Back to Journals » Cancer Management and Research » Volume 16
Risk Factors Associated with Chemotherapy-Induced Nausea and Vomiting Among Women with Breast Cancer Receiving Highly Emetogenic Chemotherapy: Individual Patient-Based Analysis of Three Prospective Antiemetic Trials
Authors Yeo W , Ngai NTY, Yip CCH, Mo FKF , Yeo VA, Ko JWH, Li LV, Lau TKH, Lai KT, Pang E, Yip CH, Yeo HL, Kwok CCH, Ko SWY, Molassiotis A
Received 22 November 2023
Accepted for publication 22 March 2024
Published 8 April 2024 Volume 2024:16 Pages 283—297
DOI https://doi.org/10.2147/CMAR.S447546
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bilikere Dwarakanath
Winnie Yeo,1 Nicole TY Ngai,1 Christopher CH Yip,1 Frankie KF Mo,1 Victoria A Yeo,1 Jonathan WH Ko,1 Leung V Li,1 Thomas KH Lau,1 Kwai Tung Lai,1 Elizabeth Pang,1 Claudia HW Yip,1 Horatio L Yeo,1 Carol Chi Hei Kwok,2 Stephanie WY Ko,1 Alex Molassiotis3
1Department of Clinical Oncology, Prince of Wales Hospital, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, SAR, People’s Republic of China; 2Department of Clinical Oncology, Princess Margaret Hospital, Kowloon, Hong Kong, People’s Republic of China; 3School of Nursing, The Hong Kong Polytechnic University, Hong Kong
Correspondence: Winnie Yeo, Department of Clinical Oncology, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, SAR, People’s Republic of China, Email [email protected]
Purpose: Although risk factors related to chemotherapy-induced nausea and vomiting (CINV) have been identified in previous studies, only a few studies have evaluated the risk factors associated with contemporary antiemetic prophylaxis, including olanzapine/aprepitant- or NEPA-containing regimens. This study aimed to identify the risk factors associated with CINV development in Chinese breast cancer patients receiving doxorubicin and cyclophosphamide chemotherapy.
Methods: Data from 304 patients enrolled in 3 previously reported prospective antiemetic studies were included. Multivariate logistic regression models were used to predict risk factors associated with CINV occurrence. Additionally, the likelihood of treatment failure in relation to the number of risk factors in individual patients was evaluated.
Results: Multivariate analysis of the entire study group revealed that obesity status (defined as body mass index/= 25.0 kg/m2) and the use of olanzapine/aprepitant- or NEPA-containing anti-emetic regimens were associated with a high likelihood, while a history of motion sickness was associated with a lower likelihood, complete response (CR), and “no nausea” in the overall phase. A history of vomiting during pregnancy was also associated with a lower likelihood of an overall CR. Patients with an increasing number of risk factors had a higher likelihood of treatment failure and shorter time to first vomiting. Those who did not achieve CR and “no nausea” in the first cycle were less likely to achieve these parameters in the subsequent cycle of chemotherapy.
Conclusion: The present study confirmed previously reported risk factors for CINV in Chinese breast cancer patients receiving doxorubicin and cyclophosphamide. Further optimization of CINV control is required for patients with identifiable risk factors; olanzapine/aprepitant- or NEPA- containing prophylaxis are the preferred contemporary anti-emetics regimens for Chinese breast cancer patients undergoing doxorubicin and cyclophosphamide chemotherapy.
Keywords: cytotoxic, nausea and vomiting, olanzapine, aprepitant, NEPA
Introduction
One of the key concerns of anticancer therapy is chemotherapy-induced nausea and vomiting (CINV), which leads to physical and psychological distress and impairs patients’ quality of life (QOL). Over the last decade, with the availability of second-generation 5-hydroxytryptamine 3 receptor antagonists (5HT3RA), neurokinin-1 receptor antagonists (NK1RA), and dopamine receptor antagonists, along with the wide adoption of recommendations from international antiemetic guidelines in clinical practice, improvements have been observed in the control of CINV and the associated quality of life.
One of the most common regimens administered in the adjuvant breast cancer setting is a combination of doxorubicin and cyclophosphamide (AC regimen). AC is highly emetogenic. As a result, for optimal control of the associated CINV, international authorities have recommended the combination antiemetic regimens that consist of 5HT3-RA, corticosteroids, with NK1-RA and/or olanzapine.1–3 However, it has been shown that despite the currently available antiemetic regimens, only 60–65% of breast cancer patients achieved complete response (CR; defined as no vomiting and no use of rescue medication) in the first 5 days after AC treatment.4–6 Apart from the issue of compliance to antiemetic prophylaxis, a number of risk factors have been identified to be associated with poor control of CINV, these could be categorized into patient- and treatment-related factors.7,8 Younger age, female sex, history of vomiting during pregnancy and history of motion sickness are some of the patient-related factors that have been associated with higher risk of emesis, while high habitual intake of alcohol has been associated with lower risk.7–11 However, studies that assessed emesis risk have mainly been based on early trials that involved first-generation 5-HT3RAs and NK1RA (specifically, aprepitant). Moreover, most reports involved heterogeneous patient populations who were receiving chemotherapy regimens comprising cytotoxic agents of different emetogenicities, and there might not be a clear distinction between CINV that occurred during the acute, delayed, and overall phases after chemotherapy.
In addition to categorizing chemotherapeutic regimens into different emetogenic potentials, the ability to identify factors associated with patients’ characteristics in the presence of wider availability of more effective antiemetic agents may help guide the appropriate use of resources, especially in parts of the world where there are particular economic constraints, to improve patients’ experience through the treatment journey and maintain their quality of life.
In this study, we aimed to identify the factors associated with the occurrence of CINV in a homogenous group of female Chinese patients with breast cancer who received AC chemotherapy. Specific objectives were to identify potential clinical factors related to the control of CINV in terms of CR and “no nausea”; determine if treatment failure was associated with the number of identified factors that an individual displayed, assess if prior experience of CINV affected emetic control in subsequent cycle.
Patients and Methods
This was a post-hoc analysis of three previously reported prospective studies which assessed the efficacy of five different antiemetic regimens. The first study was a randomized placebo-controlled study in 2007 that compared combination ondansetron and dexamethasone with either aprepitant or placebo.4 The second study was conducted between 2017 and 2018 and randomized patients to aprepitant/ondansetron/dexamethasone with or without olanzapine.5 The final study was a prospective single arm study conducted in 2018–2019 which evaluated NEPA (netupitant/palonosetron) with dexamethasone.6 All the three studies enrolled a similar patient population; patients were of ethnic Chinese women who were diagnosed with early breast cancer and were planned for (neo)adjuvant AC chemotherapy, consisting of doxorubicin 60 mg/m2 and cyclophosphamide 600 mg/m2. These patients were chemotherapy-naïve, able, and willing to complete the study diaries/questionnaires. Detailed descriptions of the study outcomes, including primary and secondary endpoints, are available in previous reports;4–6 details of the antiemetic regimens are also illustrated in Table S1. All three studies were approved by the Joint CUHK-NTEC Institutional Review Board of the Chinese University of Hong Kong and Hong Kong Hospital Authority. Additionally, as the third study involved another centre, approval was obtained from the Kowloon West Cluster Research Ethics Committee of the Hong Kong Hospital Authority. The second and third studies were conducted more recently and are registered at ClinicalTrials.gov (Identifier: NCT03386617 and NCT03079219, respectively). Informed consent was obtained from all the patients.
The following information was retrieved from the study case report forms: patients’ demographic and background characteristics including age, body weight, body height, history of motion sickness or pregnancy-associated vomiting, and alcohol intake.
Study Procedures and Assessment
All patients received AC on day 1 of the chemotherapy cycle. As part of the study procedure before AC infusion, individuals were asked to gauge their symptom of nausea on a visual analogue scale (VAS) ranging from 0 to 100 mm, with the extremes implying “no nausea” and “nausea as bad as it could be” respectively. After receiving AC, individuals were asked to log their experience of CINV in a diary over 120 hours; the symptoms that were captured included the frequency and intensity of nausea and the use of rescue antiemetic medications. All patients returned their diaries and questionnaires on day 1 of subsequent AC chemotherapy.
Control of CINV was defined as CR (no vomiting and no use of rescue medication) and “no nausea” (defined as nausea VAS score <5 mm) in the overall phase (defined as within 120 h after the start of AC administration). CR and “no nausea” rates in the acute (0–24 hours) and delayed (24–120 hours) phases were also determined. Treatment failure was defined as not achieving (i) CR or (ii) “no nausea” during the three phases.
Statistical Analyses
Analyses were made on CR and “no nausea” in the overall phases; additional analyses in the acute and delayed phases were also made. Potential clinical factors including sex, age, body surface area (BSA), body mass index (BMI), history of motion sickness, vomiting during pregnancy, alcohol intake, and antiemetic regimens received by an individual were assessed. Age as a risk factor was dichotomized into <55 versus ≥ 55 years, based on previous studies.9–11 BSA was arbitrarily categorized into two groups, </= 1.55 versus > 1.55 kg/m2. Patients with a BMI ≥ 25 kg/m2 were considered as obese based on criteria set by World Health Organization for Asians.12 Antiemetic regimens were categorized into two groups, “earlier” regimens (ie ondansetron/dexamethasone with or without aprepitant) versus “contemporary” regimens (ie olanzapine/aprepitant/ondansetron/dexamethasone or NEPA/dexamethasone), based on our recent studies which have shown that the latter regimens improved antiemetic efficacy and better quality of life.13,14
SAS version 9.4 statistical software was performed using for data analysis. Multivariate logistic regression analysis, with adjustments for potential clinical factors, was conducted to identify the significant risk factors associated with CINV, and odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Similarly, to assess the likelihood of CR and “no nausea” in cycle 2, patients’ CINV experience in cycle 1 was assessed based on multivariate regression analysis.
The Cochran–Armitage trend test was used to assess possible trends in the relationship between treatment failure and the number of identified risk factors. Those factors which were identified to be associated with lower risk of CINV were reversed for the purpose of this analysis.15 Furthermore, the time-to-treatment failure curves as classified by the number of identified factors in each subgroup were evaluated using the Kaplan–Meier method.
Results
Patient Characteristics
In this post-hoc analysis, 304 patients from three studies were included. Details of the patients’ characteristics are listed in Table S2. Pre-chemotherapy, only four patients reported any symptoms of nausea (nausea VAS ≥ 5 mm). With regard to prophylactic antiemetic regimens, 184 patients (60.5%) received historical antiemetic prophylaxis (62 received ondansetron/dexamethasone; 122 received aprepitant/ondansetron/dexamethasone) and 120 (39.5%) received contemporary antiemetic regimens (60 received olanzapine/aprepitant/ondansetron/dexamethasone and the remaining 60 received NEPA/dexamethasone).
Data on emesis outcomes during cycle 1 were available for all patients, whereas those for cycle 2 were available for 251 patients. In the overall phase, 144 patients (47.4%) achieved CR and 128 (42.1%) experienced “no nausea” during cycle 1; the corresponding figures for cycle 2 were 162 (65.4%) and 129 (51.4%) respectively. Details of the CR and “no nausea” rates in the acute and delayed phases are listed in Table 1.
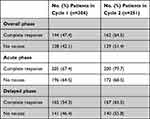 |
Table 1 Incidence of Complete Response and “No Nausea” Among Studied Patients |
Association of Clinical Variables and CR in Cycle 1 (Table 2)
In the overall phase, multivariate analysis revealed that the following factors were associated with CR in the overall phase: obesity (OR 1.95, 95% CI [95% confidence interval] 1.07–3.56, p= 0.029) and the use of contemporary antiemetic regimens (OR 1.81, 95% CI 1.31–2.51, p= 0.0003) were associated with a high likelihood of CR, whereas a history of motion sickness (OR 0.41, 95% CI 0.22–0.74, p= 0.003) and vomiting in pregnancy (OR 0.58, 95% CI 0.35–0.96, p= 0.033) were associated with a lower likelihood of CR.
 |
Table 2 Univariate and Multivariate Analyses of Association of Complete Response with Clinical Variables in Cycle 1 |
In the acute and delayed phases, obesity (acute phase: OR 2.83, 95% CI 1.44–5.56, p=0.003; delayed phase: OR 2.09, 95% CI 1.13–3.96, p= 0.019) and a history of motion sickness (acute phase: OR 0.34, 95% CI 0.19–0.60, p= 0.0002; delayed phase: OR 0.49, 95% CI 0.28–0.88, p= 0.017) were also associated with CR. In addition, BSA (OR 0.56, 95% CI 0.32–0.99, p= 0.45) and contemporary antiemetic regimens (OR 3.80, 95% CI 2.21–6.52, p<0.0001) were associated with CR in the acute and delayed phases, respectively.
Association of Clinical Variables with “No Nausea” in Cycle 1 (Table 3)
In the overall phase, multivariate analysis revealed the following factors to be associated with “no nausea” in the overall phase: obesity (OR 2.03, 95% CI 1.12–3.69; p= 0.020) and the use of contemporary antiemetic regimens (OR 2.68, 95% CI 1.51–4.47; p= 0.001) were associated with high likelihood of “no nausea”, while history of motion sickness (OR 0.39, 95% CI 0.21–0.73; p= 0.003) was associated with lower likelihood of “no nausea”.
 |
Table 3 Univariate and Multivariate Analyses of Association of “No Nausea” with Clinical Variables in Cycle 1 |
Multivariate analysis also identified that during the acute and delayed phases, being obese (acute phase: OR 1.96, 95% CI 1.03–3.73, p= 0.040; delayed phase: OR 2.09, 95% CI 1.15–3.80, p=0.016), having a history of motion sickness (acute phase: OR 0.40, 95% CI 0.23–0.72, p= 0.002; delayed phase: OR 0.40, 95% CI 0.22–0.72, p= 0.002) and having received contemporary antiemetic regimens (acute phase: OR 1.99, 95% CI 1.16–3.44, p= 0.013; delayed phase: OR 3.07, 95% CI 1.84–5.13; p<0.0001) remained to be significant factors for “no nausea”. In contrast, age (OR 1.79, 95% CI 1.31–3.12; p= 0.039) and vomiting during pregnancy (OR 0.53, 95% CI 0.32–0.89, p= 0.016) were significant only in the acute phase.
Relationship Between the Number of Identified Risk Factors and Treatment Failure
In terms of CR in the overall phase (Table 4), increased number of risk factors that an individual patient displayed was associated with increased likelihood of treatment failure during the overall phase (p< 0.0001). The proportion of patients who achieved CR was 81.2% for those without any risk factors, which decreased to 5.9% for those with four risk factors. An increased number of risk factors was also closely related to the inability to achieve CR in the acute and delayed phases (p < 0.0001).
 |
Table 4 Relationship Between Treatment Outcomes and Number of Identified Risk Factors |
In terms of nausea, an increased number of risk factors was significantly associated with an increased likelihood of treatment failure during the overall phase (p < 0.0001). The proportion of patients who experienced “no nausea” reduced from 74.1% in those without any risk factors to 16.7% in patients with three risk factors. Similarly, an increased number of identified factors were also closely related to nausea experienced in the acute and delayed phases (p < 0.0001).
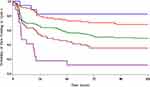
Relationship Between the Number of Identified Risk Factors and Time to First Vomiting
Figure 1 shows the Kaplan-Meier curves of the time to first vomiting according to the number of identified risk factors (obesity, history of motion sickness, history of vomiting during pregnancy, and not receiving contemporary antiemetic regimens) in all patients. The time to first vomiting was significantly related to the number of identified factors (p < 0.0001). For instance, among patients who had 0, 1, 2, and 3 risk factors, the 24-hour rate of no vomiting was 81.3%, 80.3%, 66.7%, 53.7%, and 17.7%, respectively, and similar trends were observed for analyses on 48-hour and 72-hour rates.
Association of CR and “No Nausea” in Cycle 2 Based on Clinical Variables and Patients’ CINV Experience in Cycle 1 (Table 5)
In multivariate analysis, after adjusting for prognostic factors, patients who experienced CR in the overall phase of cycle 1 AC had a higher likelihood of achieving CR in cycle 2, with odds ratios of 11.31 (95% CI, 5.52–23.16, p<0.0001). Likewise, those who experienced “no nausea” in the overall phase in cycle 1 also had a higher likelihood of “no nausea” in cycle 2 (odds ratios, 9.61 (95% CI, 5.00–18.50, p<0.0001).
 |
Table 5 Outcomes of Multivariate Analyses on Association of CR and “No Nausea” in Cycle 2 Based on Patients’ Experience in Cycle 1 |
Discussion
In this study, multivariate logistic regression analysis of the CR group demonstrated that a history of motion sickness and vomiting during pregnancy was a significant and independent risk factor for CINV, whereas obesity and the use of NEPA- or olanzapine-containing antiemetic regimens were significant and independent CINV protective factors in the overall phase. Additionally, a history of motion sickness and obesity were confirmed as risk and protective factors, respectively, associated with both the acute and delayed phases. Specifically, in the delayed phase, the use of contemporary antiemetic regimens (containing NEPA or olanzapine) was a significant independent protective factor. Similar tendencies were found in the multivariate logistic regression analysis on “no nausea”. Furthermore, the number of risk factors was significantly associated with no CR, higher likelihood of nausea, and time to first vomiting episode; CR and no nausea in subsequent cycles were associated with patients’ experience of these parameters in the first cycle. These findings are consistent with the literature.16–20
Higher likelihood of younger patients to experience CINV is a well-established risk factor, particularly those <50 years old.16,21,22 In a post-hoc analysis on 864 chemotherapy-naïve, breast cancer patients receiving AC chemotherapy, pregnancy-induced vomiting (morning sickness) was identified as a risk factor for “emesis” but not nausea in the overall phase, while motion sickness was a risk factor for “significant nausea” but not “emesis”.23 In our analysis on similar patient population but of Chinese ethnicity, pregnancy-induced vomiting only significantly contributed to “nausea” in the acute phase, while motion sickness was a significant factor for both CR and nausea in the overall phase. In another Asian study, 1910 Japanese chemotherapy-naïve subjects, including 429 breast cancer patients who received highly and moderately emetogenic chemotherapy (HEC and MEC, respectively), female sex, history of morning sickness, and motion sickness, were prospectively identified as risk factors for acute and delayed CINV [9]. Although the direct pathophysiological mechanisms are unknown, both factors are associated with female sex and positive family histories,24,25 suggesting collinearity between these factors and the role of genetics in susceptibility to CINV. Genetic variability in antiemetic interactions and metabolism may explain suboptimal control of CINV. A recent systematic review26 revealed the association between three single nucleotide polymorphisms (SNPs) in 5HT3R genes, two alleles of CYP2D6, and three SNPs in ABCB1, with the occurrence and severity of CINV. Further research utilizing whole-genome sequencing may allow new discoveries of polymorphisms as genetic risk factors for CINV.27
The role of BMI in association with CINV has been inconsistent in literature. In a study by Gilmore et al that included 1295 patients receiving HEC or MEC, the authors highlighted that overweight and obese patients had a 23% lower chance of developing CINV.21 However, another study with 5570 female patients showed no association between CINV and obesity.22 Our study findings support obesity as a protective factor against nausea and CR. However, there is limitation in assessing obesity as a factor. Obesity may merely reflect nutritional status, with patients not experiencing CINV having less impact on food intake. Further, BMI is a crude assessment of physical status of an individual, and additional investigation into the association of obesity and CINV can be aided by evaluation of body composition.
The current study also revealed that the presence of CR and “no nausea” in cycle 1 to be a significant and independent protective factor of CINV in cycle 2, for the overall, acute and delayed phases. This supports previous studies which have also shown that prior experience with CINV in earlier cycles increases the risk of subsequent CINV in later cycles.28–30 Molasiotis et al30 investigated 991 breast cancer patients from eight European countries across three chemotherapy cycles, who were scheduled to receive their first cycle of HEC or MEC. Subjects who did not achieve CR in Cycle 1 were 6.6 times more likely to have no CR in cycle 2 (p<0.001); and 8 times more likely to have no CR in cycle 3 (p<0.001). Interestingly, Navari et al31 recently reported a high repeat-failure risk only in patients receiving aprepitant-based antiemetic prophylaxis among 835 breast cancer patients receiving AC, whereas patients receiving NEPA-based regimens did not face similar risks. Our study revealed that CR/“no nausea” in cycle 2 was closely associated with patients’ experience of CINV in cycle 1 (odd ratios of 9.40–15.66), and this was independent of anti-emetic regimens in the multivariate analysis. The same was true for the time to the first vomiting episode.
Our study also revealed that an increased number of CINV risk factors led to an increase in the proportion of patients with antiemetic treatment failure, in terms of both CR and “no nausea”. Our study provided numerical evidence of this treatment failure, showing that nearly half of the patients with only a single risk factor experienced nausea, and the vast majority of those with three or four risk factors experienced nausea’ and no CR. Previously, Tsuji et al32 have reported a similar trend between the number of risk factors and treatment failure, and the preference of palonosetron over granisetron for patients who have at least one risk factor. Prediction models for CINV have been reported, and further evaluation is warranted to expedite its use in the clinical setting. For instance, Dranitsaris et al33 utilized data from 1198 patients to develop a risk-scoring algorithm, ranging from 0 to 32 units; and a score of >16 units indicated a high risk of developing grade > 2 CINV. Similarly, Molasiotis et al designed a predictive model with specificity and sensitivity of 55.4% and 80.3%, respectively.34
International guidelines classify AC chemotherapy as highly emetogenic, inducing emesis in more than 90% of patients in the absence of antiemetic prophylaxis.1–3 Earlier guidelines35 suggested a triplet antiemetic regimen consisting of 5HT3RA, corticosteroids and NK1RA, in breast cancer patients on AC. However, we recently concluded that aprepitant-containing triplets are non-superior to doublet antiemetics, wherein only 50% of our study population achieved CR.14 With olanzapine-containing regimens proving to be superior in controlling CINV in a number of studies and meta-analyses,36–40 the latest 2020 ASCO guidelines recommend the addition of olanzapine into the triplet regimen, forming a 4-drug combination.1 Similarly, for NEPA, a number of studies confirmed its efficacy in controlling CINV.41–44 Its composition of palonosetron, a long-lasting second-generation 5HT3RA, and netupitant, a highly selective NK1RA, synergistically act on major pathways reducing CINV in both the acute and delayed phases.45 Therefore, the current data support the role of the contemporary antiemetics of NEPA- or olanzapine-containing regimens as protective factors for CINV.
The present study had two limitations. Our study evaluated only 6 patient factors (age, BSA, BMI, history of motion sickness, history of pregnancy-induced vomiting, and alcohol consumption) and one treatment factor (ie historical vs contemporary antiemetic prophylaxis). Some risk factors identified in the literature are innate characteristics of our population, namely ethnicity (Chinese), sex (female), diagnosis of breast cancer, and a specific chemotherapeutic regimen of AC. Psychological elements such as anxiety and expectations of CINV were not considered. The number of patients with habitual alcohol consumption was very small in our sample, which is typical of Asian populations; hence, no meaningful analysis of this potential risk factor could be performed. Furthermore, the study population comprised only Chinese patients; consequently, these findings may not be generalizable to other ethnicities receiving non-AC chemotherapy. However, risk factor assessment in a uniform group of patients with breast cancer receiving identical treatment could be regarded as a strength of the current study. All subjects were chemotherapy-naïve, had early-stage disease with good performance status, and were recruited from two public hospitals in Hong Kong which provide free healthcare, independent of medical insurance.
Conclusion
Our analysis confirmed the importance of the commonly identified risk factors for CINV in Chinese patients with breast cancer receiving AC chemotherapy: younger age (<55 years), non-obesity, history of morning sickness, and motion sickness. Contemporary antiemetic regimens containing olanzapine or NEPA have been uniquely identified as protective factors against CINV. Furthermore, prior experience with CINV in earlier cycles predicts subsequent CINV in later cycles. We also confirmed a significant association between an increased number of risk factors and the development of CINV. These findings highlight the necessity for a personalized antiemetic prophylaxis plan, especially for patients with a higher number of risk factors. Considering that NEPA is superior to aprepitant plus a first-generation 5HT3RA, and that the addition of olanzapine provides additional benefits to an aprepitant-containing regimen, the efficacy of a combined olanzapine/NEPA regimen should be explored further alongside non-pharmacological means.
Declaration
Part of the data in the manuscript has been presented in the 2023 St Gallen Breast Cancer Conference in Vienna, Austria on 17 March 2023.
Data Sharing Statement
All data relevant to the study are included in the article or uploaded as supplementary information. The data are available from the Comprehensive Cancer Trials Unit of the Department of Clinical Oncology, Chinese University of Hong Kong, but restrictions apply to the availability of these data. These data were used under permission for the current study, and so are not publicly available. Data are, however, available from the authors (W Yeo and F Mo) upon reasonable request. Data will be made available for 15 years from the start of the clinical trials.
Ethics Approval and Informed Consents
This study was approved by the regional ethics committee (the Joint Clinical Research Ethics Committee of Chinese University of Hong Kong and New Territories East Cluster of Hospital Authority, and the Kowloon West Cluster Research Ethics Committee of the Hong Kong Hospital Authority). Written informed consents were obtained from all study patients. The trials complied with the Declaration of Helsinki.
Acknowledgment
This study was supported by an education grant from Madam Diana Hon Fun Kong Donation for Cancer Research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Yeo has been involved in the CINV Network in Asia and has been a speaker of the CINV organized by Mundipharma. Mundipharma supported the study design of the NEPA, but had no role in the present analysis, data collection and analysis, decision to publish, or preparation of the manuscript. Molasiotis has received grants and has been a speaker for Helsinn. Madam Diana Hon Fun Kong Donation for Cancer Research had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation. None of the other authors declare any conflict of interest. The statements presented in this paper are the sole responsibility of the authors.
References
1. Hesketh PJ, Kris MG, Basch E, et al. Antiemetics: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2020;38:2782–2797. doi:10.1200/JCO.20.01296
2. Herrstedt J, Roila F, Warr D, et al. 2016 updated MASCC/ESMO consensus recommendations: prevention of nausea and vomiting following high emetic risk chemotherapy. Support Care Cancer. 2017;25:277–288. doi:10.1007/s00520-016-3313-0
3. National Comprehensive Cancer Network (NCCN). Clinical practice guidelines in oncology. Antiemesis. 2023;2023:1.
4. Yeo W, Mo FK, Suen JJ, et al. A randomized study of aprepitant, ondansetron and dexamethasone for chemotherapy-induced nausea and vomiting in Chinese breast cancer patients receiving moderately emetogenic chemotherapy. Breast Cancer Res Treat. 2009;113:529–535. doi:10.1007/s10549-008-9957-9
5. Yeo W, Lau TK, Li L, et al. A randomized study of olanzapine-containing versus standard antiemetic regimens for the prevention of chemotherapy-induced nausea and vomiting in Chinese breast cancer patients. Breast. 2020;50:30–38. doi:10.1016/j.breast.2020.01.005
6. Yeo W, Lau TK, Kwok CC, et al. NEPA efficacy and tolerability during (neo)adjuvant breast cancer chemotherapy with cyclophosphamide and doxorubicin. BMJ Support Palliat Care. 2020;1:1–7. doi:10.1136/bmjspcare-2019-002037
7. Lohr L. Chemotherapy-induced nausea and vomiting. Cancer J. 2008;14:85–93. doi:10.1097/PPO.0b013e31816a0f07
8. Hesketh PJ. Chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358:2482–2494. doi:10.1056/NEJMra0706547
9. Tamura K, Aiba K, Saeki T, et al. Testing the effectiveness of antiemetic guidelines: results of a prospective registry by the CINV study group of Japan. Int J Clin Oncol. 2015;20:855–865. doi:10.1007/s10147-015-0786-7
10. Sekine I, Segawa Y, Kubota K, Saeki T. Risk factors of chemotherapy-induced nausea and vomiting: index for personalized antiemetic prophylaxis. Cancer Sci. 2013;104:711–717. doi:10.1111/cas.12146
11. Sullivan JR, Leyden MJ, Bell R. Decreased cisplatin-induced nausea and vomiting with chronic alcohol ingestion. N Engl J Med. 1983;309:796. doi:10.1056/NEJM198309293091317
12. Expert Consultation WHO. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi:10.1016/S0140-6736(03)15268-3
13. Yeo W, Mo FK, Yip CCH, et al. Quality of life associated with nausea and vomiting from anthracycline-based chemotherapy: a pooled data analysis from three prospective trials. Oncologist. 2021;26:e2288–e2296. doi:10.1002/onco.13978
14. Yeo W, Li L, Lau TK, et al. Identification of optimal contemporary antiemetic prophylaxis for doxorubicin-cyclophosphamide chemotherapy in Chinese cancer patients: post-hoc analysis of 3 prospective studies. Cancer Biol Med. 2021;18:825–832. doi:10.20892/j.issn.2095-3941.2020.0241
15. Tsuji D, Suzuki K, Kawasaki Y, et al. Risk factors associated with chemotherapy-induced nausea and vomiting in the triplet antiemetic regimen including palonosetron or granisetron for cisplatin-based chemotherapy: analysis of a randomized, double-blind controlled trial. Support Care Cancer. 2019;27:1139–1147. doi:10.1007/s00520-018-4403-y
16. Mosa ASM, Hossain AM, Lavoie BJ, et al. Patient-related risk factors for chemotherapy-induced nausea and vomiting: a systematic review. Front Pharmacol. 2020;11:329. doi:10.3389/fphar.2020.00329
17. Furukawa N, Akasaka J, Shigemitsu A, et al. Evaluation of the relation between patient characteristics and the state of chemotherapy-induced nausea and vomiting in patients with gynecologic cancer receiving paclitaxel and carboplatin. Arch Gynecol Obstet. 2014;289:859–864. doi:10.1007/s00404-013-3058-7
18. Booth CM, Clemons M, Dranitsaris G, et al. Chemotherapy-induced nausea and vomiting in breast cancer patients: a prospective observational study. J Support Oncol. 2007;5:374–380.
19. Mizuno M, Hiura M, Kikkawa F, et al. A prospective observational study on chemotherapy-induced nausea and vomiting (CINV) in patients with gynecologic cancer by the CINV Study Group of Japan. Gynecol Oncol. 2016;140:559–564. doi:10.1016/j.ygyno.2015.12.029
20. Petrella T, Clemons M, Joy A, et al. Identifying patients at high risk for nausea and vomiting after chemotherapy: the development of a practical validated prediction tool. II. Delayed nausea and vomiting. J Support Oncol. 2009;7:W9–W16.
21. Gilmore JW, Peacock NW, Gu A, et al. Antiemetic guideline consistency and incidence of chemotherapy-induced nausea and vomiting in US community oncology practice: INSPIRE Study. J Oncol Pract. 2014;10(1):68–74. doi:10.1200/JOP.2012.000816
22. Binder G, Saunders WB. Chemotherapy-Induced Nausea And Vomiting (CINV) - incidence by age and sex among patients receiving oxaliplatin. Value Health. 2018;21:14. doi:10.1016/j.jval.2018.04.080
23. Warr DG, Street JC, Carides AD. Evaluation of risk factors predictive of nausea and vomiting with current standard-of-care antiemetic treatment: analysis of Phase 3 trial of aprepitant in patients receiving Adriamycin-cyclophosphamide-based chemotherapy. Support Care Cancer. 2011;19:807–813. doi:10.1007/s00520-010-0899-5
24. Hromatka BS, Tung JY, Kiefer AK, et al. Genetic variants associated with motion sickness point to roles for inner ear development, neurological processes and glucose homeostasis. Hum Mol Genet. 2015;24:2700–2708. doi:10.1093/hmg/ddv028
25. Laitinen L, Nurmi M, Ellilä P, et al. Nausea and vomiting of pregnancy: associations with personal history of nausea and affected relatives. Arch Gynecol Obstet. 2020;302:947–955. doi:10.1007/s00404-020-05683-3
26. Singh KP, Dhruva AA, Flowers E, et al. A review of the literature on the relationships between genetic polymorphisms and chemotherapy-induced nausea and vomiting. Crit Rev Oncol Hematol. 2018;121:51–61. doi:10.1016/j.critrevonc.2017.11.012
27. Sugino S, Janicki PK. Pharmacogenetics of chemotherapy-induced nausea and vomiting. Pharmacogenomics. 2015;16:149–160. doi:10.2217/pgs.14.168
28. Schwartzberg L, Szabo S, Gilmore J, et al. Likelihood of a subsequent chemotherapy-induced nausea and vomiting (CINV) event in patients receiving low, moderately or highly emetogenic chemotherapy (LEC/MEC/HEC). Curr Med Res Opin. 2011;27:837–845. doi:10.1185/03007995.2011.556603
29. Kim HK, Hsieh R, Chan A, et al. Impact of CINV in earlier cycles on CINV and chemotherapy regimen modification in subsequent cycles in Asia Pacific clinical practice. Support Care Cancer. 2015;23:293–300. doi:10.1007/s00520-014-2376-z
30. Molassiotis A, Aapro M, Dicato M, et al. Evaluation of risk factors predicting chemotherapy-related nausea and vomiting: results from a European prospective observational study. J Pain Symptom Manage. 2014;47:839–848.e4. doi:10.1016/j.jpainsymman.2013.06.012
31. Navari R, Binder G, Molassiotis A, et al. Chemotherapy-induced nausea and vomiting (CINV) risk after prior breakthrough CINV: unmasking the false average. Cancer Res. 2021;81:PS13–09. doi:10.1158/1538-7445.SABCS20-PS13-09
32. Tsuji Y, Baba H, Takeda K, et al. Chemotherapy-induced nausea and vomiting (CINV) in 190 colorectal cancer patients: a prospective registration study by the CINV study group of Japan. Expert Opin Pharmacother. 2017;18:753–758. doi:10.1080/14656566.2017.1317746
33. Dranitsaris G, Molassiotis A, Clemons M, et al. The development of a prediction tool to identify cancer patients at high risk for chemotherapy-induced nausea and vomiting. Ann Oncol off J Eur Soc Med Oncol. 2017;28:1260–1267. doi:10.1093/annonc/mdx100
34. Molassiotis A, Stamataki Z, Kontopantelis E. Development and preliminary validation of a risk prediction model for chemotherapy-related nausea and vomiting. Support Care Cancer. 2013;21:2759–2767. doi:10.1007/s00520-013-1843-2
35. Roila F, Molassiotis A, Herrstedt J, et al. 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Ann Oncol. 2016;27:v119–v133. doi:10.1093/annonc/mdw270
36. Navari RM, Qin R, Ruddy KJ, et al. Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;375:134–142. doi:10.1056/NEJMoa1515725
37. Tienchaiananda P, Nipondhkit W, Maneenil K, et al. A randomized, double-blind, placebo-controlled study evaluating the efficacy of combination olanzapine, ondansetron and dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving doxorubicin plus cyclophosphamide. Ann Palliat Med. 2019;8:372–380. doi:10.21037/apm.2019.08.04
38. Wang X, Wang L, Wang H, et al. Effectiveness of olanzapine combined with ondansetron in prevention of chemotherapy-induced nausea and vomiting of non-small cell lung cancer. Cell Biochem Biophys. 2015;72:471–473. doi:10.1007/s12013-014-0489-0
39. Chiu L, Chow R, Popovic M, et al. Efficacy of olanzapine for the prophylaxis and rescue of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis. Support Care Cancer. 2016;24:2381–2392. doi:10.1007/s00520-016-3075-8
40. Yokoe T, Hayashida T, Nagayama A, et al. Effectiveness of antiemetic regimens for highly emetogenic chemotherapy-induced nausea and vomiting. A Systematic Review and Network Meta-Analysis. Oncologist. 2019;24:e347–e357.
41. Aapro M, Karthaus M, Schwartzberg L, et al. NEPA, a fixed oral combination of netupitant and palonosetron, improves control of chemotherapy-induced nausea and vomiting (CINV) over multiple cycles of chemotherapy: results of a randomized, double-blind, phase 3 trial versus oral palonosetron. Support Care Cancer. 2017;25:1127–1135. doi:10.1007/s00520-016-3502-x
42. Caputo R, Cazzaniga ME, Sbrana A, et al. Netupitant/palonosetron (NEPA) and dexamethasone for prevention of emesis in breast cancer patients receiving adjuvant anthracycline plus cyclophosphamide: a multi-cycle, phase ii study. BMC Cancer. 2020;20:232. doi:10.1186/s12885-020-6707-9
43. Vaswani B, Dattatreya PS, Bhaget S, et al. The effectiveness of NEPA in the prevention of chemotherapy-induced nausea vomiting among chemo naïve patients in an Indian setting. BMC Cancer. 2021;21:601. doi:10.1186/s12885-021-08342-1
44. Di Renzo N, Musso M, Scimè R, et al. Efficacy and safety of multiple doses of NEPA without dexamethasone in preventing nausea and vomiting induced by multiple-day and high-dose chemotherapy in patients with non-Hodgkin’s lymphoma undergoing autologous hematopoietic stem cell transplantation: a phase IIa, multicenter study. Bone Marrow Transplant. 2020;55:2114–2120. doi:10.1038/s41409-020-0909-2
45. Lorusso V, Russo A, Giotta F, et al. Management of chemotherapy-induced nausea and vomiting (CINV): a short review on the role of netupitant-palonosetron (NEPA). Core Evid. 2015;15:21–29. doi:10.2147/CE.S203634
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.