Back to Journals » International Journal of General Medicine » Volume 16
Risk Factors Analysis for Hemoglobin Decline Caused by Diagnostic Blood Collection in Respiratory Department in North China: A Case-Control Study
Authors Zhu L, Wang Q, Han J, Wang H
Received 25 June 2023
Accepted for publication 29 September 2023
Published 27 October 2023 Volume 2023:16 Pages 4863—4872
DOI https://doi.org/10.2147/IJGM.S427592
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Woon-Man Kung
Lin Zhu, Qiaobei Wang, Jueming Han, Hui Wang
Department of Respiratory Medicine, The Second Hospital, Cheeloo College of Medicine, Shandong University, Jinan City, Shandong Province, People’s Republic of China
Correspondence: Hui Wang, The Second Hospital, Cheeloo College of Medicine, Shandong University, NO. 247, Beiyuan Street, Jinan, Shandong, 250012, People’s Republic of China, Email [email protected]
Purpose: This study aimed to investigate the correlation between hemoglobin decline and diagnostic blood collection in the respiratory department and analyze the decline’s risk factors.
Patients and Methods: A case-control study in the respiratory department of a national tertiary hospital in north China, multivariable logistic regression analysis was used to find the risk factors. Patients excluding other factors affecting hemoglobin other than blood collection in the year 2021 were enrolled and divided into two groups according to the D-value of hemoglobin. The degree of hemoglobin decline caused by diagnostic blood collection between discharge and admission and its risk factors were analyzed.
Results: Among the 530 patients screened in the study, ΔHb (the D-value of hemoglobin between discharge and admission) showed a skewed distribution with an average value of − 4.38± 0.514 g/L. We defined the D-value less than mean-2SD (ΔHb<-5.408) as a significant hemoglobin decline, by which the patients were categorized into two groups. Some variables had apparent differences between the two groups. By multivariable logistic regression analysis on these variables, the independent risk factors for significant hemoglobin decline (ΔHb<-5.408g/L) were revealed: age (OR=1.020, 95% CI 1.008– 1.032, p=0.001), Male gender (OR=1.544, 95% CI 1.011– 2.358, p=0.044), hemoglobin value at admission (OR=1.052, 95% CI 1.039– 1.065, p< 0.001), total blood collection volume (OR=1.021, 95% CI 1.010– 1.032, p< 0.001).
Conclusion: In the respiratory department, older male and more diagnostic blood collection mean higher risks of significant hemoglobin decline. Surprisingly, the lower the hemoglobin value at admission, the lower the risk.
Keywords: respiratory department, diagnostic blood collection, hemoglobin decline, risk factors
Introduction
Iatrogenic anemia refers to anemia caused by the diagnosis and treatment of patients in a medical procedure. Blood collection for testing, invasive diagnosis and treatment techniques, application of drugs and treatments affecting hematopoiesis, and so on, were considered important causes.1–3 From the past to the present, clinicians are more likely to ignore blood loss caused by blood tests than apparent causes such as gastrointestinal bleeding, which aggravated the phenomenon of iatrogenic anemia caused by diagnostic blood collection.4 According to those researches, large amounts of diagnostic blood collection can cause a decrease in hemoglobin in some patients, of which severe cases may get iatrogenic anemia. Anemia can increase the load on the heart, lungs, and other organs and cause problems such as long hospitalization times, high hospitalization costs, increased complications, and poor prognosis.5–10 Although transfusion can be selected to relieve the symptoms of anemia, it has certain risks and threshold limits.11,12 Opposite to the clinicians, patients and their family members often worry that they will suffer iatrogenic anemia from blood collection, resulting in decreased compliance during blood examination. For patients with low compliance, clinicians are more likely to produce defensive blood examinations,13 thereby deepening the contradiction between doctors and patients. Therefore, it is essential to research the risk factors of hemoglobin decline in hospitalized patients caused by diagnostic blood collection, which not only can prevent iatrogenic anemia in patients but also have crucial humanistic value.
Presently, the risk of hemoglobin decline in inpatients caused by diagnostic blood collection is controversial in different medical departments. Some studies have found that some patients are more likely to suffer a decline in hemoglobin from blood collection, such as patients in ICU and pediatric department, patients with renal dysfunction, myocardial infarction, myasthenia gravis, blood purification, burns, or arteriovenous incision, etc.14–23 Moreover, this decline in hemoglobin is significantly associated with prognosis. The reasons may be a large amount of blood collection, low blood volume, other overt blood loss, or hematopoietic insufficiency. However, some studies consider that diagnostic blood collection has a limited impact on hemoglobin decline during hospitalization, compared with non-diagnostic blood loss and delayed erythropoiesis.24–27
In respiratory department, due to the high proportion of critically ill patients and the frequent need to monitor specific hematological parameters, high frequency and large volume of blood collection are common. However, compared with other disciplines, there are few studies on whether diagnostic blood collection causes a significant decline in hemoglobin during hospitalization and which patients are more sensitive to diagnostic blood collection in respiratory department. This study aimed to fill the gap by investigating whether patients in respiratory department appear to have a significant decline in hemoglobin during hospitalization due to diagnostic blood collection and finding the risk factors for this decline by a retrospective approach.
Subjects and Methods
A case-control design was used in this study according to the STROBE case-control reporting guidelines.28 Patients were screened strictly and their characteristics were retrospectively analysed. Our data came from the hospital’s electronic database; therefore, patients were not involved in the design, conduct, and reporting process of our study. But we had closely protected the patients’ information and obtained the consent of the hospital’s ethics committee, and the approval number was KYLL-2022LW131. In order to control the bias caused by retrospective analysis as much as possible, we used unified criteria for data collection and strictly limited the inclusion conditions, at the same time, we conducted hierarchical analysis and multiple regression analysis on the collected data.
Patient and Public Involvement
None of the patients were asked to advise on the interpretation or writing up of the results.
Data Collection
This study retrieved all patients’ information in the respiratory department of a national tertiary hospital in North China from 2021.01.01 to 2021.12.31 from its electronic medical record system, including the patient’s age, gender, height, weight, length of stay, the severity of illness, principal diagnosis, main operation, etc.
The patients were screened who were cured and discharged from the hospital, hospitalized for 7–30 days, without other causes of blood loss such as gastrointestinal bleeding, and had two or more routine blood tests during hospitalization. The patients were excluded who were dead, pregnant, with a hospital stay of fewer than 7 days or more than 30 days, with bleeding or hematologic disease, with thrombotic or embolic disease, with tumor or renal disease, with a history of transfusion or operation during hospitalization, and without reexamination of blood routine before discharge. Then, the included patients’ hemoglobin values at admission and discharge, platelet counts, blood collection volume, and stay length in hospital were recorded. Quantitative variables were expressed as mean ± standard deviation, and qualitative variables were expressed as percentages. The main observation index was the D-value between admission hemoglobin and hemoglobin in the last routine blood test before discharge (ΔHb=Hb(discharge)-Hb(admission)).
Definitions and Statistical Methods
The Laboratory Center of the hospital is the chairman-designate unit of the Laboratory Medicine Branch of the Chinese Medical Association and has passed ISO15189 certification. According to its rules, the amount of blood collection should be guaranteed for one test and two retests. The minimum blood volume required for each test is 3mL for complete blood count, 3mL for all coagulation tests, 5mL for all biochemical tests, 5mL for all immunological tests, 5mL for molecular biology tests, 20mL for blood culture, and 1mL for blood gas. The total blood collection volume was estimated by combining the minimum volume with the number of blood collection tubes.
According to the value of ΔHb, all included patients were divided into group 1 and group 2, then Chi-square test and Mann–Whitney U-test were carried out for each variable between the two groups. The information such as age, gender, height, weight, total blood collection, blood collection interval, hemoglobin at admission, diagnosis, and operation was compared to explore the statistically significant differences. And then, multi-variables logistic regression analysis was performed on variables with apparent differences. All statistical analyses were performed in Microsoft Excel and SPSS version 26. P-values below 0.05 were considered statistically significant.
Results
The results showed that from January 1, 2021, to December 31, 2021, a total of 3043 patients were hospitalized in this department. Among them, 1369 patients were excluded for being died, or hospitalized for less than 7 days or more than 30 days. Among the remaining 1674 patients, 780 were excluded for bleeding, having a transfusion, undergoing surgery, or suffering from diseases like tumor, hematological, thrombotic, embolic, or renal disease that significantly affected the hemoglobin value. For the remaining 894 patients, the basic information such as hemoglobin value at admission and discharge, age, gender, weight, height, and blood collection volume were counted, and 364 patients without reexamination of blood routine before discharge were excluded. Finally, 530 patients were included in the study. (Figure 1)
 |
Figure 1 The process of data collection, screening, grouping, and analysis. |
For these 530 patients, the D-value of hemoglobin between admission and discharge named ΔHb (Hb(discharge)-Hb(admission)) was analysed by normality test. The results showed that the mean value of ΔHb was −4.38g/L, and the SD was 0.514 g/L, the distribution of ΔHb was skewed. We defined the D-value less than mean-2SD (ΔHb<-5.408) as a significant hemoglobin decline, by which all patients were categorized into two groups: the significant hemoglobin decline group as group 1 (ΔHb<-5.408g/L) and the non-significantly hemoglobin decline group as group 2 (ΔHb>-5.408g/L). The basic information of the patients in these two groups was analysed by Chi-square test and Mann–Whitney U-test. And the results showed that the differences between the two groups in the following aspects were statistically significant, the volume of blood collection (67.53±26.977mL in group 1, 57.4±19.169mL in group 2, p<0.001), Length of stay (9.96±3.755 days in group 1, 8.55±2.986 days in group 2, p<0.001), hemoglobin value at admission (139.07±19.586/L in group 1, 125.33±17.822g/L in group 2, p<0.001), platelet value at discharge (238.23±90.509*109/L in group 1, 256.25±94.166*109/L in group 2, p=0.029), the difference of platelet between discharge and admission named ΔPlt (2.02±81.485*109/L in group 1, 18.2±67.153*109/L in group 2, p=0.003). Besides these, there were some apparent differences between the two groups (p<0.1), age (66.34±16.443 in group 1, 63.06±18.774 in group 2, p=0.093), Male (62.4% in group 1, 54.7% in group 2, p=0.076) pleural effusion as principal diagnosis (6.0% in group 1, 10.5% in group 2, p=0.066), and using a non-invasive ventilator during hospitalization (6.4% in group 1, 11.1% in group 2, p=0.059). The difference of other characteristics were not apparent such as age, gender, height, weight, other diagnosis and operation (Table 1).
 |
Table 1 Baseline Characteristics and Data of the Patients |
To further explore the independent risk factors for significant hemoglobin decline, the above variables whose p<0.1, were analysed by multi-variables logistic regression. In the model likelihood ratio test, the P value was less than 0.001, illustrating that the results are generally meaningful. Moreover, in the H-L test, the P value was more than 0.05, illustrating that the model’s goodness-of-fit is good. The results showed that the following variables were independent risk factors for the occurrence of significant hemoglobin decline (ΔHB<-5.408g/L) during hospitalization: age (OR=1.020, 95% CI 1.007–1.032, p=0.001), Male gender (OR 1.544, 95% CI 1.011–2.358, p=0.044), hemoglobin value at admission (OR=1.052, 95% CI 1.039–1.065, p<0.001), blood collection volume (OR=1.021, 95% CI 1.010–1.032, p<0.001), (Table 2). The results showed that the older age, male gender, higher Hb level at admission, and more blood collection volume are factors that increase the risk of Hb value significant reduction by 1.02, 1.544, 1.052, and 1.021 times, respectively.
 |
Table 2 Multivariable Logistic Analysis to Determine Risk Factors of Δhb |
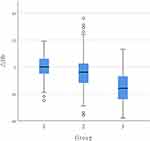
In this study, a higher hemoglobin value at admission means higher risk of a significant decline in hemoglobin. To further explore the reason, we grouped these 530 patients into three groups according to the hemoglobin value at admission. Group 1 contained patients with anemia at admission; group 2 contained patients with normal hemoglobin at admission, and group 3 contained patients with higher hemoglobin values than usual at admission. Because the patients we included were all from North China, so the average hemoglobin range adopted the consensus of Chinese experts that adult males are 120–160 g/L, and adult females (non-pregnant) are 110–150 g/L in the sea level area.29
Kruskal–Wallis’ rank-sum test was performed on the data of ΔHb, blood collection volume, age, gender, and ΔPlt of the three groups. And it was found that there was a significant difference in ΔHb among the three groups (Figure 2), group 1 was −0.16±9.417g/L, group 2 was −4.14±11.457g/L, group 3 was −15.93±12.662g/L, the difference was statistically significant (p<0.001), And the difference in ΔPlt among the three groups was also statistically significant, group 1 was 16.30±77.852*109/L, group 2 was 12.33±73.958*109/L, group 3 was −11.56±64.698*109/L, p=0.036. At the same time, the difference in age and gender among the three groups was also statistically significant (p=0.001). However, this difference could not exceed the influence of basal hemoglobin, and the differences in blood collection volume and among the three groups were not statistically significant (Table 3).
 |
Table 3 All Patients Were Grouped into Three Groups According to Hb at Admission, to Compare the Difference of Age, Gender, Blood Collection Volum, Δhb, Δplt Among the Three Groups |
Discussion
The data showed that a decline in hemoglobin value during hospitalization is widespread in the respiratory department. The hemoglobin value of 62.45% patients was decreased at discharge. Considering that there is no uniform standard for significant hemoglobin decline yet, we defined ΔHb<-5.408 (mean-2SD) as a significant hemoglobin decline. Through statistical analysis, it was found that the independent risk factors for significant hemoglobin decline were age, blood collection volume, gender, and hemoglobin value at admission. The first two are consistent with other studies that older age and more blood collection are associated with a higher risk of significant hemoglobin decline.17,18,21,23,30 About the latter two, there has no relevant research before, which is an exciting aspect of this study.
The result showed that the higher the hemoglobin value was at admission, the higher the risk of significant hemoglobin decline, and male had more risk than female. To further explore the reason, we grouped the patients into three groups, group 1 referred to patients with anemia at admission, group 2 referred to patients with normal hemoglobin values at admission, and group 3 referred to patients with high hemoglobin values. Further exploration found that patients in group 1 had the least significant decrease in hemoglobin, while the most increase in platelet, and vice versa in group 3. Meanwhile, the proportion of males was the highest in group 3. Combining these data sets, we speculated that the compensatory hematopoiesis caused by blood loss is the strongest in group 1 and the weakest in group 3, and at the same time, the phenomenon is also related to gender. Speculating about the reason, it may be that the patients in group 1 have been in a state of anemia for a long time. In order to meet the regular blood and oxygen need, the compensatory hematopoiesis is in hyperactivity. While in the patients in group 3, due to the excess hemoglobin, moderate blood collection was not enough to affect the blood supply of the body, so the compensatory hematopoietic capacity is low. To confirm this speculation, large-scale RCT studies are still needed for further validation. And reticulocyte values, Reticulocyte Production Index(RPI), and Immature Reticulocyte Fraction(IRF) will be counted in order to accurately measurements of hematopoiesis.
Although the association between hospital-acquired anemia and diagnostic blood collection has been studied in several disciplines, it has no precedent in the respiratory department. This study explored firstly whether inpatients in respiratory department would suffer from iatrogenic hemoglobin reduction due to blood examinations in the daily clinical process after excluding other factors. Furthermore, the patients more susceptible to hematological examinations were also found in this study. This study has several limitations. This study is retrospective, and the data came from one medical institution only. The sample size is not large enough in some conditions. Although the blood collection volume was calculated as accurately as possible, there was a slight waste of blood filling other venous access, and occasionally dilutional confounding factors such as intravenous fluids, which may lead to a bit of bias in blood collection volume.
Compared with other studies, the total blood collection volume and hemoglobin changes of the patients in this study were generally similar to the results in general internal medicine and relatively less than those in ICU, cardiovascular medicine, nephrology, trauma, and other fields.30–33 It is because the patients included in the study had a relatively lower proportion of critical disease and suffered less intensive hematological monitoring compared with those in ICU. At the same time, compared with other departments above, factors such as hemorrhage, transfusion, hematophagy, and other pathophysiological states affecting hematopoiesis were excluded during screening patients, and our patients had fewer invasive operations, fewer antithrombotic and antiplatelet drugs. The main intervention for hemoglobin changes during hospitalization in this study was only blood collection. The differences in hemoglobin value are the performance of the interaction from diagnostic blood collection and the compensatory ability to blood loss.
Our study demonstrated that older age and more blood collection are associated with a higher risk of significant hemoglobin decline. However, the total amount of blood collection required for daily diagnosis in the respiratory department is much less than that in ICU usually. Furthermore, due to the influence of patients’ hematopoietic compensation, this level of blood collection volume will not cause additional severe damage to the patients, which can reduce the resistance of patients and their families to blood examination. In spite of this, it is necessary to optimize blood collection as much as possible in clinical work to avoid excessive blood waste. Studies have found that most laboratories can reduce blood collection volume without affecting test results.34,35 In order to reduce the amount of blood collection, many studies have done related work and put forward some measures. For example, optimizing orders and systems for blood collection or using pediatric blood collection tubes in adults can reduce blood collection volume while meeting clinical diagnostic needs.36–42 This study found an interesting relevance among hemoglobin decline and gender and hemoglobin value at admission, which need to be further explored by large-scale RCT studies in the future.
Conclusion
In conclusion, this study found that the independent risk factors for hemoglobin decline during hospitalization in respiratory department were: age, gender, hemoglobin value at admission, and total blood collection volume. Therefore, in clinical work, blood collection should be optimized as much as possible for elderly patients to reduce the impact of blood collection on hemoglobin. In our study, it was demonstrated that older age and more blood collection are associated with a higher risk of significant hemoglobin decline. However, the total amount of blood collection required for daily diagnosis in the respiratory department is much less than that in ICU usually.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics and Consent Statements
The study protocol was submitted and approved by the Research Ethics Committee of the Second Hospital of Shandong University, and the approval number is KYLL-2022LW131. The data were collected by trained staff from the hospital’s electronic database. Data confidentiality was guaranteed by creating a password-protected database for exclusive access to research staff. This manuscript confirms it complies with the Declaration of Helsinki. The participants were fully informed about the purpose of the study and written/verbal informed consent has been obtained from them to publish this paper.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Burnum J. Medical vampires. N Engl J Med. 1986;314(19):1250–1251. doi:10.1056/nejm198605083141910
2. Foulke GE, Harlow DJ. Effective measures for reducing blood loss from diagnostic laboratory tests in intensive care unit patients. Crit Care Med. 1989;17(11):1143–1145. doi:10.1097/00003246-198911000-00008
3. Shander A, Corwin HL. A narrative review on hospital-acquired anemia: keeping blood where it belongs. Transfus Med Rev. 2020;34(3):195–199. doi:10.1016/j.tmrv.2020.03.003
4. Rosenzweig A. Iatrogenic anemia. Arch Intern Med. 1978;138(12):1843. doi:10.1001/archinte.138.12.1843
5. Dech ZF, Szaflarski NL. Nursing strategies to minimize blood loss associated with phlebotomy. AACN Clin Issues. 1996;7(2):277–287. doi:10.1097/00044067-199605000-00010
6. Fowler A, Ahmad T, Phull M, Allard S, Gillies M, Pearse R. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102(11):1314–1324. doi:10.1002/bjs.9861
7. Lasocki S, Krause R, von Heymann C, Mezzacasa A, Chainey S, Spahn D. PREPARE: the prevalence of perioperative anaemia and need for patient blood management in elective orthopedic surgery: a multicentre, observational study. Eur J Anaesthesiol. 2015;32(3):160–167. doi:10.1097/eja.0000000000000202
8. Sato T, Yamauchi H, Kanno Y, et al. Comparisons of prognostic factors between young and elderly patients with chronic heart failure. Geriatr Gerontol Int. 2015;15(4):435–442. doi:10.1111/ggi.12293
9. Wang MP, Jiang L, Zhu B, Jiang Q, Xi XM. 机械通气患者贫血的临床观察研究 [Clinical observational study of anemia in mechanically ventilated patients]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2012;24(2):70–73. Chinese.
10. Yanishi K, Nakamura T, Nakanishi N, et al. A simple risk stratification model for ST-Elevation Myocardial Infarction (STEMI) from the combination of blood examination variables: Acute Myocardial Infarction-Kyoto Multi-Center Risk Study Group. PLoS One. 2016;11(11):e0166391. doi:10.1371/journal.pone.0166391
11. Cable C, Razavi S, Roback J, Murphy D. RBC transfusion strategies in the ICU: a concise review. Crit Care Med. 2019;47(11):1637–1644. doi:10.1097/ccm.0000000000003985
12. Walker R. Special report: transfusion risks. Am J Clin Pathol. 1987;88(3):374–378. doi:10.1093/ajcp/88.3.374
13. Katz E. Defensive medicine: a case and review of its status and possible solutions. Clin Pract Cases Emerg Med. 2019;3(4):329–332. doi:10.5811/cpcem.2019.9.43975
14. Jakacka N, Snarski E, Mekuria S. Prevention of iatrogenic anemia in critical and neonatal care. Adv Clin Exp Med. 2016;25(1):191–197. doi:10.17219/acem/32065
15. Bateman ST, Lacroix J, Boven K, et al. Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. Am J Respir Crit Care Med. 2008;178(1):26–33. doi:10.1164/rccm.200711-1637OC
16. Pabla L, Watkins E, Doughty H. A study of blood loss from phlebotomy in renal medical inpatients. Transfus Med. 2009;19(6):309–314. doi:10.1111/j.1365-3148.2009.00960.x
17. Choi JS, Kim YA, Kang YU, et al. Clinical impact of hospital-acquired anemia in association with acute kidney injury and chronic kidney disease in patients with acute myocardial infarction. PLoS One. 2013;8(9):e75583. doi:10.1371/journal.pone.0075583
18. Salisbury AC, Alexander KP, Reid KJ, et al. Incidence, correlates, and outcomes of acute, hospital-acquired anemia in patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3(4):337–346. doi:10.1161/circoutcomes.110.957050
19. Salisbury AC, Amin AP, Reid KJ, et al. Red blood cell indices and development of hospital-acquired anemia during acute myocardial infarction. Am J Cardiol. 2012;109(8):1104–1110. doi:10.1016/j.amjcard.2011.11.045
20. Salisbury AC, Kosiborod M. Hospital-acquired anemia in patients with cardiovascular disease: incidence, outcomes, and opportunities for prevention. Rev Cardiovasc Med. 2012;13(4):e150–60. doi:10.3909/ricm0614
21. Mann SA, Williams LA, Marques MB, Pham HP. Hospital-acquired anemia due to diagnostic and therapy-related blood loss in inpatients with myasthenia gravis receiving therapeutic plasma exchange. J Clin Apher. 2018;33(1):14–20. doi:10.1002/jca.21554
22. Stucchi M, Cantoni S, Piccinelli E, Savonitto S, Morici N. Anemia and acute coronary syndrome: current perspectives. Vasc Health Risk Manag. 2018;14:109–118. doi:10.2147/vhrm.S140951
23. Yao RQ, Wu GS, Xu L, et al. Diagnostic blood loss from phlebotomy and hospital acquired anemia in patients with severe burns. Burns. 2020;46(3):579–588. doi:10.1016/j.burns.2019.08.020
24. van der Bom JG, Cannegieter SC. Hospital-acquired anemia: the contribution of diagnostic blood loss. J Thromb Haemost. 2015;13(6):1157–1159. doi:10.1111/jth.12886
25. von Ahsen N, Müller C, Serke S, Frei U, Eckardt KU. Important role of non-diagnostic blood loss and blunted erythropoietic response in the anemia of medical intensive care patients. CritCareMed. 1999;27(1999):2630–2639.
26. Zhou D, Luo YL, Luo SH, Feng M, Tang ML. The effect of diagnostic blood loss on anemia and transfusion among postoperative patients with congenital heart disease in a pediatric intensive care unit. J Pediatr Nurs. 2018;38:62–67. doi:10.1016/j.pedn.2017.09.007
27. Branco B, Inaba K, Doughty R, et al. The increasing burden of phlebotomy in the development of anaemia and need for blood transfusion amongst trauma patients. Injury. 2012;43(1):78–83. doi:10.1016/j.injury.2010.12.003
28. von Elm EAD, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–804. doi:10.1097/EDE.0b013e3181577654
29. Haozhu Chen GL, Wang J, Pan X, et al. Practice of Internal Medicine.
30. Thavendiranathan P, Bagai A, Ebidia A, Detsky A, Choudhry N. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20(6):520–524. doi:10.1111/j.1525-1497.2005.0094.x
31. Smoller B, Kruskall M. Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N Engl J Med. 1986;314(19):1233–1235. doi:10.1056/nejm198605083141906
32. Tosiri P, Kanitsap N, Kanitsap A. Approximate iatrogenic blood loss in medical intensive care patients and the causes of anemia. J Med AssocThailand. 2010;93 Suppl 7:S271–6.
33. Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171(18):1646–1653. doi:10.1001/archinternmed.2011.361
34. Dale J, Ruby S. Specimen collection volumes for laboratory tests. Arch Pathol Lab Med. 2003;127(2):162–168. doi:10.5858/2003-127-162-scvfl
35. Valentine SL, Bateman ST. Identifying factors to minimize phlebotomy-induced blood loss in the pediatric intensive care unit. Pediatr Crit Care Med. 2012;13(1):22–27. doi:10.1097/PCC.0b013e318219681d
36. Dolman HS, Evans K, Zimmerman LH, et al. Impact of minimizing diagnostic blood loss in the critically ill. Surgery. 2015;158(4):1083–7; discussion 1087–8. doi:10.1016/j.surg.2015.05.018
37. Pasqualetti S, Aloisio E, Birindelli S, Dolci A, Panteghini M. Impact of total automation consolidating first-line laboratory tests on diagnostic blood loss. Clin Chem Lab Med. 2019;57(11):1721–1729. doi:10.1515/cclm-2019-0133
38. Riessen R, Behmenburg M, Blumenstock G, et al. A simple “Blood-Saving Bundle” reduces diagnostic blood loss and the transfusion rate in mechanically ventilated patients. PLoS One. 2015;10(9):e0138879. doi:10.1371/journal.pone.0138879
39. Smoller BR, Kruskall MS, Horowitz GL. Reducing adult phlebotomy blood loss with the use of pediatric-sized blood collection tubes. Am J Clin Pathol. 1989;91(6):701–703. doi:10.1093/ajcp/91.6.701
40. Tinmouth A, McIntyre L, Fowler R. Blood conservation strategies to reduce the need for red blood cell transfusion in critically ill patients. Can Med Assoc J. 2008;178(1):49–57. doi:10.1503/cmaj.071298
41. Wu Y, Spaulding AC, Borkar S, et al. Reducing blood loss by changing to small volume tubes for laboratory testing. Mayo Clin Proc Innov Qual Outcomes. 2021;5(1):72–83. doi:10.1016/j.mayocpiqo.2020.08.007
42. Lyon AW, Chin AC, Slotsve GA, Lyon ME. Simulation of repetitive diagnostic blood loss and onset of iatrogenic anemia in critical care patients with a mathematical model. Comput Biol Med. 2013;43(2):84–90. doi:10.1016/j.compbiomed.2012.11.008
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.