Back to Journals » Journal of Inflammation Research » Volume 15
Response Guided Slow Infusion of Albumin, Vasoconstrictors and Furosemide Improves Ascites Mobilization and Survival in Acute on Chronic Liver Failure: A Proof-of-Concept Study
Authors Pande G, Hatti M, Rai MK, Rai P, Kumar K, VP K, Nehra A, Kumar S, Ranjan Rout S, Mishra SK, Kumar D , Kumar U , Mishra P, Majeed A, Saraswat VA, Singh K, Singh H, Misra DP , Agarwal V
Received 14 June 2022
Accepted for publication 13 August 2022
Published 1 September 2022 Volume 2022:15 Pages 5027—5039
DOI https://doi.org/10.2147/JIR.S377494
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Gaurav Pande,1 Manjunath Hatti,1 Mohit Kumar Rai,2 Praveer Rai,1 Kamlesh Kumar,1 Krishna VP,1 Abhimanyu Nehra,1 Sudeep Kumar,3 Smarak Ranjan Rout,3 Sourav Kumar Mishra,3 Dinesh Kumar,4 Umesh Kumar,4 Prabhaker Mishra,5 Abdul Majeed,1 Vivek Anand Saraswat,1,* Kritika Singh,2 Harshit Singh,2 Durga Prasanna Misra,2 Vikas Agarwal2,*
1Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India; 2Clinical Immunology and Rheumatology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India; 3Cardiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India; 4Department of Advanced Spectroscopy and Imaging, Center of Biomedical Research, Lucknow, India; 5Biostatistics, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India
*These authors contributed equally to this work
Correspondence: Vikas Agarwal, Unit III, Clinical Immunology and Rheumatology, SGPGIMS, Raebareli Road, Lucknow, India, Tel +918004904390, Fax +91522268812, Email [email protected]
Background and Aims: Acute-on-chronic liver failure (ACLF) with increasing organ failure is associated with poor outcomes. Severely deranged systemic hemodynamics and decreased effective arterial blood volume contribute to tissue damage and organ failure. Response-guided therapy with albumin, vasoconstrictors, and furosemide may help overcome effective hypovolemia, improve diuresis and impact survival.
Methods: In the observation cohort, 230 patients with ACLF (CANONIC criteria) with ascites (≥Grade II) and ACLF ≥Grade I were enrolled. A total of 136 patients (GROUP I) received response-guided (urine sodium > 80mmol/day) slow albumin-furosemide infusion ± terlipressin (SAFI ± T), while 94 patients (GROUP II) received standard medical therapy. Twenty-eight-day survival, ascites mobilization (nil or grade 1), and adverse events were noted. In another mechanistic cohort (n = 40), laboratory evidences for improvement in various pathophysiological alterations; gut permeability, endotoxemia, cytokine storm, neutrophil dysfunction, and hemodynamic alterations following SAFI ± T/Noradrenaline (NAdr) were evaluated.
Results: Age, gender, CLIF-C-ACLF, SOFA and MELD scores, ACLF grades and urine sodium were not different between the two groups in the observation cohort. Ascites was mobilized in 102/136 in GROUP I (SAFI ± T) and 23/94 in GROUP II (p < 0.05). Twenty-eight-day survival was significantly higher in GROUP I = 103/136 (75.7%) vs GROUP II = 50/94 (53.2%), (P = < 0.001). All those who were unable to reach urine sodium > 80 mmol/day died. Four patients in GROUP I developed scrotal gangrene. In the mechanistic cohort, 72% of patients survived with significant improvement in gut permeability, endotoxemia, serum cytokines, neutrophil dysfunction, and hemodynamic alterations.
Conclusion: Ascitic fluid mobilization by response-guided SAFI ± T/NAdr therapy improves survival by improving splanchnic and systemic hemodynamics, decreasing gut congestion, gut permeability, and endotoxemia, improving neutrophil functions, and reducing pro-inflammatory cytokines in circulation.
Keywords: urine sodium, hemodynamics, renal artery resistive index, cytokines, neutrophil extracellular traps
Graphical Abstract:

Introduction
Acute on Chronic liver failure (ACLF) is characterized by an acute insult leading on to severe systemic inflammation, altered intestinal permeability and bacterial translocation, endotoxemia, systemic inflammatory response syndrome (SIRS), compensatory anti-inflammatory response syndrome (CARS), immune deregulation, severely deranged systemic hemodynamics and decreased effective arterial blood volume (EABV) leading to tissue damage and one or more organ failure in patients with underlying chronic liver disease. It is associated with increased short-term mortality.1–4 Acute insult over chronic liver disease with worsening portal hypertension leads to increased gut congestion with gut flora dysbiosis leading to increased intestinal permeability (IIP).5,6 It causes the release of endotoxins, causing cytokine surge, increased interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α) in portal blood and liver, which worsens systemic and splanchnic hemodynamics and EABV.7–9 The cytokine storm and endotoxin suppress neutrophils and induce increased expression of inhibitory receptors on lymphocytes. Higher expression of inhibitory receptors and neutrophil dysfunction result in immune paralysis and increased susceptibility to infections which increases morbidity and mortality.10–12
Severe hemodynamic derangements due to decreased EABV could potentially accentuate the already tenuous state of renal vasoconstriction, water retention, ascites, and impending hepatorenal syndrome (HRS) and may eventually lead to renal failure and increased mortality.13 Moderate to large ascitic fluid mobilization is challenging as oral diuretics have limited value, due to the presence of or the increased risk of precipitating renal failure, dyselectrolytemia and hepatic encephalopathy (HE). Lowering portal pressure, decreasing gut congestion, improving gut permeability correcting deranged hemodynamics, and improving EABV and renal function may help reduce organ failures (OFs) and improve survival.
Akin to HRS therapy, the vasoconstrictor effect of low dose continuous Terlipressin combined with albumin infusions cause an increase in total blood volume with moderate reduction of the activity of vasoconstrictor and anti-natriuretic systems help increase the EABV and reverse the basic pathology of splanchnic and systemic vasodilatation, hyperdynamic circulation, sympathetic nervous system (SNS) activation, and intense renal vasoconstriction.13 The plasma expanding effect of albumin is greater at a slow rate infusion.14 Albumin is an effective plasma volume expander due to its high oncotic activity and prolonged half-life and promotes effective vascular refilling in the intravascular compartment helping, reabsorption of fluid stabilizing endothelium, and maintaining capillary permeability. It also interferes with neutrophil adhesion to the capillary endothelium thereby reducing inflammation and aiding the maintenance of endothelial integrity.15,16
Furosemide, a potent loop diuretic, is highly albumin-bound (>95%) and requires good renal perfusion and active albumin to be secreted in the tubular lumen. Furosemide combined with continuous slow albumin infusion should achieve rapid fluid mobilization.17,18 While the onset of action is rapid (within five minutes), the short half-life (1–2 hours), and short duration of diuresis (~6 hours) are offset by continuous infusion.19
We hypothesize that slow, continuous, low-dose albumin ± Terlipressin with furosemide infusion (SAFI±T) offers significant pharmacokinetic advantages. The improvement in hemodynamics by augmenting EABV and fluid mobilization shall result in improved renal perfusion, creatinine clearance and urine output with a significant decrease in plasma renin and aldosterone levels thereby reducing gut congestion, intestinal permeability (IP) and potentially decreasing endotoxemia and cytokine storm and improving extrahepatic OFs and survival.
Methods
Two hundred and fifty-nine consecutive patients with ACLF (based on CANONIC criteria) with ascites (≥ Grade II) and ACLF ≥ Grade I (as per criteria of CLIF-SOFA) were admitted to the Gastroenterology Units of the Sanjay Gandhi Postgraduate Institute of Medical Sciences during the study period from October 2013 to December 2016. A total of 29 patients were excluded (Figure 1).
 |
Figure 1 Flow chart showing the number of subjects enrolled in the study. |
In this prospective open-labeled non-randomized observational study, 230 patients were recruited, 136 were enrolled in the GROUP I (slow albumin and furosemide ±Terlipressin), and 94 patients in the standard medical treatment (SMT) group (GROUP II) after obtaining written informed consent (Figure 1). The study complied with the Declaration of Helsinki and was approved by the institutional ethics committee of SGPGI [2017–186-DM-99(B), 2017–214-DM-100, 2016–144-DM-93, 2018–86-DM-104].
Inclusion Criteria
- Adults between the ages of 18–65 years fulfilling the criteria of ACLF – Acute insult to an overlying chronic liver disease defined by liver failure as defined by Acute-On-Chronic Liver Failure in cirrhosis (CANONIC) Study.4
- All patients with ACLF grade ≥1* and ascites (≥grade 2)
- Chronic Liver Failure Consortium Acute on Chronic Liver Failure (CLIF-C-ACLF) <65
- Ascites – High SAAG (Serum albumin-ascitic albumin gradient)
- (*=as per CLIF SOFA Organ Failure scores4)
Exclusion Criteria
- Hepatocellular carcinoma
- Central venous pressure (CVP) >20mmHg
- Allergic to Albumin
- Patients requiring ventilator support within 24 hours of admission
- Chronic kidney disease on dialysis or patients with acute tubular necrosis or having undergone dialysis in the past 1 week.
- Patients with chronic diseases (coronary artery disease, cardiomyopathy, arrhythmias, pericarditis, chronic obstructive pulmonary disease, end-stage renal disease, peripheral vascular disease of lower limbs).
- Contraindication to Terlipressin.
- Patient with pre-renal acute kidney injury (AKI) based on a combination of factors including; recent history of excessive fluid loss (diuresis, diarrhea), CVP (Low CVP <4 cm H2O with ≥1cm H2O increase during inspiration, IVC collapsibility index cIVC >50% (difference between the maximum and minimum IVC diameters divided by the maximum IVC diameter, expressed as a percentage ([IVC dmax – IVC dmin]/IVC dmax × 100%) RARI <0.7.20–23
- Patients with malignancy, severe comorbid conditions, pregnancy or lactation, patients on immunosuppressants, and any coexisting history of immunodeficiency including HIV.
Organ Failure: The criteria for organ failure were based on CLIF –SOFA Scores.4
Treatment: Treatment of sepsis, spontaneous bacterial peritonitis (SBP), and other precipitating causes such as alcohol, and hepatotoxic drugs were done as per standard recommendations.24,25 Treatment between the two groups differed in fluid mobilization and correction of AKI (AKI-HRS) as highlighted below:
Treatment Protocol (GROUP 1): A response-guided therapy of slow infusion of albumin and furosemide and Terlipressin±Noradrenaline based on urinary sodium (UNa+) was initiated with close monitoring of serum and urinary electrolytes and hemodynamic measurements for ascites mobilization irrespective of AKI-HRS (details in supplementary file 1).
Standard medical treatment (GROUP II): Patients with ascites were treated as per details provided in the Supplementary file 1. If serum creatinine was high with clinical suspicion of AKI-HRS, then diuretics were withheld and the patient was initiated on albumin (20–40g/d) and Terlipressin (1–2 mg Q4-6 hourly). Albumin was also used for the treatment of SBP and large volume paracentesis as per standard guidelines wherever indicated.
Outcome Measures
The primary outcome measure was twenty-eight-day survival.
Secondary outcome measures were
- Grade 1 or no ascites on ultrasonogram
- Adverse events
Endpoint
The endpoint of the study was death or completion of 28 days of follow-up.
Furthermore, we undertook a mechanistic study to assess the laboratory evidence for improvement in various pathophysiological alterations; gut permeability, endotoxemia, cytokine storm, neutrophil dysfunction, and hemodynamics. For this purpose, a prospective longitudinal cohort study was performed on 40 patients with ACLF between January and December 2018. Systemic and splanchnic hemodynamic studies included cardiac indices on echocardiography26 and RARI, intestinal permeability, serum endotoxin levels and cytokines (TNF-α, IL1β, IL-6, IL-4, IL-10, IFN-γ), and neutrophil dysfunction by neutrophil extracellular traps (NETosis) were carried out. The protocol was tweaked to add a lower dose of Terlipressin in combination with Noradrenaline (NAdr) due to significantly greater side effects (scrotal gangrene) with a higher dose of Terlipressin in the previous phase of the study (Supplementary file 1).
Statistical Analysis
Normality of the continuous data was tested and continuous variables with normally distributed were presented using mean ± standard deviation, non-normal/discrete data in median (Range) while for categorical data, frequency and percentage were used. Independent samples t-test/Mann Whitney U-test were used for comparison between mean/medians of two groups while the Chi-square test was used to compare proportions. Paired t-test was used to compare the means between pre-post treatment observations. Kaplan–Meier method with Log rank test was used to compare the survival distributions between two groups. Two-tailed p values <0.05 were statistically significant. Statistical package for social sciences, version-23 (SPSS-23, IBM, Chicago, USA), and Med Calc software were used for the data analysis.
Results
The mean age of the patients was 40.2 ± 19.6 years (range 20–59) with 183 (79.6%) males. The baseline clinical, demographic, and biochemical characteristics of patients between GROUP-I and GROUP-II, were compared (Table 1). The mean age of the GROUP-I and GROUP-II was 42.3 ± 20.5 and 38.6 ± 18.4 (p = 0.162). The previous decompensation episodes in these patients included ascites in 136 (59.1%) patients and at least an episode of hepatic encephalopathy in 74 (32.2%). At enrolment in GROUP I, there were 54 (39.8%) patients in ACLF 1, 48 (35.2%) patients in ACLF II, and 34 patients (25%) in ACLF III. In GROUP II, there were 48 (51%) patients in ACLF I, 29 (31%) in ACLF II, and 17 (18%) in ACLF III. Alcohol and sepsis were the common aetiologies of acute decompensation in both groups. Alcohol was the commonest cause of chronic liver disease.
 |
Table 1 Characteristics of Patients in GROUP I vs GROUP II |
Survival: Twenty-eight-day survival was significantly different between the groups [GROUP I 103/136 (75.7%) vs GROUP II 50/94 (53.2%) (P=<0.001)], Figure 2A. Overall, 120/136 patients in GROUP I achieved UNa+ >80mmol/24 hours during the therapy. Analysis of the time required to achieve UNa+>80mmol/24 hrs was carried out and mortality was noted in that particular group. Thirty-six patients achieved UNa+>80mmol/24hrs within 48 hours and all survived; 70 achieved UNa+>80mmol/24 hrs between 48 and 96 hours and 63 (90%) survived; 14 achieved UNa+ >80mmol/24 hrs between 96 hours-7 days and only 4 (28%) survived and 16 could not achieve UNa+ >80mmol/24hrs and all died (100%) (Figure 2B). Urinary sodium was not measured in GROUP II as it had no requirement in SMT.
Ascites Mobilization: Ascites was mobilized (nil/grade 1 ascites) in 102/136 in GROUP I (SAFI±T) and 23/94 in GROUP II (p < 0.05). In GROUP I there was significant weight loss (9.9 ± 3.1kgs) vs 2.1± 0.9 kgs in GROUP II (p = 0.01) and a significant increase in urine sodium from admission UNa+ (A) of 33.3 ± 22 to a maximum of 244 ± 116 mmol/24 hours, compared to GROUP II where UNa+ (A) of 36.6 ± 24 increased to 54 ± 21mmol/24 hours (P <0.05). The duration of therapy and hospital admission was shorter, 15 ± 3 days, in GROUP I compared to 23 ± 5 days in GROUP II (p < 0.05). Renal artery resistive index was significantly lower after SAFI(T) therapy (0.82 to 0.74) (p < 0.05). The MAP in GROUP I increased from 76 ± 14.5 to 83 ± 22.8mm Hg (p < 0.05) and in GROUP II from 83 to 85 mmHg (p > 0.05) (Table 1). There was a significant improvement in serum creatinine in GROUP I as compared to GROUP II (Table 1). There was a significantly lower incidence of secondary/hospital-acquired infection in GROUP I as compared to GROUP II (p = 0.05) (Table 1).
Addition of Terlipressin in GROUP I (SAFIT): 48 patients achieved UNa+>80 mmol/day with SAFI while 88 required the addition of Terlipressin after 48 hours. These had higher MELD score (31.7 ± 7.1 vs 29.7 ± 7.0; P < 0.05), creatinine (1.75 ± 1.1 vs 1.3 ± 0.8; p >0.05) and mean number of organ failures (2 ± 1.1 vs 1.8 ± 1.1; P = 0.5). All patients responded partially or completely (urinary Na+ >80 mmol/d) to the addition of Terlipressin (Table 2). More than 90% of the patients who attained UNa+ >80 mmol/d within 96 hours, survived compared to 28.6% who took more than 96 hours vs no survivors who could not achieve UNa+ of 80 mmol/d within 7 days (Table 3). The median dose of albumin was 40g/d (20–40g/d), Terlipressin 3mg/d (1–4mg/d), Furosemide 8.3mg/hr (3.3 to 12.5mg/hr). The survival was not significantly different between SAFI vs SAFIT (Figure 2C).
 |
Table 2 Comparison of Organ Failures and Biochemical Parameters in Patients Receiving SAFI vs SAFIT Therapy |
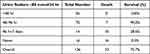 |
Table 3 Time Taken to Attain Urine Sodium ≥80mmol/24hr and Its Relationship with Survival in GROUP I |
Adverse event: GROUP I had an increased incidence of diarrhea (n = 17) in the Terlipressin group requiring discontinuation of treatment (n = 2) and dose reduction in others. Four patients in GROUP I developed scrotal gangrene. New onset or worsening of HE was seen in 11 (GROUP I) vs 23 patients in GROUP II (p < 0.05). The incidence of UGI bleed was also significantly lower in GROUP I (4 vs 13) (p < 0.05) (Table 1).
Mechanistic Cohort
Baseline clinical profile, hematological, laboratory, and systemic hemodynamic parameters of 40 patients with ACLF are shown in Supplementary tables (Supplementary file 1, Supplementary Tables 1 and 2) along with differences between survivors and non-survivors.
Survival: Among 40 patients with ACLF, 11 (28%) expired within 28 days of admission, and a survival rate of 29/40 (72%). Overall, 34/40 patients achieved urinary sodium >80mmol/24 hours (within 7 days) and achieved rapid diuresis during the therapy, and 31 completely mobilized ascites. Laboratory parameters including gut permeability, endotoxemia, serum cytokines, neutrophil dysfunction, and hemodynamic alterations are presented in Supplementary file 1 (Supplementary Tables 3 and 4). There was a linear correlation between serum endotoxin levels and intestinal permeability (R2Linear 0.719) (Supplementary file 1, Supplementary Figure 1). There was no difference in frequencies of infection at the time of admission between survivors and non-survivors but during hospitalization increased incidence of infection was found in non-survivors. (Supplementary file 1, Supplementary Table 5 and 6). Patients who had ascites mobilization showed marked improvement in hemodynamics and survival (Supplementary file 1, Supplementary Table 7 and 8).
Discussion
In the observation cohort, patients of ACLF managed with SAFI±T/NAdr (GROUP I) protocol targeting higher natriuresis, increased urine output, ascites mobilization, and improved SVR, RARI, and renal functions had better 28-day survival with a shorter mean duration of treatment. There was a lesser incidence of in-hospital infections. Similar results were replicated in the mechanistic cohort along with improvement in splanchnic and peripheral hemodynamics, gut permeability, endotoxemia, pro-inflammatory cytokines, and NETosis, indicating an association between ascites mobilization and improved pathophysiologic dysfunctions.
Ascites in ACLF is difficult to mobilize especially with worsening renal functions, and inadequate response to diuretics, HE, or multi OFs. Overall ≥2 OF have high rates of mortality.4 Ascites is a consequence of worsening of systemic hemodynamics as inflammation (hepatic and extrahepatic insults) perpetuates a vicious cycle of increased HVPG, gut congestion and increased intestinal permeability (IIP), splanchnic vasodilation with decreased effective arterial blood flow, increased RAAS, SNS stimulation then renal vasoconstriction ultimately leading to hypovolemia-induced renal dysfunction.27,28 The principle behind the SAFIT/NAdr therapy was response-guided low dose continuous infusions acting synergistically, thereby leading to volume expansion and splanchnic and systemic vasoconstriction improving EABV and RARI, thereby improving diuresis irrespective of AKI-HRS. Fluid mobilization helped to decongest the bowel and improved hemodynamics, IP, neutrophil functions, and reduction in pro-inflammatory cytokines. ACLF patients are not only hypoalbuminemic but also had dysfunctional albumin in circulation.29,30 Hence, slow albumin-furosemide combined infusion appears to achieve plasma volume expansion, optimal furosemide delivery, and action, and consequently good natriuresis and ascites mobilization in fluid overloaded, hypoalbuminemic patients, with decreased urine output.
An association between RARI and cirrhosis severity has been reported.31 There is a positive correlation of RARI with MELD, MELD-Na+ and CTP scores and a negative one with serum albumin and sodium. RARI ≤ 0.70 had a higher median GFR than those with RARI > 0.7.32 Slow continuous volume expansion with simultaneous use of a combination of vasoconstrictors; Terlipressin (splanchnic vasoconstriction) and Noradrenaline (via antagonism of alpha-1, −2 receptors, increase SVR)-improves EABV, thereby tips the renal blood flow balance. This helps in overcoming the furosemide resistance due to improvement in ECF volume and GFR.33 Aggressive diuresis ensues, achieving UNa+ >80mmol/day. The rapidity of improvement of UNa+ correlates with survival in this study. Rapid improvement, within 7 days, in UNa+ may be a surrogate marker for improved renal perfusion and outcome akin to the so-called “golden window” period.34
There are pieces of evidence suggesting immune paralysis in patients with ACLF.35–37 Patients are predisposed to infection due to inefficient immune cell function and IIP.38 Earlier it has been reported that ex vivo removal of endotoxin from patients’ plasma increased the phagocytic function of neutrophils,39 and that neutrophil phagocytic capacity and resting oxidative burst was predictive of survival at 90 days in ACLF.40 In the present study we observed that NETosis at baseline was very low when compared to healthy subjects however, it increased after ascites mobilization.
Studies have reported that both stable and decompensated cirrhotic patients have increased pro- and anti-inflammatory cytokine levels (IL-6, IL-7, IL-8, IL-10, IL 12, and TNF-α).41 A survival benefit of the removal of cytokines by plasma exchange was reported.9 In ACLF and decompensated cirrhosis altered hemodynamics depend upon a mix of plasma oncotic pressure, splanchnic and systemic vasodilatation which results in an increased inflammatory state and low GFR. For a favorable outcome, each of these altered pathophysiological mechanisms needs to be addressed simultaneously. Once plasma oncotic pressure is increased by parenteral albumin infusions, there is a need to mobilize excess fluid by using diuretics, to reduce complications like pulmonary edema. Vasoconstrictors like Terlipressin/NAdr help in counteracting splanchnic and systemic vasodilatation and improve arterial perfusion and GFR but also reduce HVPG and the risk of variceal bleed. Due to varying degrees of severity of hemodynamic alterations, targeting only a single component-like plasma albumin (≥3g/dl) as in the ATTIRE Trial may have led to partial improvement in hemodynamics but in absence of adequate diuresis resulted in increased frequency of pulmonary edema.42 Aiming for higher dose correction of plasma albumin as in the ANSWER trial did reduce the need for paracentesis and lowered the incidence of SBP, AKI, HRS, refractory ascites, and potential diuretics-induced side effects.43 This probably is due to improved hemodynamics and GFR, especially in those achieving higher serum albumin (4g/dl) as shown in the post hoc analysis. Our choice of targeting serum albumin level to 4 g/dl was based on previous experience in our unit where in-patients having a serum albumin level at or above 4 g/dl had better survival (unpublished observation), a fact supported by post hoc analysis of ANSWER trial and by Wang et al.44 Similar to our study, Terlipressin with albumin was reported to be better in reversing HRS, as compared to Placebo with albumin, with a presumed beneficial effect in reducing portal pressure and consequently decreased gut congestion, endotoxemia, and reduced pro-inflammatory cytokines.45 The merit of our study is that we have demonstrated the benefit of response-guided SAFI±T/NAdr therapy on survival through improved hemodynamics, cytokines, and Netosis (Figure 3). However, multicentric studies are needed to validate the findings of our study.
Strength and Limitations
The strength of our study is that this is the only study that assessed survival, hemodynamics, intestinal permeability, endotoxin levels, systemic inflammatory markers, and neutrophil dysfunction with ascites and after ascites mobilization in ACLF patients.
The limitations of our study are open-label, observational, non-randomized design, and single-center study. Inflammatory markers, IP, and neutrophil function were done only twice (baseline and after ascites mobilization). Additionally, hemodynamic measurements were carried out in a cohort of patients receiving SAFI-T/NAdr only not in the ones on SMT. The patients requiring ventilator support were shifted to ICU, managed by critical care physicians, and thus excluded from the study.
Conclusion
To conclude, response-guided SAFI±T/NAdr improves survival in ACLF patients by mobilizing ascitic fluid by increasing natriuresis, improving splanchnic circulation, reducing gut congestion, permeability, and endotoxemia and improving neutrophil functions, and reduction in pro-inflammatory cytokines.
Data Sharing Statement
Study materials and data related to the study are available with the corresponding author and will be made available to other researchers on reasonable request.
Funding
Intramural grant (A-18-PGI/IMP/75/2017) of Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow.
Disclosure
All authors disclose that they have no conflicts of interest.
References
1. Sarin SK, Choudhury A. Acute-on-chronic liver failure: terminology, mechanisms, and management. Nat Rev Gastroenterol Hepatol. 2016;13(3):131–149. doi:10.1038/nrgastro.2015.219
2. Garg H, Kumar A, Garg V, et al. Hepatic and systemic hemodynamic derangements predict early mortality and recovery in patients with acute-on-chronic liver failure. J Gastroenterol Hepatol. 2013;28:1361–1367.
3. Hernaez R, Solà E, Moreau R, Ginès P. Acute-on-chronic liver failure: an update. Gut. 2017;66:541–553.
4. Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144:1426–1437.
5. Chen Y, Guo J, Qian G, et al. Gut dysbiosis in acute-on-chronic liver failure and its predictive value for mortality. J Gastroenterol Hepatol. 2015;30:1429–1437.
6. Cariello R, Federico A, Sapone A, et al. Intestinal permeability in patients with chronic liver diseases: its relationship with the aetiology and the entity of liver damage. Dig Liver Dis. 2010;42:200–204.
7. Sen S, Davies NA, Mookerjee RP, et al. Pathophysiological effects of albumin dialysis in acute-on-chronic liver failure: a randomized controlled study. Liver Transplant. 2004;10:1109–1119.
8. Mookerjee RP, Sen S, Davies NA, Hodges SJ, Williams R, Jalan R. Tumour necrosis factor alpha is an important mediator of portal and systemic haemodynamic derangements in alcoholic hepatitis. Gut. 2003;52:1182–1187.
9. Clària J, Stauber RE, Coenraad MJ, et al. Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology. 2016;64:1249–1264.
10. Mookerjee RP, Stadlbauer V, Lidder S, et al. Neutrophil dysfunction in alcoholic hepatitis superimposed on cirrhosis is reversible and predicts the outcome. Hepatology. 2007;46(3):831–840. doi:10.1002/hep.21737
11. Markwick LJ, Riva A, Ryan JM, et al. Blockade of PD1 and TIM3 restores innate and adaptive immunity in patients with acute alcoholic hepatitis. Gastroenterology. 2015;148(3):590–602.e10. doi:10.1053/j.gastro.2014.11.041
12. Martin-Mateos R, Alvarez-Mon M, Albillos A. Dysfunctional immune response in acute-on-chronic liver failure: it takes two to tango. Front Immunol. 2019;10:973.
13. Lodato F, Berzigotti A, Lisotti A, et al. Transjugular intrahepatic portosystemic shunt placement for refractory ascites: a single-centre experience. Scand J Gastroenterol. 2012;47:1494–1500.
14. Lautt WW. Hepatic Circulation: Physiology and Pathophysiology. San Rafael (CA): Morgan & Claypool Life Sciences; 2009.
15. Baik SK, Jeong PH, Ji SW, et al. Acute hemodynamic effect of octreotide and terlipressin in patients with cirrhosis: a randomised comparison. Am J Gastroenterol. 2005;100:631–635.
16. Runyon BA. Refractory ascites. Semin Liver Dis. 1993;13:343.
17. Jackson EK. Drugs affecting renal excretory function. In: LL Brunton, editor. Goodman & Gilman’s the Pharmacological Basis of Therapeutics.
18. Inoue M, Okajima K, Itoh K, et al. Mechanism of furosemide resistance in analbuminemic rats and hypoalbuminemic patients. Kidney Int. 1987;32:198–203.
19. Schetz M. Loop diuretics. In: Ronco C, Bellomo R, Kellum. JA, editors. Critical Care Nephrology. Saunders; 2008:547–551.
20. Ilyas A, Ishtiaq W, Assad S, et al. Correlation of IVC diameter and collapsibility index with central venous pressure in the assessment of intravascular volume in critically ill patients. Cureus. 2017. 9: e1025.
21. Zhang Z, Xu X, Ye S, Xu L. Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: systematic review and meta-analysis. Ultrasound Med Biol. 2014;40:845–853.
22. Mindikoglu AL, Dowling TC, Wong-You-Cheong JJ, et al. A pilot study to evaluate renal hemodynamics in cirrhosis by simultaneous glomerular filtration rate, renal plasma flow, renal resistive indices and biomarkers measurements. Am J Nephrol. 2014;39:543–552.
23. Szabó M, Bozó A, Darvas K, Horváth A, Iványi ZD. Role of inferior vena cava collapsibility index in the prediction of hypotension associated with general anesthesia: an observational study. BMC Anesthesiol. 2019;19:139.
24. EASL Clinical Practice. Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406–460.
25. Harrison PM. Management of patients with decompensated cirrhosis. Clin Med. 2015;15:201–203.
26. Pudil R, Pelouch R, Praus R, Vašatová M, Hůlek P. Heart failure in patients with liver cirrhosis. Cor Vasa. 2013;55:e391–396.
27. Kumar A, Das K, Sharma P, Mehta V, Sharma BC, Sarin SK. Hemodynamic studies in acute-on-chronic liver failure. Dig Dis Sci. 2009;54:869–878.
28. Spinella R, Sawhney R, Jalan R. Albumin in chronic liver disease: structure, functions and therapeutic implications. Hepatol Int. 2016;10:124–132.
29. Oettl K, Birner-Gruenberger R, Spindelboeck W, et al. Oxidative albumin damage in chronic liver failure: relation to albumin binding capacity, liver dysfunction and survival. J Hepatol. 2013;59:978–983.
30. Fliser D, Zurbrüggen I, Mutschler E, et al. Coadministration of albumin and furosemide in patients with the nephrotic syndrome. Kidney Int. 1999;55(2):629–634.
31. Koda M, Murawaki Y, Kawasaki H. Renovascular resistance assessed by color Doppler ultrasonography in patients with chronic liver diseases. J Gastroenterol Hepatol. 2000;15:1424–1429.
32. Onwuka CC, Ayoola OO, Adekanle O, Famurewa OC, Abidoye IA. Renal arterial resistance index among subjects with liver cirrhosis in a Nigerian population. J Clin Ultrasound. 2021;49:538–545.
33. Wilcox CS, Testani JM, Pitt B. Pathophysiology of diuretic resistance and its implications for the management of chronic heart failure. Hypertension. 2020;76:1045–1054.
34. Choudhury A, Kumar M, Sharma BC, et al. Systemic inflammatory response syndrome in acute on chronic liver failure- relevance of ‘Golden Window’- A prospective study. J Gastroenterol Hepatol. 2017;32:1989–1997.
35. Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385–1396.
36. Sipeki N, Antal-Szalmas P, Lakatos PL, Papp M. Immune dysfunction in cirrhosis. World J Gastroenterol. 2014;20:2564–2577.
37. Tiegs G, Lohse AW. Immune tolerance: what is unique about the liver. J Autoimmun. 2010;34:1–6.
38. Jalan R, Fernandez J, Wiest R, et al. Bacterial infections in cirrhosis: a position statement based on the EASL special conference 2013. J Hepatol. 2014;60:1310–1324.
39. Panasiuk A, Wysocka J, Maciorkowska E, et al. Phagocytic and oxidative burst activity of neutrophils in the end stage of liver cirrhosis. World J Gastroenterol. 2005;11:7661–7665.
40. Makkar K, Tomer S, Verma N, et al. Neutrophil dysfunction predicts 90-day survival in patients with acute on chronic liver failure: a longitudinal case-control study. JGH Open. 2020;4:595–602.
41. Wasmuth HE, Kunz D, Yagmur E, et al. Patients with acute on chronic liver failure display “sepsis-like” immune paralysis. J Hepatol. 2005;42:195–201.
42. China L, Freemantle N, Forrest E, et al.; ATTIRE Trial Investigators. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384(9):808–817.
43. Caraceni P, Tufoni M, Zaccherini G, et al.; ANSWER Study Investigators. On-treatment serum albumin level can guide long-term treatment in patients with cirrhosis and uncomplicated ascites. J Hepatol. 2021;74(2):340–349.
44. Wang Z, Xie YW, Lu Q, et al. The impact of albumin infusion on the risk of rebleeding and in-hospital mortality in cirrhotic patients admitted for acute gastrointestinal bleeding: a retrospective study of a single institute. BMC Gastroenterol. 2020;20(1):198.
45. Wong F, Pappas SC, Curry MP, et al.; CONFIRM Study Investigators. Terlipressin plus albumin for the treatment of type 1 hepatorenal syndrome. N Engl J Med. 2021;384(9):818–828.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


