotions of patients. The Kaplan-Meier method was used to calculate the survival rate and plot the survival curve. The difference was compared by the Log rank test. The influencing factors for survival prognosis were analyzed by the Cox proportional regression analysis. All results were considered to be statistically significant at P < 0.05.
Results
Comparison of Perioperative SAS Score and SDS Score in Patients
The baseline data of patients are presented in Table 1. The results showed significant differences between SAS and SDS scores in the family monthly income, medical insurance, differentiation of tumors, and vascular invasion (P < 0.05). Sleep quality was significantly different in the SAS scores (P < 0.05), whereas family care degree was significantly different in the SDS scores (P < 0.05) (Table 1).
 |
Table 1 Comparison of Perioperative SAS Score and SDS Score in Patients (Mean ± SD) |
Comparison of Liver Function and Inflammatory Indices Between the Two Groups on the Third Day After Operation
The results of the experimental examination on the third day after operation showed that the mean values of TNF-α, ALP, γ-GT, TBIL, and WBC in patients with negative emotions were 4.36±0.86 μg/L, 113.45±30.67 U/L, 153.12±19.67 U/L, 187.18±35.92 µmol/L, and 13.61±4.15 ×109/L, respectively. The mean values of TNF-α, ALP, γ-GT, TBIL, and WBC in patients without negative emotions were 3.77±0.76 μg/L, 100.78±23.56 U/L, 136.32±26.94 U/L, 164.02±41.28 µmol/L, and 11.21±3.31 ×109/L, respectively. The differences in TNF-α, ALP, γ-GT, TBIL, and WBC between patients with and without negative emotions were significant (P < 0.05) (Table 2).
 |
Table 2 Comparison of Liver Function and Inflammatory Indexes Between the Two Groups on the Third Day After Operation (Mean±SD) |
Comparison of Postoperative Complications in Patients with and without Negative Emotions
Among the patients with postoperative incision infections, 16 patients had negative emotions and 13 patients had no negative emotions. Among the patients with bile leakage, 14 patients had negative emotions, and 9 patients had no negative emotions. Among all postoperative complications, the incidence of incision infection and bile leakage was significantly different between patients with and without negative emotions (P < 0.05) (Table 3).
 |
Table 3 Comparison of Postoperative Complications in Patients with or Without Negative Emotions (n, %) |
Binary Logistic Regression Analysis of Negative Emotional Risk Factors in Patients
The results of the binary logistic regression analysis showed that family monthly income (OR = 0.069), medical insurance (OR = 0.089), family care degree (OR = 0.013), sleep quality (OR = 0.071), TNF-α (OR = 5.851), and bile leakage (OR = 29.412) were independent risk factors for perioperative negative emotions (P < 0.05) (Table 4).
 |
Table 4 Binary Logistic Regression Analysis of Negative Emotional Risk Factors in Patients |
Comparison of PS, KPS, and QOL Scores Between the Groups After Radical Resection of HCCA
The differences in the PS, KPS, and QOL scores between the groups were significant (P < 0.05). The PS, KPS, and QOL scores of patients without negative emotions were better than those of patients with negative emotions (Table 5).
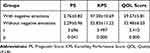 |
Table 5 Comparison of PS, KPS and QOL Scores Between the Two Groups After Radical Resection of HCCA |
Univariate Analysis of Postoperative Survival of HCCA Patients
The results of the univariate analysis showed that age, preoperative CA19-9, preoperative CEA, tumor differentiation, lymph node metastasis, vascular invasion, and combined negative emotions were the factors that significantly affected the prognosis of patients (P < 0.05) (Table 6).
 |
Table 6 Univariate Analysis of Postoperative Survival in HCCA Patients n (%) |
Cox Risk Regression Analysis of Factors Related to Postoperative Survival Status of Patients
The results of Cox regression analysis showed that negative emotions (OR = 3.054), age (OR = 2.003), preoperative CA19–9 (OR = 2.038), and lymph node metastasis (OR = 2.327) were the independent risk factors that affected the survival of patients (P < 0.05) (Table 7 and Figure 2).
 |
Table 7 Cox Risk Regression Analysis of Factors Related to Postoperative Survival of Patients |
Discussion
The results of our analysis showed that family monthly income, medical insurance, sleep quality, family care, TNF-α, and bile leakage are independent risk factors for negative emotions in patients undergoing radical resection of HCCA. It has been reported that economic conditions also play a key role in the occurrence of depression in cancer patients. High income is a protective factor for cancer patients with depression.16 Many studies in China also found that economic burden is the influencing factor in anxiety and depression. The results of this study showed that patients with good economic income (family monthly income ≥6000 yuan) have mild symptoms of anxiety and depression. Because HCCA is a disease with complex treatment methods and high medical costs, patients with a low family income often need to bear a greater economic burden, which makes these patients prone to anxiety, depression, and other negative emotions. Patients with high family incomes can choose more suitable medical resources during treatment to improve clinical symptoms and treatment effects. Additionally, medical insurance can reimburse part of the surgical treatment cost and chemotherapy cost, which can reduce the financial pressure on patients to a certain extent. Patients who do not have medical insurance need to pay for medical expenses directly from their income; therefore, they worry about the burden of high costs of treatment and chemotherapy, which increases their psychological pressure.17 Anxiety and depression affect the quality of sleep; lack of sleep and poor sleep quality adversely affect mood quality.18 The results of this study showed that patients with poor sleep quality had more significant symptoms of anxiety. Induru19 reported that the incidence of sleep disorders in cancer patients was high in a study on cancer-related insomnia. Sleep disorder is also a common complaint in patients with HCCA; pain and postoperative adverse reactions are the main causes of poor sleep and even insomnia. Additionally, the discomfort caused by various drainage tubes after the operation and the worry about prognosis affects the sleep of patients with HCCA. Some studies have shown that long-term sleep deprivation can lead to an imbalance of hormones in the body, affect the normal function of neurotransmitters, and then, affect emotional stability.20 Therefore, taking effective analgesic treatment for patients with HCCA on time after operation is important. Also, it is necessary to strengthen drainage tube nursing to decrease the discomfort of patients as much as possible to improve their sleep. Other studies have found that family care can also affect the emotions of patients. Because patients with HCCA not only suffer from physical pain but also from serious psychological trauma, they need more care and comfort from their relatives. Good family care can provide patients with HCCA with more material and emotional support, which can effectively alleviate the bad mood of patients. It can also improve the confidence and enthusiasm of patients with HCCA for treating diseases. In contrast, inadequate family care may increase the self-burden of patients with HCCA and provide them with no opportunity to express their feelings, which can lead to major negative emotions. Therefore, besides offering psychological assistance to patients, medical professionals should urge families to provide patients with greater emotional support and companionship so that patients may find spiritual support, security, and emotional support to decrease their psychological burden.
The results also showed that TNF-α was an influencing factor of negative emotions in patients with HCCA. We speculated that inflammatory response might be one of the key factors inducing depression in patients with HCCA. TNF-α is an important member of inflammatory cytokines. It plays a key role in the development of depression by regulating the synthesis, metabolism, and reuptake of monoamine neurotransmitters, causing excessive activation of the Hypothalamo-pituitary-adrenal (HPA) axis and impairing its negative feedback regulation, activating indoleamine 2,3-dioxygenase (IDO), and other mechanisms.21–23 Additionally, the occurrence of complications can adversely affect the physiology and psychology of HCCA patients. Patients suffer from depression, despair, and a reduction of self-efficacy, which causes them to lose confidence in treatment and even give up treatment in some cases; this can eventually lead to poor clinical treatment.24 Therefore, we should not only pay attention to the mental health of patients with HCCA but also focus on the indicators of patients and take timely measures to prevent the occurrence of complications, improve the prognosis, and prolong overall survival.
Some studies have found that anxiety and depression can activate the neuroendocrine-immune regulation system, destroy the cellular immune function, and induce tumor progression, and form a vicious circle.9 Negative emotions such as anxiety and depression can also lead to a loss of appetite, insomnia, and other adverse effects, further reducing the immune function of patients and the effectiveness of clinical treatment.25 The results of this study showed that negative emotion was a factor affecting the prognosis of patients undergoing radical resection of HCCA. A comparison of the quality of life scores (PS, KPS, and QOL) between patient groups indicated that the scores of patients with negative emotions were worse than those without negative emotions, indicating that negative emotions might negatively affect the prognosis of patients undergoing radical resection of HCCA. Therefore, the mental health problems of patients should be highly valued in clinical practice.
The results of the Cox regression analysis showed that age, preoperative CA19–9, and lymph node metastasis were also independent risk factors affecting the prognosis of patients with HCCA. HCCA generally occurs in middle-aged and elderly people over 50 years old. Many studies have reported that age affects the prognosis of malignant tumors,26 but so far, there are few reports on the relationship between age and HCCA prognosis. In the present study, we found that patients who were ≥ 65 years old had a poorer prognosis than patients who were below 65 years old, which might be related to the yearly decrease in immune function and poor general physical state of older patients. Elderly patients are often accompanied by chronic diseases, such as hypertension, diabetes, and heart disease, and their general health condition is relatively poor. Hence, the scope of intraoperative lymph node dissection is limited, which increases the chances of tumor recurrence and metastasis, thus leading to a poor prognosis. CA19–9 is the most commonly used diagnostic marker for biliary system tumors and an important prognostic marker for patients undergoing radical resection of HCCA. Some studies have shown that a higher preoperative CA19–9 level is an important factor in reducing the survival rate of HCCA patients.27 The results of the univariate analysis showed that the survival rate of patients with a preoperative CA19–9 level ≥ 150 U/mL was lower than that of patients with a preoperative CA19–9 < 150 U/mL, which was consistent with the above conclusions. Relevant literature reports that the probability of lymph node metastasis in HCCA is as high as 30–50%, which is an important factor affecting the survival of patients.28,29 We found that in 108 cases of lymph node metastasis, the incidence rate was 52.6%, and the one-year survival rate was 61.6%. This occurred because the lymphatic tissue around the biliary tract is rich, the tumor cells are easy to invade and metastasize, and they can metastasize with the lymphatic distribution and the intrahepatic and extrahepatic bile ducts, as well as, along the nerve lymph node space in the duodenal ligament.30 The difficulty in intraoperative dissection leads to prolonged operation time, an increase in complications, and a greater risk of postoperative recurrence and metastasis. Thus, the overall prognosis of patients with lymph node metastasis is poor.
Our study had some limitations. This was a single-center retrospective study with a small sample size and short follow-up time. The effect of negative emotions on the prognosis of patients with HCCA needs to be further evaluated by conducting larger prospective studies.
Conclusion
Anxiety and depression in patients undergoing radical operation for HCCA were found to be related to family monthly income, medical insurance, sleep quality, family care, TNF-α, and bile leakage. Negative emotions were found to have adverse effects on prognosis. In clinical work, communication with patients should be strengthened, and the emotional abnormalities of patients should be determined at the earliest to provide practical solutions, so as to fundamentally reduce the degree of anxiety and depression of patients, enhance their survival rate, and improve the prognosis.
Ethical Statement
The study was conducted following the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of The First Affiliated Hospital of Nanjing Medical University (No. 23134533). Informed consent was obtained from all patients.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no financial support for this study.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Lauterio A, De Carlis R, Centonze L, et al. Current surgical management of peri-hilar and intra-hepatic cholangiocarcinoma. Cancers. 2021;14(1):13. doi:10.3390/cancers13153657
2. Klatskin G. adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. An unusual tumor with distinctive clinical and pathological features. Am J Med. 1965;38(2):241–256. doi:10.1016/0002-9343(65)90178-6
3. Ma D, Wang W, Wang J, et al. Laparoscopic versus open surgery for hilar cholangiocarcinoma: a retrospective cohort study on short-term and long-term outcomes. Surg Endosc. 2022;36(6):3721–3731. doi:10.1007/s00464-021-08686-6
4. He YG, Huang W, Ren Q, et al. Comparison of efficacy and safety between laparoscopic and open radical resection for hilar cholangiocarcinoma-a propensity score-matching analysis. Front Oncol. 2022;12:1004974. doi:10.3389/fonc.2022.1004974
5. Zhang Y, Dou C, Wu W, et al. Total laparoscopic versus open radical resection for hilar cholangiocarcinoma. Surg Endosc. 2020;34(10):4382–4387. doi:10.1007/s00464-019-07211-0
6. Saxena A, Chua TC, Chu FC, et al. Improved outcomes after aggressive surgical resection of hilar cholangiocarcinoma: a critical analysis of recurrence and survival. Am J Surg. 2011;202(3):310–320. doi:10.1016/j.amjsurg.2010.08.041
7. Nagino M, Ebata T, Yokoyama Y, et al. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 2013;258(1):129–140. doi:10.1097/SLA.0b013e3182708b57
8. Lopez RB, Denny BT, Fagundes CP. Neural mechanisms of emotion regulation and their role in endocrine and immune functioning: a review with implications for treatment of affective disorders. Neurosci Biobehav Rev. 2018;95:508–514. doi:10.1016/j.neubiorev.2018.10.019
9. Wang YH, Li JQ, Shi JF, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2020;25(7):1487–1499. doi:10.1038/s41380-019-0595-x
10. Akechi T. Psycho-oncology: history, current status, and future directions in Japan. Jma j. 2018;1:22–29. doi:10.31662/jmaj.2018
11. Yang YL, Liu L, Wang Y, et al. The prevalence of depression and anxiety among Chinese adults with cancer: a systematic review and meta-analysis. BMC Cancer. 2013;13(1):393. doi:10.1186/1471-2407-13-393
12. Chen LH, Law W, Chang DHF, et al. Editorial: the bio-psycho-social approach to understanding mental disorders. Front Psychol. 2023;14:1225433. doi:10.3389/fpsyg.2023.1225433
13. Liu H, Wu F, Liao G, et al. Impact of the intensive psychological intervention care on post-traumatic stress disorder and negative emotions of teenage female patients seeking an induced abortion. Front Psychiatry. 2023;14:1033320. doi:10.3389/fpsyt.2023.1033320
14. Du J, Kang Z, Zhao Z, et al. Analysis of the effect of Ivor-Lewis esophagectomy and McKeown esophagectomy on perioperative anxiety and depression in patients with esophageal cancer. Eur J Cancer Prev. 2023. doi:10.1097/CEJ.0000000000000850
15. Perez Valdivieso JR, Bes-Rastrollo M, Monedero P, et al. Karnofsky performance score in acute renal failure as a predictor of short-term survival. Nephrology. 2007;12(6):533–538. doi:10.1111/j.1440-1797.2007.00880.x
16. Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 2013;22(4):745–755. doi:10.1002/pon.3055
17. Van Beek FE, Wijnhoven LMA, Holtmaat K, et al. Psychological problems among cancer patients in relation to healthcare and societal costs: a systematic review. Psychooncology. 2021;30(11):1801–1835. doi:10.1002/pon.5753
18. Acker KA, Carter P. Sleep-wake disturbances in oncology. Nurs Clin North Am. 2021;56(2):175–187. doi:10.1016/j.cnur.2021.03.001
19. Induru RR, Walsh D. Cancer-related insomnia. Am J Hosp Palliat Care. 2014;31(7):777–785. doi:10.1177/1049909113508302
20. Huang V, Mackin L, Kober KM, et al. Distinct sleep disturbance and cognitive dysfunction profiles in oncology outpatients receiving chemotherapy. Support Care Cancer. 2022;30(11):9243–9254. doi:10.1007/s00520-022-07350-6
21. Hassamal S. Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories. Front Psychiatry. 2023;14:1130989. doi:10.3389/fpsyt.2023.1130989
22. Sublette ME, Postolache TT. Neuroinflammation and depression: the role of indoleamine 2,3-dioxygenase (IDO) as a molecular pathway. Psychosom Med. 2012;74(7):668–672. doi:10.1097/PSY.0b013e318268de9f
23. Chen H, Huang X, Zeng C, et al. The role of indoleamine 2,3-dioxygenase 1 in early-onset post-stroke depression. Front Immunol. 2023;14:1125634. doi:10.3389/fimmu.2023.1125634
24. Elberg Dengsø K, Hillingsø J, Marcussen AM, et al. Health-related quality of life and anxiety and depression in patients diagnosed with cholangiocarcinoma: a prospective cohort study. Acta Oncol. 2017;56(2):198–204. doi:10.1080/0284186x.2016.1266088
25. Niedzwiedz CL, Knifton L, Robb KA, et al. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer. 2019;19(1):943. doi:10.1186/s12885-019-6181-4
26. Popescu I, Dumitrascu T. Curative-intent surgery for hilar cholangiocarcinoma: prognostic factors for clinical decision making. Langenbecks Arch Surg. 2014;399(6):693–705. doi:10.1007/s00423-014-1210-x
27. Sun Z, Feng Y, Liu H, et al. Analysis of treatment methods and prognostic factors in 354 cases of hilar cholangiocarcinoma: a cohort study. J Cancer Res Ther. 2020;16(2):230–237. doi:10.4103/jcrt.JCRT_637_19
28. Guan JF, Wang K. 肝门部胆管癌术中淋巴结清扫的研究现状[Current status of intraoperative lymph node dissection for hilar cholangiocarcinoma]. Zhonghua Wai Ke Za Zhi. 2020;58(1):48–51. Chinese. doi:10.3760/cma.j.issn.0529-5815.2020.01.011
29. Hu HJ, Mao H, Shrestha A, et al. Prognostic factors and long-term outcomes of hilar cholangiocarcinoma: a single-institution experience in China. World J Gastroenterol. 2016;22(8):2601–2610. doi:10.3748/wjg.v22.i8.2601
30. Liang L, Li C, Wang MD, et al. The value of lymphadenectomy in surgical resection of perihilar cholangiocarcinoma: a systematic review and meta-analysis. Int J Clin Oncol. 2021;26(9):1575–1586. doi:10.1007/s10147-021-01967-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

