Back to Journals » Psychology Research and Behavior Management » Volume 16
Repercussions of Pandemic and Preventive Measures on General Well-Being, Psychological Health, Physical Fitness, and Health Behavior: Mediating Role of Coping Behavior
Authors Fan X, Menhas R , Laar RA
Received 28 March 2023
Accepted for publication 24 June 2023
Published 3 July 2023 Volume 2023:16 Pages 2437—2454
DOI https://doi.org/10.2147/PRBM.S405273
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Xin Fan,1 Rashid Menhas,2 Rizwan Ahmed Laar1
1College of Physical Education, Hubei Normal University, Huangshi, 435002, People’s Republic of China; 2Research Center of Sports Social Sciences, College of Physical Education and Sports, Soochow University, Suzhou, Jiangsu Province, People’s Republic of China
Correspondence: Rashid Menhas, Research Center of Sports Social Sciences, College of Physical Education and Sports, Soochow University, Suzhou, Jiangsu Province, People’s Republic of China, Email [email protected] Rizwan Ahmed Laar, College of Physical Education, Hubei Normal University, Huangshi, 435002, People’s Republic of China, Email [email protected]
Background: Pandemic prevention measures increased physical inactivity due to travel restrictions that led to negative physical fitness, health behavior, psychological health, and general well-being. The mediating role of coping behavior must be identified before developing interventional strategies for this pandemic.
Objective: The study investigates the mediating role of coping behavior to mitigate the Coronavirus disease impact on physical fitness, health behavior, psychological health, and general well-being.
Methods: A web-based survey was used under convenience sampling to collect the primary data. Smart-PLS 3.0 was used to analyze the collected data.
Results: All 14 direct correlations (H1-H14) were correct, and coping behavior’s mediating impact was shown to be statistically significant (H9a- H14d).
Conclusion: Our study findings indicate that mediating role of coping behavior in mitigating the pandemic impacts was statistically significant. It is concluded that coping behavior is a healthy adaptation to protecting the barrier against COVID-19 adverse effects on health.
Keywords: COVID-19, lockdown, impact, strategies
Introduction
Numerous nations employed proactive and preventative measures, including population home confinement.1,2 It is widely agreed that the COVID-19 pandemic has psychological and emotional repercussions and that we must prepare for the subsequent epidemic of mental and behavioral illnesses.3,4 Recent research explored the mental, sociological, and neuroscientific aspects of COVID-19 and put forth urgent objectives and longer-term initiatives for mental health.5–8 The prevalence of sleep disruptions was higher among females and those with chronic illnesses.9–13 Studies discovered the worldwide prevalence of anxiety and its correlation with P.A. and related deficiencies in social ties, as indicated by apparent social loneliness with unfavorable health and fitness effects at each developmental stage of life.14,15 In addition, studies also show that a lack of exercise and activities and limited social connections are linked to severe sleep issues and psychological illnesses. Confinement and extended inactivity pose several health hazards and may lead to depression.16,17
Preventative interventions affect physical activity and well-being to generate insights for successful COVID-19 response and reveal gaps.18,19 COVID-19 epidemic research examines social and edifying impacts on behavior, scientific statement, ethical decision-making, direction, and stress and coping with determining the incidence of acute stress disorder and the determinants of psychological distress.20,21 Individuals endure heightened psychological distress during the COVID-19 pandemic. However, it’s uncertain whether COVID-19 influences are coping techniques beyond established pre-dictions to examine COVID-19-related psychological discomfort among Southern Germans and their coping techniques.22,23 As the COVID-19 epidemic spreads, it is critical to identify the coping methods connected with unfavorable psychosocial outcomes.24 Healthcare providers, such as physicians and nurses, are also facing mental health problems.3,4
Coping is how a person adapts to, or at least attempts to adapt to, a stressful situation or event. Depending on their focal point, coping theories may be organized differently.25 The effects of stress on one’s body and mind might be better understood if one has a firm grasp of how individuals typically deal with adversity. But there is little consensus on the structure of coping, with at least a hundred coping taxonomies and 400 lower-order categories offered in the literature.26 As a public health paradigm, health-related quality of life considers not only one’s physiological but also one’s mental and social health and fitness level.27 Self-compassion and acceptance in the face of frustration with one’s ability to find a solution are essential to good emotional coping.
The recent COVID-19 pandemic has had significant impacts on the global population, including physical health and general well-being, psychological health,3,4 physical fitness,27 and the health behavior of individuals.1 However, limited research has explored the interplay between these factors and the mediating role of coping behavior in the context of the pandemic and preventive measures. While the pandemic has resulted in widespread stress and anxiety,2 it has also led to changes in health behaviors,1 such as changes in physical activity levels,27 dietary habits, and substance use. These changes have significant impacts on physical health and fitness. Similarly, the impact of the pandemic and preventive measures on health behaviors, such as vaccine uptake, health screening behaviors, and medication adherence, is poorly understood. While these behaviors are critical to maintaining health and preventing the spread of disease, they are also influenced by a complex array of psychological, social, and cultural factors. The study investigates the mediating role of coping behavior to mitigate the Coronavirus disease impact on physical fitness, health behavior, psychological health, and general well-being. The pandemic, along with preventive measures, impact on the general well-being, psychological health, physical fitness, and health behavior of individuals is a complex and multifaceted phenomenon that requires further research to fully understand.
Literature Review
Theoretical Framework
The theoretical framework of the study is based on the protection motivation theory (PMT).28 PMT suggests that individuals are motivated to engage in preventive health behaviors when they perceive a threat and have the resources to respond to that threat.29 In the context of the pandemic, PMT can help to explain why some people may be more likely to engage in preventive behaviors (such as wearing masks and practicing physical distancing) if they perceive a high level of threat from the virus and believe that these behaviors can help to reduce their risk of exposure.30 A person’s coping behavior is crucial when dealing with challenging crisis circumstances. In the process, a threat and coping appraisal is triggered to determine the emotional and cognitive steps a person takes to get through challenging conditions and adjust to the current situation, which is an example of coping behavior.31 According to experts, the coping strategies used by individuals might differ during different times.32 The health theory of coping classifies coping mechanisms as either healthy or unhealthy, acknowledging that all coping behaviors are adaptive or may, at first, lessen suffering.33 This study’s objective is to investigate the mediating role of coping behavior to mitigate the Coronavirus disease impact on physical fitness, health (physical and psychological), and general well-being. Our conceptual framework (Figure 1) and study hypotheses were developed based on PMT. We assume people perceive the risk of the pandemic and the preventive measures of public health that impact people’s physical fitness, health (physical and psychological), and general well-being. Through the emotional and coping appraisal, coping behavior forms that will affect the outcomes of the above three perspectives produced by pandemic and preventive measures.
 |
Figure 1 Conceptual Framework. |
Operationalization of the Study Hypotheses
Direct Hypotheses
Pandemic, Health Behavior, Physical Fitness, Psychological Health, and General Well-Being
The pandemic has brought about significant changes in health behaviors, including increased hand washing and sanitization, physical distancing, and mask-wearing. The lockdown measures have also led to the reduction of physical activity and sedentary behaviors such as prolonged screen time, which can have negative impacts on health.34–36 The reduction in physical activity has negatively impacted physical health, with some people gaining weight, experiencing decreased cardiovascular fitness, and experiencing decreased muscle strength and endurance. The fears of contracting the virus, the stress of quarantine measures, and the uncertainty of the future have increased anxiety, depression, and stress.37–40 In addition, the reduction in physical activity levels and the increase in sedentary behaviors have negatively impacted overall health and well-being.28 The following hypotheses were proposed according to the conceptual framework of the study;
H1: The pandemic impacted health behaviors negatively H2: The pandemic impacted physical fitness negatively H3: The pandemic impacted psychological health negatively H4: The pandemic impacted general well-being negatively
Preventive Measures, Health Behavior, Physical Fitness, Psychological Health, and General Well-Being
The pandemic, along with social distancing, lockdowns, and travel restrictions, has caused significant changes in health behaviors.41,42 For instance, many people have started practicing good hand hygiene, wearing masks, and avoiding large gatherings, which are essential in reducing the spread of the virus.28 On the other hand, a decline in physical fitness levels and a significant increase in sedentary behaviors. Additionally, many people have reported difficulty maintaining a healthy diet and weight management, negatively impacting physical health. People are experiencing depression, anxiety, and stress due to uncertainty, fear of infection, financial insecurity, and loss of social connection.43 In addition, People have reported a decline in overall life satisfaction and happiness due to the loss of freedom, routine, and structure. The following hypotheses were proposed according to the conceptual framework of the study;
H5: Preventive measures impacted health behaviors negatively H6: Preventive measures impacted physical fitness negatively H7: Preventive measures impacted psychological health negatively H8: Preventive measures impacted general well-being negatively
Coping Behavior, Health Behavior, Physical Fitness, Psychological Health, and General Well-Being
Coping behavior refers to the various strategies an individual uses to manage stress, challenges, or difficult situations in their life. It is a key aspect of mental and physical health and overall well-being.44 Individuals who engage in healthy coping mechanisms such as exercise, mindfulness, or social support may be more likely to maintain good health. Coping mechanisms such as seeking social support, practicing mindfulness, or engaging in physical activity may experience improved psychological health.45 Healthy coping mechanisms can help individuals manage stress, improve physical fitness, maintain good psychological health, and experience greater overall well-being.46 The following hypotheses were proposed according to the conceptual framework of the study;
H9: The pandemic impacted coping behavior negatively. H10: Coping behavior impacted health behavior positively H11: Coping behavior impacted physical fitness positively H12: Coping behavior impacted psychological health positively H13: Coping behavior impacted general well-being positively H14: Preventive measures impacted coping behavior negatively.
Mediating Hypotheses
Pandemic, Preventive Measures, and Coping Behavior
The outbreak of a pandemic, such as COVID-19, can cause significant stress and disrupt daily life. In response, health organizations and governments often implement preventive measures to slow the spread of the virus.47,48 These measures can also significantly impact individuals, as they often involve changes to daily routines and the disruption of normal social and economic activities. Individuals need to adopt healthy coping behaviors.49,50 It can include engaging in physical activity, connecting with loved ones through technology, practicing mindfulness and stress-reduction techniques, and seeking support from mental health professionals if needed. The relationship between pandemics, preventive measures, and coping behavior is complex and multifaceted.51 The following hypotheses were proposed according to the conceptual framework of the study;
H9a: The relationship between pandemic and health behaviors is positively mediated by coping behavior H9b: The relationship between the pandemic and physical fitness is positively mediated by coping behavior H9c: The relationship between the pandemic and psychological health is positively mediated by coping behavior H9d: The relationship between the pandemic and general well-being is positively mediated by coping behavior H14a: The relationship between preventive measures and health behaviors is positively mediated by coping behavior H14b: The relationship between preventive measures and physical fitness is positively mediated by coping behavior H14c: The relationship between preventive measures and psychological health is positively mediated by coping behavior H14d: The relationship between preventive measures and general well-being is positively mediated by coping behavior
Materials and Methods
Study Design
A cross-sectional research design was used in the current study. The two Chinese cities where the present research was carried out were Shanghai, a financial hub of China, and Shenzhen, the city in the Guangdong province. Both cities were selected conveniently. The research adhered to the World Medical Helsinki Policy requirements and was approved by the ethics committee of Soochow University. An informed consent was obtained from the study participants before final data collection after telling them the study purpose and assuring them that their responses were used only for research purposes.
Participants
The study population consisted of (+21) people from Shanghai and Shenzhen who were isolated from home.
Questionnaire Development
A deductive (top-down) methodology and rational approach were used to create a questionnaire. The top-down method examines the literature to locate existing items or create new items based on previously-established theories.52 The rational approach was used as a standardized procedure after developing the items/constructs to refine the multi-item questionnaire.53 The rational method for questionnaire development is based upon eight steps; theoretical framework, concept analysis, item specification, item production, item judgment, scale construction, validation, and comment.54 A rationally designed questionnaire’s theoretical foundation is mainly given mostly by the constructor’s concepts of the subject. The target audience or specialists’ knowledge is typically used to create the subject standards. The concept’s/item’s typological specification is the distinguishing feature of the rational method. The target audience or specialists’ knowledge is typically used to create the subject standards. A team of six public health professionals examined the preliminary multi-item questionnaire under the rational method. Two independent translators translated (forward and backwards) the questionnaire from its original language to the targeted one.55
Data Collection
The data was collected using a convenience sampling technique by delivering an online survey in both locations. The data collection tool was pretested both in Shanghai and Shenzhen. Specific questionnaire questions were changed and modified after pretesting to acquire the most significant response rate from the research participants. Final data collection was held online from June 16 to September 30, 2022. A total of 3100 individuals were recruited to participate in the anonymous online survey. Among 997 were not eligible according to study inclusion criteria. A total of 2297 participated in the anonymous online survey. About 97 survey respondents’ answers were excluded after the data quality check. The answers of 2200 participants were included in the final analysis.
Data Analysis
Structural equation modeling techniques were employed for data analysis using the Smart-PLS 3.0.56,57 The study hypotheses were tested by using SEM techniques.58,59 Mediation analysis uses a mediator variable to divide the overall exposure-outcome relationship into direct and indirect effects.60
Results
Descriptive Statistics
Table 1 shows the demographic characteristics of the study participants. The majority (29.77%) of the study participants were 21–27 years old, about (24.72%) were 36–43 years old, about (19.04%) were 28–35 years old, while about (16.77%) were 44–51 years old, and about (9.68%) were 52+ years old according to the age statistics. The majority (55.55%) were male, and about (44.45%) were female participants. Marital status statistics show that the majority (45.68%) were single, about (45.04%) were married, about (4.72%) were divorced, and about (4.54%) were widowed. The educational context shows that the majority (29.45%) were bachelor’s degree holders, about (23.40%) were undergraduate, about (23.27%) were graduate, about (17.95%) were master’s degree holders, and about (5.91%) were others.
 |
Table 1 Background Information of the Study Participants (N=2200) |
Table 2 depicts the study constructs’ mean scores, standard deviation, excess kurtosis, and skewness values. It has been proven that all of the scales employed in this inquiry to determine the mean scores, standard deviation, excess kurtosis, and skewness values were consistently “reliable” and produced satisfactory results.
 |
Table 2 Mean, Standard Deviation, Kurtosis, and Skewness of the Study Constructs |
Factor Analysis
For factor analysis was performed by evaluating the convergent validity, discriminant validity, and scale reliability. In Table 3, for scale reliability, we utilized Cronbach’s Alpha (C.A.) and composite reliability (C.R.), both of which were above the 0.70 thresholds, ranging from (0.823 to 0.966) and (0.876 to 0.975), respectively. Convergent validity was examined by calculating each scale item’s factor loadings (F.L.) and the average variance extracted (AVE). Results show that every item’s loading was larger than 0.6, and the AVE of every construct was greater than 0.5 (See Table 3).
 |
Table 3 Factor Analysis |
Discriminant Validity: Fornell Lacker and Hetero Trait-Mono Trait
As a first step in establishing discriminant validity, Fornell Lacker was validated. One of the constructs’ AVE square root values must be greater than its inter-correlation value. A construct’s components must exhibit more variation to be considered distinct from the other constructs (See Table 4).
 |
Table 4 Discriminant Validity: Fornell Larcker |
Regarding discriminant validity, we applied the Heterotrait-Monotrait Ratio (HTMT) approach, which checks discriminant validity among each pair of variables. Table 5 shows that the HTMT values are less than the 0.90 requirements.
 |
Table 5 Hetro Trait-Mono Trait (HTMT) Discriminant Validity |
Model Fitness
Before employing structural equation modeling (SEM), the fitness model was examined (See Table 6). A model fitness criterion is based on standardized root mean square residual (SRMR), the geodesic distance (d_G), the squared euclidean distance (d_ULS), chi-square, and normed fit index (NFI) values. The structural model provides a concrete foundation for the establishment of structural equations which assess the inner route model. The critical metrics used to analyze this work’s structural model were the endogenic variable’s coefficient of determination, path coefficient, prediction significance, effect size, and multicollinearity. Table 6 of the structural model beneath gives each benchmark’s beginning value and explanation.
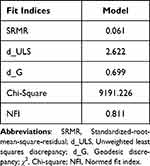 |
Table 6 Model of Fitness |
Hypothesis Testing
Table 7 and see (Figure 2) show the results regarding our direct hypotheses. All 14 direct correlations (H1: t= 10.283, p=0.000; H2: t= 10.101, p= 0.000; H3: t=11.015, p=0.000; H4: t= 7.531, p=0.000; H5: t= 2.732, p=0.010; H6: t= 5.881 p=0.000; H7: t= 2.82, p=0.010; H8: t=7.824 p= 0.000; H9: t= 9.383, p=0.000; H10: t=17.503, p=0.000; H11: t=10.947 p=0.000; H12: t=16.789 p=0.000; H13: t= 21.715, p=0.000 and H14: t= 11.967 p=0.000) were accurate. Table 7 includes all the associations that have been established.
 |
Table 7 Direct Hypotheses |
 |
Figure 2 Factor loadings, path coefficient, and R-square result (PLS-Algorithm). |
Additionally, the coping behavior’s mediating impact was shown to be statistically significant in the mediating paths. Table 8 exhibits the mediating impact both in terms of direct and indirect effects.
 |
Table 8 Mediating Hypotheses |
Discussion
People often evaluate their coping skills (as an internal resource) and assess the severity of an experience (secondary appraisal). It is up to the individual to choose how much influence they have on the situation and what they should do about it based on their current coping resources.61 A person’s coping behavior is the set of measures they take to better manage their emotional and psychological well-being in the face of adversity. Within positive psychology and cognitive psychology, the contextual model’s coping theory has the widest acceptance and application.62 Cognitive strategies like acceptance, distance, and escape attempts try to improve one’s mental state. In contrast, behavioral strategies like obtaining additional information and evidence and addressing people are made to alter the situation directly.63 Several research conducted during the global COVID-19 epidemic evaluated the mental health of middle-aged and older persons, their related variables, and the possible mediating role of coping methods.35,64
People’s mental health and quality of life suffer from the COVID-19 epidemic. Still, few studies have studied how to deal with these consequences healthily, and 14 coping techniques were assessed to see whether there was any correlation.65 The psychological well-being of older persons living in the Japanese community was linked to exercise as a health-promoting coping behavior during the stay-at-home order, with varying effects depending on the activity type. People who walked for health reported better levels of psychological well-being than those who did not exercise.66 COVID-19 disease stressors have been linked to various coping strategies in previous research.67,68 COVID-19-related stress and coping methods were explored among adults with chronic disease who reported domestic and international perceived stress levels and examined their coping techniques’ mediation effect in the pandemic’s early phases.69 Previous studies looked at stress levels, coping mechanisms, and substances during the continuing COVID-19 epidemic to see if they predicted a shift in subjective well-being. They also looked at lifestyle choices and coping techniques.69–71 Our findings indicate that positive coping behavior has a positive association with physical and psychological health, physical fitness, and overall well-being, while the lockdown policy of COVID-19 has a negative influence.
Similarly, it is reported that the COVID-19 lockdown restrictions have negative impacts on physical activity, mental health, and associated lifestyle behaviors. Another study reported that social isolation adversely impacts physical activity and particular well-being (SWB) throughout the COVID-19 pandemic. It severely threatens human society regarding health, economy, and lifestyle.72–74 Our findings show that the physical activity trend has a negative association with pandemic preventive measures, while positive coping behavior positively influences physical activity for overall well-being. Similar studies addressed social isolation obstacles globally—examining how exercise affects self-perception and self-esteem. Exercise may improve people’s mental health and quality of life by boosting their self-esteem.75,76
Closure to COVID-19 showed some encouraging impacts on self-reported mental health immediately after exercise in nature.77,78 In light of the present crisis, there is a compelling medical argument in favor of regular physical exercise performed at home to stay healthy and keep the immune system functioning normally.38,79 Understanding how context influences the connection between physical activity and mental health is crucial for tailoring interventions and policy guidelines to maximize positive effects.80,81 People’s well-being output variables usually lack operational definitions, while moderating and mediating factors get little attention in research on the effectiveness of P.A. and exercise as a treatment for most chronic illnesses.82 For this purpose, it may be helpful to examine changes in objectively recorded physical activity (P.A.) and the barriers that prevent them from engaging in physical activity.83–86 Therefore, it is essential to evaluate how the stay-at-home instruction affected P.A. and how it changed apparent P.A. and inactive behavior associated with pre-pandemic and pre-pandemic times. The people of England were told to stay home and only leave for essentials like shopping, health care, work, or exercise to minimize the spread of COVID-19.87 Overall, while the COVID-19 lockdown presented challenges for maintaining physical activity and fitness routines, individuals have found innovative ways to adapt and continue their pursuit of a healthy lifestyle. Regular physical activity during this time has helped individuals maintain their physical fitness and played a significant role in managing stress, improving mental well-being, and boosting overall resilience.88 The COVID-19 lockdown posed physical activity and fitness challenges due to restrictions on facilities and routines. However, it also provided opportunities for individuals to explore alternative forms of exercise, such as home workouts. Virtual platforms and challenges significantly motivated and connected people, fostering a sense of community despite physical distancing. Adapting to these new circumstances, individuals found creative ways to stay physically active and maintain their fitness levels, emphasizing the importance of regular exercise for overall well-being, even in challenging times.89
Study Limitations
Convenience sampling and cross-sectional research design are the main study limitations. Moreover, study participants must be 21+ years old and in home isolation during the Coronavirus disease lockdown. A self-administered questionnaire (five points Likert Scale) was used to collect the primary data, designed after a literature review on SARS and influenza epidemics. We assessed the pandemic (COVID-19) in terms of attitude. General well-being was measured in five dimensions (health behavior, psychological health, active lifestyle, emotional health, and financial stability). In this article, the term “coping behaviors” refers to positive actions taken by individuals in response to stressful COVID-19 preventive measures. Health behavior was measured in terms of regular physical activity, a balanced diet, less smoking and alcohol consumption. The study findings cannot be applied to the entire Chinese society because of the convenience sample.
Conclusion
In conclusion, our study findings provide valuable insights into the repercussions of COVID-19 countermeasures on overall well-being, specifically regarding physical and psychological health and physical fitness. The findings of this study also highlight the significance of addressing coping behavior as a means of mitigating the adverse effects of the pandemic on various dimensions of health and well-being. The implementation of preventive measures during the pandemic has had a negative impact on these aspects of well-being. However, coping behavior has emerged as a positive mediating factor, influencing the emotions of study participants regarding physical fitness and psychological and physical health, thus contributing to their general well-being. One important aspect highlighted in our study is the role of cognitive and behavioral skills as coping strategies in response to the stressful circumstances imposed by the pandemic. These coping strategies serve as tools to reduce the transient unpleasant aspects individuals may experience and improve their perception of personal control. By adopting and employing effective coping strategies, individuals are better equipped to navigate the challenges posed by the pandemic and its associated countermeasures. Furthermore, our study underscores the importance of coping behavior in promoting a sense of personal control and emotional well-being, particularly in relation to physical fitness and psychological and physical health. Adaptive coping behaviors can help individuals maintain a positive outlook, enhance their ability to manage stress, and ultimately contribute to their overall well-being.
Implications of the Study
The findings of this study have significant implications for individuals, healthcare professionals, and policymakers.
Understanding the Role of Coping Behaviour
The study highlights the role of coping behavior in mitigating the negative impact of the pandemic and its preventive measures on general well-being, psychological health, physical fitness, and health behavior. Recognizing the importance of coping strategies can help individuals develop effective ways to deal with the stress and challenges brought about by the pandemic.
Promoting Mental Health and Well-Being
The findings emphasize prioritizing mental health and well-being during the pandemic. Individuals can benefit from learning and adopting coping mechanisms that promote emotional resilience and psychological well-being. Healthcare professionals can be crucial in providing guidance and support in developing healthy coping strategies.
Integrating Physical Fitness into Coping Strategies
Physical fitness is shown to be an essential aspect of coping behavior in the study. Encouraging individuals to engage in regular physical activity can help them cope with stress and contribute to maintaining good physical health. Promoting home-based exercises, outdoor activities with social distancing, and virtual fitness resources can be beneficial.
Enhancing Health Behaviour
The study suggests that coping behavior can mediate the impact of the pandemic on health behavior. This finding underscores the importance of promoting healthy behaviors such as proper nutrition, sleep, and hygiene practices during these challenging times. Health education campaigns and targeted interventions can help individuals adopt and maintain these behaviors to safeguard their health.
Policy Implications
The study findings have implications for policymakers regarding public health interventions and policies. It emphasizes the importance of providing resources and support to individuals to develop and implement effective coping strategies. Policies should prioritize mental health services, access to physical activity resources, and education on healthy behaviors to protect and promote the population’s well-being during and beyond the pandemic.
Future Scope of the Study
Our research opens up future research opportunities to explore the long-term effects of coping behavior on health outcomes beyond the immediate impact of the pandemic. Additionally, there is scope to investigate the effectiveness of coping behavior interventions tailored to different populations, examine cross-cultural and socio-economic factors influencing coping behavior, explore the role of technology-based interventions, address health disparities and vulnerable populations, and assess the policy implications of promoting coping behavior to protect against adverse effects of similar crises on health and well-being.
Acknowledgments
We would like to express our gratitude to all survey respondents. RM is the principal investigator in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Azizi A, Achak D, Aboudi K, et al. Health-related quality of life and behavior-related lifestyle changes due to the COVID-19 home confinement: dataset from a Moroccan sample. Data Brief. 2020;32:106239. doi:10.1016/j.dib.2020.106239
2. Pang Y, Fang H, Li L, Chen M, Chen Y, Chen M. Predictive factors of anxiety and depression among nurses fighting coronavirus disease 2019 in China. Int J Ment Health Nurs. 2021;30(2):524–532. doi:10.1111/inm.12817
3. Yıldırım M, Arslan G, Özaslan A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: exploring the mediating effects of resilience and Coronavirus fear. Int J Ment Health Addict. 2020. doi:10.31234/osf.io/84xju
4. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1). doi:10.1192/j.eurpsy.2020.35
5. O’Connor RC, Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 mental health & well-being study. Br J Psychiatry. 2020;218(6):326–333. doi:10.1192/bjp.2020.212
6. Villani L, Pastorino R, Molinari E, et al. Impact of the COVID-19 pandemic on the psychological well-being of students in an Italian University: a web-based cross-sectional survey. Global Health. 2021;17(1). doi:10.1186/s12992-021-00680-w
7. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi:10.1016/s2215-0366(20)30168-1
8. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
9. Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17(13):4779. doi:10.3390/ijerph17134779
10. Rossi R, Socci V, Talevi D, et al. Covid-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. 2020;11. doi:10.3389/fpsyt.2020.00790
11. Salari N, Hosseinian-Far A, Jalali R, et al. prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1). doi:10.1186/s12992-020-00589-w
12. Antunes R, Frontini R, Amaro N, et al. Exploring lifestyle habits, physical activity, anxiety and basic psychological needs in a sample of Portuguese adults during COVID-19. Int J Environ Res Public Health. 2020;17(12):4360. doi:10.3390/ijerph17124360
13. Wright LJ, Williams SE, Veldhuijzen van Zanten JJ. Physical activity protects against the negative impact of coronavirus fear on adolescent mental health and well-being during the COVID-19 pandemic. Front Psychol. 2021;12. doi:10.3389/fpsyg.2021.580511
14. Low RS, Overall N, Chang V, Henderson AM, Sibley CG, Girme YU. Emotion regulation and psychological and physical health during a nationwide COVID-19 lockdown. Emotion. 2020;20:1005–1019. doi:10.31234/osf.io/pkncy
15. Ammar A, Chtourou H, Boukhris O, et al. Covid-19 home confinement negatively impacts social participation and life satisfaction: a worldwide multicenter study. Int J Environ Res Public Health. 2020;17(17):6237. doi:10.3390/ijerph17176237
16. Kaur H, Singh T, Arya YK, Mittal S. Physical Fitness and exercise during the COVID-19 pandemic: a qualitative enquiry. Front Psychol. 2020;11:11. doi:10.3389/fpsyg.2020.590172
17. Chtourou H, Trabelsi K, H’mida C, et al. Staying physically active during the quarantine and self-isolation period for controlling and mitigating the covid-19 pandemic: a systematic overview of the literature. Front Psychol. 2020;11:11. doi:10.3389/fpsyg.2020.01708
18. Bavel JJ, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4(5):460–471. doi:10.1038/s41562-020-0884-z
19. Shahrour G, Dardas LA. Acute stress disorder, coping self‐efficacy and subsequent psychological distress among nurses amid Covid‐19. J Nurs Manag. 2020;28(7):1686–1695. doi:10.1111/jonm.13124
20. Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of covid-19 quarantine: special focus in older people. Prog Cardiovasc Dis. 2020;63(3):386–388. doi:10.1016/j.pcad.2020.03.009
21. Lehnert K, Sudeck G, Conzelmann A. Subjective well-being and exercise in the second half of Life: a critical review of theoretical approaches. Eur Rev Aging Phys Act. 2012;9(2):87–102. doi:10.1007/s11556-012-0095-3
22. De Oliveira Neto L, Elsangedy HM, Tavares VD, Teixeira CV, Behm DG, Da Silva-Grigoletto ME. #traininginhome - home-based training during COVID-19 (SARS-COV2) pandemic: physical exercise and behavior-based approach. Rev Bras Fisiol Exerc. 2020;19(2):9–19. doi:10.33233/rbfe.v19i2.4006
23. Lindwall M, Aççı FH. Physical activity and self-esteem. Phys Act Ment Health. 2014. doi:10.5040/9781492595724.ch-005
24. Elsayed M, Schönfeldt-Lecuona C, Welte XA, et al. Psychological distress, fear and coping strategies during the second and third waves of the COVID-19 pandemic in Southern Germany. Front Psychiatry. 2022:13. doi:10.3389/fpsyt.2022.860683
25. Aldwin CM, Brustrom J. Theories of coping with Chronic Stress. Cop Chronic Stress. 1997;75–103. doi:10.1007/978-1-4757-9862-3_3
26. Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216–269. doi:10.1037/0033-2909.129.2.216
27. Sang X, Menhas R, Saqib ZA, et al. The psychological impacts of covid-19 home confinement and physical activity: a structural equation model analysis. Front Psychol. 2021:11. doi:10.3389/fpsyg.2020.614770
28. Turpin G. Perspectives in cardiovascular psychophysiology J.T. Cacioppo and R.E. Petty (eds.), (Guildford Press, New York, 1982) pp. XV + 392. Biol Psychol. 1985;21(2):145–148. doi:10.1016/0301-0511(85)90014-6
29. Rogers RW. A protection motivation theory of fear appeals and Attitude change1. J Psychol. 1975;91(1):93–114. doi:10.1080/00223980.1975.9915803
30. Hamadi HY, Zakari NM, Jibreel E, Nami FN AL, Smida JA, Ben Haddad HH. Stress and coping strategies among nursing students in clinical practice during COVID-19. Nurs Rep. 2021;11(3):629–639. doi:10.3390/nursrep11030060
31. Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behavior: a meta-analytic review of protection motivation theory. J Appl Soc Psychol. 2000;30(1):106–143. doi:10.1111/j.1559-1816.2000.tb02308.x
32. Aldwin C. Stress and Coping Across the Lifespan. Oxford Handbooks Online; 2010.
33. Scheier MF, Carver CS. Optimism, coping, and Health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4(3):219–247. doi:10.1037/0278-6133.4.3.219
34. Shillington KJ, Vanderloo LM, Burke SM, Ng V, Tucker P, Irwin JD. Ontario adults’ health behaviors, mental health, and overall well-being during the COVID-19 pandemic. BMC Public Health. 2021;21(1). doi:10.1186/s12889-021-11732-6
35. Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during covid-19 pandemic in Italy. Heliyon. 2020;6(6):e04315. doi:10.1016/j.heliyon.2020.e04315
36. Violant-Holz V, Gallego-Jiménez MG, González-González CS, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2020;17(24):9419. doi:10.3390/ijerph17249419
37. Herbert C, Gilg V, Sander M, Kobel S, Jerg A, Steinacker JM. Preventing mental health, well-being and physical activity during the Corona pandemic – recommendations from psychology and sports medicine. Ger J Sport Med. 2020;71(10):249–257. doi:10.5960/dzsm.2020.458
38. Marconcin P, Werneck AO, Peralta M, et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health. 2022;22(1). doi:10.1186/s12889-022-12590-6
39. Sudom KA, Lee JEC. Well-being of Canadian Armed Forces members during the COVID-19 pandemic: the influence of positive health behaviours. Health Promot Chronic Dis Prev Can. 2022;42(3):113–121. doi:10.24095/hpcdp.42.3.05
40. Ellis LA, Lee MD, Ijaz K, Smith J, Braithwaite J, Yin K. Covid-19 as ‘game changer’ for the physical activity and mental well-being of augmented reality game players during the pandemic: mixed methods survey study. J Med Internet Res. 2020;22(12):e25117. doi:10.2196/25117
41. Plante TG, Rodin J. Physical fitness and enhanced psychological health. Curr Psychol. 1990;9(1):3–24. doi:10.1007/bf02686764
42. Stanton R, Happell B, Reaburn P. The mental health benefits of regular physical activity, and its role in preventing future depressive illness. Nursing. 2014;45. doi:10.2147/nrr.s41956
43. Yu J, Park J, Hyun SS. Impacts of the COVID-19 pandemic on employees’ work stress, well-being, mental health, organizational citizenship behavior, and employee-customer identification. J Hosp Mark Manag. 2021;30(5):529–548. doi:10.1080/19368623.2021.1867283
44. Shen P, Slater P. The effect of occupational stress and coping strategies on mental health and emotional well-being among university academic staff during the COVID-19 Outbreak. Int Educ Stud. 2021;14(3):82. doi:10.5539/ies.v14n3p82
45. Fuentes AV, Jacobs RJ, Ip E, Owens RE, Caballero J. Coping, resilience, and emotional well-being in pharmacy students during the COVID-19 pandemic. Ment Health Clin. 2021;11(5):274–278. doi:10.9740/mhc.2021.09.274
46. Melnyk BM, Tan A, Hsieh AP, Amaya M, Regan EP, Stanley L. Beliefs, mental health, healthy lifestyle behaviors and coping strategies of college faculty and staff during the COVID-19 pandemic. J Am Coll Health. 2021;1–11. doi:10.1080/07448481.2021.1991932
47. Kim JH, Shim Y, Choi I, Choi E. The role of coping strategies in maintaining well-being during the COVID-19 outbreak in South Korea. Soc Psychol Personal Sci. 2021;13(1):320–332. doi:10.1177/1948550621990595
48. Shpakou A, Krajewska-Kułak E, Cybulski M, et al. Stress perception and coping strategies of students on both sides of the E.U.’s eastern border during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(16):10275. doi:10.3390/ijerph191610275
49. Thai TT, Le PT, Huynh QH, Thu Pham PT T, Bui HT. Perceived stress and coping strategies during the COVID-19 pandemic among public health and Preventive Medicine students in Vietnam. Psychol Res Behav Manag. 2021;14:795–804. doi:10.2147/prbm.s317059
50. Lotzin A, Ketelsen R, Krause L, Ozga A-K, Böttche M, Schäfer I. The pandemic coping scale – validity and reliability of a brief measure of coping during a pandemic. Health Psychol Behav Med. 2022;10(1):762–785. doi:10.1080/21642850.2022.2112198
51. Pilch I, Wardawy P, Probierz E. The predictors of adaptive and maladaptive coping behavior during the COVID-19 pandemic: the Protection Motivation Theory and the big five personality traits. PLoS One. 2021;16(10). doi:10.1371/journal.pone.0258606
52. Drinkwater BL. A comparison of the direction-of-perception technique with the Likert method in the measurement of attitudes. J Soc Psychol. 1965;67(2):189–196. doi:10.1080/00224545.1965.9922270
53. Simms LJ. Classical and modern methods of psychological scale construction. Soc Personal Psychol Compass. 2007;2(1):414–433. doi:10.1111/j.1751-9004.2007.00044.x
54. Oosterveld P, Vorst HC, Smits N. Methods for questionnaire design: a taxonomy linking procedures to test goals. Qual Life Res. 2019;28(9):2501–2512. doi:10.1007/s11136-019-02209-6
55. Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11(5):80. doi:10.4103/sja.sja_203_17
56. Bachl M. Conditional process modeling (mediation analysis, moderated mediation analysis, moderation analysis, and mediated moderation analysis). Int Encyclopedia Commun Res Methods. 2017;1–26. doi:10.1002/9781118901731.iecrm0038
57. Fornell C, Yi Y. Assumptions of the two-step approach to latent variable modeling. Sociol Methods Res. 1992;20(3):291–320. doi:10.1177/0049124192020003001
58. Hair JF, Hult GT, Ringle CM, Sarstedt M, Thiele KO. Mirror, mirror on the wall: a comparative evaluation of composite-based structural equation modeling methods. J Acad Mark Sci. 2017;45(5):616–632. doi:10.1007/s11747-017-0517-x
59. MacKinnon DP. Introduction to Statistical Mediation Analysis. New York: Erlbaum; 2008.
60. Vinzi VE. Handbook of Partial Least Squares: Concepts, Methods and Applications. Berlin: Springer; 2010.
61. Lorente L, Vera M, Peiró T. Nurses’ stressors and psychological distress during the COVID-19 pandemic: the mediating role of coping and resilience. J Adv Nurs. 2021;77(3):1335–1344. doi:10.1111/jan.14695
62. Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. Eur J Pers. 1987;1(3):141–169. doi:10.1002/per.2410010304
63. Malek Rivan NF, Shahar S, Singh DK, et al. Mediation effect of coping strategies on general psychological health among middle-aged and older adults during the COVID-19 pandemic. Aging Ment Health. 2021;26(10):2039–2047. doi:10.1080/13607863.2021.1972281
64. Shamblaw AL, Rumas RL, Best MW. Coping during the COVID-19 pandemic: relations with mental health and quality of life. Can Psychol. 2021;62(1):92–100. doi:10.1037/cap0000263
65. Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. Coping strategies mediate the associations between COVID-19 experiences and mental health outcomes in pregnancy. Arch Womens Ment Health. 2021;24(6):1007–1017. doi:10.1007/s00737-021-01135-2
66. Ye Z, Yang X, Zeng C, et al. Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Appl Psychol. 2020;12(4):1074–1094. doi:10.1111/aphw.12211
67. Pigaiani Y, Zoccante L, Zocca A, et al. Adolescent lifestyle behaviors, coping strategies and subjective well-being during the COVID-19 pandemic: an online student survey. Healthcare. 2020;8(4):472. doi:10.3390/healthcare8040472
68. Bourduge C, Teissedre F, Morel F, Flaudias V, Izaute M, Brousse G. Lockdown impact on stress, coping strategies, and substance use in teenagers. Front Psychiatry. 2022;12. doi:10.3389/fpsyt.2021.790704
69. Mazyarkin Z, Peleg T, Golani I, Sharony L, Kremer I, Shamir A. Health benefits of a physical exercise program for inpatients with mental health; a pilot study. J Psychiatr Res. 2019;113:10–16. doi:10.1016/j.jpsychires.2019.03.002
70. Chen -C-C, Hy-j W, Yeh M-J, Wang AH-E. Comparing stress and behavioral coping strategies during the early stages of the COVID-19 crisis among domestic and overseas Taiwanese. Sci Rep. 2022;12(1). doi:10.1038/s41598-022-15567-y
71. Girma A, Ayalew E. Covid-19 related stress and coping strategies among adults with chronic disease in southwest Ethiopia. Neuropsychiatr Dis Treat. 2020. doi:10.1101/2020.08.14.20174318
72. Bu F, Bone JK, Mitchell JJ, Steptoe A, Fancourt D. Longitudinal changes in physical activity during and after the first national lockdown due to the COVID-19 pandemic in England. Sci Rep. 2021;11. doi:10.1101/2021.04.21.21255861
73. Lesser IA, Nienhuis CP. The impact of covid-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. 2020;17(11):3899. doi:10.3390/ijerph17113899
74. Whittaker F, Kingston S. Stress, social support, and substance use in the COVID-19 pandemic. Transl Issues Psychol Sci. 2022;8:389–405. doi:10.1037/tps0000322
75. Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (covid-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9(2):103–104. doi:10.1016/j.jshs.2020.02.001
76. Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for adults: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10(1):135. doi:10.1186/1479-5868-10-135
77. Hawkley LC, Capitanio JP. Perceived social isolation, evolutionary fitness and health outcomes: a lifespan approach. Biol Sci. 2015;370(1669):20140114. doi:10.1098/rstb.2014.0114
78. Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9(1):78. doi:10.1186/1479-5868-9-78
79. Stubbs B, Koyanagi A, Hallgren M, et al. Physical activity and anxiety: a perspective from the World Health Survey. J Affect Disord. 2017;208:545–552. doi:10.1016/j.jad.2016.10.028
80. White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med. 2017;52(5):653–666. doi:10.1016/j.amepre.2016.12.008
81. Jurak G, Morrison SA, Leskošek B, et al. Physical activity recommendations during the coronavirus disease-2019 virus outbreak. J Sport Health Sci. 2020;9(4):325–327. doi:10.1016/j.jshs.2020.05.003
82. Mason MR, Hudgins JH, Campbell MS, et al. Changes in physical activity during the initial stages of the COVID-19 pandemic. J Sports Sci. 2021;40(1):116–124. doi:10.1080/02640414.2021.1976569
83. Farah BQ, Do Prado WL, Malik N, et al. Barriers to physical activity during the COVID-19 pandemic in adults: a cross-sectional study. Sport Sci Health. 2021;17(2):441–447. doi:10.1007/s11332-020-00724-5
84. Park AH, Zhong S, Yang H, Jeong J, Lee C. Impact of covid-19 on physical activity: a rapid review. J Glob Health. 2022;12. doi:10.7189/jogh.12.05003
85. Sari DK, Mani S, Fadli M, et al. Is it important to increase physical activity among university students during the second-wave covid-19 pandemic in Asian countries? A cross-sectional study of the knowledge, attitudes, and practices in Asian countries. J Multidiscip Healthc. 2022;15:1559–1571. doi:10.2147/jmdh.s368635
86. Czyż SH, Starościak W. Perceived physical activity during stay-at-home covid-19 pandemic lockdown March–April 2020 in Polish adults. Peer J. 2022;10:e12779. doi:10.7717/peerj.12779
87. Strain T, Sharp SJ, Spiers A, et al. Population level physical activity before and during the first national COVID-19 lockdown: a nationally representative repeat cross-sectional study of 5 years of active lives data in England. Lancet Reg Health. 2022;12:100265. doi:10.1016/j.lanepe.2021.100265
88. Fang P, Shi S, Menhas R, Laar RA, Saeed MM. Demographic characteristics and digital platforms for physical activity among the Chinese residents during the COVID-19 pandemic: a mediating analysis. J Multidiscip Healthc. 2022;15:515–529. doi:10.2147/JMDH.S354984
89. Yang J, Menhas R, Dai J, et al. Virtual Reality Fitness (VRF) for behavior management during the COVID-19 pandemic: a mediation analysis approach. Psychol Res Behav Manag. 2022;15:171–182. doi:10.2147/PRBM.S350666
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
