Back to Journals » OncoTargets and Therapy » Volume 11
Renal Ewing sarcoma/primitive neuroectodermal tumor in a pregnant woman who underwent robot-assisted laparoscopic nephrectomy: a case report and literature review
Authors Miao C, Yang J, Xue J, Zhu J, Chen W, Qin Y, Wang Z
Received 30 October 2017
Accepted for publication 7 March 2018
Published 11 October 2018 Volume 2018:11 Pages 6839—6843
DOI https://doi.org/10.2147/OTT.S155523
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yao Dai
Chenkui Miao,1,* Jie Yang,1,* Jianxin Xue,1,* Jundong Zhu,1 Wen Chen,2 Yuan Qin,1 Zengjun Wang1
1State Key Laboratory of Reproductive Medicine and Department of Urology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, People’s Republic of China; 2Department of Pathology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Abstract: Primary Ewing sarcoma/primitive neuroectodermal tumor (ES/PNET) of the kidney represents a spectrum of rare neoplasm with dismal clinical prognosis. This type of malignant tumor predominantly occurs in the soft tissue and bones of pediatric–young adults, and it may rarely arise from the kidney. Derived from the neuroectoderm, renal ES/PNET belongs to a group of primitive and aggressive tumors in its biological manifestation. Herein, we report the case of a 40-year-old pregnant woman with renal mass, in whom was found gross hematuria and slight lumbar acid during pregnancy. A computed tomography scan revealed an irregular soft tissue mass approximately 5×5×5 cm in size. The patient underwent robot-assisted laparoscopic nephrectomy of the right kidney after childbirth. The diagnosis of renal ES/PNET was confirmed by immunohistochemical detection and fluorescence in situ hybridization of the nephrectomy specimen. Primary renal ES/PNET represents a rare and lethal entity, especially in a 40-year-old pregnant woman. Although the clinical presentation of this tumor is nonspecific, renal ES/PNET frequently exert dismal prognosis and aggressive clinical outcomes. Thus, it is essential to distinguish ES/PNET from other renal cell carcinomas and carry out an optimum treatment strategy as soon as possible.
Keywords: Ewing sarcoma, primitive neuroectodermal tumor, kidney, pregnancy, robot-assisted surgery
Introduction
Ewing sarcoma/primitive neuroectodermal tumors (ES/PNET), as a malignant neoplasm, originate from neuroectoderm and neural crest cells and have been broadly reported to arise from the soft tissue and bones.1,2 Exceptionally rare, this kind of tumor presents as a primary malignant lesion of the kidney.3 Since first described in 1975, only a small case series of primary renal ES/PNET have been reported worldwide, with a summary of 116 cases diagnosed at a median age of 27–28 years old in a meta-analysis.4,5 Primary ES/PNET of the kidney in a pregnant woman is extremely rare with only one female reported recently, and no description of an elderly pregnant woman has been reported yet.6 Herein, we present a case report of primary renal ES/PNET in an elderly pregnant woman who underwent robot-assisted laparoscopic nephrectomy and the immunohistochemical staining and fluorescence in situ hybridization (FISH) of the nephrectomy specimen.
Case presentation
A 40-year-old woman presented with continuous hematuria and discomfort in her right lumbar for 5 months. Previous medical history indicated that the complaint of right-side lumbago occurred at approximately 6 months of pregnancy, and the symptom of hematuria began 7 months after pregnancy. Taking her pregnancy into account, no additional imaging examination was carried out except an abdominal B-ultrasound scan, which revealed a palpable mass in the right lumbar region. A blood routine examination showed a mild anemia. Accordingly, urine detection described the presence of red blood cells (RBCs) as well as positive occult blood in the urine. Considering the pregnancy, she was required only to control relevant symptoms and check regularly with follow-ups to monitor the course of the disease, until childbirth. During the pregnancy period, the volume of renal mass grew rapidly, from 26×21 mm to 47×39 mm in just 2 months. We could speculate that this kind of rare tumor might be related to hormonal changes associated with pregnancy.
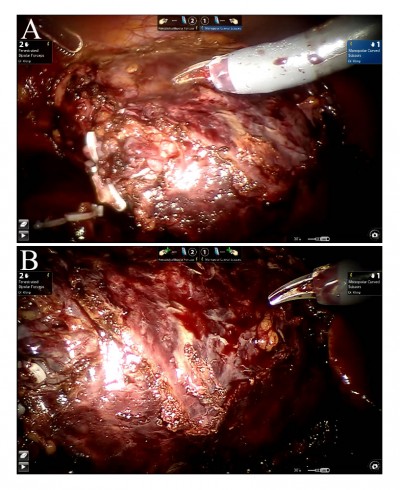
The patient gave birth to a healthy baby when it was due. After delivery, abdominal CT was performed and revealed a right renal enhancing mass about 5 cm in length, accompanied by the parenchyma invasion and pelvis expansion of the right kidney (Figure 1). Fortunately, there was no obviously abnormal density of the bilateral adrenal and left renal parenchyma. The morphology, size and density of liver, gallbladder, pancreas and spleen were found to have no obvious abnormalities. Subsequently, we performed robot-assisted laparoscopic nephrectomy for the patient and removed the entire right kidney successfully (Figure 2A–B).
  | Figure 2 (A and B) Removing the entire right kidney under robot-assisted laparoscopic nephrectomy. |
Microscopically, histologic analysis of hematoxylin and eosin (H&E) staining revealed that the tumors were composed of a monotonous population of small round cells. Extensive necrosis was also observed in histologic sections (Figure 3A–B). For further confirmation, immunohistochemical staining showed positive expression for CD99, SYN, FLI1 and 30% positive staining for Ki67 (Figure 3C–F). FISH analysis demonstrated more than 10% of cells were positive, indicating EWSR1 gene rearrangement (Figure 4).
  | Figure 4 Fluorescence in situ hybridization testing demonstrated that more than 10% of cells were positive indicating EWSR1 gene rearrangement. |
After surgery, the patient was given continuous anti-inflammatory and symptomatic treatments until gradually recovering. Moreover, no obvious complications occurred during the postoperative course of the patient who then received periodic reexaminations. Until now, no related recurrence or progression was found and the patient is still alive. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images published.
Discussion and review of the literature
Accounting for 10% of all sarcomas, ES/PNET belongs to a monomorphic small round cell tumor originating from neural crest.7 Primary renal ES/PNET as a member of the ES/PNET family is a rare entity, which was first discovered in 1975.4 Reports of pregnant women with ES/PNET of the kidney are extremely unusual, and only a single case has been defined worldwide.6 Considering its aggressive progression and dire survival rate, distinguishing an ES/PNET from another renal mass is essential for an accurate diagnosis as well as therapeutic strategies. The majority of differential diagnoses for the small round cell neoplasms includes the following types: Wilms’ tumor, neuroblastoma, lymphoma, ES and PNET.8
Diagnosis of renal ES/PNET has predominantly relied on the histopathology and immunohistochemistry analysis of resected specimens. For immunohistochemistry examination, the tumor cells of ES/PNET are typically positive for CD99 and FLI-1 in more than 90% of cases. However, CD99 has been found to be primarily nonspecific in confirming its diagnosis, thus other typical biomarkers including SYN, FLI1 and Ki67 ought to be detected.9,10
We have described a case report of primary ES/PNET of the kidney in an elderly pregnant woman, which was diagnosed by immunohistochemistry and FISH testing of the resected specimen. The patient was pregnant at an age of 39, during which period the renal mass was discovered and grew rapidly. Concerning the pregnancy, this woman determined to receive treatment after delivery. Subsequently, she was referred to our department, with the chief complaint of gross hematuria. We performed robot-assisted laparoscopic radical nephrectomy and after surgery, immunohistochemical and FISH analysis of the tumor tissues confirmed the diagnosis of ES/PNET.
Previous studies have revealed that primary renal ES/PNET displayed more aggressive behavior than that of other sites.11 Nearly 20%–50% of patients were diagnosed with distant metastases, most commonly to regional lymph nodes as well as the lung, bone and liver.12 In addition, the 5-year overall survival remains low and fewer patients survive longer than 5 year after diagnosis.13 In this case, even though the patient delayed treatment until after childbirth, no distant metastases of other organs were found at diagnosis. Therefore, timely surgical therapy is essential for the inhibition of tumor recurrence. Generally, renal ES/PNET with metastases to other sites could significantly decrease the patients’ overall survival in comparison with localized lesions.14 Meanwhile, an advanced robot-assisted technique was applied to the whole surgical procedure, which alleviated the patient’s distress to some extent, as well as greatly accelerated the recovery process.
Conclusion
In this case, we reported a rare renal ES/PNET in a pregnant woman treated with robot-assisted laparoscopic nephrectomy, pathological analysis, immunohistochemical and FISH testing of the tumorous specimen. Because of the rarity and malignancy of this tumor, it is essential to obtain an early-stage confirmation and begin with timely surgical treatment.
Acknowledgment
This work was supported by a grant from the National Natural Science Foundation of China (Nos 81270685 and 81771640).
Author contributions
ZW made contributions to the design of this study. WC and YQ performed the pathological analysis. JX carried out the study. JZ collected important background information. CM drafted the manuscript. JY conceived of this study and helped to draft the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Venkitaraman R, George MK, Ramanan SG, Sagar TG. A single institution experience of combined modality management of extra skeletal Ewings sarcoma. World J Surg Oncol. 2007;5:3. | ||
Ozkanli SS, Yildirim A, Zemheri E, Gucer FI, Aydin A, Caskurlu T. Primary synovial sarcoma of the kidney. Urol Int. 2014;92(3):369–372. | ||
Maeda M, Tsuda A, Yamanishi S, et al. Ewing sarcoma/primitive neuroectodermal tumor of the kidney in a child. Pediatr Blood Cancer. 2008;50(1):180–183. | ||
Seemayer TA, Thelmo WL, Bolande RP, Wiglesworth FW. Peripheral neuroectodermal tumors. Perspect Pediatr Pathol. 1975;2:151–172. | ||
Risi E, Iacovelli R, Altavilla A, et al. Clinical and pathological features of primary neuroectodermal tumor/Ewing sarcoma of the kidney. Urology. 2013;82(2):382–386. | ||
Ding Y, Huang Z, Ding Y, et al. Primary Ewing’s of kidney with caval involvement in a pregnant woman. Urol Int. 2016;97(3):365–368. | ||
Funahashi Y, Hattori R, Yamamoto T, et al. Ewing’s sarcoma/primitive neuroectodermal tumor of the kidney. Aktuelle Urol. 2009;40(4):247–249. | ||
Zöllner S, Dirksen U, Jürgens H, Ranft A. Renal Ewing tumors. Ann Oncol. 2013;24(9):2455–2461. | ||
Celli R, Cai G. Ewing sarcoma/primitive neuroectodermal tumor of the kidney: a rare and lethal entity. Arch Pathol Lab Med. 2016;140(3):281–285. | ||
Antonescu C. Round cell sarcomas beyond Ewing: emerging entities. Histopathology. 2014;64(1):26–37. | ||
Sun C, Du Z, Tong S, et al. Primitive neuroectodermal tumor of the kidney: case report and review of literature. World J Surg Oncol. 2012;10:279. | ||
Pakravan A, Vo TM, Sandomirsky M, Bastani B. Primary Ewing sarcoma of kidney in an elderly. Iran J Kidney Dis. 2012;6(4):307–310. | ||
Chakrabarti I, De A, Giri A. Primitive neuroectodermal tumor (PNET) of kidney – a rare entity. Iranian J Pathol. 2011;6(3):147–152. | ||
Teegavarapu PS, Rao P, Matrana MR, et al. Outcomes of adults with Ewing sarcoma family of tumors (ESFT) of the kidney: a single-institution experience. Am J Clin Oncol. 2017;40(2):189–193. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


