Back to Journals » International Journal of Women's Health » Volume 15
Retrospective Analysis of Pregnancy Outcomes Following External Cephalic Version for Breech Presentation
Received 4 July 2023
Accepted for publication 22 November 2023
Published 11 December 2023 Volume 2023:15 Pages 1941—1949
DOI https://doi.org/10.2147/IJWH.S428946
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Jun Han,1 Shuai Wang,2 Mei Ding1
1Department of Obstetrics, Guangzhou Hospital of Integrated Traditional and Western Medicine, Guangzhou, 510800, People’s Republic of China; 2Department of Critical Care Medicine, Guangzhou Hospital of Integrated Traditional and Western Medicine, Guangzhou, 510800, People’s Republic of China
Correspondence: Jun Han, Department of Obstetrics, Guangzhou Hospital of Integrated Traditional and Western Medicine, No. 87, Yingbin Avenue, Huadu District, Guangzhou, 510800, People’s Republic of China, Tel +86 020-86888565, Email [email protected]
Objective: We explored the feasibility and safety of external cephalic version (ECV) for cases of breech presentation.
Methods: We retrospectively analyzed data from 158 singleton pregnant women with breech presentation at 36 weeks gestation, admitted to Guangzhou Hospital of Integrated Traditional and Western Medicine from January 2018 to March 2022. 42 underwent ECV, categorized as the ECV group, while 116 without ECV comprised the control group. Systematic collection and evaluation of pregnancy outcomes were conducted for both groups.
Results: Within the control group, 16 cases experienced a spontaneous transition to head presentation, among which 14 cases resulted in successful vaginal deliveries. In 2 cases, cesarean deliveries were performed due to fetal macrosomia and persistent posterior occipital presentation. Furthermore, 2 cases of breech presentation in pregnant women were successfully delivered vaginally through breech traction, necessitating an emergency procedure due to the wide opening of the uterus. Within the ECV group, 28 cases were successfully inverted to the cephalic presentation. Among them, 1 case underwent an emergency cesarean delivery due to fetal distress during cephalic delivery, 3 cases required cesarean deliveries due to abnormal labor, and 24 cases were successfully delivered vaginally. The comparative analyses showed that the cesarean section rate (18/42 vs 100/116) and non-cephalic delivery rate (14/42 vs 100/116) in the ECV group were significantly lower than those in the control group (P < 0.001). There was no statistically significant differences between the two groups with respect to the rate of newborns with Apgar score < 7 (1/42 vs 3/116), premature rupture of membrane (3/42 vs 20/116), acute fetal distress (2/42 vs 2/116), and cord prolapse (0/42 vs 1/116) (P > 0.05).
Conclusion: ECV can effectively reduce the rate of cesarean delivery and non-cephalic deliveries. However, it but requires strict adherence to indications and continuous monitoring.
Keywords: abnormal fetal presentation, cesarean section rate, ECV, pregnancy complications
Introduction
Breech presentation is one of the potential fetal positions during childbirth, constituting approximately 3%–4% of all full-term deliveries. This presentation is associated with a significantly higher perinatal mortality rate, ranging from 3 to 8 times that of cephalic presentation.1 In cases of breech presentation, the cesarean section rate is as high as 80%–90%, making it the second or third most common indication for cesarean section.2,3 A nationwide multicenter study in China revealed that cesarean sections conducted in cases of breech and transverse fetal positions accounted for 5.815% of the overall cesarean section procedures performed. It is essential to acknowledge the prevalent overuse of cesarean sections in clinical practice, a practice that has potential adverse effects on both maternal and fetal health. Reports from China, along with recommendations from the World Health Organization (WHO), emphasize the importance of maintaining the cesarean section rate below 15% in any region globally. However, some experts suggest a more reasonable threshold of 19% in order to strike a balance between necessary medical interventions and natural childbirth.4 Minimizing breech deliveries can significantly contribute to controlling the overall cesarean delivery rate and, in turn, reduce the perinatal mortality rate.5 Currently, various methods, such as acupuncture and moxibustion, are employed to alter the fetal position.6 However, the effectiveness and safety of these techniques remain subjects of considerable debate within the academic community. External cephalic version (ECV) is a medical procedure employed to alter fetal presentation by applying pressure on the abdominal wall. This technique is utilized to convert a breech presentation into a cephalic presentation, effectively increasing the rate of cephalic deliveries and reducing the incidence of cesarean sections in pregnant women who are at or near term with abnormal fetal presentation before childbirth.7 Since 2018, Guangzhou Hospital of Integrated Traditional and Western Medicine has been conducting ECV procedures without anesthesia, assisted by B-ultrasonography. In this study, we retrospectively analyzed data from 158 singleton pregnant women with breech presentation at ≥ 36 weeks of gestation, admitted to Guangzhou Hospital of Integrated Traditional and Western Medicine between January 2018 and July 2021. The aim was to investigate the feasibility and safety of ECV, providing valuable evidence for clinical practice.
Materials and Methods
Study Participants
We conducted a retrospective analysis involving 158 singleton pregnant women with breech presentation at ≥ 36 weeks of gestation. These cases were treated at the obstetrics clinic of Guangzhou Hospital of Integrated Traditional Chinese and Western Medicine between January 2018 and July 2021. The study comprised 42 cases in the ECV group, where patients underwent ECV at the hospital, and 116 cases in the control group, consisting of breech presentations at 36 weeks who did not undergo ECV. The sample size calculation formula is  The ratio between the ECV group and the control group was approximately 1:3. All pregnant women in the ECV group willingly underwent the procedure to reverse fetal presentation after receiving comprehensive information about the associated risks. The study was approved by Ethics Committee of the Guangzhou Hospital of Integrated Traditional And West Medicine (20220084). Written informed consent was obtained from all participants.
The ratio between the ECV group and the control group was approximately 1:3. All pregnant women in the ECV group willingly underwent the procedure to reverse fetal presentation after receiving comprehensive information about the associated risks. The study was approved by Ethics Committee of the Guangzhou Hospital of Integrated Traditional And West Medicine (20220084). Written informed consent was obtained from all participants.
Inclusion and Exclusion Criteria
Inclusion criteria: Singleton pregnancy; breech presentation confirmed by B-ultrasonography at week 36 of gestation; amniotic fluid index ≥ 5 cm; cord around neck ≤ 2 loops.
Exclusion criteria: Suspected intrauterine fetal distress; scarred uterus (a history of ≥ 2 cesarean sections or penetration of inner membrane in myomectomy or removed myoma > 6 cm); uterine anomalies (eg, septate uterus) or fetal anomaly (eg, sacrococcygeal teratoma); antepartum hemorrhage; contraindications to vaginal delivery.
External Cephalic Version
Pre-Procedure Preparation
Pregnant women who met the inclusion criteria received essential information and were admitted at 36–37 weeks of gestation. During their admission, they underwent various examinations, including routine blood tests, coagulation and biochemical tests, cross-matching tests, establishment of intravenous access, and fetal heart rate monitoring. Subsequently, the study participants provided written consent by signing the informed consent form after receiving comprehensive information regarding the surgical procedure. Preoperative fetal heart rate monitoring indicated normal patterns, ensuring the safety of the procedure. The ECV procedure was performed in a delivery room equipped for cesarean section, with the availability of a bedside ultrasound machine. Prior to the procedure, we conducted pre-procedural ultrasonography once more to assess fetal lie, breech type, fetal position, placental location, estimated fetal weight (EFW), and amniotic fluid index (AFI). Additionally, blood pressure measurements were also taken. In instances where fetal heart rate monitoring indicated uterine contractions, a 10 mg dose of nifedipine8 was administered orally approximately 30 minutes before the procedure. Vital signs were meticulously monitored during this period. The ECV procedures were conducted by a single obstetrician with extensive experience, having performed over 500 ECVs.8
ECV Procedure
The pregnant women were positioned on their back with legs flexed and abdomen exposed. A suitable amount of lubricant was applied to the abdomen to minimize discomfort. The practitioner stood on the right side of the pregnant women and assessed the presentation. In cases of breech presentation within the pelvic cavity, the presenting part was carefully held, and gentle pressure was applied to push the breech upward, facilitating its movement out of the pelvic cavity. When the fetal spine was on the right side of the abdomen, the practitioner used their right hand to hold the fetal head and their left hand to hold the fetal buttocks. The practitioner applied gentle pressure, pushing the fetal head toward the pubic symphysis in a clockwise forward roll motion with the right hand, while simultaneously guiding the fetal buttocks clockwise toward the uterine fundus with the left hand (as depicted in Figure 1). Conversely, if the fetal spine was on the left side of the abdomen, the practitioner held the fetal head in their left hand and the fetal buttocks in their right hand, employing a counterclockwise inversion motion (as illustrated in Figure 2). Upon confirmation of the fetal presentation through ultrasonography, the practitioner used two hand towels to hold the fetal head and secured the presentation with an abdominal belt. If there was difficulty in turning the baby, the practitioner did not apply excessive force but attempted gentle maneuvers in both clockwise and counterclockwise directions. If these attempts were unsuccessful after two tries in each direction, the ECV procedure was considered unsuccessful. Regardless of the outcome of the ECV procedure, the fetal heart rate was promptly monitored after the intervention. Additional assessments, such as fetal heart monitoring and evaluation of cord blood flow, were conducted on the same day. If there were no abnormalities observed in the fetal heart rate monitoring and the pregnant women did not experience symptoms like abdominal pain, they were discharged on the following day, with the fetal presentation considered fixed until the head engaged. If abnormal fetal heart rate patterns were detected during intraoperative monitoring, the practitioner promptly halted the procedure. The position of the pregnant women was adjusted, and intrauterine resuscitation measures, such as oxygen inhalation, were initiated. If the fetal heart rate deceleration persisted and could not be restored to normal levels, an immediate cesarean section was performed to ensure the safety of both the mother and the baby.
Observation Indicators
We collected clinical data from postpartum women and newborns in both the ECV group and the control group. We observed and compared various factors, including the age, gravidity, parity, delivery gestational age, BMI, newborn birth weight of the mothers, as well as the rates of cesarean section, non-cephalic deliveries, and neonatal Apgar scores < 7 (at 5 minutes). Additionally, we examined the rates of premature rupture of membranes, cord prolapse, acute fetal distress, and fetal death between the two groups for comprehensive analysis.
Statistical Analysis
Statistical analysis was conducted using SPSS 19.0 software. Count data are presented as cases and percentages, and group comparisons were made using the chi-squared test. Logistic regression analysis was employed to assess the impact of maternal general condition on pregnancy complications in the context of EVC usage. A significance level of P < 0.05 was considered statistically significant.
Results
Comparison of General Conditions of the Puerpera Between the Two Groups
There were no statistically significant differences between the ECV group and the control group in terms of age, gravidity, parity, delivery gestational age, BMI, and newborn birth weight (P > 0.1). See Table 1.
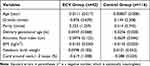 |
Table 1 Comparison of General Conditions of Puerperae Between the ECV Group and Control Group |
Comparison of Delivery Modes and Pregnancy Outcome Between the Two Groups
In the control group, out of 116 pregnant women, 16 experienced a natural transition to head presentation, resulting in a total of 16 vaginal deliveries. Consequently, the cesarean section rate was 86.2% (100 out of 116 cases), the rate of non-cephalic deliveries was also 86.2% (100 out of 116 cases), and the proportion of newborns with an Apgar score at 5 minutes < 7 was 2.6% (3 out of 116 cases). There was 1 case with cord prolapse, who underwent emergency cesarean section, and the birth score was 5-9-10 points, with satisfactory prognosis; there was 1 case with breech extraction that had a birth score of 6-10-10 points, and 1 case where there was difficulty in emergence of the head delivered by cesarean section, with a birth score of 6-9-10 points. All 3 cases had satisfactory prognosis. Among the 42 pregnant women in the ECV group, 28 were successfully inverted, and 14 failed. The non-cephalic delivery rate was 33.3% (14/42 cases). Moreover, 24 pregnant women successfully delivered vaginally, and the cesarean section rate was 42.9% (18/42 cases). Due to 1 fetal death 42 hours after the operation, the rate of newborns with Apgar score < 7 was 2.4% (1/42 cases). The cesarean section rate and non-cephalic delivery rate in the ECV group were significantly lower than that in the control group (P < 0.05), indicating a statistically significant difference; the difference in the rate of Apgar score < 7 between the two groups was not statistically significant (P > 0.05). See Table 2.
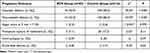 |
Table 2 Pregnancy Outcome and Pregnancy Complications Between the ECV Group and Control Group |
Comparison of Incidence of Pregnancy Complications Between the Two Groups
Among the 116 cases in the control group, 1 had cord prolapse, 20 (17.2%) had premature rupture of membrane, and 2 (1.7%) had acute fetal distress, including cord prolapse and late deceleration during breech traction. In the ECV group, 3/42 cases (7.1%) had premature rupture of membrane, no one had cord prolapse, and 2/42 cases (4.8%) had acute fetal distress, including 1 case of fetal death and 1 case who underwent emergency cesarean section due to suspected late deceleration of maternal-fetal blood transfusion within 6 hours after the ECV. See Table 2.
Discussion
Effectiveness of ECV
Breech presentation is one of the potential fetal positions during childbirth, occurring in approximately 3%–4% of all full-term deliveries. This presentation often leads to a high cesarean delivery rate. National cesarean delivery rates, reaching up to approximately 19 per 100 live births, have been associated with lower maternal or neonatal mortality in WHO member states. This suggests that previously recommended national target rates for cesarean deliveries may be underestimated and need to be reconsidered.4 Cesarean delivery is generally considered a safe procedure, but it is not without risks and complications. Immediate intraoperative and postoperative complications, such as infection or hemorrhage, can occur, along with long-term issues that may complicate or prevent future pregnancies, including conditions like placenta accreta and uterine rupture.9 The decision to perform a cesarean section is influenced by various clinical conditions, including obstructed labor, breech presentation, repeat cesarean sections, and cases of non-reassuring fetal breech presentation (10.8%).10,11
Before the 30th week of gestation, breech presentation may spontaneously transition to cephalic presentation. However, when breech presentation persists beyond the 30th week, corrective measures are typically required.1 At present, there are several methods of correcting breech presentation but their effects and safety are controversial. In 2020, the American College of Obstetricians and Gynecologists (ACOG) updated the guidelines for ECV issued in 2016: If there are no surgical contraindications, ECV should be strongly recommended in near full-term pregnant women with breech presentation.12 In 2020, the French College of Gynaecologists and Obstetricians (CNGOF) issued its clinical practice guidelines for breech presentation: Acupuncture, moxibustion, and postural changes (knee-chest or lying supine with elevated breech) cannot effectively reduce breech presentation, while ECV can effectively lower the incidence of breech presentation and cesarean section rate.13 The Royal College of Obstetricians and Gynaecologists (RCOG) issued obstetric guidelines and pointed out that the success rate of ECV performed by trained operators could reach 50% (30%–80%), with individual differences.14 In full-term or near full-term pregnant women with breech presentation, External Cephalic Version (ECV) has been shown to reduce the rates of non-cephalic deliveries and cesarean sections. These findings are consistent with results from a prospective cohort study.15,16 In line with these findings, the current study demonstrated that out of 42 pregnant women with breech presentation in the ECV group, 28 successfully converted to cephalic presentation. The cesarean section rate was 42.9%, and the non-cephalic delivery rate was 33.3%, both significantly lower than the control group (86.2%). These results indicate that ECV can substantially reduce both cesarean section and non-cephalic delivery rates.
Safety of ECV
In 2015, a meta-analysis involving 8 studies was conducted, and the results showed that, compared with breech presentation without ECV, the risk of non-cephalic delivery after ECV was reduced by about 60%, and the risk of cesarean section was reduced by about 40%. There was no significant difference in the incidence of adverse neonatal outcomes (low Apgar score, low umbilical vein pH, and death) between the two groups.17 The CNGOF pointed out that, compared with the expectant management of breech presentation, ECV did not increase the risk of intrauterine death, whose incidence was close to 0.5% in both groups. Moreover, ECV reduced the rate of emergency cesarean section due to bleeding or change in fetal heart rate below l%. Collins et al18 reported that the risks associated with External Cephalic Version (ECV) primarily include placental abruption, cord prolapse, premature rupture of membranes, intrauterine death, and fetomaternal transfusion. The overall incidence of these complications is lower than 1%, and the rate of emergency cesarean section was approximately 0.5%. Macharey et al19 conducted a retrospective study and found that the incidence of ECV was 1.3%, which was close to the incidence of planned cesarean section. Some studies on the safety of ECV showed that ECV had a low rate of complications, but there was still a latent possibility of risk; therefore, it should be performed only in medical institutions with monitoring equipment and emergency delivery set-ups. For correcting full-term and near-full-term singleton breech presentation, it is essential for the medical staff performing the procedure to clearly identify the indications and contraindications. Adequate monitoring and adherence to appropriate techniques as per regulations are crucial steps to achieve a high success rate and ensure safety during the procedure.20,21 ECV is a valuable management technique and, when applied to a properly selected population, presents minimal risks to both the mother and the fetus. If successful, ECV offers a distinct benefit to the mother by providing her with the opportunity for a successful vertex vaginal delivery. Given the small risk of adverse events associated with ECV and the significantly lower cesarean birth rate observed in women who have undergone successful ECV, it is recommended that all women near term with breech presentations should be offered ECV if there are no contraindications.12 In the present study, the rate of Apgar score < 7 at 5 min in the ECV group was not significantly different from that in the control group, which is consistent with the current data. ECV did not increase the incidence of neonatal asphyxia. While the rate of premature rupture of membranes was low in the ECV group, it is important to note that, due to the inadequate sample size, there were no statistically valid data to conclusively demonstrate that ECV can reduce the incidence of premature rupture of membranes. Additionally, there was no statistically significant difference in the rate of cord prolapse and acute fetal distress between the two groups. The results mentioned above indicated that ECV did not lead to an increased incidence of pregnancy complications. However, it is noteworthy that one case in the ECV group experienced spontaneous repeated deceleration during routine fetal heart rate monitoring after the procedure, with frequent late deceleration occurring six hours post-ECV. While the outcome was satisfactory due to the prompt treatment of abnormalities detected through continuous postoperative fetal heart rate monitoring, this highlights the necessity for vigilant fetal monitoring and timely intervention during and after ECV to prevent adverse outcomes.
Regrettably, in another case involving a 37-week pregnant woman, the fetus passed away 38 hours after ECV. During vaginal delivery, it was observed that the fetus had two loops of cord around the neck. Consequently, the cause of death was determined to be cord-around-The-neck and polyhydramnios. Following ECV, fetal heart rate monitoring revealed an atypical rate (without acceleration), and 34 hours later, the fetal presentation reverted to breech presentation once again. Under ultrasound guidance, the physician corrected the presentation and stabilized the fetal position. Despite normal findings in fetal blood flow and absence of cord entanglement around the neck during ultrasonography, the physician found that the fetal heart rate was not recorded four hours after the ECV. During delivery, it was observed that the umbilical cord was thin, approximately 100 cm in length, and wrapped in two loops around the neck. Additionally, the amniotic fluid volume was measured to be about 3000 mL. Lesson from this case: 1. The fetal heart rate monitoring displayed an atypical pattern (lacking acceleration), and further examination indicated the presence of polyhydramnios. The estimated fetal weight at 37 weeks was 2.5 kg. In this scenario, the physician should have taken into account the possibility that the abnormal fetal heart rate monitoring indicated intrauterine fetal distress, rather than solely relying on surgical indications. 2. Following ECV, the fetal heart rate monitoring displayed an atypical pattern with good baseline variation but without noticeable accelerations. The physician continued to monitor the fetal heart rate but attributed the abnormality to reduced fetal movement caused by the fixed presentation. Consequently, the physician loosened the abdominal belt. Unfortunately, the physician did not diagnose intrauterine hypoxia promptly. 3. The physician did not halt the procedure immediately upon detecting abnormal fetal heart rate patterns but instead chose to re-fix the inverted fetal presentation. 4. Prior to conducting ECV, a thorough assessment, including evaluating gestational age, fetal position, fetal size, placental location, cord entanglement, and amniotic fluid levels, is essential. In cases where the fetus has the cord wrapped around the neck for more than two loops, ECV should be approached with caution, and strict monitoring of the fetal heart rate is imperative. There were shortcomings in monitoring and treatment. In this study, 2 of the 42 cases that underwent ECV exhibited abnormal fetal heart rates, indicating an elevated likelihood of fetal distress and the risk of fetal demise associated with the procedure. ECV should be conducted following the principle of effectively enhancing the success rate while minimizing maternal and fetal risks.
In summary, before performing ECV for singleton pregnant women with breech presentation, it is crucial to conduct a comprehensive evaluation of relevant factors, identify both indications and contraindications, provide complete information to the pregnant women, ensure adequate preparation for the procedure, and conduct it under conditions where emergency cesarean section is readily available. The procedure should be executed in a standardized manner, with vigilant monitoring of the maternal and fetal conditions afterward. Any issues that arise should be accurately assessed and promptly addressed.
Limitations of the Study
As a retrospective study, there may be some bias in the inclusion of cases, and the sample size was small. There was a significant difference in the number of cases between the two groups. All these factors could affect the accuracy of the findings. To ensure more reliable results, it is imperative to enlarge the sample size and conduct a prospective study. Additionally, adjustments should be made to the results to mitigate the influence of residual confounding variables.
Conclusion
In 2014, a domestic multicenter study showed that cesarean sections with breech and transverse position accounted for 5.815% of the total number of cesarean sections In indications for cesarean section are fifth22 perinatal mortality (0.5 / 1000) and vaginal delivery (2 / 1000) Compared with, slightly lower, but also face the risk of surgery.23 The cesarean section rate and non-cephalic delivery rate significantly decreased following ECV without a corresponding increase in the incidence of pregnancy and delivery complications. However, there is still considerable progress needed in promoting the widespread adoption of ECV in China. Multi-center clinical studies with a large sample size are essential to investigate training methods for enhancing the success rate of the procedure, assess the necessity of preoperative anesthesia, and evaluate the use of contraction inhibitors to improve success rates. Furthermore, rigorous measures are needed to minimize procedural risks and to implement thorough intraoperative and postoperative monitoring and management to promote normal delivery.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Guangzhou Hospital of Integrated Traditional And West Medicine (No.20220084). Written informed consent was obtained from all participants.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
No external funding was received to conduct this study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Cunningham FG, Leveno KJ, Bloom S. Williams Obstetrics.
2. Shen Y, Lin JH, Lin QD, et al. Influencing factors of cesarean section rate in some areas of china and analysis of operation indications. J Pract Obstetrics Gynecol. 2011;27(03):183–187.
3. Guo Z, Zhang RX, Guo HJ, et al. Contrast analysis of rate and indications for cesarean section from 1990 to 2009. Maternal Child Health Care China. 2012;27(20):3089–3092.
4. Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA. 2023;314(21):2263–2270. doi:10.1001/jama.2015.15553
5. Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR; Term Breech Trial Collaborative Group. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet. 2000;356(9239):1375–1383. doi:10.1016/s0140-6736(00)02840-3
6. Libretti A, Surico D, Corsini C, Aquino CI, Fracon S, Remorgida V. YouTube™ as a source of information on acupuncture for correction of breech presentation. Cureus. 2023;15(2):e35182. doi:10.7759/cureus.35182
7. Xie X, Kong BH, Duan T. Obstetrics and Gynecology[M].
8. Lee R, Anat L, Yuval F, et al. Efficacy of a second external cephalic version (ECV) after a successful first external cephalic version with subsequent spontaneous reinversion to breech presentation: a retrospective cohort study. Arch Gynecol Obstetrics. 2021;303:911–916. doi:10.1007/s00404-020-05819-5
9. Grootscholten K, Kok M, Oei SG, Mol BWJ, van der Post JA External cephalic version-related risks: a meta-analysis. Obstet Gynecol. 2008;112:1143–1151.
10. Cegolon L, Mastrangelo G, Maso G, Dal Pozzo G, et al. Understanding factors leading to primary cesarean section and vaginal birth after cesarean delivery in the friuli-venezia giulia region (north-eastern Italy), 2005–2015. Scientific Reports. 2021;10:380 (2020). doi:10.1038/s41598-019-57037-y
11. Cegolon L, Mastrangelo G, Heymann WC, Dal Pozzo G, Ronfani L, Barbone F. A systematic evaluation of hospital performance of childbirth delivery modes and associated factors in the Friuli venezia Giulia region (North-Eastern Italy), 2005-2015. Sci Rep. 2019;9(1):19442. doi:10.1038/s41598-019-55389-z
12. Baxi Laxmi. External cephalic version: acog practice bulletin, number 221. Obstet Gynecol. 2020;135(5):e203–e212. doi:10.1097/AOG.0000000000003837
13. Sentilhes L, Schmitz T, Azria E, et al. Breech presentation: Clinical Practice Guidelines From The French College of Gynaecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol. 2020;252:599–604. doi:10.1016/j.ejogrb.2020.03.033
14. Hussin OA, Mahmoud MA, Abdel Fattah MM. External cephalic version and reducing the incidence of term breech presentation: Green-top Guideline No. 20a. BJOG. 2017;124(7):e178–e192. doi:10.1111/1471-0528.14466
15. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Data Base Syst Rev. 2012;10(10):CD000051. doi:10.1002/14651858.CD000051.pub2
16. Hussin OA, Mahmoud MA, Abdel-Fattah MM. External cephalic version for breech presentation at term: predictors of success, and impact on the rate of caesarean section. East Mediterr Health J. 2013;19(2):162–166. doi:10.26719/2013.19.2.162
17. Hofmeyr GJ, Kulier R. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012;10:CD000083. doi:10.1002/14651858.CD000083.pub2
18. Collins S, Ellaway P, Harrington D, Pandit M, Impey LW. The complications of external cephalic version: results from 805 consecutive attempts. BJOG. 2007;114(5):636–638. doi:10.1111/j.1471-0528.2007.01271.x
19. Macharey G, Ulander VM, Heinonen S, Kostev K, Nuutila M, Väisänen-Tommiska M. Risk factors and outcomes in “well-selected” vaginal breech deliveries: a retrospective observational study. J Perinat Med. 2017;45(3):291–297. doi:10.1515/jpm-2015-0342
20. Li X, Hu J, Wang X, Zhang H, Liu J. Moxibustion and other acupuncture point stimulation methods to treat breech presentation: a systematic review of clinical trials. Chin Med. 2009;4:4. doi:10.1186/1749-8546-4-4
21. He DM, Lu J, Huang M. Clinical study on auricular acupressure therapy cooperate with self-correcting method to correct breech presentation. Fujian Univ Trad Chin Med. 2011;6. doi:10.1186/1749-8546-6-27
22. Lei H, Li G, Zou L, et al. A central study of the national composition ratio of cesarean section rate and indications of cesarean section. Chin J Obstet Gyneco. 2014;49(10):728–735.
23. Goffinet F, Azria E, Kayem G, et al. Re: the risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies: let’s avoid simplistic radicalism when reality is complex. BJOG. 2016;123(1):145–147. doi:10.1111/1471-0528.13734
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


