Back to Journals » Infection and Drug Resistance » Volume 16
Risk Factors Associated with Multi-Drug Resistance in Neonatal Sepsis Caused by Escherichia coli
Authors Zhu M, Wang L, Zhuge Z, Li W, Zheng Y , Mai J, Lin Z , Lin J
Received 30 December 2022
Accepted for publication 23 March 2023
Published 10 April 2023 Volume 2023:16 Pages 2097—2106
DOI https://doi.org/10.2147/IDR.S403135
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Minli Zhu,1 Leying Wang,1 Zhangming Zhuge,1 Wei Li,1,2 Yihui Zheng,1 Jingyun Mai,1 Zhenlang Lin,1 Jing Lin1,3
1Key Laboratory of Perinatal Medicine of Wenzhou, Department of Neonatology, the Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, 325027, People’s Republic of China; 2Zhijin People’s Hospital of Guizhou Province, Guizhou, 552100, People’s Republic of China; 3Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, NY, 10029, USA
Correspondence: Jing Lin, Department of Pediatrics, Icahn School of Medicine at Mount Sinai, One Gustave Levy Place, New York, NY, 10029, USA, Tel +1-212-241-6186, Fax +1-212534-5207, Email [email protected] Zhenlang Lin, Department of Neonatology, the Second Affiliated Hospital and Yuying Children’s Hospital, Wenzhou Medical University, Wenzhou, 325027, People’s Republic of China, Tel +86 13806689800, Email [email protected]
Background and Objective: An increasing number of cases of neonatal sepsis due to extended-spectrum beta-lactamase (ESBL)-producing multi-drug resistant (MDR) Escherichia coli (E. coli) have been reported worldwide. The aim of this study was to explore the risk factors associated with ESBL-producing MDR E. coli among neonates with culture-confirmed E. coli sepsis and thereby to help selection of appropriate empirical antibiotics.
Patients and Methods: All newborn infants with a confirmed pathogen isolated from blood or cerebrospinal fluid (CSF) from 2016 to 2021 were identified and those with E. coli infection were included in this analysis. We compared a group of neonatal patients with ESBL-producing MDR E. coli sepsis (n=69) to a group with ESBL-negative E. coli (n=70) based on antimicrobial susceptibility reports. We used multivariable regression analysis to determine the risk factors associated with ESBL-producing MDR E. coli strains among the neonates with culture-confirmed E. coli sepsis.
Results: ESBL-producing MDR E. coli sepsis was more common in premature infants and newborns with hospital-acquired late-onset sepsis (HALOS). The mortality rate of neonatal sepsis caused by ESBL-producing E. coli was about twice as that of sepsis caused by ESBL-negative E. coli. Antepartum exposure to cephalosporins (OR=25.191, 95% CI: 3.184– 199.326, P< 0.01) and parenteral nutrition for more than 1 week (OR=4.495, 95% CI: 2.009– 10.055, P< 0.01) were independent risk factors for neonatal infection with ESBL-producing stains among infants with E. coli sepsis.
Conclusion: E. coli remains the most common Gram-negative bacterial pathogen causing neonatal sepsis. A higher proportion of ESBL-producing MDR E. coli is seen in premature infants and those newborns with HALOS and is associated with higher mortality. Antepartum use of cephalosporins and prolonged use of parenteral nutrition may be important factors to consider in the selection of empirical antibiotics for use in neonatal sepsis caused by gram-negative rods prior to the availability of the results of antimicrobial susceptibility.
Keywords: infant, newborn, neonatal sepsis, Escherichia coli, drug resistance, extended-spectrum beta-lactamase
Introduction
Neonatal sepsis is a major cause of neonatal mortality and therefore a significant global health issue. The reported incidence of neonatal sepsis is about 1–4%,1 with a higher incidence being reported in developing countries.1,2 To reduce neonatal mortality and long term adverse consequences caused by bacterial infection, it is vital to select appropriate empirical antibiotics when a neonatal infection is suspected. In most developing countries, including China, Escherichia coli (E. coli) is usually the leading pathogen in neonatal sepsis,2–7 especially in premature infants.1,8–10 E. coli plays an important role in causing both early-onset sepsis (EOS) and late-onset sepsis (LOS).3,6–8,11–14 E. coli is also one of the most common pathogenic bacteria causing neonatal bacterial meningitis.15–17 Neonate with E. coli meningitis can have adverse nervous system sequelae, which is an important cause of poor long-term prognosis of newborns with E. coli sepsis.
Selection and timely administration of antibiotics to which the bacteria is sensitive to has important clinical significance for improving the prognosis of neonates with bacterial infections. The first-line empirical antibiotic regimen should be selected to cover E. coli and other common local pathogens based upon their historical antimicrobial sensitivity patterns. Recently, increasing reports show that the proportion of multi-drug resistant (MDR) E. coli is rising,6,18,19 which brings big challenges to clinicians. Our recent meta-analysis based on a systematic review of the published studies in the Chinese literature demonstrates that in newborn infants hospitalized in Chinese NICUs, roughly 50% of all E. coli bloodstream isolates, whether early or late onset, are MDR due to extended spectrum beta-lactamase (ESBL) production.20 We have further demonstrated that ESBL-producing MDR E. coli has emerged as the major pathogen responsible for EOS, particularly in preterm infants.5
The main mechanism of MDR gram-negative Enterobacteriaceae such as E. coli is ESBL production.21,22 In neonatal intensive care units (NICUs) with a high prevalence of ESBL-producing Enterobacteriaceae infections, carbapenem antibiotics are usually selected for gram-negative bacterial infections before antimicrobial susceptibility test results are available. The abuse of carbapenem antibiotics has led to the emergence of carbapenem-resistant Enterobacteriaceae (CRE) which may be resistant to all available antibiotics.23 Therefore, it is urgent for most NICUs to have an antibiotic stewardship program to reduce the abuse of broad-spectrum antibiotics. In the current study, we compared the clinical characteristics of a group of hospitalized neonates with culture-confirmed ESBL-producing E. coli sepsis with a group infected with ESBL-negative E. coli in order to determine the potential risk factors associated with ESBL-producing MDR E. coli infection among the neonates with confirmed E. coli sepsis. These results may inform the selection of appropriate empirical antibiotics before antimicrobial susceptibility results are available in the future.
Materials and Methods
Data Collection
This is an observational cohort study based on prospectively collected data on infants with positive blood culture results from the Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University. Starting in 2016, all infants with a positive blood or cerebrospinal fluid (CSF) culture have been recorded in our specific neonatal sepsis database. For the current study, all infants with a confirmed pathogen isolation from blood or CSF from 2016 to 2021 were identified and those with E. coli infection were included in the study for further analysis.
The detailed medical history and relevant clinical data of neonates with confirmed E. coli sepsis were retrospectively retrieved from the hospital electronic medical records. The information collected includes basic demographic information, perinatal factors, antimicrobial susceptibility tests, and pre-infection conditions. If a patient had multiple positive cultures during hospitalization, only the first result was included to avoid overrepresentation. Cases with incomplete data were excluded. EOS with E. coli is defined as the presence of E. coli grown from blood or CSF in cultures drawn in any newborn infant within 72 hours of birth. LOS is arbitrarily further divided into community acquired and hospital-acquired. Community acquired late-onset sepsis (CALOS) with E. coli infection is defined as the isolation of E. coli from blood or CSF from outpatients >72 hours after birth or inpatients >72 hours after birth and within 48 hours of re-admission into hospital. Hospital-acquired late-onset sepsis (HALOS) with E. coli infection is defined as the isolation of E. coli from blood or CSF from hospitalized infant >72 hours after birth. The definition of previous antibiotic use was that antibiotics were administered intravenously for more than 48 hours prior to culture collection. The Institutional Ethics Committee of the Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University approved the study protocol. A waver for parental consent to review medical records was granted by the Institutional Ethics Committee. The handling of the patient data confidentiality strictly followed the rules set by the institution and were in compliance with the Declaration of Helsinki.
Bacterial Identification and Antimicrobial Susceptibility Testing
The clinical laboratory in our hospital employs routine microbiological tests according to the standard set by the Clinical & Laboratory Standards Institute (CLSI, USA). Bacterial identification was accomplished using a MALDI-TOF/MS mass spectrometer (Bruck, Germany). Bacterial drug sensitivity testing was conducted using the Vitek2 Compact automated drug susceptibility analyzer (Mérieux, France) or disk diffusion method (30ug, British OXOID). The Gram-Negative Susceptibility card (BioMerieux, France) was utilized to determine antibiotic susceptibility of bacterial isolates. ESBL-producing strains were identified by the double-disk synergy method.24 Results were interpreted following the recommendations and definitions of the CLSI.
Statistical Analysis
Statistical analysis and production of graphs were performed using SPSS Statistics (version 24; IBM Corp, Armonk, NY) and GraphPad Prism (version 9.0; GraphPad Software, La Jolla, CA, USA), respectively. The normality of continuous variables was tested using the Kolmogorov–Smirnov test. Normally distributed data were presented as the mean ± standard deviation (M±SD) and were analyzed using the Student’s t-test. Non-normally distributed data were described as median (25–75 percentile) and were analyzed using the Mann–Whitney U-test. Homogeneity test was used to check whether the variance of the data is homogeneous. For more than two groups, analysis of variance (ANOVA) was used for normal and homogeneous data, and Kruskal–Wallis H-test was used for non-normal data. When ANOVA results identified the statistical difference among the groups, post hoc tests were used to determine the significance between the particular pairs of means. Categorical variables were compared using the chi-square test or Fisher’s exact test. The level of significance was set at P < 0.05. Multivariable logistic regression was conducted to determine the risk factors associated with infection by an ESBL+ strains in neonates with confirmed E. coli infection. All relevant variables significantly associated with ESBL+ strains in the univariate analysis were entered into the model. A stepwise selection was used with an alpha-to-enter and alpha-to-exit set at 0.10 and 0.05, respectively. The odds ratio (OR) and 95% confidence intervals (CIs) were reported.
Results
During the study period, a total of 21,439 newborns were admitted to the NICU of the Second Affiliate Hospital and Yuying Children’s Hospital of Wenzhou Medical University, of which 233 were diagnosed with gram-negative bacterial sepsis. Of the 233 cases, 141 (60.5%) were confirmed to be E. coli sepsis. After careful review of the cases, 2 patients were excluded due to incomplete data, and the remaining 139 cases were included in the analysis. Among these, 69 cases were reported to be ESBL-producing and 70 cases were reported to be ESBL-negative E. coli, as shown as flow diagram in Figure 1.
 |
Figure 1 Screening flowchart of research subjects. |
Of the total 139 strains of E. coli identified from the blood or CSF samples sent from the neonates in our NICU from 2016 to 2021, the proportion of ESBL producing E. coli among all E. coli isolates each year is presented in Figure 2. It fluctuated and decreased to the lowest value of 31.6% in 2019. Since then, the proportion of ESBL-producing strains has gradually increased, rising to 66.7% in 2021.
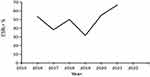 |
Figure 2 The proportion of ESBL+ in all E. coli isolates from 2016 to 2021. |
Based on the timing of initial culture and hospitalization status, all enrolled patients were divided into EOS, CALOS and HALOS groups for further analysis. As shown in Table 1, the gestational age and birth weight of infants in the CALOS group were significantly higher than those in the other two groups, while the proportions of in vitro fertilization (IVF), multiples and prolonged rupture of membrane (PROM) in the HALOS group were significantly higher than that in the other two groups (P<0.05). While all E. coli strains isolated from enrolled patients were still sensitive to Amoxicillin/clavulanic acid, amikacin, and carbapenem, the proportion of ESBL-producing stains was significantly higher in the HALOS group, and as the results, the antimicrobial resistance rates to gentamycin, ceftriaxone, ceftazidime and cefepime were also significantly higher in the HALOS group (Figure 3).
 |
Table 1 The Basic Clinical Characteristics of the Three Types of Neonatal E. coli Sepsis |
 |
Figure 3 Antimicrobial resistance rate of E. coli isolated from three different types of neonatal sepsis. *P < 0.05. |
Comparisons of the basic clinical characteristics between the ESBL-producing and ESBL-negative groups are presented in Table 2. As shown in the table, the birth weight and gestational age (GA) of children in ESBL-producing group were significantly lower than those in ESBL-negative group (P<0.05). There were no statistically significant differences between ESBL-producing and ESBL-negative groups in gender, mode of delivery, multiple births, maternal diabetes, maternal chorioamnionitis, low Apgar scores, EOS ratio, and exclusive breastfeeding (P>0.05). However, the proportion of pregnant women with age >35y, use of prenatal antibiotics, IVF, PROM, proportion of HALOS, and antepartum cephalosporins use in the ESBL-producing group were significantly higher than that in the ESBL-negative group (P<0.05). The proportion of CALOS in ESBL-producing group is lower, while that of HALOS is higher (P<0.05). Characteristics prior to infection indicated that babies in the ESBL-producing group had longer hospitalization prior to infection, were more likely to have central lines, had greater use of antibiotics, were more likely to be on mechanical ventilation, and more often receiving parental nutrition for greater than 1 week. For clinical complications and outcomes, the mortality of ESBL-producing group was significantly higher than that of ESBL-negative group, but there was no significant difference in the proportion of children with meningitis, septic shock between the two groups (Table 3).
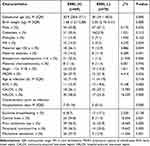 |
Table 2 Comparison of the Basic Clinical Characteristics Between the Two Groups |
 |
Table 3 Comparison of Clinical Complications and Outcomes Between the Two Groups |
To determine the risk factors associated with an ESBL-producing strain among all infants with confirmed E. coli sepsis, a multivariate logistic regression analysis was conducted. All relevant variables with P<0.1 in univariate analysis were included in the model. As shown in Table 4, antepartum exposure to cephalosporins (OR=25.191, 95% CI: 3.184–199.326, P=0.002) and parenteral nutrition for more than 1 week (OR=4.495, 95% CI: 2.009–10.055, P=0.000) were independent risk factors of neonatal infection with ESBL-producing stain among infants with E. coli sepsis. In this multivariate logistic regression model, all other variables included in the model appear to be covariates and, therefore, not independent risk factors with statistical significance.
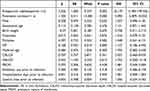 |
Table 4 Logistic Regression Analysis of Risk Factors for Neonatal MDR E. coli Sepsis |
Discussion
An increasing number of cases of neonatal sepsis due to ESBL-producing MDR E. coli have been reported worldwide.5,6,18,19 In this study, we collected data on hospitalized neonates with culture-confirmed E. coli infection and analyzed the risk factors associated with ESBL-producing strains among the neonates with confirmed E. coli infection. We demonstrate that E. coli remains the most common Gram-negative bacterial pathogen for neonatal sepsis, which is similar to the reports both from China and other countries.2,4 We further demonstrate that antepartum maternal exposure to cephalosporins and parenteral nutrition for longer than 1 week are strong and independent risk factors associated with neonatal infection with ESBL-producing stains among infants with culture-confirmed E. coli sepsis.
ESBL-producing E. coli represents a major worldwide threat among MDR bacteria in both hospital and community settings. ESBLs are often located on large plasmids that also harbor genes resistant to other antimicrobial classes, resulting in MDR isolates.19,25 Our data show that the overall incidence of neonatal E. coli sepsis in our hospitalized neonates was 0.65% (141/21,439) in the last 6 years and that half of those were ESBL-producing strains. The mortality rate in ESBL+ group was significantly higher than that of the ESBL-negative group (24.6% vs 11.4%). These findings are consistent with other reports that the mortality of neonatal sepsis caused by ESBL producing Enterobacteriaceae is twice as high as that of all other bloodstream infections.6,26,27 As a consequence, the increase in the prevalence of ESBL-producing Enterobacteriaceae infection is associated with significant increase in neonatal mortality.28
Previous study demonstrated that in EOS, the MDR rate was higher in preterm infants when compared to that of full-term infants.5 In the current study, we found that E. coli isolated from HALOS had the highest proportion of ESBL-producing strains, followed by EOS. E. coli isolated from CALOS had the lowest rate of ESBL positivity. By comparing the different types of neonatal sepsis caused by E. coli, we found that the three groups had statistically significant differences in gestational age, birth weight, rates of multiples, IVF, antenatal antibiotic therapy, and PROM. Giannoni et al reported that HALOS occurred in lower gestational age infants and CALOS was more commonly seen in full-term infants and boys,29 similar to the findings in our study. Antenatal antibiotic therapy and PROM were more common in EOS. Multiples and IVF, which usually associated with lower gestational age, were more common in HALOS. A recent multicenter study across China also showed similar ESBL positivity rate and patterns of E. coli strains among hospitalized neonates.30
Univariate statistical analysis showed that there were differences in many variables between the ESBL-producing group and the ESBL-negative group. Babies in ESBL-producing group had a lower gestational age and birth weight, longer hospitalization time before infection, were more likely to have central lines, more often on mechanical ventilation, higher chance be on parenteral nutrition for more than 1 week, and received antibiotics before onset of sepsis. Babies in the ESBL-producing group were also more like to be a product of an IVF, to have mother’s age over 35 years, to be exposed to antepartum cephalosporins, and PROM. Most of the above factors were high-risk factors of nosocomial infection. Therefore, nosocomial infection was more common in the ESBL-producing group, while community infection was more common in the ESBL-negative group. Premature infants, especially those with very low birth weight, usually have prolonged stay in the NICU and are at increased risk for hospital-acquired infections. Most premature infants also have a history of antibiotic exposure. Abuse of third-generation cephalosporins and other broad-spectrum β-lactam antibiotics in NICUs can easily induce the production of ESBL in gram-negative pathogens, which leads to more MDR E. coli infections in premature infants. It has been reported that restricting overall cephalosporin use can significantly reduce the incidence of ESBL-producing gram-negative bacterial infection.31
Previous studies on risk factors related to ESBL-producing Enterobacteriaceae mainly focused on hospital-acquired infection or colonization. No comprehensive studies include analysis involving early onset neonatal sepsis and community-acquired sepsis.32–35 A meta-analysis has revealed that many risk factors were related to infection and/or colonization with ESBL-producing bacteria in NICUs.36 Interestingly, by using multivariate logistic regression analysis, we found that only prenatal cephalosporin use and prolonged use of parenteral nutrition were independent risk factors for MDR E. coli infection, indicating that most other factors that significantly differed between the ESBL-producing and ESBL-negative groups by univariate analysis were covariates. Indeed, the antenatal use of cephalosporins in mothers increases the possibility of colonization of MDR bacteria in the birth canal and increases the chance of infection of ESBL-producing E. coli in neonates both as EOS and LOS. A single-center study in Sri Lanka tested 159 pairs of maternal vaginal swabs and neonatal perianal swabs. Random amplification of polymorphic DNA analysis revealed that Enterobacteriaceae with same strain type was present in 6.9% of the mother-infant pairs, indicating possible transfer between the mother and neonate.37 In addition, vaginal bacteria colonization by E. coli in mothers with PROM was significantly correlated with the microorganisms from the neonatal blood culture.38 For newborns with prolonged need of parenteral nutrition, most of them have a central line and are at much higher risk for infections due to bacterial translocation from the gastrointestinal tract.39 Restricting prenatal antibiotic use especially of cephalosporins and promoting active feeding strategies in premature infants to reduce the duration of parenteral nutrition may protect newborns from MDR E. coli sepsis.
There are certainly some limitations in our study. Limited by being single-center and observational cohort study, the risk factors selected for analysis are not comprehensive enough to include all possible factors. In addition, as a regional perinatal medical center, there are many premature infants and critical newborns which may not be universally representative of NICUs. In addition, the identification of specific drug resistance genes were not performed. A more representative multi-center study is warranted and should be conducted in the future.
Conclusion
E. coli remains the most common Gram-negative bacterial pathogen for neonatal sepsis. Higher proportion of ESBL-producing MDR E. coli are seen in premature infants and those newborns with HALOS. The mortality rate of neonatal sepsis caused by ESBL-producing E. coli is twice as high as that of sepsis caused by ESBL-negative E. coli. Furthermore, antepartum use of cephalosporins and prolonged use of parenteral nutrition may be important factors to consider in the selection of sensitive empirical antibiotics for use in neonatal sepsis caused by gram-negative rods prior to the availability of the results of antimicrobial susceptibility.
Acknowledgments
We would like to thank Dr Robert Green for advice and critical review of the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by the Medical Health Science and Technology Project of Zhejiang Province (No. 2020KY644) and Wenzhou Science and Technology Plan Projects (No. Y20170137, No. Y20220012).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390(10104):1770–1780. doi:10.1016/S0140-6736(17)31002-4
2. Jin Z, Wang Z, Li J, et al. Clinical laboratory features of microbes that cause neonatal sepsis: an 8-year retrospective study. Infect Drug Resist. 2022;15:2983–2993. doi:10.2147/IDR.S367068
3. Lu IC, Chang YC, Chen YT, et al. Epidemiological evolution of early-onset neonatal sepsis over 12 years: a single center, population-based study in central Taiwan. J Neonatal Perinatal Med. 2022;15:575–582. doi:10.3233/NPM-210938
4. Størdal EH, Solevåg AL, Bjørnholt JV, et al. Sepsis treatment options identified by 10-year study of microbial isolates and antibiotic susceptibility in a level-four neonatal intensive care unit. ACTA Paediatr. 2022;111:519–526. doi:10.1111/apa.16189
5. Zhu M, Jin Y, Duan Y, et al. Multi-drug resistant Escherichia coli causing early-onset neonatal sepsis - a single center experience from China. Infect Drug Resist. 2019;12:3695–3702. doi:10.2147/IDR.S229799
6. Awad HA, Mohamed MH, Badran NF, et al. Multidrug-resistant organisms in neonatal sepsis in two tertiary neonatal ICUs, Egypt. J Egypt Public Health Assoc. 2016;91:31–38. doi:10.1097/01.EPX.0000482038.76692.3
7. Zou H, Jia X, He X, et al. Emerging threat of multidrug resistant pathogens from neonatal sepsis. Front Cell Infect Microbiol. 2021;11:694093. doi:10.3389/fcimb.2021.694093
8. Sikias P, Biran V, Foix-L’Hélias L, et al. Early-onset neonatal sepsis in the Paris area: a population-based surveillance study from 2019 to 2021. Arch Dis. 2022;F1–F7. doi:10.1136/archdischild-2022-324080
9. Köstlin-Gille N, Härtel C, Haug C, et al. Epidemiology of early and late onset neonatal sepsis in very low birthweight infants: data from the German Neonatal Network. Pediatr Infect Dis J. 2021;40:255–259. doi:10.1097/INF.0000000000002976
10. Stoll BJ, Puopolo KM, Hansen NI, et al. Early-onset neonatal sepsis 2015 to 2017, the rise of Escherichia coli, and the need for novel prevention strategies. JAMA Pediatr. 2020;174:e200593. doi:10.1001/jamapediatrics.2020.0593
11. Yu YQ, He XR, Wan LJ, et al. Etiology, antimicrobial resistance, and risk factors of neonatal sepsis in China: a systematic review and meta-analysis from data of 30 years. J Matern. 2021;9:1–10. doi:10.1080/14767058.2021.1951217
12. Pan T, Zhu Q, Li P, et al. Late-onset neonatal sepsis in Suzhou, China. BMC Pediatr. 2020;20:261. doi:10.1186/s12887-020-02103-y
13. Berardi A, Sforza F, Baroni L, et al. Epidemiology and complications of late-onset sepsis: an Italian area-based study. PLoS One. 2019;14:e0225407. doi:10.1371/journal.pone.0225407
14. Gao K, Fu J, Guan X, et al. Incidence, bacterial profiles, and antimicrobial resistance of culture-proven neonatal sepsis in South China. Infect Drug Resist. 2019;12:3797–3805. doi:10.2147/IDR.S223597
15. Liu Y, Zhu M, Fu X, et al. Escherichia coli causing neonatal meningitis during 2001–2020: a study in eastern China. Int J Gen Med. 2021;14:3007–3016. doi:10.2147/IJGM.S317299
16. Okomo U, Akpalu ENK, Le Doare K, et al. Aetiology of invasive bacterial infection and antimicrobial resistance in neonates in sub-Saharan Africa: a systematic review and meta-analysis in line with the STROBE-NI reporting guidelines. Lancet Infect Dis. 2019;19:1219–1234. doi:10.1016/S1473-3099(19)30414-1
17. El-Naggar W, Afifi J, McMillan D, et al. Epidemiology of meningitis in Canadian neonatal intensive care units. Pediatr Infect Dis J. 2019;38:476–480. doi:10.1097/INF.0000000000002247
18. Sáez-López E, Guiral E, López Y, et al. Characterization of CTX-M-14 and CTX-M-15 producing Escherichia coli strains causing neonatal sepsis. Microb Drug Resist. 2014;20:281–284. doi:10.1089/mdr.2013.0190
19. Naselli A, Venturini E, Oss M, et al. Early-onset fulminant neonatal sepsis caused by multi-drug resistant and ESBL producing E. coli (CTX-M gene) in a late-preterm neonate: case report and literature review. New Microbiol. 2022;45:223–226.
20. Li JY, Chen SQ, Yan YY, et al. Identification and antimicrobial resistance of pathogens in neonatal septicemia in China-A meta-analysis. Int J Infect Dis. 2018;71:89–93. doi:10.1016/j.ijid.2018.04.794
21. Parascandalo FA, Zarb P, Tartari E, et al. Carriage of multidrug-resistant organisms in a tertiary university hospital in Albania-a point prevalence survey. Antimicrob Resist Infect Control. 2016;5:29. doi:10.1186/s13756-016-0128-1
22. Tsai MH, Chu SM, Hsu JF, et al. Risk factors and outcomes for multidrug-resistant gram-negative bacteremia in the NICU. Pediatrics. 2014;133:e322–9. doi:10.1542/peds.2013-1248
23. Freire MP, Carvalho LB, Reusing JO, et al. Carbapenem-resistant Enterobacteriaceae among kidney transplant recipients - insights on the risk of acquisition and CRE infection. Infect Dis Nor. 2021;53:430–439. doi:10.1080/23744235.2021.1887511
24. Dong L, Zhang XY, Li CC, et al. Characteristics of epidemiology and antimicrobial resistance of gram-negative bacterial bloodstream infections in children. Zhonghua Er Ke Za Zhi. 2017;55:683–688. doi:10.3760/cma.j.issn.0578-1310.2017.09.012
25. Zhanel GG, DeCorby M, Adam H, et al. Prevalence of antimicrobial-resistant pathogens in Canadian hospitals: results of the Canadian Ward Surveillance Study (CANWARD 2008). Antimicrob Agents. 2010;54:4684–4693. doi:10.1128/AAC.00469-10
26. Flokas ME, Karanika S, Alevizakos M, Mylonakis E, Simeoni U. Prevalence of ESBL-producing Enterobacteriaceae in pediatric bloodstream infections: a systematic review and meta-analysis. PLoS One. 2017;12:e0171216–e0171228. doi:10.1371/journal.pone.0171216
27. Yusef D, Shalakhti T, Awad S, et al. Clinical characteristics and epidemiology of sepsis in the neonatal intensive care unit in the era of multi-drug resistant organisms: a retrospective review. Pediatr Neonatol. 2018;59:35–41. doi:10.1016/j.pedneo.2017.06.001
28. Marando R, Seni J, Mirambo MM, et al. Predictors of the extended-spectrum-beta lactamases producing Enterobacteriaceae neonatal sepsis at a tertiary hospital, Tanzania. Int J Med Microbiol. 2018;308:803–811. doi:10.1016/j.ijmm.2018.06.012
29. Giannoni E, Agyeman PKA, Stocker M, et al. Neonatal sepsis of early onset, and hospital-acquired and community-acquired late onset: a prospective population-based cohort study. J Pediatr. 2018;201:106–114.e4. doi:10.1016/j.jpeds.2018.05.048
30. Gu S, Lai J, Kang W, et al. Drug resistance characteristics and molecular typing of Escherichia coli isolates from neonates in class A tertiary hospitals: a multicentre study across China. J Infection. 2022;85:499–506. doi:10.1016/j.jinf.2022.09.014
31. Murki S, Jonnala S, Mohammed F, Reddy A. Restriction of cephalosporins and control of extended spectrum beta-lactamase producing gram negative bacteria in a neonatal intensive care unit. Indian Pediatr. 2010;47:785–788. doi:10.1007/s13312-010-0118-y
32. Chiu S, Huang YC, Lien RI, et al. Clinical features of nosocomial infections by extended spectrum beta-lactamase-producing Enterobacteriaceae in neonatal intensive care units. Acta paediatr. 2005;94:1644–1649. doi:10.1080/08035250510037704
33. Huang Y, Zhuang S, Du M. Risk factors of nosocomial infection with extended-spectrum beta lactamase-producing bacteria in a neonatal intensive care unit in China. Infection. 2007;35:339–345. doi:10.1007/s15010-007-6356-9
34. Shakil S, Ali SZ, Akram M, et al. Risk factors for extended-spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae acquisition in a neonatal intensive care unit. J Trop Pediatrics. 2010;56:90–96. doi:10.1093/tropej/fmp060
35. Vijayakanthi N, Bahl D, Kaur N, et al. Frequency and characteristics of infections caused by extended-spectrum beta-lactamase-producing organisms in neonates: a prospective cohort study. BioMed Res Int. 2013;2013:756209. doi:10.1155/2013/756209
36. Li X, Xu X, Yang X, et al. Risk factors for infection and/or colonisation with extended-spectrum β-lactamase-producing bacteria in the neonatal intensive care unit: a meta-analysis. Int J Antimicrob. 2017;50:622–628. doi:10.1016/j.ijantimicag.2017.06.027
37. Nanayakkara D, Liyanapathirana V, Kandauda C, et al. Maternal vaginal colonization with selected potential pathogens of neonatal sepsis in the era of antimicrobial resistance, a single center experience from Sri Lanka. BMC Infect Dis. 2018;18:351. doi:10.1186/s12879-018-3262-y
38. Kwon DY, Seo MR, Park H, et al. Differential impact of abnormal vaginal colonization on perinatal outcome and association with early-onset neonatal sepsis: preterm labor vs. preterm premature rupture of membrane. J Matern. 2021;9:1–7. doi:10.1080/14767058.2021.1974384
39. Pierro A, van Saene HK, Donnell SC, et al. Microbial translocation in neonates and infants receiving long-term parenteral nutrition. Arch Surg. 1996;131:176–179. doi:10.1001/archsurg.1996.01430140066018
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
