Back to Journals » International Journal of General Medicine » Volume 16
Risk Factor Analysis and Intervention Study for Unspecific Functional Enteropathy in a Maritime Environment: A Cross-Sectional Analytical Survey
Authors Zhang C, Yang Z, Xie W, Li C, Huang X
Received 31 May 2023
Accepted for publication 22 September 2023
Published 20 October 2023 Volume 2023:16 Pages 4757—4763
DOI https://doi.org/10.2147/IJGM.S423773
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Luca Testarelli
Chunyan Zhang, Zhijian Yang, Wenxiu Xie, Congyong Li, Xuefei Huang
Sixth Health Care Department, Second Medical Center of PLA General Hospital, Beijing, 100853, People’s Republic of China
Correspondence: Chunyan Zhang, Sixth Health Care Department, Second Medical Center of PLA General Hospital, No. 28 Fuxing Road, Haidian District, Beijing, 100853, People’s Republic of China, Tel +86 01066957818, Email [email protected]
Background: The study aimed to investigate the risk factors and interventions for unspecific functional bowel disorders (U-FBDs) in military personnel under maritime environment.
Methods: This cross-sectional analytical survey used the Rome III questionnaire for surveying 1018 military personnel involved in overseas humanitarian medical services from June 2013 to January 2016. Individuals diagnosed with U-FBDs were included in the U-FBDs group, while those without FBDs or other diseases were considered the control group. The psychological and sleep conditions of military personnel with U-FBDs were assessed using the SCL-90 scale and the Pittsburgh Sleep Quality Index scale, respectively. Health education and treatment were provided to individuals diagnosed with U-FBDs, and the improvements were evaluated after three months.
Results: Among 923 qualified questionnaires, 243 subjects was included in U-FBDs group and 240 in the control group. Smoking, alcohol consumption, and multiple seafaring missions were identified as risk factors for U-FBDs in military personnel on ocean-going missions. The U-FBDs group had significantly worse sleep quality, sleep efficiency, daytime dysfunction score, and total PSQI score compared to the control group (P < 0.05). Additionally, 10 factor scores of SCL-90 and the total score in the U-FBDs group were significantly higher than those in the control group (P < 0.01). Patients with U-FBDs also reported the highest rate of somatic symptoms (P < 0.01).
Conclusion: The onset of U-FBDs among military personnel on long-haul maritime may be closely related to mental, psychological, and sleep factors. Health education and treatment may help improve the symptoms of U-FBDs.
Keywords: military, maritime environment, non-specific functional enteropathy, functional enteropathy
Introduction
Functional bowel disorders (FBDs) are a class of chronic gastrointestinal illnesses.1,2 According to Rome III criteria, irritable bowel syndrome (IBS), functional diarrhoea (FDR), functional constipation (FC), functional abdominal bloating/distension (FAB/DA), and unspecified functional bowel disorders (U-FBDs) are the five categories of FBDs.3 Those with intestinal symptoms that do not meet the diagnostic criteria of IBS, FDR, FC, or FAB/DA are classified as U-FBDs.4 Some studies have shown that U-FBDs are among the most prevalent FBDs.5,6 U-FBDs are a group of disorders that are characterized by chronic or recurrent gastrointestinal symptoms such as abdominal pain, bloating, constipation, and diarrhea, without any identifiable organic or structural abnormalities. Smoking and alcohol consumption are associated with an increased risk of U-FBDs.5 In addition, multiple seafaring missions have been identified as a risk factor for developing functional gastrointestinal disorders, including IBS, due to the stressful and challenging work environment, as well as the dietary and lifestyle factors that are often associated with seafaring work.7
A meta-analysis revealed that FBD patients had greater levels of anxiety and sadness than healthy controls.8 Inadequate sleep and/or circadian misalignment frequently contribute to the major mental and physical derangements brought on by deteriorated metabolic, cardiovascular, skeletomuscular, and cognitive health.9,10 Environmental stressors like fear and anger have an impact on a person’s cognition and mood. They also alter gastrointestinal motility by controlling the production of the hormone corticotrophin through the autonomic nervous system.11,12 Mucosal microinflammation is one of the mechanisms that can cause numerous gastrointestinal symptoms, along with alterations in the gastrointestinal motility.13
Over the past few years, China has been expanding its international humanitarian medical services, including regular long-distance ocean voyages.14 Compared to previous short-term training near the coast, these voyages increase the work intensity, physical demands, and psychological stress on crew members, making them more susceptible to functional gastrointestinal disorders (FGIDs) such as unexplained functional bowel disorders (U-FBDs).15
U-FBDs are one of the most common illnesses among military personnel, but the psychological and sleep profiles of U-FBDs and FGIDs in military person in military maritime environments have rarely been reported. Therefore, this study aims to identify risk factors for U-FBDs among military personnel on long-distance voyages and develop intervention measures to reduce their symptoms during these journeys.
Information and Methods
Study Population
This cross-sectional study was performed with the approval by the institutional ethical committee of Second Medical Center of PLA General Hospital. Written informed consent was obtained from each participant for the study. All methods were carried out in accordance with relevant guidelines and regulations, and in compliance with the Declaration of Helsinki.
The 1018 cases of mission military person who performed the Harmony Mission on the Peace Ark hospital ship from June 2013 to January 2016 were included and completed the survey, with 631 cases of male and 387 cases of female; age 18–43 years old and 1.5–18 years of military service.
Diagnosis and Intervention Methods
The Rome III questionnaire (consisting of 105 items in 19 categories) issued by the Rome Committee of the FGIDs was used to design the questionnaire, taking into account the general conditions of the respondents. The diagnostic criteria were strictly in accordance with the Rome III criteria of FGIDs, and the classification and diagnosis were based on the answers to the questionnaire filled in by the respondents. Based on the survey obtained from 923 subjects, we diagnosed 243 U-FBDs patients and they were used as the study group. The inclusion criteria for U-FBDs were: recurrent or chronic gastrointestinal symptoms including diarrhea, constipation, bloating, and abdominal discomfort without any apparent organic or structural abnormalities. Irritable bowel syndrome (IBS), functional diarrhea, and functional constipation are some of these conditions. The control group (n=240) was healthy military person without U-FBDs and other diseases. The rest subject who did not meet the above criteria were excluded. All the studied subjects were free from metabolic diseases and organic lesions of the digestive tract. The rest subject (n=440) who did not met the above criteria were excluded.
Evaluation Method of Psychological Factors
The SCL-90 scale, which has 90 items and is divided into 10 factors—somatization, obsession, interpersonal relationship, depression, anxiety, hostility, terror, paranoia, psychoticism, and others—was used to measure psychological factors. Each item was scored on a scale from none to very heavy on a 1–5 scale.
Data Entry
Uniform explanation and instruction by two gastroenterologists specializing in functional gastroenterology when questionnaires are distributed.16 The questionnaires are collected and checked blindly by trained personnel, and unqualified questionnaires are eliminated according to quality control. The data were proofread and entered by two people blindly while consistency testing and error correction were performed.
Statistical Analysis
Data analysis was processed using SPSS18.0 statistical software. The scores of each factor of the PSQI scale were non-normally distributed measurement data, expressed as the median (interquartile range) [M (P25, P75)], and the non-parametric Mann–Whitney U-test was used between groups; The measurement data that meet the normal distribution were expressed as mean±standard deviation ( ) and rates, and the χ2 test was used for comparisons between independent sample groups; The paired χ2 test (McNemar’s test) was used for comparisons of the prevalence of FBDs before and after intervention. Logistic regression analysis was used to analyze related factors. P<0.05 was considered statistically significant.
) and rates, and the χ2 test was used for comparisons between independent sample groups; The paired χ2 test (McNemar’s test) was used for comparisons of the prevalence of FBDs before and after intervention. Logistic regression analysis was used to analyze related factors. P<0.05 was considered statistically significant.
Results
Onset of FBDs, Including U-FBD, and Interventions for Task Military Person in Military Maritime Environments
The epidemiological survey was conducted by applying FGIDs Rome III questionnaire to 1018 mission military person before the voyage, and 923 valid questionnaires were returned. The results showed that out of 923 subjects, there were 450 cases of FGIDs with a total prevalence of 48.75% (450/923); 353 cases of FBDs with a prevalence of 38.24% (353/923); 53 cases of IBS (5.74%, 53/923); 45 cases of FAB (4.87%, 45/923); 10 cases of FC (1.08%, 10/923); 2 cases of FDR (0.22%, 2/923); 243 cases of U-FBD (26.33%, 243/923); 5 cases of IBS+FC (0.54%, 5/923); 2 cases of FAB+FDR (0.22%, 2/923); FAB+FDR 2 cases (0.22%, 2/923); FAB+FC 3 cases (0.33%, 3/923). Various functional gastrointestinal disorders have some overlaps among the whole population. There were 240 (26%, 240/923) cases without functional gastrointestinal disease and other diseases, who were chosen as control group. Through systematic health education and appropriate adjuvant medication, the symptoms of FBDs were significantly relieved by the reexamination in March, and the remission rate of the original patients’ symptoms disappeared reached 59.21%. A total of 209 cases with FBDs had fewer episodes and their symptoms disappeared or remitted after intervention, including 33 cases of IBS, 25 cases of FAB (55.00%), 4 cases of FC (40%), 1 case of FDR (50%), and 146 cases of U-FBD (60.08%). There was a significant difference in the incidence of each FBDs before and after the voyage (P < 0.05), as shown in Table 1.
 |
Table 1 The Prevalence of Functional Enteropathy Before and After the Voyage of Military Person of the Long Voyage |
Comparison of Clinical Characteristics of Military Personnel with U-FBDs Performing Seafaring Duties and Healthy Controls
The U-FBDs group consisted of 243 military personnel diagnosed with U-FBDs, with a mean age of 26.3 ± 3.1 years and military service of 3.7 ± 3.3 years. The control group included 240 military personnel without FGIDs and other diseases, with a mean age of 27.3 ± 3.5 years and military service of 3.6 ± 2.8 years. There were no significant differences in age, military service, and marital status between the two groups (P > 0.05). In the U-FBDs group, 63 individuals (25.92%) reported smoking, and 125 individuals (51.4%) reported alcohol consumption, while in the control group, 35 individuals (14.4%) reported smoking and 82 individuals (34.16%) reported alcohol consumption, with significant differences between the two groups (P < 0.05). The U-FBDs group had a higher number of ocean-going missions (4.15 ± 2.51) compared to the control group (2.27 ± 1.34), with a significant difference between the two groups (P < 0.01).
Comparison of Sleep Status Between U-FBDs and Healthy Controls
Compared to the control group, the U-FBDs group had significantly poorer sleep quality, sleep efficiency, longer sleep latency, and more sleep disturbances (P < 0.01). The daytime dysfunction score and total PSQI score were also significantly higher in the U-FBDs group than in the control group (P < 0.05) (Table 2).
 |
Table 2 Comparison of Sleep Status Between Non-Specific Functional Enteropathy and Healthy Controls |
Comparison of SCL-90 Scores Between Military Personnel with U-FBDs and Healthy Controls
The SCL-90 scale scores for the U-FBDs group were significantly higher than those for the control group, with statistical differences observed in all 10 factors and the total score (P < 0.01) (Table 3). The U-FBDs group reported the highest rate of somatic symptoms (P < 0.01), as well as higher levels of obsessive-compulsive, interpersonal, and anxiety symptoms (all P < 0.01).
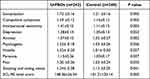 |
Table 3 Comparison of SCL-90 Scores Between U-FBDs and Control Group |
Discussions
Our study revealed that U-FBDs had a significantly higher prevalence of 26.33% in military personnel deployed in a long-distance environment compared to other FBDs. This finding is consistent with previous studies, including one conducted by Yao Xin, which reported a 25.74% prevalence of U-FBDs among military personnel serving in the central war zone.17 Additionally, a multicenter study in Japan found that U-FBDs accounted for 15.9% of functional bowel diseases.18 While U-FBD diagnosis is relatively stable, it remains poorly understood and requires further investigation into its pathogenesis.
Our study also found that military personnel with U-FBDs experienced sleep abnormalities, with 32.4% experiencing suspected insomnia and 33.8% experiencing sleep disorders. Military personnel with U-FBDs had significantly poorer sleep quality, longer sleep times, more sleep disturbances, higher daytime dysfunction scores, and higher total PSQI scores than the control group, which is consistent with the results by Ballou et al.19 Chronic sleep deprivation can have a negative effect on how well the body works and how well people perform at work because sleep is so important for both physical and psychological health. Thus, it is crucial to improve psychological health and alleviate fatigue to enhance sleep quality in military personnel with U-FBDs.
The study revealed that mental health level (SCL-90 total score) had the greatest impact on sleep quality. Pilots who experienced anxiety, nervousness, irritability, and depression had significantly poorer sleep quality, and those with poor sleep quality had significantly poorer responsiveness and short-term memory.20 The prevalence of anxiety/depression at the end of long voyages was 28.42%, which suggests that long voyages can lead to significantly high prevalence of anxiety/depression. A recent report finds that U-FBDs had high scores on measures of depression, anxiety, and sleep disturbances.19 This study found that the 10-factor SCL-90 scores and total scores of the U-FBDs group were significantly higher than those of the control group, which indicates that U-FBDs are closely related to mental and psychological factors such as anxiety, depression, interpersonal sensitivity, and somatization. Compared to other FBDs, patients with U-FBDs reported the highest rate of somatic symptoms, and they also had higher levels of obsessive-compulsive, interpersonal, and anxiety symptoms.
A patho-mechanism through the gut-brain axis is implied by the accumulating evidence of altered gut microbiota in autism spectrum disorder (ASD), notwithstanding the inconsistent microbiome profiles reported across investigations. One of the information gaps in the existing ASD microbiota studies is the lack of a detailed analysis of the involvement of FGID in the relationship between ASD and altered gut microbiome.21 The typically developing(TD) groups were split apart from the ASD FGID+ and ASD FGID microbiota. ASD FGID+ differed from ASD FGID in terms of quality and also had the highest Firmicutes: Bacteroidetes ratio, which was associated with higher levels of anxiety and overall psychopathology. Concomitant FGID appeared to have no connection to ASD’s altered gut microbiome.21 The patho-mechanism and effect of psychological factors on U-FBDs still need further explorations.
In recent years, the Internet of Things technology (IoT) has developed rapidly and is widely used in the medical field. The IoT is based on the combination of wireless sensors, computer technology and network facilities. Some scholars have proposed that IoT devices can replace gastrointestinal endoscopy, and the application of intelligent ingestible sensors (pills) is activated by being swallowed, “moves” in the body through the colon, and sends Gastric and colonic data to computers and smartphones.22 For patients who are not suitable for gastrointestinal endoscopy, we can transmit patient data (including symptoms, stool characteristics, sleep, diet, treatment, etc.) to doctors, and doctors can provide accurate evaluations and treatments vie IoT.22
During the long voyage, the health prevention and treatments for U-FBDs mainly include lifestyle adjustments, dietary advice, stress-relieving psychotherapy, dietary supplement guidance, drugs and acupuncture treatment. Although no patients with severe constipation were found in the population we studied, patients with slow transit constipation who were ineffective to nonsurgical treatment and who had significant abnormalities on specific examination for constipation may also be considered for surgery if they meet the indications for surgery.23
These findings should have significant clinical implications for improving the effectiveness of ocean rescue capabilities, reducing non-war attrition, enhancing the ability of long-distance voyagers to perform their tasks, and increasing security and safety during actual disaster and humanitarian medical relief operations. However, the study’s main flaws include its small sample size and the fact that it was carried out in a single military unit, which may limit the findings’ applicability to other military units or civilian populations. Additionally, the study relied on self-report measures for the diagnosis of U-FBDs, which may be subject to recall bias and may not accurately reflect the actual prevalence of the disorder. The cross-sectional design of the study also makes it difficult to establish causal relationships between U-FBDs and the factors examined, and longitudinal studies may be needed to confirm the findings. Finally, the study did not investigate the impact of U-FBDs on work performance or other aspects of daily life, which may be important to consider in future research.
Conclusion
Our study indicates that U-FBDs are highly prevalent among military personnel serving in long-distance environments. Additionally, our findings demonstrate that U-FBDs are closely associated with psychiatric, psychological, and sleep factors, as evidenced by significantly higher SCL-90 and PSQI scores in U-FBD patients. Furthermore, patients with U-FBDs are more likely to experience somatic symptoms and have poor interpersonal relationships and anxiety. Thus, further research on the pathogenesis of U-FBDs is necessary to inform effective clinical prevention and treatment strategies for this condition.
Data Sharing Statement
All data analyzed during this study are included in this published article.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Wang Y, Chen Y, Zhang X, Lu Y, Chen H. New insights in intestinal oxidative stress damage and the health intervention effects of nutrients: a review. J Functional Foods. 2020;75:104248. doi:10.1016/j.jff.2020.104248
2. Tang WH, Li DY, Hazen SL. Dietary metabolism, the gut microbiome, and heart failure. Nat Rev Cardiol. 2019;16(3):137–154. doi:10.1038/s41569-018-0108-7
3. Wells JM, Gao Y, de Groot N, Vonk MM, Ulfman L, van Neerven RJ. Babies, bug, and barriers: dietary modulation of intestinal barrier function in early life. Annu Rev Nutr. 2022;2022:42.
4. Ou W, Yu G, Zhang Y, Mai K. Recent progress in the understanding of the gut microbiota of marine fishes. Marine Life Sci Technol. 2021;3(4):434–448. doi:10.1007/s42995-021-00094-y
5. Singh S, Dulai PS. Ulcerative colitis: clinical manifestations and management. Yamada’s Textbook Gastroenterol. 2022;2022:1248–1293.
6. Saettone V, Biasato I, Radice E, Schiavone A, Bergero D, Meineri G. State-of-the-art of the nutritional alternatives to the use of antibiotics in humans and monogastric animals. Animals. 2020;10(12):2199. doi:10.3390/ani10122199
7. Patel N, Shackelford K. Irritable Bowel Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
8. Lee C, Doo E, Choi JM, et al. The increased level of depression and anxiety in irritable bowel syndrome patients compared with healthy controls: systematic review and meta-analysis. J Neurogastroenterol Motil. 2017;23(3):349–362. doi:10.5056/jnm16220
9. Good CH, Brager AJ, Capaldi VF, Mysliwiec V. Sleep in the United States Military. Neuropsychopharmacology. 2020;45(1):176–191. doi:10.1038/s41386-019-0431-7
10. Lee SY, Ryu HS, Choi SC, Jang SH. A study of psychological factors associated with functional gastrointestinal disorders and use of health care. Clin Psychopharmacol Neurosci. 2020;18(4):580–586. doi:10.9758/cpn.2020.18.4.580
11. Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28:203–209.
12. Kuwahara A, Matsuda K, Kuwahara Y, Asano S, Inui T, Marunaka Y. Microbiota-gut-brain axis: enteroendocrine cells and the enteric nervous system form an interface between the microbiota and the central nervous system. Biomed Res. 2020;41(5):199–216. doi:10.2220/biomedres.41.199
13. Quigley EMM. Gut microbiome as a clinical tool in gastrointestinal disease management: are we there yet? Nat Rev Gastroenterol. Hepatol. 2017;14:315–320.
14. Wong K, Isaac DM, Wine E. Growth delay in inflammatory bowel diseases: significance, causes, and management. Dig Dis Sci. 2021;66(4):954–964. doi:10.1007/s10620-020-06759-5
15. Fernández-Bravo A, Figueras MJ. An update on the genus Aeromonas: taxonomy, epidemiology, and pathogenicity. Microorganisms. 2020;8(1):129. doi:10.3390/microorganisms8010129
16. Fernandez-Tome S, Hernandez-Ledesma B, Chaparro M, Indiano-Romacho P, Bernardo D, Gisbert JP. Role of food proteins and bioactive peptides in inflammatory bowel disease. Trend Food Sci Technol. 2019;88:194–206. doi:10.1016/j.tifs.2019.03.017
17. Yao X, Wang Q, Wen H, et al. Clinical features of unspecified functional bowel disorder in servicemen from a Chinese army unit. Med J Chin People”s Lib Army. 2017;42(1):76–80.
18. Ono M, Kato M, Miyamoto S, et al. Multicenter observational study on functional bowel disorders diagnosed using Rome III diagnostic criteria in Japan. J Gastroenterol. 2018;53(8):916–923. doi:10.1007/s00535-017-1428-9
19. Ballou S, Rangan V, Eidelberg A, et al. What is unspecified functional bowel disorder? A commonly seen, rarely recognized, and poorly understood diagnosis. Am J Gastroenterol. 2023;118(8):1402–1409. doi:10.14309/ajg.0000000000002281
20. Wu G, Wu L, Yang P, et al. Effects of long voyage of surface ships and nuclear submarines on anxiety, depression and sleep quality of sailors. J Prev Med Chin People”s Lib Army. 2002;6:418–421.
21. Wong OWH, Lam AMW, Or BP, et al. Disentangling the relationship of gut microbiota, functional gastrointestinal disorders and autism: a case-control study on prepubertal Chinese boys. Sci Rep. 2022;12(1):10659. doi:10.1038/s41598-022-14785-8
22. Mulita F, Verras GI, Anagnostopoulos CN, Kotis K. A smarter health through the internet of surgical things. Sensors. 2022;22(12):4577. doi:10.3390/s22124577
23. Pannemans J, Masuy I, Tack J. Functional constipation: individualising assessment and treatment. Drugs. 2020;80(10):947–963. doi:10.1007/s40265-020-01305-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
