Back to Journals » Infection and Drug Resistance » Volume 16
Risk Factors and Outcomes of Patients with Carbapenem-Resistant Pseudomonas aeruginosa Bloodstream Infection
Authors Wei X, Li L, Li M , Liang H, He Y, Li S
Received 6 November 2022
Accepted for publication 30 December 2022
Published 19 January 2023 Volume 2023:16 Pages 337—345
DOI https://doi.org/10.2147/IDR.S396428
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Xianzhen Wei,* Linlin Li,* Meng Li, Hongjie Liang, Yu He, Shan Li
Department of Clinical Laboratory, the First Affiliated Hospital of Guangxi Medical University, Nanning, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shan Li, Email [email protected]
Purpose: The rising incidence of carbapenem-resistant Pseudomonas aeruginosa (PA) bloodstream infection (BSI) has made the selection of antibiotic therapy more difficult and caused high mortality. This study was aimed at exploring the risk factors for carbapenem-resistant Pseudomonas aeruginosa (CRPA) bloodstream infection and identifying the risk factors for the outcomes of patients with PA-BSI.
Methods: We performed a retrospective cohort study of patients with PA-BSI in a tertiary hospital from January 2017 to December 2021 in China. Epidemiological, clinical, and microbiological characteristics were described. Risk factors for CRPA-BSI and the outcomes of PA-BSI inpatients were identified, using multivariate logistic regression analysis.
Results: A total of 198 PA-BSI inpatients were included. The negative outcome rate was significantly higher in patients infected with CRPA (15/34, 44.12%) than with carbapenem-susceptible Pseudomonas aeruginosa (CSPA) (35/164, 21.34%), and the difference was statistically significant (P=0.005). Multivariate logistic regression analysis showed that previous exposure to carbapenem (OR 3.519, 95% CI 1.359– 9.110, P=0.010) was an independent risk factor for CRPA-BSI. In addition, CRPA (OR 1.615, 95% CI 0.626– 4.171, P=0.32) was not an independent risk factor for negative outcome among PA-BSI inpatients.
Conclusion: Our study showed that previous exposure to carbapenem was an independent risk factor for CRPA-BSI. CRPA was not an independent risk factor for a negative outcome in PA-BSI inpatients.
Keywords: carbapenem-resistant, Pseudomonas aeruginosa bloodstream infection, risk factors, outcomes
Introduction
Pseudomonas aeruginosa is one of the mainly Gram-negative bacteria (GNB) species associated with nosocomial infections that cause high morbidity and mortality rates.1,2 Indeed, the mortality rate of PA bloodstream infection reportedly ranges from 20% to 50%.1,3,4 With the widespread use of broad-spectrum antibiotics, CRPA, multidrug-resistant (MDR) and extensively drug-resistant (XDR) PA isolates are gradually increasing.5,6 According to the China Antimicrobial Surveillance Network (https://www.chinets.com/Data/GermYear), the resistance rates of imipenem and meropenem in PA infections were 23.6% and 20.9% in 2017, and 23% and 18.9% in 2021, respectively. The resistance rates of imipenem and meropenem in China have slightly decreased over the past 5 years but remained at a high level. Carbapenem antibiotics are commonly used for the treatment of PA infection and their high resistance rates limit the choices of antimicrobial therapy.7 Despite a great deal of research on epidemiology, the incidence of CRPA remains high, and support for CRPA infection management remains insufficient. Meanwhile, risk factors for the outcomes of patients with PA infection remain unclear. Recio et al reported that inappropriate empirical therapy, XDR isolate, severe neutropenia and septic shock were associated with high mortality in PA bacterial pneumonia.8 Teelucksingh et al identified that septic shock, age and Pitt bacteremia score ≥4 were risk factors for poor outcome in PA-BSI.9 Recognizing the risk factors for the prognosis of patients with PA infection is important, so that special attention would be paid to patients with these risk factors to improve the prognosis.
Therefore, our study aimed at exploring the epidemiology, clinical characteristics, antimicrobial resistance, and risk factors of patients with CRPA-BSI, we also identified the risk factors for the outcomes of patients with PA-BSI. This study may provide clues for clinicians to take special measures to curb the spread of CRPA and adjust their treatment strategies.
Methods
Study Setting
This was a retrospective study conducted at the First Affiliated Hospital of Guangxi Medical University (2750-bed) from January 2017 to December 2021. Data from patients with PA-BSI were collected, including patients’ demographic and clinical characteristics, comorbidities, laboratory examination, invasive procedures, antibiotics’ exposure and outcomes. The inclusion criteria were as follows: the first episode of PA occurred during the study period, and patients met the diagnostic criteria for bloodstream infection, only the first episode of PA-BSI was included, and recurrent infections were excluded. In addition, outpatients and incomplete or missing medical records were also excluded.
To identify the risk factors for CRPA-BSI, the patients were divided into two groups: a CRPA group and a CSPA group. In addition, to explore the risk factors for the outcomes of PA-BSI, patients were divided into a negative outcome group and a positive outcome group.
Definitions
Bloodstream infection was defined as viable bacteria appeared in the bloodstream and cause clinical signs or symptoms of infection according to the definitions for bloodstream infection by the Centers for Disease Control.10 CRPA was defined as a minimum inhibitory concentration of ≥8μg/mL imipenem or meropenem or disk zone diameter ≤15mm for meropenem or imipenem consistent with the breakpoints of 2021 Clinical and Laboratory Standards Institute (CLSI) guidelines.11 MDR was defined as non-susceptibility to at least one agent in three or more antimicrobial categories, XDR as non-susceptibility to at least one agent in all but two or fewer antimicrobial categories (ie, bacterial isolates remain susceptible to only one or two categories).12 Outcomes were classified as follows: according to the medical records, patients were cured or in better condition when discharged were identified as positive outcome, dead or in serious condition when discharged were recognized as negative outcome.
Bacterial Identification and Antimicrobial Susceptibility Testing
In this study, all isolates were identified by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) (bioMérieux, Lyons, France), or the VITEK2 Compact system (bioMérieux, Marcy l’Etoile, France). All antibiotic susceptibility tests were performed using the VITEK 2 Compact system or the disk-diffusion method, except Polymyxin B, which were performed with broth microdilution testing, and the results were interpreted as recommended by the Clinical and Laboratory Standards Institute (CLSI), version 2021. Escherichia coli (ATCC25922), Klebsiella pneumoniae (ATCC700603), and Pseudomonas aeruginosa (ATCC27853) were used as the quality control bacterial strains.
Statistical Analysis
Continuous variables with normal distribution were expressed as the mean ± standard deviation (using Student’s t-test) or as the median (interquartile range [IQR]) (using the Mann–Whitney U-test) when the distribution was not normal. Categorical variables were expressed as counts or counts/total (percentages) and were analyzed using the Chi-squared test or two-tailed Fisher's exact test. Multivariate logistic regression analysis was used to identify the risk factors for CRPA-BSI and the outcomes of PA-BSI. The results were reported as the odds ratio (OR) and 95% confidence interval (CI). P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 23.0.
Results
Demographics and Clinical Characteristics of Patients with PA-BSI
Excluded 15 inpatients with missing or incomplete data, a total of 198 PA-BSI inpatients were enrolled in our study. Of the 198 PA-BSI inpatients, there were 130 males (65.66%) and 68 females (34.34%); the median age and the length of stay were 37(17–56) years and 26.5(14–38) days, respectively. PA inpatients predominantly came from the hematology department (34.30%), pediatric hematology ward (11.10%), intensive care unit (ICU 9.09%), or stem cell transplantation department (8.60%). The main comorbidities were hematological diseases (54.55%), pulmonary diseases (39.90%) (including chronic obstructive pulmonary disease and pneumonia), and hepatobiliary and pancreatic diseases (32.83%), as shown in Table 1.
 |
Table 1 Demographics, Clinical Characteristics, and Outcomes of Patients with PA-BSI |
Antimicrobial Susceptibility Results
The antimicrobial susceptibility results, as shown in Table 2, revealed the following total antibiotic resistance rates: carbapenems (17.17%), imipenem (15.15%), meropenem (13.64%), amikacin (2.02%) and polymyxin B (0.0%). Additionally, the highest and lowest resistance rates of carbapenems were 31.03% and 7.14% in 2020 and 2019, respectively. Other antibiotic resistance rates are shown in Table 2.
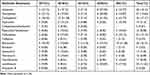 |
Table 2 Antimicrobial Susceptibility Results |
Risk Factors for CRPA-BSI
Univariate analysis showed that there were nine risk factors associated with CRPA-BSI (Table 1): previous exposure to carbapenems or glycopeptides, leukopenia, neutropenia, cardiovascular diseases, longer hospital stay before bacteremia onset, mechanical ventilation, central venous catheterization, placement of a drainage tube. The mortality rate of the CRPA group and CSPA group were 8.82% and 7.32%, respectively. In addition, patients with CRPA-BSI tended to have negative outcome compared with patients with CSPA-BSI (P = 0.005), as shown in Table 1. The multivariate logistic regression analysis revealed that previous exposure to carbapenem (OR 3.519, 95% CI 1.359–9.110, P=0.010) was an independent risk factor for CRPA-BSI, as shown in Table 3.
 |
Table 3 Multivariate Analysis of the Risk Factors for CRPA-BSI |
Risk Factors for the Outcomes of PA-BSI Inpatients
The negative and positive outcome rates of PA-BSI inpatients were 25.25% (50/198) and 74.75% (148/198), respectively. Univariate analyses showed that the risk factors for negative outcome of PA-BSI mainly included CRPA isolation, previous exposure to cephalosporins, tigecycline, carbapenems or glycopeptides, as shown in Table 4. Multivariate logistic regression analysis showed that CRPA was not an independent risk factor for negative outcome of PA-BSI (OR 1.615, 95% CI 0.626–4.171, P=0.32). As shown in Table 5.
 |
Table 4 Risk Factors for the Outcomes of PA-BSI Inpatients |
 |
Table 5 Multivariate Analysis for the Outcomes of PA-BSI Inpatients |
Discussion
Pseudomonas aeruginosa is one of the main causes of nosocomial infections especially when patients are immunocompromised, readily causes PA bloodstream infections, which are often severe and difficult to treat due to the frequent emergence of antibiotic-resistant mutants during therapy.13,14 With the widespread use of carbapenems and other broad-spectrum antibiotics, carbapenem resistance and even MDR/XDR PA have increased, limiting the choice of antimicrobial therapy. Therefore, our study explored the risk factors for CRPA-BSI and the outcomes of PA-BSI and aimed at providing useful advice for interventions and control of CRPA-BSI.
Univariate analysis showed that risk factors for CRPA-BSI mainly included previous exposure to carbapenems or glycopeptides, leukopenia, neutropenia, longer hospital stays before bacteremia onset, mechanical ventilation, central venous catheterization, placement of a drainage tube. Further, multivariate logistic regression analysis showed that previous exposure to carbapenems was an independent risk factor for CRPA-BSI, which was consistent with previous publications.15–17 Righi et al performed a meta-analysis and found that carbapenem resistance appeared to be associate with prior use of carbapenems.15 Shi et al identified that prior use of carbapenems was an independent risk factor for development of CRPA-BSI in a retrospective analysis.16 Raman et al also identified that previous exposure to carbapenems was significantly correlated with acquisition of CRPA compared with CSPA.17 The acquisition of CRPA may be because that PA is a highly diverse pathogen which capable of adaptation to the surrounding environment, when under antibiotic selective pressure, the induced response promotes bacterial survival and develops antibiotic resistance.18 The mechanism of PA acquired resistance to carbapenems may be due to the efflux pumps, low outer membrane permeability, production of carbapenemase and AmpC β-lactamase.19–23 In addition, PA also shows resistance to many other available antibiotics via the acquisition of chromosomal mutations and transferable resistance determinants, especially those encoding carbapenemases frequently co-transferred with aminoglycoside-modifying enzymes.20,24–26
Our study showed that PA-BSI inpatients mainly came from the hematology department (34.30%) and pediatric hematology department (11.10%), and the main comorbidities were hematologic diseases(54.55%), pulmonary diseases (39.90%) (including chronic obstructive pulmonary disease and pneumonia), and hepatobiliary and pancreatic diseases (32.83%). Patients with hematologic diseases are vulnerable to PA-BSI due to unique disease characteristics, including severe neutropenia, prolonged hospitalizations, and special treatments such as corticosteroids, chemotherapy, and hematopoietic stem cell transplantation (HSCT).15,27–29 Pulmonary disease patients tend to have damaged respiratory mucosal, which may lead to the colonize PA entering the blood stream and causing PA-BSI.8,9,30,31 Patients with hepatobiliary and pancreatic diseases generally undergo surgery and drainage, thus increasing their risk of being infected by bacterial and resulting in PA-BSI.14,21,24
Our study revealed that PA showed resistance to most antimicrobials, which is consistent with previous studies.21,24,32 We found that among the 198 PA isolates, the highest resistance rate was found in carbapenems (17.17%), followed by aztreonam (16.15%), and ceftazidime (12.12%). In contrast, PA showed less resistance to amikacin, with a rate of 2.02%. In addition, no PA isolations showed resistance to polymyxin B. Polymyxins (polymyxin B and colistin) were regarded as the alternative therapeutic option for many cases of MDR/XDR PA infections. However, their usage is complicated due to narrow therapeutic window and loading dose polymyxins frequently associated with higher risk of nephrotoxicity.21,33–35 Furthermore, whether polymyxins-based combination therapy in CR/MDR/XDR PA infections associated with better clinical outcomes remains unclear. A cohort study showed that colistin-based combination therapy with two active drugs for XDR PA pneumonia patients was associated with better survival than monotherapy.36 Interestingly, a systematic review about combination therapy in CRGNB showed that polymyxin combined with tigecycline or carbapenems and/or aminoglycosides had an unadjusted association with survival; however, when bias studies removed, the association between combination therapy and survival diminished, and unnecessary use of carbapenems may cause prevalence of CRGNB.37 At present, carbapenems are still commonly used for PA infection,38 and our study found that previous exposure to carbapenems was an independent risk factor for CRPA-BSI, so it would be important to prescribe carbapenems prudently to reduce the incidence of CRPA infection.
Previous studies revealed that resistance to carbapenems increased the incidence of mortality in patients with PA infection.4,15,39 A meta-analysis showed that carbapenem resistance had a deleterious effect on the mortality of PA-BSI.4 Righi et al demonstrated that there was an association between mortality and carbapenem resistance in a meta-analysis.15 Lee et al found a higher mortality rate among patients with carbapenem-only resistant PA compared to all susceptible PA.39 Interestingly, our study found no statistically significant difference on in-hospital mortality rates between the CRPA and CSPA groups, probably because many Chinese choose to be discharged home when they are gravely ill. Thus, there was a relatively lower in-hospital mortality rate, with a rate of 8.82% and 7.32% in the CRPA group and CSPA group, respectively. However, when comparing positive and negative outcomes, there was a statistically significant difference (p=0.005). Thus, we divided PA-BSI inpatients into two groups (a positive outcome group and a negative outcome group) and explored the risk factors for the outcomes of PA-BSI inpatients.
Univariate analysis showed that moderate anemia, hypoalbuminemia, diabetes mellitus, mechanical ventilation and central venous catheterization were associated with negative outcomes. Invasive procedures such as central venous catheterization and mechanical ventilation, increased the chance of PA-BSI and affected the outcomes of patients, which was consistent with previous studies.16 Univariate analysis also showed that CRPA-BSI inpatients were likelier to have a negative outcome. However, when it came to the multivariate logistic regression analysis, CRPA was not an independent risk factor for negative outcome, which was consistent with previous reports.7,40 Buehrle et al previous found that there was no significant difference on 14-day mortality rates among patients with CRPA and CSPA infection.7 A prospective multicenter study identified that carbapenem resistance significantly increased the risk of mortality from the fifth day after the onset of PA-BSI, but this difference diminished during the first 4 days or as the comorbidities increased.40 These may be because that compared to the resistant bacteria, the patient’s underlying diseases, primary site of infection, virulence of the pathogens, clinical characteristics and management probably play more important roles in the outcomes of PA-BSI.7,40–42 Indeed, impact of CRPA-BSI on outcomes remains controversial, and more prospective multicenter studies are needed.
Admittedly, our study had several limitations. First, it was a retrospective analysis with a relatively small size of samples, and our study conducted at a single medical center which may just reflects the experience of one single center, and the results may not be applicable to other settings. Second, the risk factors included were limited, factors such as Charlson comorbidity index and initial antibiotic therapy that may have influenced the outcomes of PA-BSI were not included in our study.8,42,43 Third, we did not study the mechanism of resistance, which would be the key to determining the relationship between CRPA drug resistance types and clinical characteristics.
Conclusion
Our study showed that previous exposure to carbapenems was an independent risk factor for CRPA-BSI. In addition, PA shows resistance to a variety of antibiotics. Carbapenems and other antibiotics should be used appropriately to reduce the incidence of CRPA-BSI and antibiotic resistance.
Data Sharing Statement
Any datasets analyzed during this study are available from the corresponding author at reasonable request.
Ethical Approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University. The need for written informed consent was waived due to the retrospective non-interventional study and the research did not involve personal privacy or commercial interests. We declare that this study was conducted in accordance with the principles of the Declaration of Helsinki and the information of all patients included in this study was confidential.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (81460431), the Natural Science Foundation of Guangxi (2018GXNSFAA 281123) and the scientific research project of Guangxi Health Commission (No. Z20201166).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Raúl Recio MM, Esther V, Jennifer V, María Ángeles O, Jaime L-T, Fernando C. Predictors of Mortality in Bloodstream Infections Caused by Pseudomonas aeruginosa and Impact of Antimicrobial Resistance and Bacterial Virulence. Antimicrob Agents Chemother. 2020;64(2):e01759–01719. doi:10.1128/AAC.01759-19
2. Gaynes REJ. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis. 2005;41:848–854. doi:10.1086/432803
3. Lodise TP, Bassetti M, Ferrer R, et al. All-cause mortality rates in adults with carbapenem-resistant Gram-negative bacterial infections: a comprehensive review of pathogen-focused, prospective, randomized, interventional clinical studies. Expert Rev Anti Infect Ther. 2022;20(5):707–719. doi:10.1080/14787210.2022.2020099
4. Zhang Y, Chen X-L, Huang A-W, et al. Mortality attributable to carbapenem-resistant Pseudomonas aeruginosa bacteremia: a meta-analysis of cohort studies. Em Microbes Infections. 2019;5(1):1–6.
5. Jernigan JA, Hatfield KM, Wolford H, et al. Multidrug-resistant bacterial infections in U.S. hospitalized patients, 2012-2017. N Engl J Med. 2020;382(14):1309–1319. doi:10.1056/NEJMoa1914433
6. Montero MM, Lopez Montesinos I, Knobel H, et al. Risk factors for mortality among patients with Pseudomonas aeruginosa bloodstream infections: what is the influence of XDR phenotype on outcomes? J Clin Med. 2020;9(2):514. doi:10.3390/jcm9020514
7. Buehrle DJ, Shields RK, Clarke LG, Potoski BA, Clancy CJ, Nguyen MH. Carbapenem-resistant Pseudomonas aeruginosa bacteremia: risk factors for mortality and microbiologic treatment failure. Antimicrob Agents Chemother. 2017;61(1). doi:10.1128/AAC.01243-16
8. Recio R, Viedma E, Gonzalez-Bodi S, et al. Clinical and bacterial characteristics of Pseudomonas aeruginosa affecting the outcome of patients with bacteraemic pneumonia. Int J Antimicrob Agents. 2021;58(6):106450. doi:10.1016/j.ijantimicag.2021.106450
9. Teelucksingh K, Shaw E. Clinical characteristics, appropriateness of empiric antibiotic therapy, and outcome of Pseudomonas aeruginosa bacteremia across multiple community hospitals. Eur J Clin Microbiol Infect Dis. 2021;41(1):53–62. doi:10.1007/s10096-021-04342-y
10. Julia S, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128–140. doi:10.1016/0196-6553(88)90053-3
11. Performance CLSI. Standards for Antimicrobial Susceptibility Testing.
12. Magiorakos A-P, Srinivasan A, Carey RB. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
13. Liu T, Zhang Y, Wan Q. Pseudomonas aeruginosa bacteremia among liver transplant recipients. Infect Drug Resist. 2018;11:2345–2356. doi:10.2147/IDR.S180283
14. Zhang Y, Li Y, Zeng J, et al. Risk factors for mortality of inpatients with Pseudomonas aeruginosa bacteremia in China: impact of resistance profile in the mortality. Infect Drug Resist. 2020;13:4115–4123. doi:10.2147/IDR.S268744
15. Righi E, Peri AM, Harris PNA, et al. Global prevalence of carbapenem resistance in neutropenic patients and association with mortality and carbapenem use systematic review and meta-analysis. J Antimicrobial Chemother;2016;dkw459. doi:10.1093/jac/dkw459
16. Shi Q, Huang C, Xiao T, Wu Z, Xiao Y. A retrospective analysis of Pseudomonas aeruginosa bloodstream infections: prevalence, risk factors, and outcome in carbapenem-susceptible and -non-susceptible infections. Antimicrob Resist Infect Control. 2019;8(1). doi:10.1186/s13756-019-0520-8
17. Raman G, Avendano EE, Chan J, Merchant S, Puzniak L. Risk factors for hospitalized patients with resistant or multidrug-resistant Pseudomonas aeruginosa infections: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2018;7:79. doi:10.1186/s13756-018-0370-9
18. Pachori P, Gothalwal R, Gandhi P. Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes Dis. 2019;6(2):109–119. doi:10.1016/j.gendis.2019.04.001
19. Livermore DM. Multiple mechanisms of antimicrobial resistance in Pseudomonas aeruginosa: our worst nightmare? Antimico Resistance. 2002;34(5):634–640.
20. Geisinger E, Isberg RR. Interplay between antibiotic resistance and virulence during disease promoted by multidrug-resistant bacteria. J Infect Dis. 2017;215(suppl_1):S9–S17. doi:10.1093/infdis/jiw402
21. Horcajada JP, Montero M, Oliver A, et al. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa infections. Clin Microbiol Rev. 2019;32(4). doi:10.1128/CMR.00031-19
22. Del Barrio-Tofino E, Sanchez-Diener I, Zamorano L, et al. Association between Pseudomonas aeruginosa O-antigen serotypes, resistance profiles and high-risk clones: results from a Spanish nationwide survey. J Antimicrob Chemother. 2019;74(11):3217–3220. doi:10.1093/jac/dkz346
23. Breidenstein EB, de la Fuente-Nunez C, Hancock RE. Pseudomonas aeruginosa: all roads lead to resistance. Trends Microbiol. 2011;19(8):419–426. doi:10.1016/j.tim.2011.04.005
24. Del Barrio-Tofino E, Lopez-Causape C, Cabot G, et al. Genomics and susceptibility profiles of extensively drug-resistant Pseudomonas aeruginosa Isolates from Spain. Antimicrob Agents Chemother. 2017;61(11). doi:10.1128/AAC.01589-17
25. Del Barrio-Tofiño E, Zamorano L, Cortes-Lara S, et al. Spanish nationwide survey on Pseudomonas aeruginosa antimicrobial resistance mechanisms and epidemiology. J Antimicrobial Chemother. 2019;74(7):1825–1835. doi:10.1093/jac/dkz147
26. Potron A, Poirel L, Nordmann P. Emerging broad-spectrum resistance in Pseudomonas aeruginosa and Acinetobacter baumannii: mechanisms and epidemiology. Int J Antimicrob Agents. 2015;45(6):568–585. doi:10.1016/j.ijantimicag.2015.03.001
27. Viasus D, Puerta-Alcalde P, Cardozo C, et al. Predictors of multidrug-resistant Pseudomonas aeruginosa in neutropenic patients with bloodstream infection. Clin Microbiol Infection. 2020;26(3):345–350. doi:10.1016/j.cmi.2019.07.002
28. Zhao Y, Lin Q, Liu L, et al. Risk factors and outcomes of antibiotic-resistant Pseudomonas aeruginosa bloodstream infection in adult patients with acute leukemia. Clin Infectious Dis. 2020;71(Supplement_4):S386–S393. doi:10.1093/cid/ciaa1522
29. Marin M, Gudiol C, Ardanuy C, et al. Bloodstream infections in neutropenic patients with cancer: differences between patients with haematological malignancies and solid tumours. J Infection. 2014;69(5):417–423. doi:10.1016/j.jinf.2014.05.018
30. Babich T, Naucler P, Valik JK, et al. Risk factors for mortality among patients with Pseudomonas aeruginosa bacteraemia: a retrospective multicentre study. Int J Antimicrob Agents. 2020;55(2):105847. doi:10.1016/j.ijantimicag.2019.11.004
31. Recio R, Villa J, Viedma E, Orellana MÁ, Lora-Tamayo J, Chaves F. Bacteraemia due to extensively drug-resistant Pseudomonas aeruginosa sequence type 235 high-risk clone: facing the perfect storm. Int J Antimicrob Agents. 2018;52(2):172–179. doi:10.1016/j.ijantimicag.2018.03.018
32. Tam VH, Rogers CA, Chang KT, Weston JS, Caeiro JP, Garey KW. Impact of multidrug-resistant Pseudomonas aeruginosa bacteremia on patient outcomes. Antimicrob Agents Chemother. 2010;54(9):3717–3722. doi:10.1128/AAC.00207-10
33. Satlin MJ. Languid uptake of ceftazidime-avibactam for carbapenem-resistant gram-negative infections and continued reliance on polymyxins. Clin Infect Dis. 2021;72(4):622–625. doi:10.1093/cid/ciaa065
34. Motsch J. RESTORE-IMI 1: a multicenter, randomized, double-blind trial comparing efficacy and safety of imipenem/relebactam vs colistin plus imipenem in patients with imipenem-nonsusceptible bacterial infections. Clin Infect Dis. 2020;70(9):1799–1808. doi:10.1093/cid/ciz530
35. Kadri SS, Hohmann SF, Orav EJ, et al. Tracking colistin-treated patients to monitor the incidence and outcome of carbapenem-resistant Gram-negative infections. Clin Infect Dis. 2015;60(1):79–87. doi:10.1093/cid/ciu741
36. Khawcharoenporn T, Chuncharunee A, Maluangnon C, Taweesakulvashra T, Tiamsak P. Active monotherapy and combination therapy for extensively drug-resistant Pseudomonas aeruginosa pneumonia. Int J Antimicrob Agents. 2018;52(6):828–834. doi:10.1016/j.ijantimicag.2018.09.008
37. Zusman O, Altunin S, Koppel F, Dishon Benattar Y, Gedik H, Paul M. Polymyxin monotherapy or in combination against carbapenem-resistant bacteria: systematic review and meta-analysis. J Antimicrob Chemother. 2017;72(1):29–39. doi:10.1093/jac/dkw377
38. Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America Guidance on the treatment of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infectious Dis. 2021;72(7):1109–1116. doi:10.1093/cid/ciab295
39. Lee CH, Su TY, Ye JJ, et al. Risk factors and clinical significance of bacteremia caused by Pseudomonas aeruginosa resistant only to carbapenems. J Microbiol Immunol Infect. 2017;50(5):677–683. doi:10.1016/j.jmii.2015.06.003
40. Pena C, Suarez C, Gozalo M, et al. Prospective multicenter study of the impact of carbapenem resistance on mortality in Pseudomonas aeruginosa bloodstream infections. Antimicrob Agents Chemother. 2012;56(3):1265–1272. doi:10.1128/AAC.05991-11
41. Lin K-Y, Lauderdale T-L, Wang J-T, Chang S-C. Carbapenem-resistant Pseudomonas aeruginosa in Taiwan: prevalence, risk factors, and impact on outcome of infections. J Microbiol Immunol Infection. 2016;49(1):52–59. doi:10.1016/j.jmii.2014.01.005
42. Jeong SJ, Yoon SS, Bae IK, Jeong SH, Kim JM, Lee K. Risk factors for mortality in patients with bloodstream infections caused by carbapenem-resistant Pseudomonas aeruginosa: clinical impact of bacterial virulence and strains on outcome. Diagn Microbiol Infect Dis. 2014;80(2):130–135. doi:10.1016/j.diagmicrobio.2014.07.003
43. Raman G, Avendano E, Berger S, Menon V. Appropriate initial antibiotic therapy in hospitalized patients with gram-negative infections: systematic review and meta-analysis. BMC Infect Dis. 2015;15:395. doi:10.1186/s12879-015-1123-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
