Back to Journals » Infection and Drug Resistance » Volume 17
Risk Factors and Predictive Nomogram for Carbapenem-Resistant Klebsiella pneumoniae in Children in a Grade 3 First-Class General Hospital in Central China
Authors Chu X, Ning L, Fang Y, Jia H, Wang M
Received 29 August 2023
Accepted for publication 25 December 2023
Published 5 January 2024 Volume 2024:17 Pages 41—49
DOI https://doi.org/10.2147/IDR.S437742
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Sandip Patil
Xinmin Chu,1 Lijuan Ning,2,3,* Yuting Fang,2,3,* Hengmin Jia,4 Meng Wang2,3
1Department of Clinical Laboratory, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, 230001, People’s Republic of China; 2Department of Pharmacy, the First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, 230001, People’s Republic of China; 3Anhui Provincial Key Laboratory of Precision Pharmaceutical Preparations and Clinical Pharmacy, Hefei, Anhui, 230001, People’s Republic of China; 4Department of Infection Office, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, 230001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Meng Wang, Department of Pharmacy, the First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, 230001, People’s Republic of China, Email [email protected]
Background: This study determined risk factors for Carbapenem-resistant Klebsiella pneumoniae (CRKP)in children admitted to a grade 3 first-class general hospital and developed an individualized line graph predictive model.
Methods: The clinical data of 185 children infected with Klebsiella pneumoniae from January 2015 to December 2019 were analyzed retrospectively. Patients were grouped according to carbapenem resistance: CRKP group (50 cases) and CSKP (carbapenem-sensitive Klebsiella pneumoniae) group (135 cases). Risk factors for CRKP in children were screened by logistic regression analysis. The predictive model was established using R software and validated using the Bootstrap method.
Results: Age (odds ratio [OR]=0.104, 95% confidence interval [CI]: 0.026– 0.408), intensive care unit admission (OR =2.829, 95% CI: 1.138– 7.030), mechanical ventilation (OR =7.510, 95% CI: 3.140– 17.961), surgery history (OR =5.005, 95% CI: 1.507– 16.618) and glucocorticoid (OR =0.235, 95% CI: 0.099– 0.557) were independent risk factors for CRKP in children (P < 0.05), The total risk score of each factor was 362.5, and the risk rate was 0.1– 0.9. In receiver-operating characteristic curve analysis, the area under the curve of CRKP predicted by the total risk score was 0.872 (95% CI=0.844– 0.901; P < 0.001). The correction curve indicated that the consistency between the observed value and the predicted value was good.
Discussion and Conclusion: This study successfully established a model based on the risk factors, with high accuracy and good predictive value for CRKP in children. Hospitals should take necessary preventive measures against the risk factors for drug-resistant bacteria, such as optimizing the configuration of ICU space, timely isolation of infected children, and adequate disinfection of ICU equipment. Which may reduce CRKP infection rate.
Keywords: Klebsiella pneumoniae, carbapenem resistance, risk factors, nomogram, children
Background
Carbapenem-resistant Klebsiella pneumoniae (CRKP) is an independent risk factor for death in patients with nosocomial infection due to its difficulty in preventing and controlling infection. The mortality rate of hospitalized patients infected with CRKP is high, and CRKP has spread globally and locally in China.1
pneumoniae is the third leading cause of bloodstream infection (BSI) in children, and the carbapenem-resistant Enterobacterales species have become a public health concern worldwide. The clinical infection caused by CRKP is the most common and severe.2 The CRKP detection rate in children increased from 5.6% in 2014 to 9.6% in 2018,3 according to the China Antimicrobial Surveillance Network (CHINET). CHINET resistance data from China showed that the detection rate of CRKP in children increased from 2.2% to 25.4% during 2005–2018, with Beijing and Shanghai reporting the highest rates. A survey conducted by Yan et al in 10 children-specialty hospitals in China showed that the detection rate of CRKP was approximately 20.0%.4 Due to the immature immune system of children, children are more susceptible to CRKP infection, and there are fewer antibiotics available for children than adults, and more complications occur in children, which brings great challenges to clinical treatment.5 Therefore, there is a need to explore risk factors for CRKP in children to prevent antimicrobial resistance and consequently improve the prognosis. However, there are no scientific techniques or reliable methods to predict the prognosis of patients based on a single factor.
A nomogram is a comprehensive risk assessment tool that can individually predict the risk of clinical events based on various influencing factors in the logistic regression model.6 It is widely used in disease risk assessment, for example, gastric cancer recurrence,7 postoperative survival of duodenal adenocarcinoma,8 overall survival in patients with low-grade endometrial stromal sarcoma.9 The present study aimed to explore risk factors for CRKP infection in children and establish a line graph nomogram model for the prediction of the risk of CRKP infection in children based on individual factors, to provide an early and accurate diagnosis for the prevention and treatment of CRKP infection in children.
Materials and Methods
Data Source
Clinical data of children infected with K. pneumoniae (Such as respiratory infections, blood infections, and other infections)and admitted to the First Affiliated Hospital of the University of Science and Technology of China (Anhui Provincial Hospital) between January 2015 and December 2019 were collected retrospectively through the hospital infection management system and the hospital electronic medical records system. All data were based on original medical records. Antimicrobial susceptibility was determined by a Vitek-2 Compact system.
Patients were divided into two groups according to the presence of carbapenem resistance: the CRKP group and the CSKP (carbapenem-sensitive Klebsiella pneumoniae) group.
This study has passed the ethical review of the First Affiliated Hospital of University of Science and Technology of China (Anhui Provincial Hospital) (no. 2022-RE-035)
Patient Population
A total of 185 children were identified from the hospital records system, The CRKP group included 50 participants, and the CSKP group included 135 participants. The inclusion criteria were as follows: (1) patients who met the diagnostic criteria for hospital infection promulgated by the Ministry of Health of the People’s Republic of China in 2001 and the relevant diagnostic criteria for carbapenem antibiotic resistance; (2) patients whose drug resistance was confirmed in the drug sensitivity test; (3) patients aged 0–14 years; (4) patients with complete data.
The exclusion criteria were as follows: (1) patients who did not meet the diagnostic requirements of “Hospital infection diagnostic criteria”.
Data Extraction and Management
Information on the influencing factors that may be related to CRKP infection was collected by reviewing relevant literature. All the data of the same child were collected by the same person, and the data collected were input and checked by two people to ensure accuracy. The data, which included general demographic data (such as age, sex, weight), presence of complications, presence of hospital infection bacteria, Nosocomial infection site, pre-infection medication use such as antibiotics (Penicillins, cephalosporins, macrolides, carbapenems, glycopeptides), glucocorticoid, parenteral nutrition, immunosuppressants, admission to the intensive care unit (ICU), mechanical ventilation, invasive procedures, pre-infection surgical history, etc. were then investigated, compared, and analyzed.
Statistical Analysis
All the experimental data in this study were analyzed using SPSS 22.0 (IBM Corp., Armonk, NY). The counting data were expressed as rates, and the inter-group comparison was performed using χ2 test. The collected variables were analyzed by single-factor analysis, and the independent risk factors for CRKP infection in children were screened using multivariate logistic regression analysis. Finally, the variables of the line chart model were introduced, which aided in establishing line chart for CRKP infection in children. P < 0.05 was considered statistically significant. We used R3.5.3 software (http://www.r-project.org/) to establish the prediction model of the alignment map, caret program package to perform the Bootstrap method for the internal verification, and RMS program package to calculate the consistency index (C-index). Receiver operating characteristic (ROC) curves were generated to evaluate the forecasting efficiency of CRKP risk.
Results
A total of 185 children were analyzed retrospectively, which included 132 boys and 53 girls, aged 0–9 years. The isolates were derived from sputum culture, pus culture and other culture, among which 160 cases (86.48%) were derived from sputum culture, 13 cases (7.02%) from pus culture, and 12 cases (6.48%) from other cultures the CRKP group included 50 participants, and the CSKP group included 135 participants.
Single-Factor Analysis of Basic Data of Children in Both Groups
As shown in Table 1, there were significant differences between the two groups in terms of age, weight, hospital infection, admission to the ICU, mechanical ventilation, surgical history before infection, types of antibacterial agents used before infection, glucocorticoid use, and length of stay (P < 0.05). There was no significant difference in sex, complication, infection site, parenteral nutrition, and immunosuppressive therapy between the two groups (P > 0.05).
 |
Table 1 Single-Factor Analysis of Basic Data in the Two Groups |
Logistic Regression Analysis of Risk Factors for K. pneumoniae Drug Resistance in Children
As shown in Table 2, logistic binary regression analysis was conducted for age, weight, nosocomial infection, admission to the ICU, mechanical ventilation, invasive surgery, types of antibiotics used, surgical history before infection, and history and of glucocorticoid use. The results showed that age (odds ratio [OR] = 0.104, 95% confidence interval [CI]: 0.026–0.408), admission to the ICU (OR = 2.829, 95% CI: 1.138–7.030), mechanical ventilation (OR = 7.510, 95% CI: 3.140–17.961), surgical history (OR = 5.005, 95% CI: 1.507–16.618), and history of glucocorticoid use (OR = 0.235, 95% CI: 0.099–0.557) were significant risk factors for CRKP (P < 0.05).
 |
Table 2 Logistic Regression Analysis of Individual Predictors of CRKP in Children |
Establishment of CRKP Risk Mapping Model for Children
Using the variables of multiple logistic regression analysis as the predictive factor, a line graph model was developed for CRKP risk in children using R software. For patients younger than 1 years of age, the line chart, ICU admission, non-mechanical ventilation treatment, pre-infection surgical history, and non-use of glucocorticoids pre-infection scores were 100, 45, 70, and 62.5, respectively; the total score was 362.5 (Figure 1). Calibration analysis indicated that the line graph model developed in this study predicts the risk of CRKP infection in children with a consistency index of 0.872 (95 CI: 0.844–0.901), as shown in Figure 2. The calibration curve indicated a good consistency between the observed and predicted values, as shown in Figure 3.
 |
Figure 1 Risk model of carbapenem-resistant Klebsiella pneumoniae (CRKP) for children. |
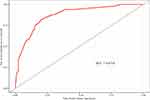 |
Figure 2 Receiver-operating characteristic curve for predicting carbapenem-resistant Klebsiella pneumoniae (CRKP) infection risk in children. AUC, area under the curve. |
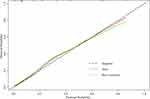 |
Figure 3 Calibration curve of the line graph model for predicting the risk of carbapenem-resistant Klebsiella pneumoniae (CRKP) occurrence in children. |
Discussion
Once children are infected with CRKP, the mortality rate is high and the prognosis is poor.10 Therefore, there is a need to understand the risk factors for CRKP infection in children for the purpose of formulating the treatment plan, choosing antibiotics, and improving prognosis.
Compared with the traditional logistic regression analysis, the established predictive model can calculate the corresponding scores of each influencing factor, add up the total scores and match them to the predicted P value, thereby providing the most accurate prediction by simple graphical representation.
This type of model has been widely used in clinical cohort studies.9,11 In this study, a linear model predicting the risk associated with drug-resistant K. pneumoniae infection in children was constructed based on clinical-related predictive variables and was used to assess the risk of CRKP infection in children; we intended to provide a reliable basis for reducing and preventing the drug resistance of K. pneumoniae in children.
The present study showed that age, admission to the ICU, mechanical ventilation, surgical history, and glucocorticoid use were independent risk factors for CRKP infection in children. Additionally, the correction curve indicated that the consistency between the observed value and the predicted value was good. The established nomogram had high accuracy and predictive ability.
Unlike the conclusion of Zhang, here we concluded that the younger the child, the higher the risk of drug resistance of K. pneumoniae (OR = 0.104, 95% CI: 0.026–0.408).12 Research findings showed that nosocomial infection surveillance revealed an unexpectedly high rate of failure in neonatal units to meet hospital hygiene and hand hygiene requirements.5 Bai et al found that nosocomial surveillance systems are needed to limit the spread of the infection caused by these pathogens resulting from the environmental exposure in NICUs. In the delivery room, neonatal intensive care unit (NICU), and the follow-up clinic, in collaboration with the interdisciplinary group, contact precautions and isolation procedures were instituted. None of the infants exhibited infection with CP-CRE.13 Seesahai et al have found that simple infection control measures involving contact precautions, staff education, and parental cohorting can be useful and cost-effective in preventing transmission. Attention to NICUspecific measures, including screening of at-risk mothers (in vitro fertilization conception) and their probands, careful handling of breastmilk, judicious antibiotic choice, and duration of treatment, are warranted.14 Second, the risk of K. pneumoniae resistance is high (OR = 2.829, 95% CI: 1.138–7.030). The same results are valid in adult studies. Most critical patients in the ICU have chronic or acute illnesses, especially with the use of antibiotics and immunosuppressants, and poor internal airflow. ICU has become the department with the highest rate of drug-resistant bacterial infection.15–17 The results of this study showed that mechanical ventilation was associated with a high risk of drug-resistant infection in children. In addition, K. pneumoniae can deposit on the artificial equipment in the form of a biofilm and remain viable for a long time, which is consistent with the conclusion that the infection rate of CRKP in mechanically ventilated patients is generally higher than that in non-mechanically ventilated patients.12,16 Moreover, the present study found a higher risk of drug-resistant K. pneumoniae (OR = 5.005, 95% CI: 1.507–16.618) in children with a history of previous surgery; for children with more complex disease types, the body’s resistance to bacteria is poor, and the recent use of antibacterial drugs may lead to drug-resistant infections, consistent with relevant research conclusions.18,19 Finally, children who received glucocorticoids before infection had a low risk of Klebsiella pneumoniae resistance (OR = 0.235, 95% CI: 0.099–0.557), which may be because most glucocorticoids in this study were administered by atomization, which has relatively little influence on the body’s immunity and does not increase the risk of drug-resistant bacteria. For example, inhaled budesonide has been widely used in neonatal respiratory distress syndrome, but no obvious adverse reactions have been registered.20,21
Zhang et al found that hematologic malignancies and previous cephalosporin administration were associated with the development of CRKP BSI, while mechanical ventilation, septic shock, and CRKP infection were independent mortality predictors for K. pneumoniae associated BSI (Zhang Y et al 2018).12 Bor M et al found that previous antifungal use, congenital anomalies, and TPN use were found to be independent risk factors for mortality in neonates with CRKP infection.22 In contrast, we found that no antimicrobial agents were identified as risk factors for CRKP, partly because of the strict management of the clinical use of antibiotics in our hospital in recent years.
Based on logistic regression analysis, this study constructed a linear graph model to predict the risk of K. pneumoniae infection. The total risk score was 362.5. The higher the total risk score, the higher was the risk of drug-resistant K. pneumoniae infection. The probability of occurrence of drug-resistant K. pneumoniae in a child can be obtained using the line chart prediction model, and the intuitive prediction of the occurrence of drug-resistant K. pneumoniae in children can be realized. The ROC curve analysis showed that the area under the curve was 0.872 (95% CI = 0.844–0.901), indicating that the prediction efficiency was good.
The shortcoming of this study is that due to the limited sample size from a single center, there is a certain degree of data bias. Therefore, the accuracy of the model still needs multi-center, large sample verification.
Conclusions
In conclusion, This study successfully established a model based on the risk factors, with high accuracy and good predictive value for CRKP in children. Hospitals should take necessary preventive measures against the risk factors for drug-resistant bacteria, such as optimizing the configuration of ICU space, timely isolation of infected children, and adequate disinfection of ICU equipment which may reduce CRKP infection rate.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
The project titled“Risk factors and predictive nomogram for carbapenem-resistant Klebsiella pneumoniae in children in a grade 3 first-class general hospital in Central China” was approved by the Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China.(Approval Number: 2022-RE-035). Informed consent was waived by our Institutional Review Board because of the retrospective nature of our study, all data is limited to research and analysis purposes and confidential. This study was conducted in accordance with the Declaration of Helsinki. All data used in the study is confidential.
Acknowledgment
The authors would like to thank for WuwuShi and Saisai Cheng for their valuable assistance in creating the data set used in this study.
Lijuan Ning and Yuting Fang are co-first authors.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Shen P, Berglund B, Chen Y, et al. Hypervirulence markers among Non-ST11 strains of carbapenem- and multidrug-resistant Klebsiella pneumoniae Isolated from patients with bloodstream infections. Front Microbiol. 2020;11:1199. PMID: 32625176; PMCID: PMC7314899. doi:10.3389/fmicb.2020.01199
2. Fu P, Xu H, Jing C, et al. Bacterial epidemiology and antimicrobial resistance profiles in children reported by the ISPED program in China, 2016 to 2020. Microbiol Spectr. 2021;22(9):e0028321. PMID: 34730410; PMCID: PMC8567242. doi:10.1128/Spectrum.00283-21
3. China Antimicrobial Resistance Surveillance System. 2014至2017年中国儿童及新生儿患者细菌耐药监测研究 [Surveillance of bacterial resistance in children and newborns across China from 2014 to 2017]. Zhonghua Yi Xue Za Zhi. 2018;98:3279–3287. Chinese. Chinese. doi:10.3760/cma.j.issn.0376-2491.2018.40.013
4. Guo Y, Hu FP, Zhu DM, et al. 儿童临床分离碳青霉烯类耐药肠杆菌科细菌的耐药性变迁 [Antimicrobial resistance changes of carbapenem-resistant Enterobacteriaceae strains isolated from children]. Zhonghua Er Ke Za Zhi. 2018;56:907–914. Chinese. Chinese. doi:10.3760/cma.j.issn.0578-1310.2018.12.005
5. Yang Y, Liu J, Muhammad M, et al. Factors behind the prevalence of carbapenem-resistant Klebsiella pneumoniae in pediatric wards. Medicine. 2021;100:e27186. PMID: 34516520; PMCID: PMC8428699. doi:10.1097/MD.0000000000027186
6. Park SY. Nomogram: an analogue tool to deliver digital knowledge. J Thorac Cardiovasc Surg. 2018;155:1793. PMID: 29370910. doi:10.1016/j.jtcvs.2017.12.107
7. Jeong SH, Kim RB, Park SY, et al. Nomogram for predicting gastric cancer recurrence using biomarker gene expression. Eur J Surg Oncol. 2020;46:195–201. PMID: 31564475. doi:10.1016/j.ejso.2019.09.143
8. Jiang S, Zhao R, Li Y, et al. Prognosis and nomogram for predicting postoperative survival of duodenal adenocarcinoma: a retrospective study in China and the SEER database. Sci Rep. 2018;8:7940. PMID: 29786691; PMCID: PMC5962558. doi:10.1038/s41598-018-26145-6
9. Wu J, Zhang H, Li L, et al. A nomogram for predicting overall survival in patients with low-grade endometrial stromal sarcoma: a population-based analysis. Cancer Commun. 2020;40:301–312. PMID: 32558385; PMCID: PMC7365459. doi:10.1002/cac2.12067
10. Yu J, Tan K, Rong Z, et al. Nosocomial outbreak of KPC-2- and NDM-1-producing Klebsiella pneumoniae in a neonatal ward: a retrospective study. BMC Infect Dis. 2016;16(1):563. doi:10.1186/s12879-016-1870-y
11. Lv J, Liu YY, Jia YT, et al. A nomogram model for predicting prognosis of obstructive colorectal cancer. World J Surg Oncol. 2021;19(1):337. PMID: 34857001; PMCID: PMC8638364. doi:10.1186/s12957-021-02445-6
12. Zhang Y, Guo LY, Song WQ, Wang Y, Dong F, Liu G. Risk factors for carbapenem-resistant K. pneumoniae bloodstream infection and predictors of mortality in Chinese paediatric patients. BMC Infect Dis. 2018;18:248. PMID: 29855274; PMCID: PMC5984460. doi:10.1186/s12879-018-3160-3
13. Bai Y, Shao C, Hao Y, Wang Y, Jin Y. Using whole genome sequencing to trace, control and characterize a hospital infection of IMP-4-Producing Klebsiella pneumoniae ST2253 in a neonatal unit in a tertiary hospital, China. Front Public Health. 2021;9:755252. PMID: 34976919; PMCID: PMC8715938. doi:10.3389/fpubh.2021.755252
14. Seesahai J, Church PT, Asztalos E, Eng-Chong M, Arbus J, Banihani R. Neonates with maternal colonization of carbapenemase-producing, carbapenem-resistant enterobacteriaceae: a mini-review and a suggested guide for preventing neonatal infection. Children. 2021;8:399. PMID: 34063374; PMCID: PMC8156425. doi:10.3390/children8050399
15. Candevir Ulu A, Kurtaran B, Inal AS, et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infection: a serious threat in ICUs. Med Sci Monit. 2015;21:219–224. PMID: 25595166; PMCID: PMC4304439. doi:10.12659/MSM.892516
16. Liu P, Li X, Luo M, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection: a meta-analysis. Microb Drug Resist. 2018;24:190–198. PMID: 28749714; PMCID: PMC5873294. doi:10.1089/mdr.2017.0061
17. Wu D, Cai J, Liu J. Risk factors for the acquisition of nosocomial infection with carbapenem-resistant Klebsiella pneumoniae. South Med J. 2011;104:106–110. PMID: 21258230. doi:10.1097/SMJ.0b013e318206063d
18. Tanır Basaranoglu S, Ozsurekci Y, Aykac K, et al. A comparison of blood stream infections with extended spectrum beta-lactamase-producing and non-producing Klebsiella pneumoniae in pediatric patients. Ital J Pediatr. 2017;43(1):79. PMID: 28899399; PMCID: PMC5596860. doi:10.1186/s13052-017-0398-0
19. Akturk H, Sutcu M, Somer A, et al. Carbapenem-resistant Klebsiella pneumoniae colonization in pediatric and neonatal intensive care units: risk factors for progression to infection. Braz J Infect Dis. 2016;20:134–140. PMID: 26867474. doi:10.1016/j.bjid.2015.12.004
20. Berglund B, Hoang NTB, Lundberg L, et al. Clonal spread of carbapenem-resistant Klebsiella pneumoniae among patients at admission and discharge at a Vietnamese neonatal intensive care unit. Antimicrob Resist Infect Control. 2021;10:162. PMID: 34801068; PMCID: PMC8606094. doi:10.1186/s13756-021-01033-3
21. Elfarargy MS, Abu-Risha SE, Younis RL. Therapeutic effect of inhaled budesonide in transient tachypnea of newborn: a placebo-controlled study. J Popul Ther Clin Pharmacol. 2020;27:e78–e86. PMID: 32543161. doi:10.15586/jptcp.v27i2.663
22. Bor M, Ilhan O. Carbapenem-resistant Klebsiella pneumoniae outbreak in a neonatal intensive care unit: risk factors for mortality. J Trop Pediatr. 2021;67:fmaa057. PMID: 32778897. doi:10.1093/tropej/fmaa057
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
